Abstract
Gardner Syndrome is a rare disease with clinical manifestations of familial intestinal polyposis with osteomas. Cutaneous and subcutaneous lesions are common and epidermoid cyst is a characteristic dermatologic finding. This case report presents a novel finding of an intracranial epidermoid situated in the fourth ventricle in a patient with Gardner Syndrome. This intracranial epidermoid has been followed with sequential magnetic resonance imaging (MRI) for 10 years with progressive growth of the lesion. This suggests the conservative management is an option in patients with an enlarging epidermoid cyst in the fourth ventricle.
Plain language summary
Non-operative treatment of a cyst in the brain in a syndrome called Gardner syndrome.
What is Gardner syndrome?
Gardner syndrome is a rare disease and form of familial adenomatous polyposis (FAP) that is characterized by multiple small growths of cells (polyps) in the colon and various types of tumors, both noncancerous (benign) and cancerous (malignant). It is caused by changes (mutations) in the APC gene. Abnormal changes on the skin and under the skin are common as well as growths called epidermoid cysts. The cysts develop when cells that are meant to become skin, hair, and nails (epithelial cells) are trapped among the cells that form the brain. Epidermoid brain cysts may be diagnosed by magnetic resonance imaging (MRI) and computerized tomography (CT) scans. Typical treatment usually involves surgery.
What was the aim of this case report?
To present a different management strategy for patients with Gardner Syndrome with epidermoid brain cysts.
How was this patient treated?
This patient is the first patient with Gardner Syndrome with a very rare epidermoid brain cyst reported to be treated in a conservative manner.
The patient was monitored for 10 years with regular MRI scans and the cyst continued to grow over this time.
Despite this growth the patient has shown no signs of a buildup of fluid in the cavities deep within the brain (called hydrocephalus).
The patient experienced nonfocal headaches, which were relieved with medication so doctors decided not to surgically remove the cyst.
Why is this case important?
Conservative management of epidermoid brain cysts in Gardner patients has not been reported before. This case report shows that conservative management may be an alternative option for patients with a growing epidermoid cyst in the fourth ventricle of the brain. Conservative treatment is designed to avoid invasive treatments or surgery and provides a different option for patients who are unable to have surgery.
Keywords: epidermoid, Gardner syndrome, intracranial
Introduction
Gardner syndrome is an intestinal polyposis syndrome with associated bone tumors: osteomas. Cutaneous and subcutaneous manifestations are common as well, with epidermoid cysts representing the most common lesion.1 Intracranial epidermoid cyst can occur most commonly in the cerebellar pontine angle cistern. Intraventricular epidermoids are distinctly rare.2,3 When present, surgical management is the standard of care in the treatment of an intracranial epidermoid cyst.4–6 Conservative management of intracranial epidermoid cyst has not been reported previously in the literature.
Case report
A 42-year-old male with a clinical history of Gardner syndrome and multiple sclerosis underwent magnetic resonance imaging (MRI) evaluation which revealed a 1.8 cm heterogeneous mass without enhancement within the fourth ventricle (Figure 1). The mass restricted diffusion and was followed subsequently by the Department of Neurosurgery (Figure 2). The mass demonstrated progressive enlargement and, at 10 years, now measures 2.7 cm in greatest dimension (Figure 3). While the lesion has increased in size, the ventricular system is overall stable in appearance. The patient has exhibited no clinical manifestations of hydrocephalus, complaining only of rare, nonfocal headaches, which were relieved with acetaminophen 325 mg. Given the lack of clinical symptoms, the treating neurosurgeon and patient have opted for conservative management.
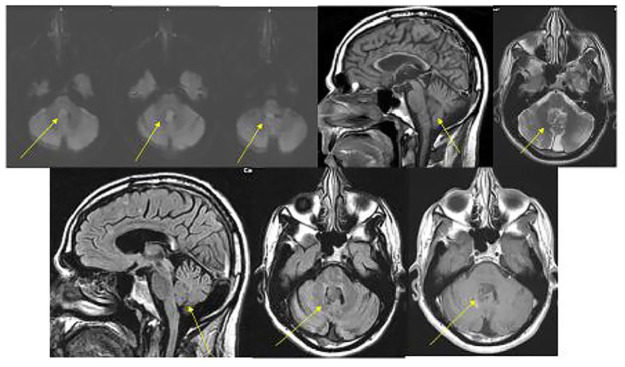
Figure 1.
Initial MRI study demonstrates an epidermoid situated in the fourth ventricle. The epidermoid restricts diffusion, is heterogeneous on sagittal T1, axial T2 weighted and FLAIR images and does not enhance (yellow arrows).
MRI, magnetic resonance imaging.
Figure 2.
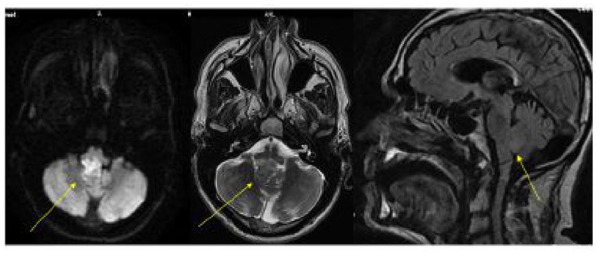
MRI performed 6 years following the initial study reveals interval growth of the epidermoid cyst (yellow arrows).
MRI, magnetic resonance imaging.
Figure 3.
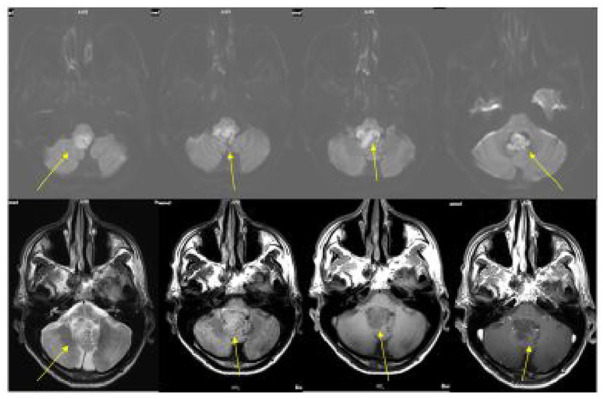
Follow up MRI performed 10 years following initial study reveals progressive enlargement of the epidermoid cyst. The lesion restricts diffusion, is heterogeneous on T2 weighted and flair images and does not enhance (yellow arrows).
MRI, magnetic resonance imaging.
Discussion and implication for clinical care
Gardner syndrome is familial intestinal polyposis with osteomas. Cutaneous and subcutaneous lesions are a common manifestation, with epidermoid the most common lesion noted.1 A subset of these patients can also present with intracranial malignancies, as seen in Turcot syndrome. However, an intracranial epidermoid in Gardner syndrome is distinctly rare, with one case noted in the literature.2 This epidermoid, noted by Leblanc, was situated in the left cerebellar pontine angle cistern, the most common location for intracranial epidermoid.2
Fourth ventricular epidermoid have not been reported previously in Gardner syndrome. Intracranial epidermoid as a whole rarely involve the ventricular system.3,4 They are noted to be slow growing and the typical treatment is surgical.4–6 As such, this is the first report of conservative management of an intracranial epidermoid, especially given its interval growth over a 10 year period.
MRI is the primary method for diagnosis. Epidermoid cysts demonstrates heterogeneous signal characteristics on conventional T1 and T2 weighted images with a paucity of enhancement. However, these lesions restrict diffusion motion, and, therefore, diffusion weighted imaging is the primary imaging sequence for the diagnosis.7
Symptomatology leading to surgical intervention includes posterior fossa symptoms, such as vertigo, nausea and vomiting, and gait abnormalities. In addition, symptoms secondary to hydrocephalus, including visual disturbance secondary to papilledema, as well as dysarthria and hemiparesis, may lead to neurosurgical intervention.4,6
However, neurosurgical intervention is not without its complications, including aseptic meningitis. Complete resection is difficult as the epidermoid can adhere to vital, adjacent tissues.3,4
In addition, epidermoid cysts have been reported in the neurosurgical literature to have up to a 24% incidence of regrowth following resection.8 Two patients, of the seven resected in the Lunardi paper, did recur.3
This case demonstrates novel intracranial findings in Gardner syndrome. Furthermore, this case demonstrates that nonoperative management of fourth ventricular epidermoid is an alternate treatment option, even in the face of continued growth of the lesion.
Footnotes
Author contributions: Gordon D. Heller: Conceptualization; data curation; validation; visualization; writing-original draft; writing-review and editing.
The author declare that there is no conflict of interest.
Ethics statement: This report is original and written by the author. It has not been previously published and has only been submitted to this journal. The report has been referenced appropriately, does not infringe on any rights of others, including privacy rights and intellectual property rights. The case report data is true, not manipulated. This report does not have conflicting or competing interest. Ethical approval is not required for case reports or case series as they are not deemed to constitute research at Mount Sinai. Guidelines on patient consent have been met and written informed consent to publish this case and images was obtained from the patient.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gordon D. Heller  https://orcid.org/0000-0001-9792-5699
https://orcid.org/0000-0001-9792-5699
References
- 1. Vijay K, Choudhary AK. Multiple scalp epidermoid cysts in a child with Gardner syndrome. Pediatr Radiol 2010; 40(Suppl. 1): S172. [DOI] [PubMed] [Google Scholar]
- 2. Leblanc R. Familial adenomatous polyposis and benign intracranial tumors: a new variant of Gardner’s syndrome. Can J Neurol Sci 2000; 27: 341–346. [DOI] [PubMed] [Google Scholar]
- 3. Lunardi P, Missori P, Gagliardi FM, et al. Epidermoid tumors of the 4th ventricle: report of seven cases. Neurosurgery 1990; 27: 532–534. [DOI] [PubMed] [Google Scholar]
- 4. Liu M, Liu Y, Zhu S, et al. Intraventricular epidermoids. J Clin Neurosci 2006; 13: 428–430. [DOI] [PubMed] [Google Scholar]
- 5. Franko A, Holiar-Erlic I, Miletic D. Lateral ventricle epidermoid. Radiol Oncol 2008; 42: 66–68. [Google Scholar]
- 6. Fiume D, Gazzer G, Spallone A, et al. Epidermoid cysts of the fourth ventricle. Surg Neurol 1988; 29: 178–182. [DOI] [PubMed] [Google Scholar]
- 7. Sirin S, Gonul E, Kahraman S, et al. Imaging of posterior fossa epidermoid tumors. Clin Neurol Neurosurg 2005; 107: 461–467. [DOI] [PubMed] [Google Scholar]
- 8. Yamakawa K, Shitara N, Genka S, et al. Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery 1989; 24: 568–573. [DOI] [PubMed] [Google Scholar]