Abstract
Immune checkpoint inhibitors (ICIs) could cause type 1 diabetes (T1D). However, the underlying mechanism remains unclear. We immunohistochemically analyzed pancreatic specimens from three individuals with ICI-related T1D, and their histopathological data were compared those from three patients who had received ICI therapy but did not develop T1D (non-T1D) and seven normal glucose-tolerant subjects as control subjects. All ICI-related T1D patients had susceptible HLA haplotypes. In ICI-related T1D, the β-cell area decreased and the α-cell area increased compared with non-T1D and control subjects. The number of CD3-positive cells around islets increased in ICI-related T1D and non-T1D compared with control subjects, while the number of CD68-positive cells around islets increased in ICI-related T1D compared with non-T1D and control subjects. The expression ratios of programmed death-ligand 1 (PD-L1) on islets decreased in non-T1D and almost completely disappeared in ICI-related T1D, while PD-L1 expression was observed in most cells of pancreatic islets in control subjects. This study, therefore, indicates that ICI therapy itself could reduce PD-L1 expression on islets in all subjects, which may be related to β-cell vulnerability. In addition, we showed that absence of PD-L1 expression on β-cells, genetic susceptibility, and infiltration of macrophages as well as T lymphocytes around islets might be responsible for T1D onset.
ARTICLE HIGHLIGHTS
Immune checkpoint inhibitors (ICIs) could cause type 1 diabetes (T1D). However, the underlying mechanism remains unclear.
Pancreatic histological findings of ICI-related T1D patients were compared with those of patients who had received ICI therapy but did not develop T1D (non-T1D) and control subjects.
Programmed death-ligand 1 expression on islets decreased in non-T1D and almost completely disappeared in ICI-related T1D, while it was observed in control subjects. Patients with ICI-related T1D had T1D-susceptible HLA haplotypes and islet inflammation.
ICIs may decrease programmed death-ligand 1 expression on islets, and its absence and additional islet inflammation in genetically susceptible patients can lead to development of T1D.
Introduction
Immune checkpoint proteins, such as cytotoxic T lymphocyte antigen 4 (CTLA-4) and programmed death-ligand 1 (PDL-1), negatively regulate T-cell activation and maintain self-tolerance (1). Inhibition of these pathways leads to activation of the immune system and can stimulate immune responses against tumor cells (2,3). However, immune checkpoint inhibitors (ICIs) can also cause immune-related adverse events in some patients, including hypophysitis, thyroiditis, and type 1 diabetes (T1D) (4).
There have been many clinical case reports and case-based systematic reviews of ICI-related T1D (5,6). However, there has been little information about the pancreatic histopathology of ICI-related T1D. We first in the world immunohistochemically analyzed the pancreas of a patient who developed T1D after administration of anti–CTLA-4 and anti–programmed death (PD)-1 antibodies (7) and found β-cell depletion, infiltration of T cells into islets, negative expression of PD-L1 on β-cells, and low expression levels of PD-L1 on α-cells. However, there have been few reports in the literature on the pancreas tissue of ICI-related T1D, and whether these histological findings are characteristic of ICI-related T1D remains unclear. The purpose of this study was to clarify, by newly examining pancreatic tissues of those who did not develop T1D after receiving ICI (non-T1D patients), the differences as well as the similarities in histological findings between ICI-related T1D and non-T1D patients.
Research Designs and Methods
Subjects
We enrolled three ICI-related T1D patients, three non-T1D patients, and seven control subjects. Two autopsy case patients with ICI-related T1D were entered into our research (cases 1 and 2), and their pancreases were immunohistochemically analyzed in addition to the previously reported surgical case patient with T1D (case 3) (7). One of the non-T1D case patients was a case of surgical resection (case 4), and two of the non-T1D case patients were autopsy cases (cases 5 and 6). The clinical course of case 6 was previously reported (8). Control subjects were individuals who were diagnosed with normal glucose tolerance preoperatively and had undergone pancreatic resection between 2008 and 2013 in Osaka University Hospital. All control samples were included in our previous study (9). The case presentations as well as the clinical characteristics and laboratory data of the ICI-related T1D patients are shown in Supplementary Materials and Table 1. The clinical characteristics and laboratory data of the non-T1D patients and the control subjects are also shown in Supplementary Tables 1 and 2, respectively.
Table 1.
Clinical characteristics and laboratory data in ICI-related T1D patients
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age at onset of T1D (years) | 84 | 55 | 55 |
| Sex | Male | Male | Male |
| Cancer of primary origin | Urothelial carcinoma | Hodgkin lymphoma | Renal cell carcinoma |
| ICI | Pembrolizumab | Nivolumab | Ipilimumab/nivolumab |
| Doses, n | 2 | 5 | 4 / 9 |
| Duration from first administration to T1D onset (month) | 1 | 6 | 5 |
| Plasma glucose (mmol/L) | 62.4 | 18.8 | 36.5 |
| Hemoglobin A1c (mmol/mol) | 49 | 87 | 71 |
| Glycoalbumin (%) | 18.7 | 29.8 | 33.5 |
| Serum C-peptide (nmol/L) | <0.02 | 0.04 | 0.60→<0.03 |
| Urine C-peptide (µg/day) | <0.3 | 1.40 | 5.6 |
| Atrial blood pH | 6.827 | NA | 7.163 |
| Acetoacetic acid (µmol/L) | 2,144 | NA | 3,060 |
| 3-Hydroxybutyrate (µmol/L) | 5,281 | NA | 7,930 |
| Amylase (IU/L)* | 1,109 (44–132) | 53 (44–132) | 108 (44–132) |
| Lipase (IU/L)* | 368 (11–59) | 45 (11–53) | 118 (11–53) |
| Elastase-1 (ng/dL)* | 1,280 (0–300) | 187 (0–300) | NA (0–300) |
| Anti-GAD (units/mL) | >2,000 | 6.8 → — | — |
| Anti-IA2 (units/mL) | 1.3 | — | — |
| Anti-IAA antibodies (units/mL) | NA | — | — |
| HLA | DRB1-DQB1*04:05- *04:01/*08:02-*03:02 | A24, A26 B39, B51 DR4, DR14 | DRB1-DQB1*11:01-*03:01/*09:01-*03:03 |
| Other immune-related adverse events | — | Destructive thyroiditis | — |
| Duration from T1D onset to death or pancreatectomy (month) | 1 | 12 | 24 |
| Extraction method | Autopsy | Autopsy | Total pancreatectomy |
| Collected parts of pancreas (n blocks) | Head (1)/body (1)/tail (1) | Tail (3) | Head (1)/body (1)/tail (1) |
| Pancreatic weight (g) | NA | NA | NA |
IAA, insulin autoantibody; NA, not available.
Values in parentheses indicate standard values in each facility.
Pancreatic Tissue Processing
Normal pancreatic tissues obtained from surgery and autopsy were fixed immediately in formaldehyde, embedded in paraffin for subsequent analysis, and then cut into 5-μm-thick sections. The tissues examined in this study were confirmed to be noncancerous lesions and not adjacent to the tumor by hematoxylin and eosin staining.
Immunohistochemistry
The primary and secondary antibodies and chromogenic substrates used in the current study are listed in Supplementary Table 3.
As a surrogate for α-cell mass and β-cell mass, we evaluated relative α-cell area and relative β-cell area, which was determined by the proportion of glucagon-positive cell area or insulin-positive cell area in the entire pancreatic section, using the indirect immunoperoxidase technique. We used anti-glucagon and anti-insulin Igs primary antibodies and biotinylated Igs secondary antibodies. The reactions were developed with an avidin–biotin complex and a 3,3-diaminobenzidine tetrahydrochloride substrate, followed by methyl green counterstaining.
To evaluate the PD-L1 expression and the infiltration of inflammatory cells in pancreatic section tissue, we performed double immunofluorescence staining with glucagon or insulin and PD-L1 or cell surface markers. We identified CD3-positive cells as T lymphocytes, CD68-positive cells as macrophages, CD4-positive cells as helper T lymphocytes, and CD8-positive cells as cytotoxic T lymphocytes. Pancreatic sections were incubated with anti–PD-L1, CD3, CD68, CD4, or CD8 Igs as primary antibodies and biotinylated Igs as secondary antibodies, followed by streptavidin Alexa Fluor 488 conjugate. Sections were then incubated with anti-glucagon or anti-insulin, followed by Alexa Fluor 546- or 555-conjugated Igs. We observed the pancreatic tissues using an optical microscope and a fluorescence microscope (BX53; Olympus, Tokyo, Japan).
Morphometric Analysis
We basically analyzed one section per block, and one to three sections were analyzed in each case patient, depending on the number of blocks that we could obtain (cases 1–4: 3 blocks, case 5: 2 blocks, case 6: 1 block).
The relative β-cell or α-cell area was quantified digitally using the WinROOF software program (10).
To evaluate the infiltration of inflammatory cells into islets, islets stained with glucagon and >100 µm in diameter were examined, and we regarded inflammatory cells found in the islet periphery and throughout the islet parenchyma as “infiltrating” (11).
To assess the immunofluorescent intensity of PD-L1 on islets, islets >100 µm in diameter were examined. We observed pancreatic tissues in seven sections of four paraffin blocks for β-cells in each ICI-related T1D patient. We randomly selected up to 20 islets for α-cells in each ICI-related T1D patient and for β-cells and α-cells in each control subject or non-T1D patient. We judged PD-L1 was positive when the immunofluorescent intensity of β-cells or α-cells was increased compared with that of the exocrine region. Numbers of the cells coexpressing PD-L1 and insulin or glucagon were divided by total numbers of insulin- or glucagon-positive cells and were presented as a percentage.
Statistical Analysis
Data for the same patient were considered to be normally distributed and summarized by the mean ± SD. When comparing between groups, the mean value of each patient was used as the representative value, and the representative value was regarded as a nonnormal distribution and summarized by the median and interquartile range. All tests were deemed to be exploratory. No adjustment for multiplicity was performed. Group comparisons were done by the exact Wilcoxon test. Differences were considered statistically significant when P ≤ 0.05. All statistical analyses were performed with JMP Pro 15 software (SAS Institute, Cary, NC).
Study Approval
The study protocol was approved by the Osaka University Ethics Committee and was conducted according to the principles of the Declaration of Helsinki. All patients provided informed consent before their participation (approval number 13279-7, 17459-4).
Data and Resource Availability
All data generated or analyzed during this study are included in the published article and its online supplementary files. No applicable resources were generated or analyzed during the current study.
Results
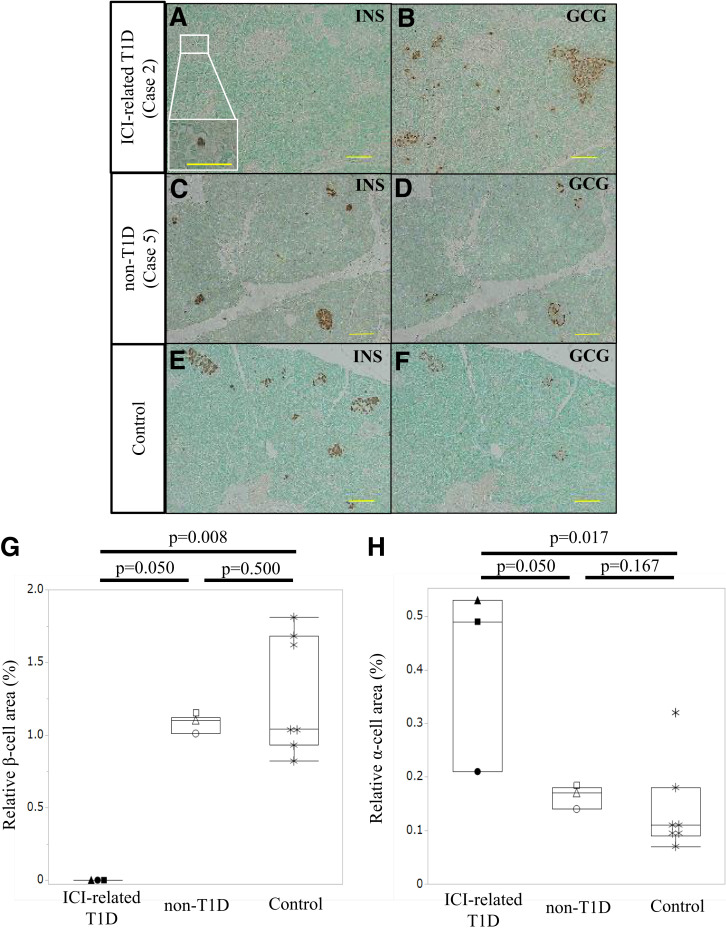
Residual β-Cells and α-Cells
We calculated the relative β-cell area and relative α-cell area in the three groups (Supplementary Table 4). Figure 1A–F shows representative images of insulin and glucagon staining in an ICI-related T1D patient (case 2), a non-T1D patient (case 5), and a control subject. Only a few single β-cells were present in case 2 (Fig. 1A) compared with case 5 (Fig. 1C) and the control subject (Fig. 1E), while α-cells were observed throughout the pancreatic section in case 2 (Fig. 1B), case 5 (Fig. 1D), and the control subject (Fig. 1F). The relative β-cell area in the ICI-related T1D patients was significantly lower than that in the non-T1D patients (P = 0.050) and the control subjects (P = 0.008), while there was no difference between that in the non-T1D patients and control subjects (P = 0.500) (Fig. 1G). The relative α-cell area in the ICI-related T1D patients was significantly higher than that in the non-T1D (P = 0.050) and the control subjects (P = 0.017), while there was no difference between that in the non-T1D patients and control subjects (P = 0.167) (Fig. 1H).
Figure 1.
Residual α-cells and β-cells. Representative images of chromogenic staining for insulin (INS) or glucagon (GCG) shows immunohistochemical analyses in an ICI-related T1D patient (case 2) (A and B), a non-T1D patient (case 5) (C and D), and a control subject (E and F). Chromogenic staining for insulin (A, C, and E) and glucagon (B, D, and F) in serial sections (case 2: A and B, case 5: C and D, control: E and F). Scale bars: 100 µm (A and B), 50 µm (A, inset bar), and 200 µm (C–F). Comparison of the relative β-cell area (G) and relative α-cell area (H) among the three groups. Asterisks (*), control subjects; closed circle (●), case 1; closed triangle (▲), case 2; closed square (■), case 3; open circles (○), case 4; open triangle (▵), case 5; open square (◻), case 6.
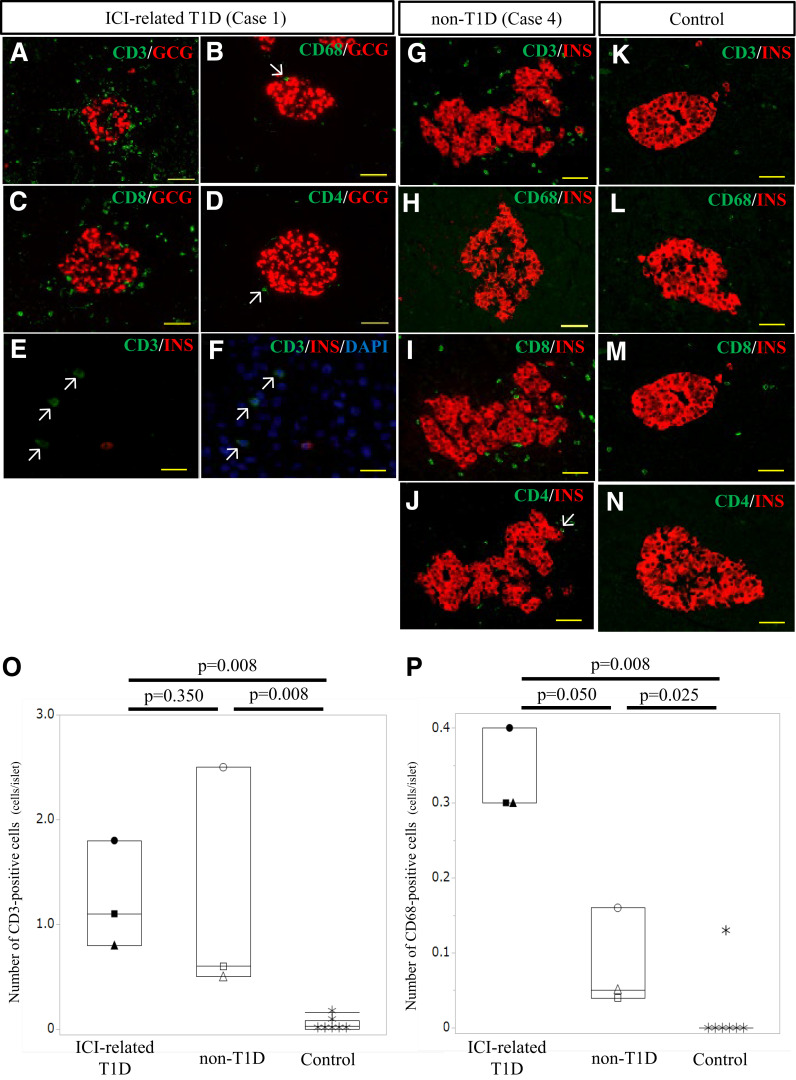
Infiltration of Inflammatory Cells
Next, we evaluated the infiltration of inflammatory cells in pancreatic tissues (Supplementary Table 5). Figure 2A–N shows representative images depicting inflammatory cell infiltration into islets in an ICI-related T1D patient (case 1), a non-T1D patient (case 4), and a control subject. In case 1, many CD3-positive cells (mainly CD8-positive cells) were observed to and around islets (Fig. 2A, C, and D), and a few CD68-positive cells were present around islets (arrow) (Fig. 2B), compared with control subjects (Fig. 2K–N). Several CD3-positive cells infiltrated around single β-cells (Fig. 2E and F). The lobular distribution of insulitis, which had been reported in recent-onset T1D (12), was not observed, and the insulitis was observed throughout the pancreas. In case 4, many CD3-positive cells (mainly CD8-positive cells) were observed to and around islets (Fig. 2G, I, and J), but almost no CD68-positive cells were present (Fig. 2H). The numbers of infiltrating CD3-positive cells in the ICI-related T1D and the non-T1D patients were significantly higher than those in the control subjects (P = 0.008, P = 0.008), while there was no difference between those in the ICI-related T1D and non-T1D patients (P = 0.350) (Fig. 2O). The numbers of infiltrating CD68-positive cells in the ICI-related T1D and the non-T1D patients were significantly higher than those in the control subjects (P = 0.008, P = 0.025), and those in the ICI-related T1D patients were significantly higher than those in the non-T1D patients (P = 0.050) (Fig. 2P). The number of infiltrating CD8-positive cells to and around each islet was higher than the number of infiltrating CD4-positive cells both in the ICI-related T1D and the non-T1D patients (Supplementary Table 5).
Figure 2.
Inflammatory cell infiltration to and around islets and a single β-cell. Representative images of immunofluorescence staining for cell surface markers show immunohistochemical analyses in an ICI-related T1D patient (case 1) (A–F), a non-T1D patient (case 4) (G–J), and a control subject (K–N). Double immunofluorescence staining for glucagon (GCG, red) (A–D) or insulin (INS, red) (E–N), and CD3 (green) (A, E–G, and K), CD68 (green) (B, H, and L), CD8 (green) (C, I, and M), or CD4 (green) (D, J, and N) with DAPI (blue) in case 1 (A–F), case 4 (G–J), and control (K–N). Scale bars: 50 µm (A–D and G–N) and 15 µm (E and F). The arrows point to inflammatory cells around islets and a single β-cell. Comparison of the number of infiltrating CD3-positive cells (O) and CD68-positive cells (P) around each islet among the three groups. Asterisks (*), control subjects; closed circle (●), case 1; closed triangle (▲), case 2; closed square (■), case 3; open circles (○), case 4; open triangle (▵), case 5; and open square (◻), case 6.
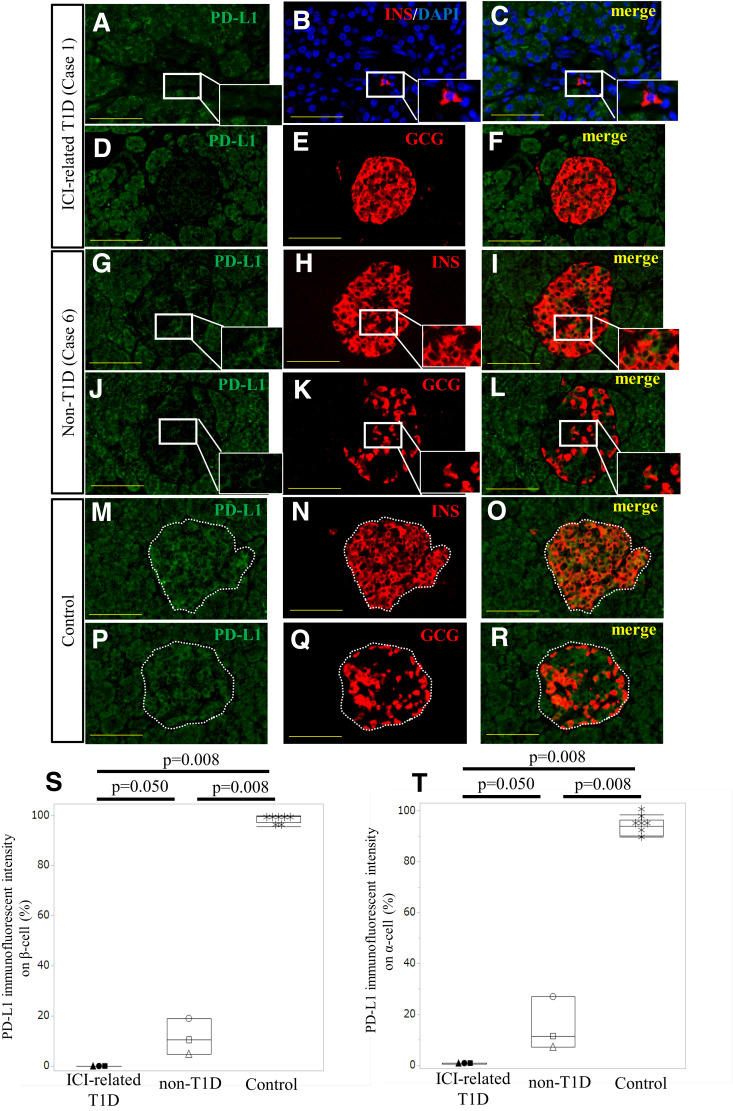
Expression of PD-L1 on β-Cells and α-Cells
Finally, we examined the PD-L1 immunofluorescent intensity on β-cells and α-cells (Supplementary Table 6). Figure 3A–R shows representative images depicting PD-L1 immunofluorescent intensity on islets in an ICI-related T1D patient (case 1), a non-T1D patient (case 6), and a control subject. Almost all β-cells and α-cells expressed PD-L1 in the control subject (Fig. 3M–O and P–R), but no residual β-cells and only a few α-cells expressed PD-L1 in the ICI-related T1D patient (Fig. 3A–C and D–F), while a fraction of β-cells and α-cells faintly expressed PD-L1 in the non-T1D patient (Fig. 3G–I and J–L). The ratios of PD-L1 immunofluorescent intensity on β-cells, both in the ICI-related T1D and the non-T1D patients, were significantly lower than those in the control subjects (P = 0.008, P = 0.008), and those in the ICI-related T1D patients were significantly lower than those in the non-T1D patients (P = 0.050) (Fig. 3S). The ratios of PD-L1 immunofluorescent intensity on α-cells, both in the ICI-related T1D and the non-T1D patients, were significantly lower than those in the control subjects (P = 0.008, P = 0.008), and those in the ICI-related T1D patients were significantly lower than those in the non-T1D patients (P = 0.050) (Fig. 3T).
Figure 3.
Expression of PD-L1 on islets. Representative images of immunofluorescence staining for PD-L1 show immunohistochemical analyses in an ICI-related T1D patient (case 1) (A–F), a non-T1D patient (case 6) (G–L), and a control subject (M–R). Double immunofluorescence staining for PD-L1 (green) (A, C, D, F, G, I, J, L, M, O, P, and R) and insulin (INS; red) (B, C, H, I, N, and O), glucagon (GCG; red) (E, F, K, L, Q, and R), with DAPI (blue) in case 1 (A–F), case 6 (G–L), and a control subject (M–R). Scale bars: 50 µm (A–R). Comparison of PD-L1 immunofluorescent intensity on β-cells (S) and on α-cells (T) among the three groups. Asterisks (*), control subjects; closed circle (●), case 1; closed triangle (▲), case 2; closed square (■), case 3; open circles (○), case 4; open triangle (▵), case 5; open square (◻), case 6.
Discussion
We confirmed the depletion of β-cell area, the increase of α-cell area, and the infiltration of macrophages as well as T lymphocytes to and around the islets in the ICI-related T1D patients. We also revealed the absence of PD-L1 expression on residual β- and α-cells in these patients, which is consistent with the results of our previous report (7) and another report (13). In addition, surprisingly, we revealed that the PD-L1 expression levels on β- and α-cells were also reduced in the non-T1D patients compared with subjects without diabetes without ICI therapy whose PD-L1 immunostaining was positive in this study and was also similar to our previous report (7), although another study showed that it was weakly positive (14). This is the first finding in the world and suggests that ICI therapy itself could affect PD-L1 expression levels on normal islet cells, although the mechanism remains to be elucidated. PD-L1–deficient NOD mice presented early onset of diabetes (15,16). Furthermore, PD-L1 expression was upregulated in residual β-cells under autoimmune responses in NOD mice (17). Hence, PD-L1 may exhibit a protective role against β-cells exposed to islet inflammation. In humans, residual β-cells also exhibited higher PD-L1 expression in T1D patients compared with that in control subjects (14), which was different from the result of ICI-related T1D patients in the current study. The complete absence of PD-L1 expression on β-cells in the ICI-related T1D patients might be partly responsible for rapid β-cell destruction. In addition, despite the absence of PD-L1 expression also in α-cells in ICI-related T1D patients, α-cell volume was preserved. This may indicate that infiltrating macrophages and lymphocytes selectively target β-cells.
In the ICI-related T1D patients, both T lymphocytes, especially CD8-positive T lymphocytes, and macrophages infiltrated to and around islets. T lymphocytes predominantly infiltrated to and around islets rather than macrophages; however, this T-lymphocyte infiltration was also similarly observed in non-T1D patients. This reason is unknown, and more detailed studies will be needed to assess T-cell clonality and T-cell phenotype. On the other hand, the number of infiltrating macrophages was higher in the ICI-related T1D patients than in the non-T1D patients. Macrophage infiltration was reported to be associated with the development of T1D after administration of anti–PD-L1 or anti–PD-1 antibodies in a NOD mouse model (18,19), suggesting that macrophages might also play an important role in the development of ICI-related T1D in humans.
In the current study, we revealed the marked reduction of β-cell area and the increase of α-cell area in the ICI-related T1D patients. The degree of β-cell destruction in ICI-related T1D patients was similar to that in fulminant T1D patients (20). However, the increase of α-cell area has not been observed in established T1D patients (20,21). In addition to the pancreatic atrophy after ICI-related T1D onset (22), the unchanged Ki67-positive labeling index of α-cells (data not shown) suggests that the increase in α-cell area might be a relative increase rather than a true increase.
Furthermore, susceptible HLA may also have a significant impact on the development of ICI-related T1D. In this study, all three patients with ICI-related T1D had T1D-susceptible HLA (case 1: DRB1*04:05-DQB1*04:01 [23], case 2: DR4 [23], case 3: DRB1*09:01-DQB1*03:03 [23]) (Table 1). On the other hand, case 4 (non-T1D), who is still alive and has not developed T1D for >2 years, has one susceptible HLA (DRB1*09:01-DQB1*03:03 [23]) and one resistant HLA (DRB1*08:03-DQB1*06:01 [23]) (Supplementary Table 1). Resistant HLA is more dominant than susceptible factors (24). Therefore, having only susceptible HLA could elicit an immune response to β-cells.
There were some limitations in this study. First, this study included surgical cases and autopsy cases. Pancreatic tissues of autopsy cases may be less stained than those of surgical cases because of pancreatic autolysis due to the postmortem interval (25), and the results should be interpreted with caution. However, there was no clear difference in staining under these two conditions in this study.
Second, the effect of ICI on PD-L1 expression on islets needs to be carefully discussed because there was no comparison of the PD-L1 immunofluorescent intensity between pre- and postadministration of ICI in this study. However, our previous report showed that PD-L1 expression was strongly decreased in islets of NOD mice receiving ICI, while the expression was observed in islets of NOD mice not receiving ICI (19). This may support our hypothesis that ICI therapy itself could decrease PD-L1 expression levels on normal islet cells.
Finally, we could not analyze monoclonality of T-lymphocytes infiltrating into the pancreas in both ICI-related T1D patients and non-T1D patients. All of our samples were formalin fixed and paraffin blocked; therefore, all samples had fragmented RNA and low RNA yield. More detailed studies, including T-cell repertoire analysis, would be needed to assess T-lymphocyte clonality and phenotype.
In conclusion, we revealed the reduced expression of PD-L1 in pancreatic islets in response to ICI therapy, which is one of the novel findings of this study. In addition, the absence of PD-L1 expression on β-cells, infiltration of macrophages as well as T lymphocytes to and around the islets, and possession of T1D-susceptible HLA may lead to the development of ICI-related T1D.
Article Information
Acknowledgments. The authors thank Misako Kobayashi, Department of Metabolic Medicine, Graduate School of Medicine, Osaka University, for her excellent technical assistance. The authors would like to thank the timely help given by Ryotaro Saita, Data Coordinating Center, Department of Medical Innovation, Graduate School of Medicine, Osaka University Hospital, for data analysis.
Funding. This study was supported in part by a Grant-in-Aid from the Japan Society for the Promotion of Science (grant number T19K180070).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. S.K. researched the data and wrote the manuscript. J.K., S.Y., and Y.F. contributed to the discussion and reviewed and edited the manuscript. R.K.-T. researched the data of α-cell area. T.K., Y.H., and M.Y.B. contributed to the discussion. S.U. and R.U. provided the dissected pancreatic tissues of case 2. K.N. provided the dissected pancreatic tissues of case 1. Y.K. and M.U. contributed to immunohistochemistry of PD-L1 staining. Y.T. and H.E. provided the resected pancreatic tissues of case 3, case 4, and the control subjects. H.H., S.N., and E.M. provided the dissected pancreatic tissues of case 6. A.I. contributed to the discussion and provided the dissected pancreatic tissues of case 5. I.S. contributed to the discussion and reviewed the manuscript. J.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 65th Annual Meeting of the Japan Diabetes Society, Kobe, Japan, 12–14 May 2022.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21913008.
References
- 1. Fife BT, Bluestone JA. Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol Rev 2008;224:166–182 [DOI] [PubMed] [Google Scholar]
- 2. Parry RV, Chemnitz JM, Frauwirth KA, et al. CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Mol Cell Biol 2005;25:9543–9553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Martins F, Sofiya L, Sykiotis GP, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol 2019;16:563–580 [DOI] [PubMed] [Google Scholar]
- 5. Baden MY, Imagawa A, Abiru N, et al.; consultation of the Japan Diabetes Society Committee on Type 1 Diabetes Mellitus Research . Characteristics and clinical course of type 1 diabetes mellitus related to anti-programmed cell death-1 therapy. Diabetol Int 2018;10:58–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Filette JMK, Pen JJ, Decoster L, et al. Immune checkpoint inhibitors and type 1 diabetes mellitus: a case report and systematic review. Eur J Endocrinol 2019;181:363–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yoneda S, Imagawa A, Hosokawa Y, et al. T-lymphocyte infiltration to islets in the pancreas of a patient who developed type 1 diabetes after administration of immune checkpoint inhibitors. Diabetes Care 2019;42:e116–e118 [DOI] [PubMed] [Google Scholar]
- 8. Sawai T, Hosokawa T, Shigekiyo T, Ogawa S, Sano E, Arawaka S. An autopsy case of nivolumab-induced myasthenia gravis and myositis. Rinsho Shinkeigaku 2019;59:360–364 [in Japanese] [DOI] [PubMed] [Google Scholar]
- 9. Fujita Y, Kozawa J, Iwahashi H, et al. Human pancreatic α- to β-cell area ratio increases after type 2 diabetes onset. J Diabetes Investig 2018;9:1270–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003;52:102–110 [DOI] [PubMed] [Google Scholar]
- 11. Campbell-Thompson ML, Atkinson MA, Butler AE, et al. The diagnosis of insulitis in human type 1 diabetes. Diabetologia 2013;56:2541–2543 [DOI] [PubMed] [Google Scholar]
- 12. Foulis AK, Liddle CN, Farquharson MA, Richmond JA, Weir RS. The histopathology of the pancreas in type 1 (insulin-dependent) diabetes mellitus: a 25-year review of deaths in patients under 20 years of age in the United Kingdom. Diabetologia 1986;29:267–274 [DOI] [PubMed] [Google Scholar]
- 13. Mukaida S, Adachi J, Otsubo N, et al. An autopsy report of fulminant type 1 diabetes mellitus that developed during anti-programmed cell death-1 treatment. J Jpn Diabetes Soc 2020;63:711–716 [in Japanese] [Google Scholar]
- 14. Colli ML, Hill JLE, Marroquí L, et al. PDL1 is expressed in the islets of people with type 1 diabetes and is up-regulated by interferons-α and-γ via IRF1 induction. EBioMedicine 2018;36:367–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ansari MJ, Salama AD, Chitnis T, et al. The programmed death-1 (PD-1) pathway regulates autoimmune diabetes in nonobese diabetic (NOD) mice. J Exp Med 2003;198:63–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keir ME, Liang SC, Guleria I, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med 2006;203:883–895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rui J, Deng S, Arazi A, Perdigoto AL, Liu Z, Herold KC. β cells that resist immunological attack develop during progression of autoimmune diabetes in NOD mice. Cell Metab 2017;25:727–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hu H, Zakharov PN, Peterson OJ, Unanue ER. Cytocidal macrophages in symbiosis with CD4 and CD8 T cells cause acute diabetes following checkpoint blockade of PD-1 in NOD mice. Proc Natl Acad Sci U S A 2020;117:31319–31330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kawada-Horitani E, Kita S, Okita T, et al. Human adipose-derived mesenchymal stem cells prevent type 1 diabetes induced by immune checkpoint blockade. Diabetologia 2022;65:1185–1197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sayama K, Imagawa A, Okita K, et al. Pancreatic beta and alpha cells are both decreased in patients with fulminant type 1 diabetes: a morphometrical assessment. Diabetologia 2005;48:1560–1564 [DOI] [PubMed] [Google Scholar]
- 21. Butler AE, Galasso R, Meier JJ, Basu R, Rizza RA, Butler PC. Modestly increased beta cell apoptosis but no increased beta cell replication in recent-onset type 1 diabetic patients who died of diabetic ketoacidosis. Diabetologia 2007;50:2323–2331 [DOI] [PubMed] [Google Scholar]
- 22. Marchand L, Thivolet A, Saintigny P, Fabien N, Vouillarmet J, Thivolet C. Anti-programmed death 1 (PD-1) antibodies and the pancreas: a diabetic storm ahead? Diabetes Care 2018;41:638–639 [DOI] [PubMed] [Google Scholar]
- 23. Tsutsumi C, Imagawa A, Ikegami H, Makino H, Kobayashi T; Japan Diabetes Society Committee on Type 1 Diabetes Mellitus Research . Class II HLA genotype in fulminant type 1 diabetes: a nationwide survey with reference to glutamic acid decarboxylase antibodies. J Diabetes Investig 2012;3:62–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ikegami H, Ogihara T. Genetics of insulin-dependent diabetes mellitus. Endocr J 1996;43:605–613 [DOI] [PubMed] [Google Scholar]
- 25. Shimizu M, Hayashi T, Saitoh Y, Ohta K, Itoh H. Postmortem autolysis in the pancreas: multivariate statistical study. The influence of clinicopathological conditions. Pancreas 1990;5:91–94 [DOI] [PubMed] [Google Scholar]