Abstract
This article describes the implementation of an equity-focused strategy to increase the uptake of COVID-19 vaccination among communities of color and in traditionally underserved geographic areas using mobile health clinics (MHCs). The MHC Vaccination Program was implemented through a large integrated healthcare system in North Carolina using a grassroots development and engagement strategy along with a robust model for data-informed decision support to prioritize vulnerable communities. Several valuable lessons from this work can replicated for future outreach initiatives and community-based programming:
•Health systems can no longer operate under the assumption that community members will come to them, particularly those experiencing compounding social and economic challenges. The MHC model had to be a proactive outreach to community members, rather than a responsive delivery mechanism.
•Barriers to access included financial, legal, and logistical challenges, in addition to mistrust among historically underserved and marginalized communities.
•A MHC model can be adaptable and responsive to data-informed decision-making approaches for targeted service delivery.
•A MHC model is not a one-dimensional solution to access, but part of a broader strategy to create diverse points of entry into the healthcare system that fall within the rhythm of life of community members.
Keywords: Health equity, Mobile healthcare, COVID-19, Vaccination, Community partnerships
1. Background
As of February 20, 2023, the U.S. reported 102,998,014 cases and 1,113,254 deaths from the novel coronavirus disease 2019 (COVID-19), a condition caused by infection from the SARS-CoV-2 virus.1 Higher rates of COVID-19 cases, severe disease, and mortality have been widely documented among racial and ethnic minority populations,2 , 3 along with compounding social and economic inequities that contribute to a higher risk of SARS-CoV-2 exposure and disease complications.4 , 5 Nonpharmaceutical interventions to mitigate viral transmission and prevent disease spread (e.g., social distancing, mask-wearing, and shelter-in-place policies) were inconsistently deployed,6 , 7 necessitating a global immunization strategy through vaccinations.
To address COVID-19 health equity, experts recommended a place-based approach focused on the hardest hit communities and delivered in partnership with trusted local stakeholders.8 , 9 Health systems have successfully leveraged Mobile health clinics (MHCs) to target COVID-19 vaccine delivery.10 , 11 Mobile approaches offer many advantages for care delivery including the ability to rapidly deploy and tailor services in response to community needs and data-informed decision making12, 13, 14 Atrium Health, a large integrated healthcare system with a mission to “improve health, elevate hope, and advance healing – for ALL”, leveraged MHCs as part of an equity-focused strategy for COVID-19 vaccination. The purpose of this report is to describe the population served by Atrium Health through the MHC Vaccination Program by race/ethnicity and geographic social vulnerability, and discuss the implications of MHC strategies for improving equitable access to healthcare services beyond the COVID-19 pandemic response.
2. Organizational context
Atrium Health is the largest integrated, nonprofit healthcare system in the southeast with more 42 hospitals and 1,500 care locations that support over 10 million patient interactions annually. Our headquarter community in Mecklenburg County, North Carolina has remained one of hardest hit regions in the state throughout the pandemic.15 Structural inequity is an ongoing challenge in Mecklenburg County. A widely-cited study by Chetty and colleagues (2014) ranked Charlotte (the largest city in Mecklenburg County) last among America's 50 largest cities in upward economic mobility, highlighting a cycle of inter-generational poverty, poor educational attainment, and health disparities that disproportionately impact the community's residents of color.16 A majority of social and health risk factors are concentrated in six ZIP codes, identified by the local health department as Public Health Priority Areas (PHPAs).17
3. Problem
Given the disproportionate burden of disease, communities of color and low-income populations were prioritized for vaccine deployment. Despite these efforts, early data from initial vaccine rollout indicated that Black (12.4% population vs. 8.9% vaccinated) and Latinx (17.2% population vs. 13.3% vaccinated) populations were being vaccinated at lower rates than their White counterparts (61.2% population vs. 62.5% vaccinated),18 and communities with high social vulnerability were being disproportionately underserved.19 Disparate uptake of the COVID-19 vaccine was influenced by a combination of barriers to access, along with cultural distrust stemming from a history of discrimination and unequal treatment by the medical system.20 Despite these complexities, experts warned that inequitable uptake of vaccination inhibited progress towards herd immunity, increased community vulnerability to dangerous disease variants, and contributed to long-standing social and health inequities experienced by historically underserved and marginalized populations.21 , 22 As of May 13, 2021, local outlets in Mecklenburg County reported a 40 percentage-point gap (approximately 20% vs. 60%) between PHPAs and the larger county in the rate of vaccination among eligible adults.23 As the largest provider of healthcare in Mecklenburg and surrounding counties, Atrium Health was focused on promoting COVID-19 vaccination equity.
4. Solution
In February 2021, Atrium Health launched the MHC Vaccination Program with a mission to improve access to healthcare and increase the uptake of COVID-19 vaccination among communities of color and in traditionally underserved geographic areas. The MHC model was developed using a grassroots engagement strategy with trusted community leaders, along with a robust infrastructure for data-informed decision support. In addition to COVID-19 vaccinations, MHCs provided access to care and resources for health and social service needs. Community members were screened for basic health vitals (i.e., blood pressure, temperature, pulse, etc.) and social determinants of health risks including food and housing insecurity. A social worker and advanced practice provider were on site to address identified needs through referrals and follow-up appointments. All community members were served, regardless of prior engagement with Atrium Health.
Locations for MHC sites were strategically chosen using two methods of data-informed decision-making. First, real-time patient data (COVID-19 diagnosis by residential address) were visualized using geographic information systems (GIS) technology to identify areas with high rates of transmission using a hotspot analysis. Communities with the highest rates of transmission were prioritized for MHC deployment. Second, publicly available data were obtained through the North Carolina Department of Health and Human Services, COVID-19 Vaccine Management System dashboard as the aggregate rates of vaccination by race and ethnicity and county. These data were used to calculate a metric of vaccine disparity as the percentage point difference between a demographic group among those vaccinated in a county and the representation of that group within the county as:
where % Vaccinated is the percent of demographic group a among county i residents vaccinated through any system or provider, and % County is the percent of demographic group a among county i residents. Counties with high vaccine disparity were also prioritized for MHC Deployment.
The MHC Vaccination Program was deployed up to 4 days per week, generally between the hours of 8am to 4pm with up to 5 unique sites per day. Hours varied based in response to stakeholder feedback and partner collaboration. At the height of demand, the MHCs were able vaccinate approximately 500 community members per day. However, the model could also scale down to serve just 10 people and allowed for efficient expansion into adjacent rural communities with smaller population densities. The model was designed to eliminate common barriers to access and uptake, with ongoing iterative process improvement to adapt as information and community needs changed over time. Health services were available without an appointment or referral and did not require any proof of insurance or verification of citizenship status. All services were free to uninsured community members. A targeted advertising and communication strategy was specifically developed to highlight the “easy entry” of our MHC model, and disseminated through various media channels (e.g., internet, radio, newspaper) along with leveraging word-of-mouth endorsement and communication channels from trusted community stakeholders. Special considerations were also made to ensure that our model was inclusive for the local Hispanic community. All advertising and program information was available in Spanish, including a specialized information and education campaign, “Para Tu Salud” – simply translated to “For Your Health”.24 All MCU events included bilingual staff members to facilitate communication and connection, and all marketing specifically highlighted that immigration status will never be asked, shared, or reported to any government entity.
4.1. Data
A retrospective, cross-sectional analysis was conducted. Patients served on MHCs and all other care access points completed self-report enrollment at the time of registration for vaccination that was entered into the electronic medical record (EMR), including discrete race and ethnicity variables using pre-defined, standardized categories. Data for the analysis were obtained from Atrium Health's Enterprise Data Warehouse. Data were extracted for all patients who received a single dose of vaccines requiring one (Johnson & Johnson) or two shots (Moderna and Pfizer) to complete their primary series between January 1, 2021 and October 4, 2021. Publicly available data were obtained from the Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry website as the 2018 social vulnerability index estimates by census tract.25
4.2. Measures
Vaccinated was defined as completed a single dose of vaccines requiring one (Johnson & Johnson) or two shots (Moderna and Pfizer) to complete their primary series.
Social Vulnerability was measured using the Centers for Disease Control and Prevention's social vulnerability index (SVI).26 The SVI uses 15 U.S. census variables including poverty, lack of vehicle access, and crowded housing to help emergency response planners identify and map communities that will most likely need extra support during emergency events. Studies have shown that the SVI is associated with COVID-19 outbreaks.27, 28, 29
Race/Ethnicity was calculated using pre-determined categories for race and ethnicity available through the EMRs as a combined variable. Patients reporting Hispanic/Latino were classified as Latinx in the combined variable, while all other patients using the race variable as Non-Latinx Black, White, Asian, or Other.
Access Type was dichotomized into MHC and non-mobile location types. MHC locations represent all community sites participating in the program, and non-mobile locations comprised all other access types including ambulatory care.
4.3. Analysis
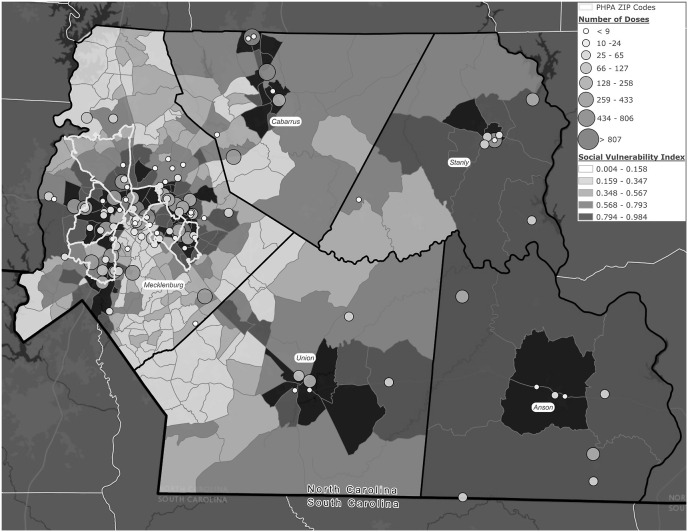
Descriptive analysis was used to assess the equitable distribution of vaccinations among communities of color and priority geographic areas. The proportion of race/ethnicity among those vaccinated through Atrium Health was calculated by access type and visualized over time. Geographic SVI was visualized by census tract using a choropleth map, with an overlay of rings (centroids located at vaccination sites) visualizing the total counts of community members vaccinated by Atrium Health through the MHC Vaccination Program. Map visualization was created using ArcGIS Pro® software by Esri (version 2.8.3).30 The analysis protocol was approved by Atrium Health Institutional Review Board (IRB) as a quality improvement effort that was exempt from human subjects’ oversight by the IRB and did not require participant consent.
5. Results
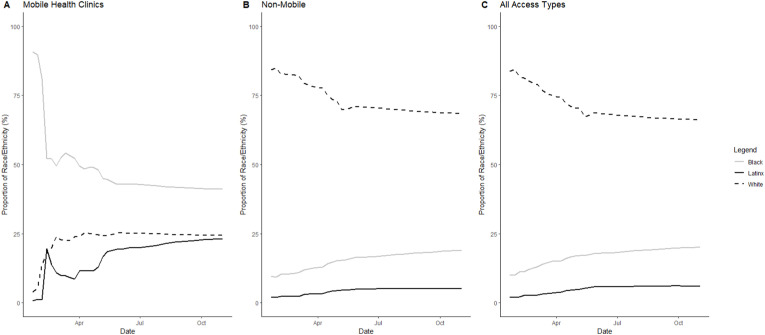
As of October 4, 2021, MHCs provided 15,459 first- or single-dose vaccinations in Mecklenburg and surrounding counties. A majority (63%) of patients vaccinated through MHCs were Black or Latinx. Compared to other Non-Mobile access types, MHCs vaccinated a larger proportion of Black (43% vs. 18%) and Latinx (20% vs. 5%) patients and a smaller proportion of White (24% vs. 67%) patients. Furthermore, a larger proportion of vaccines delivered to communities of color occurred through MHCS (approximately 11% of vaccinations delivered to Black patients and 20% of vaccines delivered to Latinx patients) compared to 2% of vaccines delivered to White patients (Table 1 ). When examining the cumulative total of vaccinations over time by access type, the disproportionate uptake through MHCs remained relatively stable among Black patients, and increased among Hispanic patients (Fig. 1 ).
Table 1.
Race and ethnic demographics of vaccinated population by access type.
| Access Type |
All Types# (%) | ||
|---|---|---|---|
| Mobile Health Clinic# (%) | Non-Mobile# (%) | ||
| Black | 6,286 (43.0) | 50,830 (18.0) | 57,116 (19.3) |
| White | 3,735 (23.9) | 186,703 (66.9) | 190,438 (64.7) |
| Latinx | 3,494 (20.0) | 14,159 (4.9) | 17,653 (5.7) |
| Asian | 1,207 (8.3) | 14,689 (5.3) | 15,896 (5.4) |
| Other | 522 (3.5) | 5,609 (1.9) | 6,131 (2.0) |
| Not Specified | 215 (1.3) | 8,648 (3.0) | 8,863 (2.9) |
| Total | 15,459 (100) | 280,638 (100) | 296,097 (100) |
Note: Vaccinated is defined as completed single dose of vaccines requiring one (Johnson & Johnson) or two shots (Moderna and Pfizer) to complete their primary series as of 10/4/2021.
Data Source: Atrium Health electronic medical records.
Fig. 1.
Proportion of race/ethnicity demographics among atrium health patients vaccinated over time by (A) mobile health clinic (B) non-mobile (C) all access types.
Source/Notes: SOURCE Atrium Health electronic medical records. NOTES Vaccinated is defined as completed single dose of vaccines requiring one (Johnson & Johnson) or two shots (Moderna and Pfizer) to complete their primary series as of 10/4/2021.
The MHC Vaccination Program was deployed with a goal of prioritizing communities with the greatest disparity of uptake among communities of color and greatest social vulnerability. The cumulative total of persons vaccinated through the MHCs is visualized in Fig. 2 by event location, along with the social vulnerability by census tract. Results demonstrated that MHC vaccinations were clustered in counties with a high social-vulnerability index. In Mecklenburg County, a notable cluster of vaccinations occurred in PHPAs.
Fig. 2.
Social vulnerability and vaccinations through mobile health clinics.
Source/Notes: SOURCE Atrium Health electronic medical records, Centers for Disease Control and Prevention 2018 social vulnerability index estimates by census tract.26 NOTES Vaccinated is defined as completed single dose of vaccines requiring one (Johnson & Johnson) or two shots (Moderna and Pfizer) to complete their primary series as of 10/4/2021, Social Vulnerability is calculated as a percentile ranking of vulnerability ranging from 0 to 1, with higher values indicating greater vulnerability.
6. Unrespoved questions and lessons from the field
The Atrium Health MHC Vaccination Program was designed to improve access to healthcare and increase the uptake of COVID-19 vaccination among communities of color and in traditionally underserved geographic areas. This strategy is consistent with evidence showing that residents of communities with robust primary care infrastructure and low exposure to social vulnerability have a reduced risk of COVID-19 infection and mortality.31 Results from our descriptive analysis showed that the MHC Vaccination Program successfully prioritized counties and census tracts with inequitable vaccination uptake among communities of color, and high exposure to social risk factors. In addition, patients served through the MHC units were disproportionately Black (43%, n = 6,286) and Latinx (20%, 3,494) compared to the non-mobile care models (18% and 5%, respectively). Results should be interpreted with regards to data limitations and a dynamic policy environment. Self-report race/ethnicity is subject to missingness that can be disproportionately greater among Latinx and other communities of color.
These results are consistent with other reports demonstrating the efficacy of MHCs in reaching communities of color. Prior to vaccine availability, Atrium Health mobilized a COVID-19 testing program using MHCs. Results from a recently published evaluation showed that a majority of patients served were communities of color (46% Latinx and 22% Black).32 A mobile COVID-19 vaccination community clinic through Loma Linda University in San Bernardio, California reported serving an 84% Black (n = 351) population,33 while another grass-roots driven effort through community coalitions in the Boston metropolitan area reported serving a 57% Hispanic (n = 2,745) population.34 Another strategy used MHCs to improve adherence to routine childhood vaccination schedules during the COVID-19 pandemic, with a Boston-area pilot serving a 77% Black (n = 40) and 21% Hispanic (n = 11) population.35
The MHC outreach team learned many valuable lessons that can be replicated for future outreach initiatives and community-based programming. First, “we can't wait for them to come to us, we have to go to them”, meaning we can't expect community members without a relationship with the healthcare system to establish one through traditional channels. The MHC model had to be a proactive outreach to community members, rather than a responsive delivery mechanism. Second, convenient access had to remove financial, legal, and logistical barriers. In addition to geographic proximity through location directly in historically underserved communities, MHC sites were the only access point for COVID-19 vaccination that did not require an appointment, doctor's referral, or presentation of insurance at the time of care. Third, service delivery was not a “one and done’ approach and serving traditionally underserved community members was an opportunity to build trust and establish an ongoing relationship. The MHC model was designed to offer wrap-around services including health and social risk screenings. Staffing included social workers and advanced practice providers to address identified needs through referrals and follow-up appointments.
While many have praised the moral value of MHCs as the “right thing to do”, the effectiveness and sustainability of this model offers an equally compelling argument for health system leaders and policy makers. Evidence has demonstrated that MHC programs have the potential to reduce costs and improve health outcomes.36 One study estimated a return-on-investment ratio of 1.3 that was associated with improved management of chronic disease and reduced emergency department utilization.37 Compared to traditional brick-and-mortar clinics, MHCs are rapidly adaptable to changes in community needs in addition to neighborhood transition and healthcare gentrification, both of which are known to exacerbate health equity gaps.38 The adaptability of MHCs also allows for data-informed decision-making approaches to targeted service delivery. Health systems can partner with local health departments, using internal EMR data along with public surveillance data to identify and respond to emergent and preventive health needs. For example, MHCs were deployed in Flint, Michigan as a response to lead contamination in the city's drinking water supply. Areas with the greatest need were identified using a spatial analysis,39 and the MHC program offered screening for lead poisoning and developmental issues along with comprehensive primary care.40
As the U.S. healthcare system moves towards value-based care, delivery models are shifting focus to increase accessibility and improve health outcomes among communities that have been historically disenfranchised from traditional healthcare.41 MHCs are not a one-dimensional solution to access, but part of a broader strategy to create diverse points of entry into the healthcare system that fall within the rhythm of life of community members. Experts highlight that MHC models can successfully reach “hard to reach” community members and, in addition to direct service delivery, can operate as connector to the larger healthcare and social service systems.42 Results from our evaluation of Atrium Health's MHC COVID-19 testing program showed that patients who were uninsured, and not connected to a primary medical home were more likely to be tested through a MHC than through any other access point (i.e., emergency or ambulatory care).32 It is important note that MHCs may not be the right fit for all populations. Other non-traditional methods, including telemedicine, portable clinics, and street medicine, may be more appropriate for younger populations and those experiencing homelessness.43 , 44
The COVID-19 pandemic has been a catalyst for innovation in healthcare service delivery, with many calling for a permanent adoption of successful strategies like MHCs.45 Health systems and independent providers can no longer operate under the assumption that community members will come to them, particularly those experiencing compounding social and economic challenges. More evidence is needed to demonstrate return on investment, reimbursement and payment models, along with implementation strategies for large-scale adoption of new models. Atrium Health has committed to a MHC strategy and will be transitioning our MHC Vaccination Program into a MHC Primary Care program. MHCs will be equipped like a brick-and-mortar physician practice to provide basic acute and primary care services for adults and children, including patient education, diagnosis and treatment of acute and chronic illnesses, and recommended vaccinations and screenings. While a patient may first engage with care through the MHC, additional wrap-around services will be provided, including connection to a primary care medical home and enrollment with a community health worker for ongoing support with accessing community and health system resources.
7. Conclusions
The Atrium Health MHC Vaccination Program successfully increased access to COVID-19 vaccination and care among historically underserved communities. MHCs address common barriers to healthcare access and support an effective and sustainable model of care delivery for “hard to reach” populations. Health systems can leverage MHCs to advance health equity as part of a broad strategy to expand points of entry into the health system.
Financial disclosure
The authors have indicated they have no financial relationships to disclose.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human participant compliance statement
The analysis protocol was approved by Atrium Health Institutional Review Board (IRB) as a quality improvement effort that was exempt from human subjects’ oversight by the IRB and did not require participant consent.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
A number of people have made significant contributions to success of Atrium Health's COVID-19 vaccination response and our mobile-based strategy for health equity. We would like to acknowledge Dr. Kinneil Coltmen, Executive Vice President and Chief Community & Social Impact Officer; Dr. Garry Little, Chief Medical Officer; and Dr. Katie Passaretti, Enterprise Chief Epidemiologist for their transformational leadership during this challenging time, along with Saul Amezquita and Rita Dominguez for their leadership of the Para Tu Salud program. We would also like to express gratitude to other members of the numerous vaccine oversight committees and work groups for their tireless efforts and continuous support of our system's response strategy, in addition to the thousands of clinical teammates that worked on the front-lines to deliver vaccines through our mobile and non-mobile programs. Your sacrifices have saved lives and kept our community safe.
Data availability
The authors do not have permission to share data.
References
- 1.Centers for Disease Control and Prevention . 2023. COVID Data Tracker.https://covid.cdc.gov/covid-data-tracker/#datatracker-home Available from: Last accessed 02/20/2023. [Google Scholar]
- 2.Moore J.T., Ricaldi J.N., Rose C.E., et al. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020—22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020. Aug 21;69(33):1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mackey K., Ayers C.K., Kondo K.K., et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Dorn A., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karmakar M., Lantz P.M., Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021 Jan 4;4(1) doi: 10.1001/jamanetworkopen.2020.36462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adolph C., Amano K., Bang-Jensen B., et al. Pandemic politics: timing state-level social distancing responses to COVID-19. J Health Polit Policy Law. 2021;46(2):211–233. doi: 10.1215/03616878-8802162. [DOI] [PubMed] [Google Scholar]
- 7.Fischer C.B., Adrien N., Silguero J.J., et al. Mask adherence and rate of COVID-19 across the United States. PLoS One. 2021;16(4) doi: 10.1371/journal.pone.0249891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bibbins-Domingo K., Petersen M., Havlir D. Taking vaccine to where the virus is—equity and effectiveness in coronavirus vaccinations. JAMA. 2021;2(2):e210213. doi: 10.1001/jamahealthforum.2021.0213. e210213. [DOI] [PubMed] [Google Scholar]
- 9.Jean-Jacques M., Bauchner H. Vaccine distribution—equity left behind? JAMA. 2021;325(9):829–830. doi: 10.1001/jama.2021.1205. [DOI] [PubMed] [Google Scholar]
- 10.Alcendor D.J., Juarez P.D., Matthews-Juarez P., et al. Meharry Medical College mobile vaccination program: implications for increasing COVID-19 vaccine uptake among minority communities in middle Tennessee. Vaccines. 2022 Jan 29;10(2):211. doi: 10.3390/vaccines10020211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shukla S., Fressin F., Un M., Coetzer H., Chaguturu S.K. Optimizing vaccine distribution via mobile clinics: a case study on COVID-19 vaccine distribution to long-term care facilities. Vaccine. 2022 Jan 31;40(5):734–741. doi: 10.1016/j.vaccine.2021.12.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Attipoe-Dorcoo S., Delgado R., Gupta A., et al. Mobile health clinic model in the COVID-19 pandemic: lessons learned and opportunities for policy changes and innovation. Int J Equity Health. 2020;19(1):1–5. doi: 10.1186/s12939-020-01175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malone N.C., Williams M.M., Fawzi M.C., et al. Mobile health clinics in the United States. Int J Equity Health. 2020;19(1):1–9. doi: 10.1186/s12939-020-1135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mills M.C., Salisbury D. The challenges of distributing COVID-19 vaccinations. EClinicalMedicine. 2021:31. doi: 10.1016/j.eclinm.2020.100674. 100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.North Carolina Department of Health and Human Services . 2022. COVID-19 Vaccine Management System.https://covid19.ncdhhs.gov/vaccines/info-health-care-providers/covid-19-vaccine-management-system-cvms Available from: Last accessed 11/14/2021. [Google Scholar]
- 16.Chetty R., Hendren N., Kline P., et al. Where is the land of opportunity: the geography of intergenerational mobility in the United States. Q J Econ. 2014;129(4):1553–1623. [Google Scholar]
- 17.Cole A.J. Collaboration is critical: working together to optimize health in our communities. N C Med J. 2017;78(4):255–257. doi: 10.18043/ncm.78.4.255. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . 2022. Demographic Trends of COVID-19 Cases and Deaths in the US Reported to CDC.https://covid.cdc.gov/covid-data-tracker/#demographics Available from: Last accessed 05/15/2021. [Google Scholar]
- 19.Hughes M.M., Wang A., Grossman M.K., et al. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernández L., Shorett P. Lessons in equity from the front lines of COVID-19 vaccination. JAMA. 2021;2(4) doi: 10.1001/jamahealthforum.2021.0612. e210612. [DOI] [PubMed] [Google Scholar]
- 21.McClung N., Chamberland M., Kinlaw K., et al. The Advisory Committee on Immunization Practices' ethical principles for allocating initial supplies of COVID-19 vaccine—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(47):1782. doi: 10.15585/mmwr.mm6947e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salmon D., Opel D.J., Dudley M.Z., et al. Reflections on governance, communication, and equity: challenges and opportunities in COVID-19 vaccination. Health Aff. 2021;40(3):419–425. doi: 10.1377/hlthaff.2020.02254. [DOI] [PubMed] [Google Scholar]
- 23.A Neighborhood-By-Neighborhood Look at COVID Vaccination Rates Shows Large Disparities. The Charlotte Observer; 2021. https://www.charlotteobserver.com/news/coronavirus/article251242354.html#storylink=cpy Available from: Last accessed 11/11/2021. [Google Scholar]
- 24.Atrium Health . 2020. Atrium Health Increases Ongoing Commitment to Charlotte's Hispanic Community amid COVID-19.https://atriumhealth.org/about-us/newsroom/news/2020/05/atrium-health-increases-ongoing-commitment-to-charlottes-hispanic-community-amid-covid19 Available from: Last accessed 11/11/2021. [Google Scholar]
- 25.Centers for disease Control and prevention/agency for toxic Substances and disease registry/geospatial research, analysis, and services program. CDC/ATSDR social vulnerability index 2018 database North Carolina. 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html Available from. Last accessed 05/15/2021.
- 26.Centers for Disease Control and Prevention Agency for toxic Substances and disease Registry. CDC/ATSDR social vulnerability index. 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html Available from: Last accessed 05/15/2021.
- 27.Dasgupta S., Bowen V.B., Leidner A., et al. Association between social vulnerability and a county's risk for becoming a COVID-19 hotspot—United States, June 1–July 25, 2020. MMWR Morb Wkly Rep. 2020;69(42):1535. doi: 10.15585/mmwr.mm6942a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karaye I.M., Horney J.A. The impact of social vulnerability on COVID-19 in the US: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Biggs E.N., Maloney P.M., Rung A.L., et al. The relationship between social vulnerability and COVID-19 incidence among Louisiana census tracts. Front Public Health. 2021;8:1048. doi: 10.3389/fpubh.2020.617976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Environmental Systems Research Institute (ESRI) [Internet] ArcGIS Pro Release. 2021;2.8(3) Redlands, CA. [Google Scholar]
- 31.Jabbarpour Y., Jetty A., Westfall J.M., et al. 2021. Primary Care and COVID-19: It's Complicated. Primary Care Collaborative.https://www.pcpcc.org/sites/default/files/resources/PCC_Primary_Care_COVID-19_Its_Complicated.pdf Available from: Last accessed 11/11/2021. [Google Scholar]
- 32.Sparling A., Walls M., Mayfield C.A., et al. Racial/ethnic disparities in health care setting choice for adults seeking severe acute respiratory syndrome coronavirus 2 testing. Med Care. 2022;60(1):3–12. doi: 10.1097/mlr.0000000000001654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdul-Mutakabbir J.C., Casey S., Jews V., et al. A three-tiered approach to address barriers to COVID-19 vaccine delivery in the Black community. Lancet Global Health. 2021;9(6):e749–e750. doi: 10.1016/s2214-109x(21)00099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Velasquez D., Gondi S., Lu R., et al. GOTVax: a novel mobile covid-19 vaccine program. NEJM Catalyst Innovations in Care Delivery. 2021;2(3) [Google Scholar]
- 35.Leibowitz A., Livaditis L., Daftary G., et al. Using mobile clinics to deliver care to difficult-to-reach populations: a COVID-19 practice we should keep. Prev Med Rep. 2021;24 doi: 10.1016/j.pmedr.2021.101551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aung K.K., Hill C., Bennet J., et al. The emerging business models and value proposition of mobile health clinics. Am J Accountable Care. 2015;3(4):36–40. [PMC free article] [PubMed] [Google Scholar]
- 37.Song Z., Hill C., Bennet J., et al. Mobile clinic in Massachusetts associated with cost savings from lowering blood pressure and emergency department use. Health Aff. 2013;32(1):36–44. doi: 10.1377/hlthaff.2011.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cole H.V., Mehdipanah R., Gullón P., et al. Breaking down and building up: gentrification, its drivers, and urban health inequality. Curr Environ Health Rep. 2021;8(2):157–166. doi: 10.1007/s40572-021-00309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanna-Attisha M., LaChance J., Sadler R.C., et al. Elevated blood lead levels in children associated with the Flint drinking water crisis: a spatial analysis of risk and public health response. Am J Publ Health. 2016;106(2):283–290. doi: 10.2105/AJPH.2015.303003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allen R. Detroit Free Press; 2016. Mobile Doctor's Office Arrives in Flint from NYC.http://www.freep.com/story/news/local/michigan/flint-water-crisis/2016/02/12/mobile-doctors-office-arrives-flint-nyc/80302086/ Available from: Last accessed 05/17/2022. [Google Scholar]
- 41.Yu S.W., Hill C., Ricks M.L., et al. The scope and impact of mobile health clinics in the United States: a literature review. Int J Equity Health. 2017;16(1):1–2. doi: 10.1186/s12939-017-0671-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malone N.C., Williams M.M., Smith Fawzi M.C., et al. Mobile health clinics in the United States. Int J Equity Health. 2020;19(1):1–9. doi: 10.1186/s12939-020-1135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bashshur R., Doarn C.R., Frenk J.M., et al. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J e Health. 2020;26(5):571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 44.Feldman B.J., Kim J.S., Mosqueda L., et al. From the hospital to the streets: bringing care to the unsheltered homeless in Los Angeles. Healthc (Amst) 2021;9(3) doi: 10.1016/j.hjdsi.2021.100557. [DOI] [PubMed] [Google Scholar]
- 45.Leibowitz A., Livaditis L., Daftary G., et al. Using mobile clinics to deliver care to difficult-to-reach populations: a COVID-19 practice we should keep. Prev Med Rep. 2021;24 doi: 10.1016/j.pmedr.2021.101551. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.