Abstract
Yoga, a physical and contemplative practice, offers the practitioner a unique mind-body exercise experience demonstrating preliminary efficacy in improving cognitive health. We examine the evidence for underlying mechanisms that explain the yoga-cognition relationship in healthy older adults. The cognitive benefits of yoga may be the result of improved stress regulation and neurocognitive resource efficiency that facilitate bi-directional brain-body communication.
Keywords: Yoga, Brain, Default Mode Network, Aging, Cognitive Decline, Cortisol, Functional Connectivity
Summary for table of contents:
Yoga may improve cognition in older adults as the result of improved stress regulation and neurocognitive resource efficiency.
INTRODUCTION
Yoga’s origins date back more than 2000 years to ancient India. The original term yug means ‘to unite’ and it signifies the harmony or unification of the mind, body and spirit. Yoga is often depicted metaphorically as a tree and comprises eight branches: yama (universal ethics), niyama (individual ethics), asana (physical postures), pranayama (breathwork), pratyahara (control of the senses), dharana (concentration), dyana (meditation), and samadhi (bliss) and is considered a way of life. Over the course of its existence and spread across the globe, the practice of yoga has largely evolved to a combination of three of the eight branches: physical postures, breathwork, and meditation, which fall under the umbrella of Hatha yoga, the most popular form of practice. Styles of yoga vary greatly in their emphasis on each of the eight branches of yoga, therefore, for the purpose of this review, we only include yoga studies that incorporate these three elements.
The active attentional component of yoga may incur cognitive benefits over and above the habitual bodily movements involved in traditional forms of exercise. A mindful movement practice, yoga enables the practitioner to move slowly and safely into physical postures while concentrating on relaxing the body, breathing fully, and developing awareness of bodily sensations and passing thoughts. Additionally, breathing and meditation exercises are practiced to calm and focus the mind, and develop greater self-awareness. This focused effort and attentional practice of yoga appears to mimic the conventionally assessed cognitive functions including attention, memory, and higher-order executive functions.
With a rising proportion of older and elderly adults in the populations of developed countries (1), there is a growing interest in identifying interventions that may improve brain health and ameliorate the effects of age-related cognitive decline in healthy adults. We published the first meta-analysis examining the acute and chronic effects of yoga on cognition (2). A significant moderate effect of yoga on cognition (g=0.33) was observed for randomized controlled trials, with the strongest effect for attention and processing speed (g=0.29), followed by executive function (g=0.27) and memory (g=0.18). Acute studies also demonstrated a significant overall effect of yoga on cognition (g=0.56). The effect was strongest for memory (g=0.78), followed by attention and processing speed (g=0.49) measures and executive functions (g=0.39). These studies compared yoga, primarily Hatha yoga, against a variety of conditions ranging from breath awareness, music, stretching and strengthening, aerobic exercise and waitlist control among healthy adult populations. While collectively yoga practice was associated with moderate improvements in cognitive function, none of these studies examined the possible mechanisms underlying the yoga-cognition relationship.
This review proposes two primary mechanisms contributing to the cognitive benefits of yoga: improved stress regulation and improved neurocognitive resource efficiency. While the benefits of yoga for stress and stress-related physical and mental health, mood, and psychological functioning have received extensive attention in recent reviews (3–6); this review specifically reviews the mechanisms underlying the relationship between yoga and cognitive health in older adults. Our first mechanism highlights the role of improved stress regulation potentially underlying the yoga-cognition relationship and our second mechanism hypothesizes that improvements in cognition (2) and brain structure and function (7) in response to yoga practice are the result of improved neurocognitive resource efficiency (Figure 1).
Figure 1: Cognitive Benefits of Yoga: Potential Neurocognitive and Stress-Regulating Mechanisms.
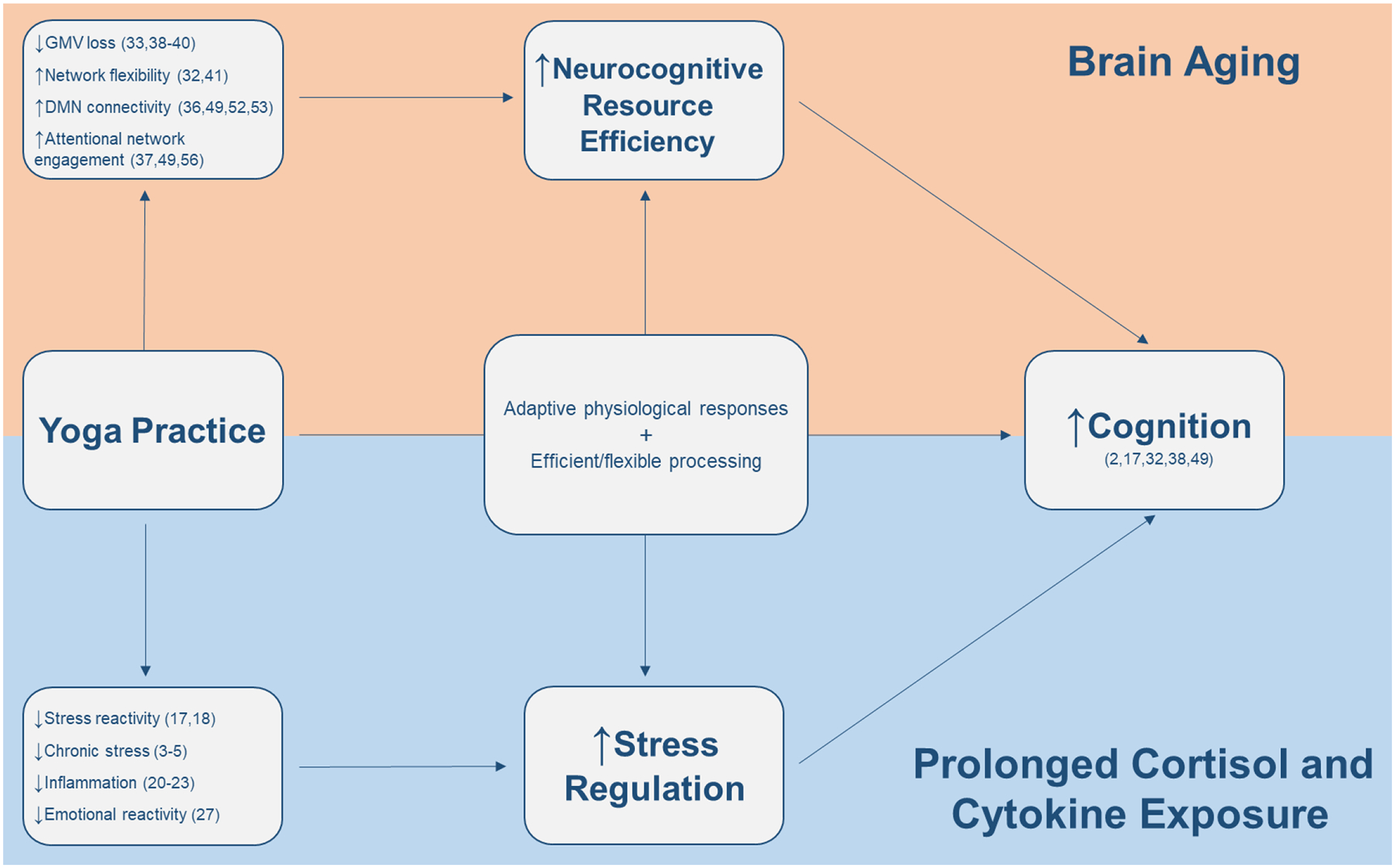
Cognitive deficits occur in the context of age-related cognitive decline (1) and prolonged cortisol and cytokine exposure (8,11). Yoga practice may improve stress regulation and neurocognitive resource efficiency, providing the practitioner with more adaptive physiological responses to stressors along with more efficient and automatic cognitive processing. Improved stress regulation may blunt the deleterious effects of prolonged cortisol exposure associated with chronic stress; and improved neurocognitive resource efficiency may provide neuroprotective benefits to limit age-related cognitive decline. A mindful movement practice, yoga facilitates the integration of top-down neurocognitive and bottom-up physiological processes by combining physical postures with meditation and breathing techniques. GMV; gray matter volume; DMN; Default mode network.
MECHANISMS
Stress Regulation
Interventions, such as yoga, that improve stress regulation and limit inflammation may provide neuroprotective cognitive benefits to older adults by limiting prolonged exposure to elevated cortisol and IL-6 levels. Longitudinal data link chronically elevated cortisol levels (measured over a 30-day period, yearly for 5 years) to hippocampal atrophy and memory deficits in older adults (8). Additionally, elevated cortisol is associated with increased risk for cognitive decline and Alzheimer’s Disease (AD) (9) and IL-6 levels are well known to increase with advancing age (10) and are associated with increased risk for cognitive decline in older adults (11).
Improved stress regulation may be particularly beneficial for preserving cognitive function in older adults, as the aging brain is more vulnerable to prolonged cortisol and cytokine exposure (11–13). Stress-reduction and relaxation are popular reasons for engaging in yoga practice (14), however the physiological effects of yoga on the stress response may be more complex than simply reducing stress. Rather, yoga may improve stress regulation by providing practitioners with the self-regulatory tools to tolerate stressful experiences “off the mat,” balancing homeostatic mechanisms and reducing allostatic load via the integration of bottom-up physiological mechanisms and top-down cognitive control (for a review on self-regulatory mechanisms, see Gard et al. 2014 (15)). While the precise mechanisms underlying the yoga-stress-cognition relationship remain to be elucidated, we hypothesize that improved stress regulation likely contributes to the cognitive benefits of yoga.
Stress Reactivity
Measures of stress reactivity are particularly useful to yoga researchers in determining how individuals respond to stressful stimuli experienced in daily life. For the purpose of this review, we define stress reactivity as the psychophysiological changes in response to an acute stressor as measured by changes in hypothalamic-pituitary-adrenal (HPA) axis activity, affect and inflammatory response. Sympathetic activation is an important component of stress reactivity however, while the yoga literature demonstrates beneficial effects on markers such as heart rate and blood pressure (3–5), little work has been done to examine the relationship between yoga, markers of sympathetic activation, and cognition. We include affective changes within the concept of stress reactivity as the emotional state is an important filter regulating the impact of stress on cognition (13) and emotionally-laden information is known to impair cognitive processing (16).
To our knowledge, a single study to date specifically examines the yoga-stress-cognition relationship, demonstrating that attenuated stress reactivity predicts improved executive functioning in older adults in response to a yoga intervention (17). A group of sedentary older adults participated in an 8-week Hatha yoga intervention and demonstrated improved performance on the running span task, n-back working memory and task-switching paradigm post-intervention when compared to stretching controls. Attenuated cortisol in response to a mild cognitive stressor and self-reported stress and anxiety levels predicted improvements in executive functioning in the yoga group, whereas elevated cortisol responses in the control group predicted poorer performance on the cognitive tasks. Notably, there were no differences in pre-stressor cortisol levels, suggesting that an 8-week intervention was insufficient to produce significant changes in basal stress markers. However, these findings demonstrate that short-term practice appears to be sufficient to reduce stress reactivity and improve affect, suggesting that yoga may provide neurocognitive benefits to older adult practitioners via a more adaptive response to acute cognitive stressors. Yoga practice encourages detachment from negative thoughts and emotions during physical postures. Therefore, it is plausible that yoga provided these individuals with the psychosocial resources to selectively disengage from negative, stress-induced cognitive processing to concentrate on the cognitive demands of the task, associated with decreased HPA axis activity.
Immunological findings also support the premise that yoga improves stress reactivity (18). Yoga practitioners with a minimum of 2 years of regular yoga practice and novices, each participated in a single session of restorative Hatha yoga and two control conditions on three separate visits. A single yoga session improved positive affect in both, yoga practitioners and controls, but no inflammatory or endocrine responses were unique to a single yoga session. However, compared to novices, yoga practitioners demonstrated lower heart rate during a mild cognitive stressor and produced less lipopolysaccharide stimulated IL-6 in response to the stressor, indicative of decreased stress and emotional reactivity. Differences in stress response between yoga practitioners and novices were hypothesized to explain differences in basal IL-6 levels between groups, where novices had levels 41% higher across sessions and were 4.75 times more likely to have detectable C-reactive protein levels. These findings suggest that regular yoga practice promotes a more adaptive physiological response to acute stressors, and dampened stress reactivity could account for differences in basal inflammatory markers and the long term health benefits of regular yoga practice (18). Collectively the above two studies suggest that short-term yoga practice is sufficient to improve stress reactivity and cognitive function, but long-term yoga practice is essential to shift the homeostatic balance towards more automatic, adaptive and efficient psychophysiological responses (15).
Chronic Stress and Inflammation
Regular yoga practice may provide neuroprotective benefits by contributing to an overall reduction in elevated cortisol and IL-6 levels, associated with chronic stress, age-related cognitive decline (8,11,12), and increased risk for neurodegenerative disorders, including AD and Multiple Sclerosis (19). Numerous reviews report the beneficial effects of yoga on autonomic, neuroendocrine and immune markers of chronic stress in healthy and clinical adult populations (4,20,21), but the physiological mechanisms underlying how yoga may protect against chronic stress and systemic inflammation warrant further study.
Findings from clinical trials in breast cancer survivors provide insight into how yoga may regulate inflammatory processes (22,23). Breast cancers survivors randomized into a 12-week Iyengar yoga intervention demonstrated reductions in upstream inflammation-related gene activity compared to a health education control (22). Yoga participants demonstrated reductions in pro-inflammatory nuclear factor kappa B (NF-κB) and cAMP response binding element (CREB) transcription factor activity, indicating decreased inflammation-related gene expression, despite no significant changes in downstream inflammatory markers (CRP and IL-6) or cortisol. The authors posit that mind-body practices with yogic elements may reduce inflammation via the NF-κB pathway. Additionally, yoga increased anti-inflammatory glucocorticoid receptor (GR) activity, suggesting that yoga may increase the sensitivity of GR to the anti-inflammatory effects of cortisol, rather than daily cortisol secretion (22). Indeed, GR resistance is linked to chronic stress (24,25) and the inability to downregulate the acute inflammatory response leading to subsequent inflammatory disease processes (24,26). These findings are particularly noteworthy as GR resistance may be essential in regulating stress reactivity, as decreased GR sensitivity could contribute to elevated cortisol levels (24).
A separate trial found that the regularity and frequency of yoga practice is essential for reducing systemic inflammation in breast cancer survivors (23), consistent with systematic review revealing >1000 minutes of yoga practice was associated with greater reductions in inflammation (20). Breast cancer survivors randomized into a 12-week Hatha yoga intervention demonstrated reductions in fatigue and downstream inflammatory markers (IL-6, TNF-α and IL-1β) at 3 months post-intervention, but not immediately after intervention, when compared to a waitlist control (23). Notably, increased frequency of practice post-intervention was associated with greater reductions in fatigue, IL-6 and IL-1β, where an increase of 10 minutes of yoga practice per day was associated with a 5% decrease in mean IL-6 and an 8% decrease in mean IL-1β. Given the apparent benefits of yoga on inflammatory gene expression (22) and the value of regular, long-term practice in a clinical population (23), these mechanisms warrant further study in the yoga-stress-cognition relationship.
Emotional Reactivity
Cross-sectional neuroimaging findings suggest that yoga practitioners are able to selectively disengage from aversive stimuli (27,28), providing them with a more adaptive response to stressors and decreased cognitive interference from emotionally-laden information. Stress and emotional regulation are intimately linked processes, where brain regions involved in emotion processing, such as the amygdala and ventrolateral prefrontal cortex (vlPFC) (16), are among the aging brain regions vulnerable to prolonged glucocorticoid exposure (12). Additionally, improved emotional regulation of negative stimuli predicts steeper cortisol slopes in older adults (29), and acute administration of synthetic cortisol has been shown to increase emotional interference (30). Yoga practitioners with at least 3 years of ongoing Hatha yoga experience demonstrate increased vlPFC activation – associated with inhibitory cognitive control over emotional distraction (16) – when presented with negative emotional distractors (27). Effectively, yoga practitioners are able to selectively disengage from negative emotional processing to focus on the cognitive demands of the task (27). Both yoga practitioners and controls demonstrated an increased amygdala response during negative emotional stimuli, reflecting limbic reactivity to emotional stimuli. However, only controls demonstrated a decrease in positive affect associated with the magnitude of amygdala response, suggesting that limbic reactivity was uncoupled from downstream effects on affect in yoga practitioners (27). Additional indirect findings report that expert yoga practitioners, with a mean of 9.6 years of regular practice, demonstrate improved pain tolerance as mediated by insular gray matter volume (GMV) (28). Notably, yoga practitioners were equipped with cognitive strategies cultivated during regular yoga practice to tolerate pain, a stressor experienced “off the mat.” These included parasympathetically activating and interoceptive strategies such as breathing, observation and acceptance, versus ignoring or distracting techniques utilized by controls (28). These findings suggest that yoga practitioners are able to downregulate and reappraise their emotional response to aversive emotional and pain stimuli, contributing to structural neurological and behavioral changes, and may reflect a more adaptive response to stressors. Yoga may therefore enable practitioners to shift neurocognitive resources away from aversive stimuli to limit interference from emotionally-laden information and enhance cognitive efficiency.
NEUROCOGNITIVE RESOURCE EFFICIENCY
The concept of neurocognitive resource efficiency used in this review builds and borrows from previous constructs laid in the literature (1,31), and will be used as an umbrella term that aims to capture structural (e.g., changes in grey matter volume), functional (e.g., regional BOLD activation and network connectivity) and behavioral differences (e.g., processing speed, selective and sustained attention; higher-order processes: crystallized, and fluid intelligence) between controls and yoga practitioners, as well as changes that might ensue as result of yoga practice, primarily in the context of age-related decline.
In the context of age-related cognitive decline (1), yoga may improve cognition in older adults by enhancing overall neurocognitive resource efficiency (7); allowing yoga practitioners to selectively disengage from task-irrelevant stimuli (27), create more resilient resting-state and tasking functional networks (32), and protect against age-related structural decline (33). The hippocampus is a commonly examined region in yoga-cognition research, as hippocampal neurogenesis is one of the most consistent effects of exercise training (34) and is susceptible to age- (35) and stress-induced atrophy (8) associated with cognitive deficits in AD (9).
By attending to physical postures, mental processes, and controlled breathing, yoga practitioners are thought to derive ample psychophysiological benefits (15). The literature points to structural and functional advantages in beginners, as well as regular yoga practitioners (7) from acute to chronic effects in cognition (2). Emerging evidence suggests that yoga practice might improve discrete (2) and higher-order (32) cognitive processes likely related to positive reorganizational changes, resulting in densely interconnected intrinsic connectivity networks (36,37), and ultimately leading to higher neurocognitive resource efficiency (Figure 2).
Figure 2: Neurocognitive Resource Efficiency: Network Connectivity and Structural Benefits.
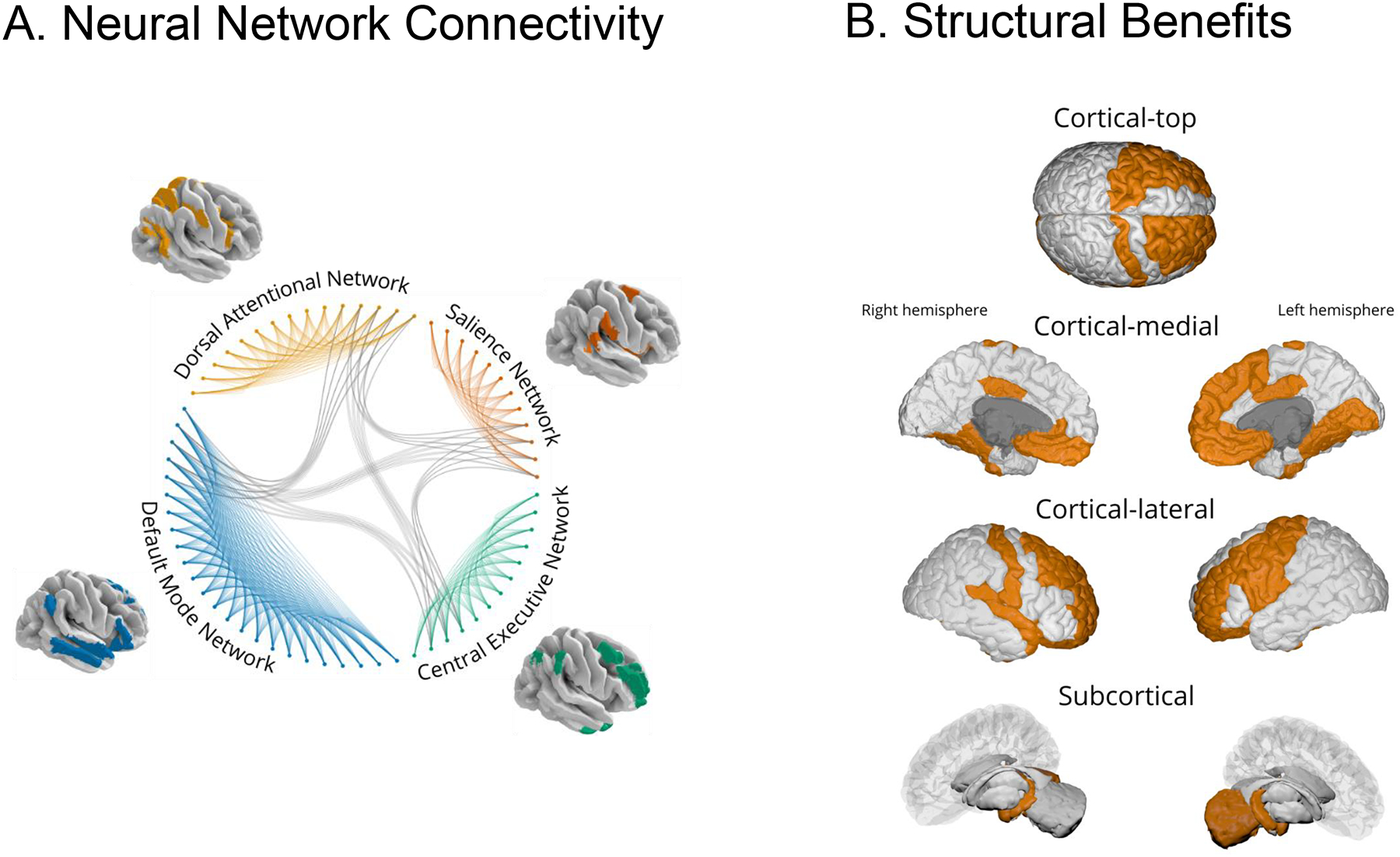
Left-side panel displays the hypothetical differential connectivity in relevant intrinsic connectivity networks in (A) yoga practitioners, as well as their corresponding topological distributions across networks. Our theoretical framework posits that repeated engagement of key nodes in overlapping attentional networks enhances rapid and flexible coupling with the Default Mode Network, resulting in dense within- and between-network connectivity (32,36). Right-side panel (B) showcases known structural benefits derived from yoga practice in cortical and subcortical brain regions(7,33,38,39).
Primary Structural and Functional Benefits
Cross-sectional findings demonstrate that yoga practitioners with at least 3 years of experience demonstrate greater GMV in frontal, limbic, temporal, occipital, and cerebellar regions and fewer cognitive failures compared to matched controls (38). GMV was positively correlated with years of experience and negatively correlated with cognitive failures, suggesting that years of yoga experience contributes to enhanced cognitive function associated with structural and neurological differences (38). Yoga practitioners, with a minimum of 3 years of experience, also demonstrate greater left hippocampal volume, a key region in learning and memory-related processes when compared to matched controls (39). Within the same cohort, activation of the left dorsolateral prefrontal cortex (dlPFC) was lower in the encoding phase of the working memory task, despite no differences in accuracy or reaction time between groups, suggesting greater neural efficiency in yoga practitioners when initially processing and storing information (39). These neurological findings corroborate results from meta-analyses on behavioral cognitive function (2), with the strongest effect of yoga on measures of attention and processing speed. Furthermore, yoga practitioners with ~10 years of experience did not demonstrate the classic trajectory of age-related GMV decline, displayed in matched controls, providing evidence for neuroprotective effects of yoga (33). Of note, frequency of physical postures followed by yogic meditation practice was the best predictor of hippocampal GMV (33), emphasizing the importance of breathing and meditation in combination with physical practice. Years of practice were also positively correlated with GMV in left hemisphere orbitofrontal cortex and mid-insula, suggested by authors to reflect improved emotional and autonomic regulation (33), aligning with effects of yoga on stress (18) and emotional regulation (27). More recent findings suggest that yoga may provide neuroprotective benefits, even after only 12 weeks of intervention (40). In this study, women with subjective cognitive decline and risk factors for AD participating in a Kundalini yoga plus Kirtan Kriya yoga intervention, did not demonstrate reductions in GMV as demonstrated by a memory enhancement training control group, aligning with the cross-sectional findings described above.
Improved Neural Network Flexibility
Yoga practice may contribute to complex reorganization of neural structures and dynamics, resulting in distinctive resting-state and task-related network connectivity (32,41). The above findings support the benefits of yoga on hippocampal volume (33,39), which is also associated with higher fluid intelligence, defined as the ability to cope with novel challenges using abstract reasoning thereby enabling flexible, adaptive behavior (42). These findings imply that this region might act a key moderator/mediator supporting higher fluid intelligence and improving network flexibility due to the high within-network density in the brain (43). Interestingly, fluid intelligence, hippocampal volume, and higher-order cognitive functions are highly susceptible to age-related decline (44), but simultaneously show considerable plasticity to yoga training (32).
Middle-age Kripalu yoga and meditation practitioners show lower rates of decline in fluid intelligence, more integrated brain networks, greater global efficiency, greater trade-off recruitment between segregated and integrated networks, and more resilient networks compared to controls (32). More resilient neural networks reflect less decline in global efficiency, a measure of integration between functionally adjacent brain regions, upon removal of key nodes after simulated aging-related neural damage (32). Trait mindfulness also positively correlated with network resiliency and global efficiency, and negatively correlated with characteristic path length, indicating greater overall network efficiency and integration, respectively (32). These results suggest that age-related decline in fluid intelligence might be attenuated by higher trait mindfulness, developed in regular yoga and meditation practice (45). Kripalu yoga is a form of Hatha yoga with an emphasis on meditation that could induce regular states of mindfulness. Although individuals with higher trait mindfulness and fluid intelligence may reflect a self-selection bias to practice yoga, other factors that could influence cognitive function were controlled including age, gender, education, crystallized intelligence, physical activity, and cognitive engagement in daily life. Therefore, network architecture seems to be affected by yoga practice, and network modularity and flexibility may contribute to higher-order cognitive outcomes such as fluid intelligence (32). By contributing to more efficient and integrated neural networks, yoga practice may lead to increased “cognitive bandwidth” available for cognitive demands to enhance overall neurocognitive resource efficiency.
Using the same group of aging Kripalu and meditation practitioners, Gard et al. conducted a follow-up study with an exploratory, network-based approach to examine local differences in resting-state functional networks (41), rather than global resting-state properties (32). Connectivity of the caudate nucleus (CN) was revealed to be a central node distinguishing between practitioners and controls, and network-based analyses demonstrated stronger connectivity of left and right CN to a number of brain regions, with no differences between yoga and meditation practitioners. The CN demonstrates age-related decline in volume (35), and authors hypothesize that increased caudate connectivity may mediate reductions in age-related cognitive decline, as indexed by lower rates of age-related decline in fluid intelligence from their earlier study (32), and contribute to cognitive and behavioral flexibility (41). These findings demonstrate increased local and global connectivity, aligning with network-based differences observed among experienced yoga practitioners during resting conditions (36).
Reorganizational Changes in the Default Mode Network
Yogic postures, breathing and meditation practices all rely on a strong attentional component, inferring that regular practice may impact connectivity in networks that decrease in activity during attention-demanding tasks, such as the default mode network (DMN). The DMN is related to episodic memory, self-referential, and discrete emotional processing, among other cognitive processes (46). Importantly, DMN connectivity is susceptible to age-related cognitive decline (47), and is improved by physical activity (48), and yoga practice (49). Elderly Hatha yoga practitioners, with at least 8 years of yoga practice, demonstrate greater anteroposterior connectivity between structures such as the medial prefrontal cortex (mPFC) and angular gyrus, as compared to controls (36). Additionally, a 12-week Kundalini and Kirtan Kriya yoga intervention in older adults with mild cognitive impairment showed an increase in DMN functional connectivity which positively correlated with verbal memory recall when compared to memory enhancement training (49). These findings suggest that yoga may enhance functional DMN connectivity to provide neuroprotective benefits during aging. Despite variations regarding specific areas within the DMN that increase or decrease in connectivity in the yoga-cognition relationship (7), protective effects against age-related decline in neural architecture and functionality are clearly apparent. In addition, the dlPFC, ventromedial PFC (vmPFC), posterior cingulate cortex (PCC) and the anterior cingulate cortex (ACC) have been repeatedly implicated in studies assessing regional differences (39) and within/between large-scale brain network connectivity (32,33) such as the DMN connectivity (36), and inform our mechanistic framework.
The PCC is a highly informative midline structure in our model of improved neurocognitive resource efficiency. Yoga practitioners demonstrate greater PCC GMV volume compared to controls, and weekly hours of yoga-related meditation, performed in addition to postures, positively predicts PCC GMV in practitioners (33). The yoga literature has primarily focused on regional activation (7), however, deactivation of key nodes may be more informative. Complementary findings demonstrate that advanced meditation practitioners consistently and volitionally deactivate DMN hubs such as the PCC and mPFC (50,51), associated with subjective experiences of “concentration” and “effortless doing” (51) and decreased mind-wandering (50). Less mind-wandering may decrease distractions related to task-irrelevant stimuli and reduce lapses in attention (50). Depth of mental silence (i.e. less mind wandering), was associated with GMV and functional connectivity in 23 Sahaja yoga practitioners (meditation-focused yoga practice), with an average of 14 years of practice (52). Greater right ACC GMV was significantly correlated with subjective report of depth of mental silence in practitioners. Similar positive associations were found between the resting-state functional connectivity between the right ACC and bilateral insula, and decreased connectivity between the ACC/mPFC and parahippocampal gyrus, a key mediotemporal node of the DMN. The authors suggest that these findings provide evidence for enhanced functional connectivity in regions essential for attention and emotion regulation, that are associated with depth of mental silence in experienced Sahaja yoga practitioners (52). In the same cohort of practitioners, increased functional connectivity between the left insula and mid-ACC was associated with lower interference in reaction time in a selective attention/interference inhibition task (53). Deactivation in the PCC could lead to an increased signal-to-noise ratio and thus, greater availability of cognitive resources and improve functional coupling between task-related networks (36).
Reorganizational Changes in Attentional Networks
Yoga instructors direct novice practitioners to attend to bodily sensations, breathing, and passing thoughts. As practitioners become more adept, they progress to open monitoring of thoughts, sensations and experiences, thereby compounding task demand as perceptual, sensory, and cognitive load increases. Greater cognitive load may shield against distraction, and enhance attentional abilities, by suppressing task-irrelevant information (54). Higher cognitive load demonstrates an inhibitory effect on antagonistic cortical and subcortical regions (54). These findings suggest that higher cognitive load enhances a state of high focal-task engagement by concomitantly activating fronto-insular regions related to attention-demanding tasks, while also preemptively suppressing activity in the bilateral amygdala, which could contribute to emotional distraction, and inform our mechanistic framework of the yoga-cognition relationship.
Task-related networks such as the dorsal attentional network (DAN), frontoparietal/central executive network (CEN), and cingulo-opercular network (CO) (46,55) are engaged during attention-demanding tasks. Meditation practitioners with an active Hatha yoga practice of at least 3 years demonstrate stronger interregional coupling within DAN regions, as well as stronger coupling between the ACC, dlPFC, and PCC compared to controls, indicating stronger coupling in attention and emotion regulation networks (37). Notably, a review of the yoga literature shows clear engagement of these attentional networks (56). Strong coupling between key nodes of the DAT, CEN, and CO have been found with key nodes of the DMN, such that older adults with MCI randomized to a 12-week yoga intervention demonstrated significant improvements in verbal memory correlated with increased resting-state functional connectivity between the PCC, ACC, right middle frontal cortex, and left lateral occipital cortex (49). Interestingly, experienced yoga practitioners with an average of 10 years of practice had the largest left frontal operculum volumes (33), a key node in the CO responsible for tonic attention/alertness (55), involved in language and hierarchical sequence processing (57). Authors suggest that an increased volume could reflect sequencing a personal practice, as experienced yoga practitioners are more likely to do (33). Alternatively, recruitment of key nodes in the CO, such as the anterior operculum, anterior insula and ACC (41,53), instead of CEN- and DAT-related regions (arguably more costly to engage) may represent a strategic switch in order to sustain attention and hence, performance. The overlapping engagement of attentional networks with visual, salience and default networks might indicate that over time, yoga participants repeatedly engage key nodes between networks and systematically increase node and edge functional coupling, possibly leading to a shielding against task-irrelevant distractors and resulting in higher neural efficiency. As yoga practitioners develop proficiency, they may become more efficient in their utilization of neurocognitive and attentional resources, contributing to improvements in cognitive function (32,39,49).
YOGA AS A HOLISTIC PRACTICE
A key limitation to this review, and the yoga literature as a whole, is the inherent difficulty in comparing findings across heterogeneous yoga interventions and styles. While much of modern yoga practiced in the Western world falls under the umbrella of Hatha yoga, including physical postures, meditation, and breath work, stylistic differences still abound. Some forms of yoga place a greater emphasis on chanting, meditation, and breath work (e.g., Kirtan Kriya, restorative), some emphasize vigorous physical activity (e.g., Bikram, Vinyasa or power yoga), some follow strict traditional sequencing or alignment guidelines (e.g., Ashtanga, Iyengar yoga), and some are designed for specific populations (e.g., prenatal, trauma-informed yoga). Additionally, the type of breathing and meditation practices can vary dramatically between sessions and styles of yoga, where breathing practices can have differential effects on autonomic arousal and meditation practices may challenge distinct cognitive processes by emphasizing focused attention versus open awareness. However, it is becoming increasingly apparent that integrating the core components of yoga (postures, breath work and meditation) is essential for deriving its cognitive benefits and may lead to summative or synergistic effects.
Studies comparing styles of yoga are rare but provide emerging insight into the components of yoga practice essential for cognitive health. A 7-week integrated yoga program incorporating all eight limbs of yoga, demonstrated greater reductions in cortisol and anxiety levels compared to a yoga as exercise group (emphasizing physical postures) and a questionnaire control group (58). An acute intervention comparing a single 30-minute meditative (Hatha) yoga to a 30-minute power (Vinyasa) yoga session demonstrated comparable findings (59). Anxiety scores and salivary cortisol levels were significantly lower after the meditative yoga session, but not power yoga. Combined, these findings suggest that the inclusion of meditation and breathing practices in addition to the physical postures, three of the eight limbs of yoga, are essential for yoga’s effects on stress regulation, a key mechanism in our model of yoga and cognitive health.
To the authors’ knowledge, only one study to date has specifically compared two types of yoga on objective cognitive outcomes (60) in which sedentary breast and ovarian cancer survivors were randomized into 12 weeks of either restorative yoga (minimal physical exertion and more meditative practice) or vigorous yoga (more physical exertion (approximately 60–70% maximal heart rate) and minimal meditative practice). Only the restorative yoga group (mean age 55 years) demonstrated significant improvements in overall cognitive function and fluid intelligence as measured by the NIH Toolbox Cognition domain, while participants in the vigorous yoga group (mean age 58 years) only improved in crystallized intelligence assessed at week 24. These findings suggest that the inclusion of breathing and meditative practices in restorative yoga had a greater impact on fluid cognitive function, such as processing speed, problem solving and memory, than vigorous yoga with an emphasis on physical activity. While limited by small sample sizes and lack of usual care control groups, these findings provide intriguing and preliminary implications that the cognitive benefits of yoga can be attributed to more than physical activity.
PARALLEL FINDINGS
The meditation and exercise literature provide complementary insight into the yoga-cognition relationship. Meditation improves attention and decreases stress reactivity (61), and higher levels of physical fitness are associated with decreased cortisol reactivity, decreased anxiety and more favorable mood in response to psychosocial stress utilizing the Trier Social Stress Test (62). Yoga practices are often referred to as “moving meditation,” accordingly, by combining an active attentional practice with physical movement, yoga may influence stress regulation via comparable mechanisms. Similar hypotheses exist in the exercise literature; the Cross-Stressor Adaptation hypothesis suggests that exposure to the stress of physical exercise promotes generalization to non-physical stressors (63) and the mindfulness stress-buffering hypothesis posits that mindfulness practice improves health outcomes by attenuating negative appraisal and stress reactivity to aversive stimuli (64). These align with self-regulatory mechanisms in yoga, in which yoga is believed to provide practitioners with the self-regulatory strategies to sustain the physical stress of an asana practice that can be generalized to stressors “off the mat” (15).
Parallel findings from the exercise and meditation literature suggest that the cognitive benefits of yoga may be attributed to more than physical activity; the combination of postures, breathing, and meditation practices appear to be essential to improving stress regulation and neurocognitive efficiency. Aerobic exercise is well accepted to enhance neurocognitive functioning (34). Similar to yoga practitioners, meditation practitioners demonstrate similar improvements in functional connectivity, flexibly coupling attentional networks with the DMN and other networks (65,66). Complementary findings on emotional reactivity to aversive painful stimuli in mindfulness practitioners suggest an uncoupling of the emotional experience from the aversive pain stimulus (67), paralleling findings in the yoga literature described above. Differences between mindfulness practitioners and controls were hypothesized to reflect an attentional shift to cognitive reappraisal and nonjudgmental sensory awareness of painful stimuli (67). Contemplative practices that aid practitioners in downregulating emotional reactivity may allow them to shift neurocognitive resources by neutrally reappraising aversive stimuli to focus on other cognitive demands and enhance cognitive efficiency. Additionally, theoretical arguments posit that bidirectional signaling via interoceptive processing (15) and stimulation of the vagus nerve along the gut-brain axis (68) may facilitate mind-body integration in yoga practice but remain to be systematically explored in examining the yoga-cognition relationship.
CONCLUSION
A recurrent theme in the yoga literature is the value of regular, long-term yoga practice, contributing to improvements in stress reactivity (18), markers of chronic stress and inflammation (18,20), emotional reactivity (27), GM volume (7,33,39), as well as neurocognitive behavioral responses (2,38), collectively improving neurocognitive efficiency. Short-term practice may initially improve stress regulation in order to form the foundations of a more adaptive stress response (17), reduce chronic stress, systemic inflammation and contribute to positive changes in brain structure and functional connectivity networks with consistent long-term practice. While regular, long-term yoga practice appears to be beneficial, determining the optimal frequency and duration of yoga practice to improve brain health remains challenging to interpret from the yoga literature. Many of the studies included in this review present cross-sectional findings with expert practitioners with at least 3 years of experience, or interventional studies typically lasting 12 weeks; therefore, yoga practice effects on cognition between these study durations remain to be investigated. Additionally, there is a need for more nuanced studies examining the differential effects of specific postures and breathing/meditation practices. Bidirectional signaling pathways, along with exploration of stylistic differences and optimal dosage effects, present an exciting avenue for future yoga-cognition research.
Key Points.
Mounting evidence highlights the role of yoga practice in improving cognition.
Few studies have examined the mechanisms underlying the yoga-cognition relationship.
Preliminary studies underscore the role of stress regulation and improved neurocognitive health as mediators.
Mechanisms discussed in this review corroborate the evidence for yoga as a lifestyle behavior to combat age-related cognitive decline.
ACKNOWLEDGEMENTS
This review was supported in part by grant R01 AG066630 from the National Institute on Aging. The authors would like to acknowledge the contribution of Martín Irani for his assistance in the generation of Figure 2A.
Funding:
This review was supported in part by grant R01 AG066630 from the National Institute on Aging.
Footnotes
Conflicts of interest: The authors report no conflict of interest.
REFERENCES
- 1.Park DC, Reuter-Lorenz P. The adaptive brain: Aging and neurocognitive scaffolding. Annu Rev Psychol. 2009;60:173–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gothe NP, McAuley E. Yoga and Cognition: A Meta-Analysis of Chronic and Acute Effects. Psychosom Med. 2015;77(7):784–97. [DOI] [PubMed] [Google Scholar]
- 3.Pascoe MC, de Manincor MJ, Hallgren M, Baldwin PA, Tseberja J, Parker AG. Psychobiological mechanisms underlying the mental health benefits of yoga-based interventions: A narrative review. Mindfulness (N Y). 2021;12:2877–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology. 2017;86:152–68. [DOI] [PubMed] [Google Scholar]
- 5.Pascoe MC, Bauer IE. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J Psychiatr Res. 2015;68:270–82. [DOI] [PubMed] [Google Scholar]
- 6.Schmalzl L, Powers C, Blom EH. Neurophysiological and neurocognitive mechanisms underlying the effects of yoga-based practices: Towards a comprehensive theoretical framework. Front Hum Neurosci. 2015;9(MAY):1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gothe NP, Khan I, Hayes J, Erlenbach E, Damoiseaux JS. Yoga Effects on Brain Health: A Systematic Review of the Current Literature. Brain Plast. 2019. Nov 8;5:105–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lupien SJ, De Leon M, De Santi S, Convit A, Tarshish C, Nair NPV, et al. Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci. 1998;1(1):69–73. [DOI] [PubMed] [Google Scholar]
- 9.Ouanes S, Popp J. High cortisol and the risk of dementia and alzheimer’s disease: A review of the literature. Front Aging Neurosci. 2019;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ershler WB. Interleukin-6: A Cytokine for Gerontolgists. J Am Geriatr Soc. 1993;41(2):176–81. [DOI] [PubMed] [Google Scholar]
- 11.Bradburn S, Sarginson J, Murgatroyd CA. Association of peripheral interleukin-6 with global cognitive decline in non-demented adults: A meta-analysis of prospective studies. Front Aging Neurosci. 2018;9:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–45. [DOI] [PubMed] [Google Scholar]
- 13.McEwen BS, Sapolsky RM. Stress and cognitive function. Curr Opin Neurobiol. 1995;5(2):205–16. [DOI] [PubMed] [Google Scholar]
- 14.Park CL, Riley KE, Bedesin E, Stewart VM. Why practice yoga? Practitioners’ motivations for adopting and maintaining yoga practice. J Health Psychol. 2016;21(6):887–96. [DOI] [PubMed] [Google Scholar]
- 15.Gard T, Noggle JJ, Park CL, Vago DR, Wilson A. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. 2014;8:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dolcos F, McCarthy G. Brain systems mediating cognitive interference by emotional distraction. J Neurosci. 2006;26(7):2072–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gothe NP, Keswani RK, McAuley E. Yoga practice improves executive function by attenuating stress levels. Biol Psychol. 2016;121:109–16. [DOI] [PubMed] [Google Scholar]
- 18.Kiecolt-Glaser JK, Cristian L, Preston H, Houts CR, Malarkey WB, Emery CF, et al. Stress, inflammation and yoga practice. Psychosom Med. 2010;72:113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuroendocrinol Lett. 2002;23(3):199–208. [PubMed] [Google Scholar]
- 20.Djalilova DM, Schulz PS, Berger AM, Case AJ, Kupzyk KA, Ross AC. Impact of Yoga on Inflammatory Biomarkers: A Systematic Review. Biol Res Nurs. 2019;21(2):198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Falkenberg RI, Eising C, Peters ML. Yoga and immune system functioning: a systematic review of randomized controlled trials. J Behav Med. 2018;41(4):467–82. [DOI] [PubMed] [Google Scholar]
- 22.Bower JE, Greendale G, Crosswell AD, Garet D, Sternlieb B, Ganz PA, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: A randomized controlled trial. Psychoneuroendocrinology. 2014;43:20–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiecolt-Glaser JK, Bennett JM, Andridge R, Peng J, Shapiro CL, Malarkey WB, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: A randomized controlled trial. J Clin Oncol. 2014;32(10):1040–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A. 2012;109(16):5995–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller GE, Sheldon C, Ritchley AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid resistance model. Heal Psychol. 2002;21(6):531–41. [DOI] [PubMed] [Google Scholar]
- 26.Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332(20):1351–62. [DOI] [PubMed] [Google Scholar]
- 27.Froeliger BE, Garland EL, Modlin LA, McClernon FJ. Neurocognitive correlates of the effects of yoga meditation practice on emotion and cognition: A pilot study. Front Integr Neurosci. 2012;6:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Villemure C, Čeko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014;24(10):2732–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Urry HL, Van Reekum CM, Johnstone T, Kalin NH, Thurow ME, Schaefer HS, et al. Amygdala and ventromedial prefrontal cortex are inversely coupled during regulation of negative affect and predict the diurnal pattern of cortisol secretion among older adults. J Neurosci. 2006;26(16):4415–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henckens MJAG, van Wingen GA, Joels M, Fernandez G. Time-dependent effects of cortisol on selective attention and emotional interference: A functional MRI study. Front Integr Neurosci. 2012;6:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reuter-Lorenz PA, Park DC. How Does it STAC Up? Revisiting the Scaffolding Theory of Aging and Cognition. Neuropsychol Rev. 2014;24(3):355–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gard T, Taquet M, Dixit R, Hölzel BK, de Montjoye YA, Brach N, et al. Fluid intelligence and brain functional organization in aging yoga and meditation practitioners. Front Aging Neurosci. 2014;6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villemure C, Čeko M, Cotton VA, Catherine Bushnell M. Neuroprotective effects of yoga practice: Age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci. 2015;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hillman CH, Erickson KI KA. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9:58–65. [DOI] [PubMed] [Google Scholar]
- 35.Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, et al. Regional brain changes in aging healthy adults: General trends, individual differences and modifiers. Cereb Cortex. 2005;15(11):1676–89. [DOI] [PubMed] [Google Scholar]
- 36.Santaella DF, Balardin JB, Afonso RF, Giorjiani GM, Sato JR, Lacerda SS, et al. Greater anteroposterior default mode network functional connectivity in long-term elderly yoga practitioners. Front Aging Neurosci. 2019;10:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Froeliger B, Garland EL, Kozink RV., Modlin LA, Chen NK, McClernon FJ, et al. Meditation-state functional connectivity (msFC): Strengthening of the dorsal attention network and beyond. Evidence-based Complement Altern Med. 2012;2012:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Froeliger B, Garland EL, McClernon FJ. Yoga meditation practitioners exhibit greater gray matter volume and fewer reported cognitive failures: Results of a preliminary voxel-based morphometric analysis. Evidence-based Complement Altern Med. 2012;2012:0–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gothe NP, Hayes JM, Temali C, Damoiseaux JS. Differences in Brain Structure and Function Among Yoga Practitioners and Controls. Front Integr Neurosci. 2018;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krause-Sorio B, Siddarth P, Kilpatrick L, Milillo MM, Aguilar-Faustino Y, Ercoli L, et al. Yoga Prevents Gray Matter Atrophy in Women at Risk for Alzheimer’s Disease: A Randomized Controlled Trial. J Alzheimer’s Dis. 2022;87:569–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gard T, Taquet M, Dixit R, Hölzel BK, Dickerson BC, Lazar SW. Greater widespread functional connectivity of the caudate in older adults who practice kripalu yoga and vipassana meditation than in controls. Front Hum Neurosci. 2015;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daugherty AM, Sutton BP, Hillman CH, Kramer AF, Cohen NJ, Barbey AK. Individual differences in the neurobiology of fluid intelligence predict responsiveness to training: Evidence from a comprehensive cognitive, mindfulness meditation, and aerobic exercise intervention. Trends Neurosci Educ. 2020. Mar 1;18:1–10. [DOI] [PubMed] [Google Scholar]
- 43.van den Heuvel MP, Sporns O. Rich-club organization of the human connectome. J Neurosci. 2011. Nov 2;31(44):15775–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raz N, Lindenberger U, Ghisletta P, Rodrigue KM, Kennedy KM, Acker JD. Neuroanatomical correlates of fluid intelligence in healthy adults and persons with vascular risk factors. Cereb Cortex. 2008;18(3):718–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kiken LG, Garland EL, Bluth K, Palsson OS, Gaylord SA. From a state to a trait: Trajectories of state mindfulness in meditation during intervention predict changes in trait mindfulness. Pers Individ Dif. 2015;81:41–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raichle ME. The Brain’s Default Mode Network. Annu Rev Neurosci. 2015;38:433–47. [DOI] [PubMed] [Google Scholar]
- 47.Toussaint PJ, Maiz S, Coynel D, Doyon J, Messé A, de Souza LC, et al. Characteristics of the default mode functional connectivity in normal ageing and Alzheimer’s disease using resting state fMRI with a combined approach of entropy-based and graph theoretical measurements. Neuroimage. 2014;101:778–86. [DOI] [PubMed] [Google Scholar]
- 48.Boraxbekk CJ, Salami A, Wåhlin A, Nyberg L. Physical activity over a decade modifies age-related decline in perfusion, gray matter volume, and functional connectivity of the posterior default-mode network-A multimodal approach. Neuroimage. 2016;131:133–41. [DOI] [PubMed] [Google Scholar]
- 49.Eyre HA, Acevedo B, Yang H, Siddarth P, Van Dyk K, Ercoli L, et al. Changes in Neural Connectivity and Memory Following a Yoga Intervention for Older Adults: A Pilot Study. J Alzheimer’s Dis. 2016;52(2):673–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A. 2011;108(50):20254–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garrison KA, Santoyo JF, Davis JH, Thornhill IV TA, Kerr CE, Brewer JA. Effortless awareness: Using real time neurofeedback to investigate correlates of posterior cingulate cortex activity in meditators’ self-report. Front Hum Neurosci. 2013;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hernández SE, Barros-Loscertales A, Xiao Y, González-Mora JL, Rubia K. Gray Matter and Functional Connectivity in Anterior Cingulate Cortex are Associated with the State of Mental Silence During Sahaja Yoga Meditation. Neuroscience. 2018;371:395–406. [DOI] [PubMed] [Google Scholar]
- 53.Barrós-Loscertales A, Hernández SE, Xiao Y, González-Mora JL, Rubia K. Resting State Functional Connectivity Associated With Sahaja Yoga Meditation. Front Hum Neurosci. 2021;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sörqvist P, Dahlström Ö, Karlsson T, Rönnberg J. Concentration: The neural underpinnings of how cognitive load shields against distraction. Front Hum Neurosci. 2016;10:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sadaghiani S, D’Esposito M. Functional characterization of the cingulo-opercular network in the maintenance of tonic alertness. Cereb Cortex. 2015;25(9):2763–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Aalst J, Ceccarini J, Demyttenaere K, Sunaert S, Van Laere K. What Has Neuroimaging Taught Us on the Neurobiology of Yoga? A Review. Front Integr Neurosci. 2020;14:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Friederici AD. The brain basis of language processing: From structure to function. Physiol Rev. 2011;91(4):1357–92. [DOI] [PubMed] [Google Scholar]
- 58.Smith JA, Greer T, Sheets T, Watson S. Is There More to Yoga Than Exercise? Altern Ther Health Med. 2011;17(3):22–9. [PubMed] [Google Scholar]
- 59.Marshall M, McClanahan M, Warren SM, Rogers R, Ballmann C. A Comparison of the acute effects of different forms of yoga on physiological and psychological stress: A pilot study. Int J Environ Res Public Health. 2020;17:6090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Deng G, Bao T, Ryan EL, Benusis L, Hogan P, Li QS, et al. Effects of Vigorous Versus Restorative Yoga Practice on Objective Cognition Functions in Sedentary Breast and Ovarian Cancer Survivors: A Randomized Controlled Pilot Trial. Integr Cancer Ther. 2022;1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, et al. Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci U S A. 2007;104(43):17152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mücke M, Ludyga S, Colledge F, Gerber M. Influence of regular physical activity and fitness on stress reactivity as measured with the Trier Social Stress Test protocol: A systematic review. Sport Med. 2018;48:2607–22. [DOI] [PubMed] [Google Scholar]
- 63.Sothmann MS. The Cross-Stressor Adaptation Hypothesis and Exercise Training. In: Acevedo EO, Ekkekakis P, editors. Psychobiology of physical activity. Human Kinetics; 2006. p. 149–60. [Google Scholar]
- 64.Creswell JD, Lindsay EK. How Does Mindfulness Training Affect Health? A Mindfulness Stress Buffering Account. Curr Dir Psychol Sci. 2014;23(6):401–7. [Google Scholar]
- 65.Zhang Z, Luh WM, Duan W, Zhou GD, Weinschenk G, Anderson AK, et al. Longitudinal effects of meditation on brain resting-state functional connectivity. Sci Rep. 2021;11(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vago DR, Zeidan F. The brain on silent: mind wandering, mindful awareness, and states of mental tranquility. Vol. 1373, Annals of the New York Academy of Sciences. 2016. p. 96–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gard T, Hölzel BK, Sack AT, Hempel H, Lazar SW, Vaitl D, et al. Pain attenuation through mindfulness is associated with decreased cognitive control and increased sensory processing in the brain. Cereb Cortex. 2012;22(11):2692–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]


