Abstract
Background:
Disparities in socioeconomic status (SES) have been associated with less weight loss after bariatric surgery. The objective of this study was to identify socioeconomic barriers to weight loss after bariatric surgery.
Methods:
We performed semi-structured interviews with bariatric surgery patients and providers from April-November 2020. Participants were asked to describe their post-operative experiences regarding dietary habits, physical activity, and follow-up care. Interview data were coded using Directed Content Analysis based on domains in Andersen’s Behavioral Model of Health Services Use and Torain’s Surgical Disparities Model.
Results:
24 patients (median of 4.1 years post-operatively; mean age 50.6 ±10.7 years; 12 bypass and 12 sleeve; 83% female) and 21 providers (6 bariatric surgeons, 5 registered dietitians, 4 health psychologists, and 6 primary care providers) were interviewed. Barriers to weight loss included: 1) challenging employment situations; 2) limited income; 3) unreliable transportation; 4) unsafe/inconvenient neighborhoods; and 5) limited health literacy.
Conclusions:
Interventions targeting socioeconomic barriers to weight loss are needed to support patients, particularly those who are socioeconomically disadvantaged.
Keywords: bariatric surgery, socioeconomic status, qualitative research
INTRODUCTION
The most effective weight loss treatment for adults with severe obesity (body mass index [BMI] ≥ 35 kg/m2) is bariatric surgery, which is performed on nearly 260,000 patients annually in the U.S.1-4 Compared to behavioral weight management alone, bariatric surgery generates greater morbidity resolution, particularly for conditions such as type 2 diabetes, hypertension, and non-alcoholic steatohepatitis.5 Bariatric surgery also results in improved quality of life and a longer lifespan,2,5 and is associated with improved outcomes related to Covid-19.6
Despite the effectiveness of bariatric surgery, disparities in surgical outcomes related to socioeconomic status (SES) have been described. Using Medicaid as a proxy for socioeconomic deprivation, multiple studies have concluded that Medicaid patients undergoing bariatric surgery experience less weight loss compared to non-Medicaid patients and have higher rates of emergency department visits and readmissions.7,8,9 In single institution retrospective studies, Medicaid patients lost 50-54% of their excess body weight after one year, while non-Medicaid patients lost 64-66%.8,9 Analyses of national databases have concluded that Medicaid insurance status is associated with longer hospital lengths of stay10,11 and higher complication rates.11 The reasons for these outcomes disparities according to SES have not been investigated.
The objective of this study was to investigate patient and provider perceptions of SES-related barriers to care following bariatric surgery. We hypothesized that patients and providers would describe numerous barriers to care after bariatric surgery that made long-term weight loss more challenging for low SES patients.
MATERIALS AND METHODS
Study population and setting
Bariatric surgery patients, bariatric surgeons, RDs, health psychologists, and PCPs were recruited for participation given their involvement in the management of bariatric surgery patients and to ensure comprehensive representation of the post-operative bariatric surgery experience.
Bariatric surgery patients – Patients were identified via the prospectively maintained institutional bariatric surgery database at the University of Wisconsin Hospital and Clinics (UW-Madison). Those who had undergone laparoscopic sleeve gastrectomy or Roux-en-Y gastric bypass between January 2014 and December 2017 were eligible for participation. This period was selected to ensure that patients had at least one year of follow-up. Given that our research question involved SES and weight loss outcomes, we sought to recruit similar numbers of low and high SES patients, and patients with “suboptimal” and “optimal” weight loss. Low SES was defined as having Medicaid within 3 years of their bariatric procedure. This period was chosen given that Medicaid patients typically have limited socioeconomic mobility.12 “Optimal” weight loss was defined as ≥ 50% excess weight loss (EWL) at the most recent follow-up. Although there is no clear consensus regarding what constitutes “optimal” weight loss after bariatric surgery, >50% excess weight loss is a commonly applied parameter.13
Providers – Providers from two bariatric surgery programs in Wisconsin (UW-Madison and Froedtert Hospital) were eligible for participation. The provider specialties included the three core groups that comprise bariatric programs: bariatric surgeons, dietitians, and health psychologists. PCPs were also recruited for participation because they are closely involved in the long-term care of bariatric surgery patients. PCPs who had referred at least one Medicaid patient for bariatric surgery within the past year were eligible. PCPs were recruited from the Wisconsin Network for Health Research (WiNHR), a state-wide collaborative that includes primary care providers from four institutions (UW-Madison; Marshfield Clinic; Aurora Health Care; and Gundersen Health System) that care for regionally (urban/rural) and ethnically diverse patient populations.14
Interview Guide Construction
Two conceptual models were used to generate the interview guides. One model was Andersen’s Behavioral Model of Health Services Use, which our group has previously adopted for bariatric surgery15 and used to assess system-level barriers to bariatric surgery.16 Andersen’s model focuses on utilization of health care services by individuals, patients-provider interactions, and the health care system.17 The second conceptual model, Torain’s Framework for Surgical Disparities, was incorporated because it targets disparities in surgical care.18 In addition to the patient, provider, and health care system domains in Andersen’s model, Torain’s model includes two additional domains: post-operative/rehabilitation care and clinical care/quality. The interview guides (eMethods 1) focused on patient and provider perspectives on the facilitators and barriers to post-operative weight loss within these five conceptual model domains and three areas of clinical relevance for bariatric surgery patients: 1) dietary; 2) physical activity; and 3) follow-up care recommendations.
Participant recruitment and data collection
Recruitment letters and emails were sent to eligible patients and providers, respectively. Individuals were invited to participate in audio-recorded, semi-structured interview (60 minutes for patients; 30 minutes for providers). Interviews were conducted by two research team members (EA, BP) between January and November 2020 via WebEx video teleconferencing (with the exception of three interviews with UW-Madison bariatric surgeons, which were conducted in person). Verbal consent was obtained prior to all interviews. We purposefully sampled patients and providers to achieve thematic saturation regarding the primary research question, which investigated socioeconomic disparities in weight loss outcomes after bariatric surgery. Following each interview, participants completed a demographic survey, which included questions about age, sex and gender identity, race and ethnicity, marital status, education, and employment (patients only).
Data analysis
Each interview was transcribed, de-identified, and uploaded to NVivo Version 12.19 A priori codes were created based on Andersen and Torain models, according to the principles of directed content analysis.20 After creation of the initial codebook, six research team members (LMF, EA, CRB, BP, DFE, CIV) independently coded five transcripts (11% of the total, one transcript from each participant group). They subsequently met as a group after each transcript was independently coded to discuss coding annotations and uncertainties, clarify code definitions (i.e., coding rules), and finalize the codebook. Any emerging themes (e.g., Covid-19) were captured as new code. A detailed decision log was kept and shared with the entire team after each meeting. There were 46 codes created within five domains adopted from the Andersen and Torain models in the codebook (eTable 1). This manuscript includes data from 17 codes pertaining to the “Patient factors” domain.
Once the codebook was finalized, four coders (EA, CRB, LE, BP) coded the remaining transcripts using the technique of constant comparison.21 The coders met weekly to discuss any transcript segments that were unclear, assess coding consistency, and reach consensus for data interpretation. Once all of the transcripts for a participant group were coded, the research team discussed whether thematic saturation had been achieved or whether additional interviews were needed. Thematic saturation was achieved when the study team felt that additional analysis of a participant group would lead to limited or no new information.22 Once all 45 transcripts were coded, the research team created data matrices, which categorized the codes with dietary habits, physical activity, and adherence to follow-up care as the rows, and participant groups (patients and providers) as the columns. The themes emerging from this process were discussed among research team members (LMF, EA, JAM, CRB, BP, LE, DFE, CIV) to articulate higher-level concepts and make broader connections to the field.23
The UW-Madison Institutional Review Board approved the study (IRB protocol #2017-0443). All study procedures were performed in accordance with the Helsinki Declaration of 1975. A detailed description of our adherence to the 32 items in the Consolidated Criteria for Reporting Qualitative Research (COREQ) reporting guidelines is included in eMethods 2.
RESULTS
Participant characteristics
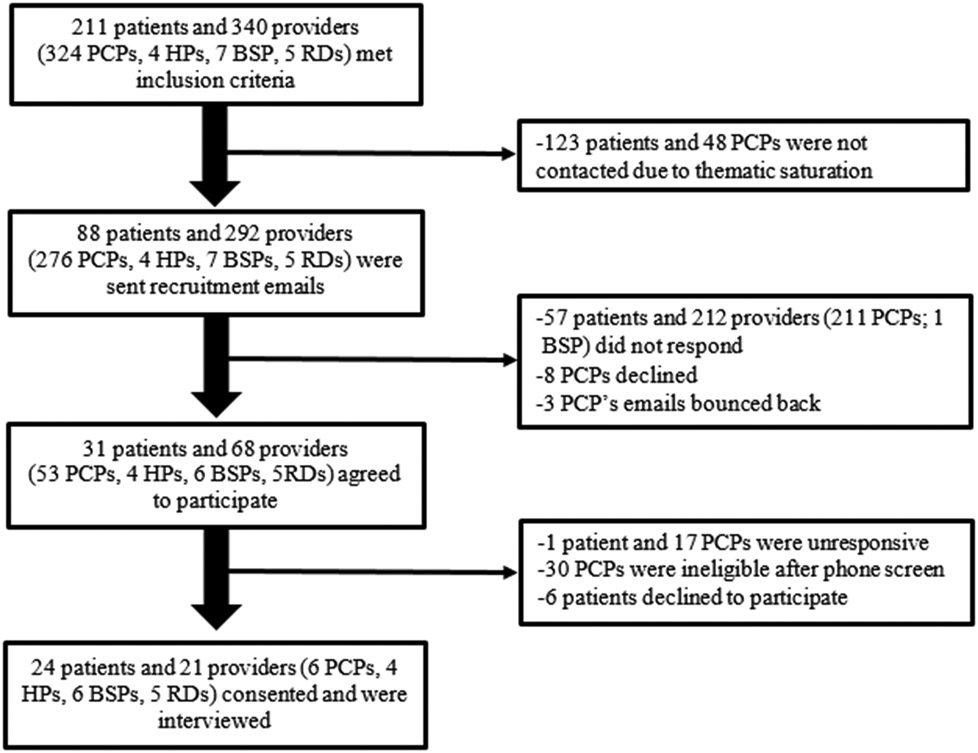
Five hundred fifty-one patients and providers met the study inclusion criteria (Figure 1). Recruitment materials were sent to 88 patients and 292 providers. The remaining 171 individuals were not contacted because thematic saturation was reached prior to needing their participation. Forty-five participants were interviewed, including 24 patients and 21 providers (6 bariatric surgeons, 4 HPs, 5 RDs, and 6 PCPs). The average age of patients and providers was 50.6 (±10.7) and 40.9 (±7.7) years, respectively (Table 1). The patient cohort was nearly evenly split between Medicaid “optimal weight loss” (n=6), Medicaid “suboptimal weight loss” (n=6), non-Medicaid “optimal weight loss” (n=5), and non-Medicaid “suboptimal weight loss” (n=7) patients. Compared to non-Medicaid patients, patients with Medicaid were slightly younger (49.9 vs. 51.3 mean age for non-Medicaid patients), less commonly female (75% of the Medicaid group vs. 91%), and had higher starting BMIs (50.3 vs. 47.0 mean starting BMI for non-Medicaid patients). The median time that had elapsed for patients since their bariatric procedure was 4.1 (IQR 0.9) years. Half of the patient cohort was employed part or full time, and 59% reported a household income of $49,000 or less.
Figure 1. Study participant flowchart.
PCP: Primary care providers; HP: Health psychologist; BSP: Bariatric surgery provider; RD: Registered dietitian
Table 1.
Study participant demographics
| Patients (n=24) |
Providers (n=21) |
|
|---|---|---|
| Age (mean, SD) | 50.6 (±10.7) | 40.9 (±7.7) |
| Sex (n, %) | ||
| Male | 4 (17) | 4 (19) |
| Female | 20 (83) | 17 (81) |
| Race (n, %) | ||
| White | 19 (79) | 21 (100) |
| Black or African American | 5 (21) | 0 |
| Ethnicity (n, %) | ||
| Hispanic or Latino | 0 | 2 (10) |
| Not Hispanic or Latino | 24 (100) | 19 (90) |
| Insurance status (n, %) | ||
| Medicaid | 12 (50) | |
| Non-Medicaid | 12 (50) | |
| Excess weight loss (n, %) | ||
| ≥50% excess weight loss | 13 (54) | |
| <50% excess weight loss | 11 (46) | |
| Type of bariatric surgery (n, %) | ||
| Roux-en-Y gastric bypass | 12 (50) | |
| Laparoscopic sleeve gastrectomy | 12 (50) | |
| Years of follow-up (mean) | 4.0 (0.6) | |
| Years in practice (mean, SD) | 11.5 (±8.2) | |
| Marital status (n, %) | ||
| Married | 6 (25) | |
| Single, never married | 12 (50) | |
| Divorced/Separated/Widowed | 6 (25) | |
| Highest level of education (n, %) | ||
| Bachelor’s/Associate Degree or Trade/Technical/vocational school |
14 (58) | |
| High school grad/some college/no degree | 9 (38) | |
| Some high school | 1 (4) | |
| Current work status (n, %) | ||
| Employed, full or part-time | 12 (50) | |
| Unemployed | 3 (13) | |
| Retired | 4 (17) | |
| Disabled | 5 (21) | |
| Annual household income (n, %) | ||
| Greater than $100,000 | 4 (17) | |
| $50,000-$99,999 | 3 (13) | |
| $25,000-$49,000 | 7 (29) | |
| Less than $25,000 | 9 (38) | |
| Declined to answer | 1 (4) | |
| Financial situation (n, %) | ||
| Difficulty paying bills or little to spare | 15 (63) | |
| No difficulties | 9 (37) | |
Study themes
We identified five themes pertaining to socioeconomic status and barriers to weight loss after bariatric surgery: 1) limited health literacy; 2) challenging employment situations; 3) limited income; 4) unreliable transportation; and 5) unsafe/inconvenient neighborhoods (Table 2). Representative patient and provider quotations are shown in Table 3.
Table 2.
Socioeconomic barriers to weight loss after bariatric surgery
| Barrier theme | Description of barrier theme |
|---|---|
| 1. Challenging employment situations | Patients who had physically demanding jobs or multiple jobs struggled to follow dietary, physical activity, and follow-up care recommendations. |
| 2. Limited income | Lower income patients: a) had a difficult time affording supplements and vitamins; b) skipped meals or relied on cheaper convenience food options/unhealthy options at food pantry; c) did not have access to affordable fitness centers; d) did not have reliable internet access for virtual follow-up meetings; e) struggled with gas money and co-pays, which prevented their attendance to follow-up meetings. |
| 3. Unreliable transportation | Patients who did not have reliable transportation were restricted by bus routes to obtain healthier foods. Public transportation or insurance-provided transportation (e.g., scheduled service driver) was often unreliable. |
| 4. Unsafe/inconvenient neighborhoods. | Grocery stores in disadvantaged neighborhoods carried fewer healthy options. Patients in these neighborhoods struggled to have groceries delivered to their homes because of fear of theft. These neighborhoods were often unsafe for exercising or did not have sidewalks. |
| 5. Limited health literacy | Patients with less formal education needed more training/teaching regarding recommendations for diet, physical activity, and post-op care. |
Table 3.
Representative patient and provider quotes
| Themes | Quotations |
|---|---|
| Challenging employment situations | “Before, the position I had was at night, so I wasn’t able to make a lot of the support groups, because they were held at night…a lot of it was between my hours and the distance. It was hard to make my yearly follow up appointments and even the support groups.” (P38) |
| “An employer might not let them have the day off, or if they fill out the FMLA paper…some employers will subtly punish an employee for using their FMLA because that means that their work is shorthanded that day. So, the employee may choose not to take that day off and make it into the appointment for dietitian post-op visits.” (PCP4) | |
| Limited income | “I’m not at a point where I want to go workout at an in person club. Also, finances, it’s expensive, and it’s not something that I have the money to spend on right now.” (P51) |
| “My higher socioeconomic patients can go out their front door and go for a walk, or they’ll join a gym that you know, not everyone has access to.” (RD5) | |
| “[Lower SES patients] may not be able to watch workout videos as easily because they don’t have access to internet. Medicare just approved that we can do phone visits for patients because some people don’t have the ability to do virtual visits…we can’t get enough of a connection to do one.” (HP2) | |
| Unreliable transportation | “I don’t think we’re going to be able to get a new car when my car dies. So, that’s gonna present a problem because right now we’re able to go through the mobile food pantry.” (P1) |
| “The only thing that makes you mad is the wait time. They [medical ride] almost make you late, and then they’re always late picking you up.” (P16) | |
| “There’s no public transit [in rural areas], so they’re really reliant on getting that one weekly ride to the store. If they don’t have what they need at that time, they’re kind of out of luck until the next time that ride comes.” (PCP6) | |
| “I had a number of patients who would not be there on time. They would show up an hour late or not at all. They would call and say, ‘Oh my ride never came’ even though they scheduled with the service.” (HP4) | |
| Unsafe/inconvenient neighborhoods | “My [neighborhood] is hilly. It’s an upward climb. Then you’ve got to walk straight back down the hill, and there aren’t a lot of sidewalks.” (P16) |
| So many people cannot go walking in their neighborhood or can’t go walking at night…If you work, work first shift, by the time you get home, it might be dark and unsafe. (HP2) | |
| Limited health literacy | “I’m a college graduate so they don’t say anything that’s like above what I comprehend and understand. So, I know, anything they would say whether they use medical terminology or not, I understand.” (P17) |
| “I think there is clearly a correlation between [patients’] financial socioeconomic status and their education. I think that contributes to their misunderstanding or, inappropriate expectations of what life after surgery is gonna be like. [They think] they just have the surgery, lose the weight, and they’re done.” (PCP 4) | |
| If [Southern] is the cooking you had, and you come from a family where maybe you’re the first person to graduate from high school, maybe you haven’t had that exposure, so once we teach you, you’ll know…because in your family, corn and creamy coleslaw are vegetables. (HP 2) |
HP=health psychologist; P=patient; RD=registered dietitian; BSP=bariatric surgery provider; PCP=primary care physician
Theme #1: Challenging employment situations
All four provider types and patient groups reported that patient occupation affected a patient’s ability to adhere to recommendations after surgery. Challenging employment situations included physically strenuous jobs, holding multiple jobs at once, or jobs that required significant travel. A PCP remarked, “My patients…when they are working double shifts, they will be less interested in doing things like meal planning and definitely will eat more by impulse.” Patients also reported that sedentary jobs and working from home made it more difficult to comply with dietary and physical activity-related recommendations. A health psychologist felt that “just the physical idea of going to the gym at the end of a long factory shift…it can be really a challenge to even encourage patients to want to do that after work.”
Theme #2: Limited income
All four provider groups and both groups of Medicaid patients described challenges related to obtaining nutritious foods and supplements after surgery. A health psychologist stated that “Sometimes it’s not necessarily forthright non-adherence; it’s a matter of circumstance. Some people say, ‘I can afford only one shake a day and that’s all I can have.’ Or, ‘I ran out of money for my vitamins or my shakes, so I’m not really sure what I can do to get my protein up again.’” Given these challenges, patients occasionally skipped meals or obtained less expensive, non-nutritious foods from convenience stores or food pantries. “Patients have to delay meals, skip meals or have very subpar nutritional intake, because they just don’t have the income to buy more balanced meals, healthier options, or just are reliant on convenience food options that are cheaper,” according to another health psychologist participant. One Medicaid patient described her experience at a food pantry: “They don’t give you [healthy food] at the food pantry, and that’s where we are at this point. We need to get food from the food pantry sometimes. It’s high sodium, processed meats, processed foods.”
Theme #3: Unreliable transportation
Providers and Medicaid patients reported that patients who did not have their own car or another form of reliable transportation faced unique challenges to attending follow-up visits. A dietitian remarked, “We definitely have patients who will have to cancel because they just don’t have a ride or their ride didn’t show up or things like that.” Public transportation services could be unreliable. A bariatric surgeon commented, “Sometimes it’s transportation…maybe they don’t have a car. The bus line that comes [to the clinic] does not go to all the neighborhoods where our patients come from.” Patients who lived in rural areas also described having difficulty attending visits in the winter due to unsafe road conditions.
Theme #4: Unsafe/inconvenient neighborhoods
Providers reported that patients who lived in some rural settings had limited access to grocery stores with healthier food options and nutritional supplements. One PCP remarked, “We’re fairly rural here; Walmart is 30 miles away. Local grocery stores…there’s only one in the county. There are dozens of convenience stores. So, being rural definitely makes it harder to get to a quality food source.” Patients in socioeconomically disadvantaged neighborhoods faced another set of challenges. According to one PCP, “A lot of my disadvantaged patients live in the area where it’s difficult for them to easily get out and take walks. I hear that a lot. I literally hear from people that, ‘If I take a walk, I may be robbed or shot.’” Patients who lived in a rural environment reported different challenges related to physical activity: “We live out in the country, so we have less of the ability to go walking,” noted one bariatric patient.
Theme #5: Limited health literacy
Providers reported that patients with less formal education needed more teaching about the dietary, physical activity, and follow-up recommendations from the bariatric surgery team. One bariatric surgeon noted that “I think there’s a great degree based on educational status how patients understand exactly what is expected of them to make them achieve a great result.” A registered dietitian felt that “some patients just don’t feel comfortable performing exercises by themselves because they don’t know if they are doing them correctly.” A bariatric surgeon stated that “Sometimes… people have never learned how to exercise. They don’t know what to do.”
Participant type comparison
A comparison of the categories of sub-themes that each participant group experienced is shown in eTable 2. Notably, Medicaid patients expressed difficulty affording nutritional supplements and relying on convenience store options while non-Medicaid patients did not. Both Medicaid and non-Medicaid patients with suboptimal weight loss reported that not having access to a gym made it more difficult to work out.
DISCUSSION
Bariatric surgery patients and providers involved in bariatric care described numerous socioeconomic barriers to optimal weight loss after surgery. All participant groups reported that challenging employment situations and limited income were barriers to long-term weight loss. Difficulties pertaining to household location and transportation were also described as important barriers. Providers felt that patients with lower health literacy encountered difficulties in adhering to the postoperative treatment recommendations.
Our participants described numerous barriers to optimal weight loss following bariatric surgery that were attributable to the workplace. There is a paucity of data, particularly qualitative research, describing how a surgical patient’s employment environment affect their outcomes. Numerous studies have explored whether bariatric surgery is associated with the likelihood of employment,24-26 but they have not examined the context within which bariatric patients are employed. This is a highly understudied area, one in which interventions may be developed and tested to help patients navigate post-operative dietary and physical activity recommendations in the context of their employment situations. For example, patients working from home may need modified dietary counseling and support given their mostly unstructured workdays compared to a patient who works in a factory.
All provider groups and our Medicaid participants noted that low income created difficulties after bariatric surgery given that nutrition supplements, healthy foods, and environments promoting physical activity, such as health clubs, were costly. One study of claims data from 2011-2017 found that out-of-pocket costs pertaining to medical care and prescription medications alone exceed $1,000 annually during the three years after bariatric surgery.27 To our knowledge, there is no published literature on out-of-pocket costs related to vitamins, supplements, healthy diets, and physical activity following bariatric surgery. An anonymous survey of 529 British bariatric surgery patients found that cost was the most important reason for poor supplement adherence in 11.5% of patients.28 It is unclear if these findings generalize to patients in the U.S. given that the British system of healthcare differs substantially. Additionally, there is significant variation in supplement recommendations, brands, and dosing that bariatric surgery programs may recommend for patients. This represents another potential target for research and innovation. Standardization of supplement recommendations and minimizing out-of-pocket costs, particularly for low SES patients, may increase adherence to supplements and optimize long-term outcomes.
Transportation difficulties and challenging patient household locations (both urban and rural) were reported by patients and providers to be important barriers to optimal weight loss after bariatric surgery. Multiple studies, including a qualitative study of bariatric patients in the Veterans Health Administration system,16 have found that long travel distances are problematic for bariatric patients.29 However, these studies have primarily focused on challenges to receipt of bariatric surgery, rather than how distance is a barrier for long-term follow-up and weight loss. Recent advances in telemedicine availability spurred on by the Covid-19 pandemic have resulted in improved obesity care access for some patients.30 Yet, patients from lower socioeconomic strata are more likely have limited capabilities to receive telemedicine services, as our participants noted. Additionally, the ability to exercise outside is limited for some patients who live in rural or unsafe environments. Ensuring universal access to safe places to exercise represents another area ripe for innovation and investment.
Our provider participants were concerned that low health literacy adversely impacted bariatric surgery patients, particularly patients from lower socioeconomic strata. The literature indicates that the information available to patients from academic and community medical centers generally fails to meet healthcare literacy standards. In a 2022 review of hernia center websites in the U.S., 0 of 96 websites had an appropriate reading level (6th grade), and most websites at a 12th grade reading level.31 An observational study by Miller-Matero and colleagues found that bariatric surgery patients with lower health literacy were more likely to regain weight 2-4 years after bariatric surgery.32 Similarly, limited health literacy has been identified as a barrier to weight loss for patients participating in medical weight loss programs.33 Interventions targeting bariatric patients with lower health literacy could help address the long-term disparity in weight loss outcomes.
This study has several limitations. First, recall bias may have impacted our participant comments. However, all themes identified in our analysis were reported by multiple groups of participants, so the likelihood of recall bias altering our findings is low. Second, our participants were predominantly White and from the Midwest. The perspectives of our participants may not be representative of other groups of patients and providers. Given that our study was focused on socioeconomic differences, we obtained viewpoints from widely disparate economic backgrounds. For example, 50% of the patient participants were insured by Medicaid, compared to 30% of our overall bariatric surgery cohort from 2008-2017.12 Additionally, 21% of the patients in the current study were non-white, compared to 11% of our overall cohort.12 Third, we categorized patients into weight loss groups using an “optimal” weight loss cut-off of 50% EWL. This may have miscategorized some patients. For example, a participant may have had 49% EWL at the time of the data pull, but a 52% excess weight loss at the time of the interview. However, we reported the experiences of all patients based on their descriptions of their socioeconomic challenges and thus still would have captured themes related to SES barriers.
In conclusion, socioeconomic barriers to optimal bariatric surgery outcomes included challenges related to employment, transportation, housing location, income, and education. To level the playing field, interventions targeting these areas, which leverage technology and financial resources, are essential. Given that perceptions about barriers may differ between patients and providers, tailored, theory-based solutions must be developed, tested, and implemented in a multidisciplinary fashion to ensure optimal outcomes and access for our bariatric patients.
Supplementary Material
HIGHLIGHTS.
We interviewed 45 patients and providers (surgeons, dietitians, health psychologists, PCPs)
SES barriers after bariatric surgery included employment, income, and transportation challenges.
Unsafe/inconvenient neighborhoods and limited health literacy were also barriers.
Interventions targeting these factors are needed to support bariatric surgery patients.
Sources of Funding and Conflicts of Interest
Effort on this study and manuscript was made possible by a National Institutes of Health R-21 (R21MD012655-01), an American College of Surgeons George H.A. Clowes Career Development Award, and a VA Career Development Award to Dr. Funk (CDA 015-060), as well as a VA Research Career Scientist award to Dr. Voils (RCS 14-443). Funding was also through the NIH Metabolism and Nutrition Training Program T32 (DK007665) to Dr. Murtha. Through collaboration with the Wisconsin Network for Health Research (WiNHR), this publication was supported by Grant Number UL1TR002373 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, the DVA, or the U.S. Government. The authors declare no conflicts of interest related to these funding sources.
REFERENCES
- 1.Estimate of bariatric surgery numbers, 2011-2018. (Accessed September 22, 2020, at https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers.)
- 2.Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. New Engl J Med 2017;376:641–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. New Engl J Med 2012;366:1577–85. [DOI] [PubMed] [Google Scholar]
- 4.Maciejewski ML, Arterburn DE, VS L.V., et al. Bariatric Surgery and Long-Term Durability of Weight Loss. JAMA Surg. 2016;151(11):1046–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The Effectiveness and Risks of Bariatric Surgery: An Updated Systematic Review and Meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aminian A, Fathalizadeh A, Tu C, et al. Association of prior metabolic and bariatric surgery with severity of coronavirus disease 2019 (COVID-19) in patients with obesity. Surg Obes Relat Dis 2021;17:208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mora-Pinzon MC, Henkel DS, Miller RS, et al. Emergency department visits and readmissions within one year of bariatric surgery: a statewide analysis using hospital discharge records. Surgery 2017;162:1155–1162 [DOI] [PubMed] [Google Scholar]
- 8.Funk LM, Suzo A, Mikami DJ, Needleman BJ. Two-year outcomes for medicaid patients undergoing laparoscopic Roux-en-Y gastric bypass: a case-control study. Obes Surg 2014;24:1679–85. [DOI] [PubMed] [Google Scholar]
- 9.Chen EY, Fox BT, Suzo A, et al. One-year Surgical Outcomes and Costs for Medicaid Versus Non-Medicaid Patients Undergoing Laparoscopic Roux-en-Y Gastric Bypass: A Single-Center Study. Surg Laparosc Endosc Percutan Tech. 2016;26(1):38–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dallal RM, Datta T, Braitman LE. Medicare and Medicaid status predicts prolonged length of stay after bariatric surgery. Surg Obes Relat Dis 2007;3:592–6. [DOI] [PubMed] [Google Scholar]
- 11.Carbonell AM, Lincourt AE, Matthews BD, Kercher KW, Sing RF, Heniford BT. National study of the effect of patient and hospital characteristics on bariatric surgery outcomes. Am Surg 2005;71:308–14. [PubMed] [Google Scholar]
- 12.Liu N, Venkatesh M, Hanlon BM, et al. Association Between Medicaid Status, Social Determinants of Health, and Bariatric Surgery Outcomes. Ann Surg Open 2021;2:e028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grover BT, Morell MC, Kothari SN, Borgert AJ, Kallies KJ, Baker MT. Defining Weight Loss After Bariatric Surgery: a Call for Standardization. Obesity Surg 2019;29:3493–9. [DOI] [PubMed] [Google Scholar]
- 14.Bailey H, Agger W, Baumgardner D, et al. The Wisconsin Network for Health Research (WiNHR): a statewide, collaborative, multi-disciplinary, research group. WMJ 2009;108:453–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen’s Model of Health Services Use. Surg Obes Relat Dis 2018;14:404–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Funk LM, Alagoz E, Jolles SA, et al. A Qualitative Study of the System-level Barriers to Bariatric Surgery Within the Veterans Health Administration. Ann Surg. 2022. Jan 1;275(1):e181–e188. doi: 10.1097/SLA.0000000000003982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen's Behavioral Model of Health Services Use: a systematic review of studies from 1998-2011. Psychosoc Med 2012;9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Torain MJ, Maragh-Bass AC, Dankwa-Mullen I, et al. Surgical Disparities: A Comprehensive Review and New Conceptual Framework. J Am Coll Surg 2016;223:408–18. [DOI] [PubMed] [Google Scholar]
- 19.Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration's MOVE! Weight Management Program. Translational behavioral medicine 2011;1:551–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- 21.Charmaz K. Constructing Grounded Theory: a practical guide through qualitative analysis. London: SAGE Publications; 2006. [Google Scholar]
- 22.Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018;18:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Broom A. Conceptualizing Qualitative Data. Qual Health Res 2021;31:1767–70. [DOI] [PubMed] [Google Scholar]
- 24.Durand-Moreau Q, Gautier A, Becouarn G, Topart P, Rodien P, Salle A. Employment and professional outcomes in 803 patients undergoing bariatric surgery in a French reference center for obesity. Int J Occup Environ Med 2015;6:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tarride JE, Breau R, Sharma AM, et al. The Effect of Bariatric Surgery on Mobility, Health-Related Quality of Life, Healthcare Resource Utilization, and Employment Status. Obes Surg 2017;27:349–56. [DOI] [PubMed] [Google Scholar]
- 26.Bramming M, Becker U, Jorgensen MB, Neermark S, Bisgaard T, Tolstrup JS. Bariatric Surgery and Risk of Unemployment and Sickness Absence. Obesity Surg 2022;32:720–8. [DOI] [PubMed] [Google Scholar]
- 27.Chao GF, Yang J, Thumma JR, et al. Out-of-pocket Costs for Commercially-insured Patients in the Years Following Bariatric Surgery: Sleeve Gastrectomy Versus Roux-en-Y Gastric Bypass. Ann Surg. 2021. Nov 11. doi: 10.1097/SLA.0000000000005291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahawar KK, Clare K, O'Kane M, Graham Y, Callejas-Diaz L, Carr WRJ. Patient Perspectives on Adherence with Micronutrient Supplementation After Bariatric Surgery. Obes Surg 2019;29:1551–6. [DOI] [PubMed] [Google Scholar]
- 29.Eisenberg D, Lohnberg JA, Kubat EP, Bates CC, Greenberg LM, Frayne SM. Systems innovation model: an integrated interdisciplinary team approach pre- and post-bariatric surgery at a veterans affairs (VA) medical center. Surg Obes Relat Dis 2017;13:600–6. [DOI] [PubMed] [Google Scholar]
- 30.Chao GF, Ehlers AP, Telem DA. Improving obesity treatment through telemedicine: increasing access to bariatric surgery. Surg Obes Relat Dis 2021;17:9–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Docimo S Jr., Seeras K, Acho R, Pryor A, Spaniolas K. Academic and community hernia center websites in the United States fail to meet healthcare literacy standards of readability. Hernia 2022. Mar 27. doi: 10.1007/s10029-022-02584-z. [DOI] [PubMed] [Google Scholar]
- 32.Miller-Matero LR, Hecht L, Patel S, Martens KM, Hamann A, Carlin AM. The Influence of Health Literacy and Health Numeracy on Weight Loss Outcomes Following Bariatric Surgery. Surg Obes Relat Dis 2021;17:384–9. [DOI] [PubMed] [Google Scholar]
- 33.Spreckley M, de Lange J, Seidell JC, Halberstadt J. Patient insights into the experience of trying to achieve weight-loss and future expectations upon commencement of a primary care-led weight management intervention: A qualitative, baseline exploration. PloS One 2022;17:e0270426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.