Abstract
Background
Small‐bore chest tube (SBCT) placement via modified Seldinger technique is a commonly performed invasive procedure for treatment of pleural effusion and pneumothorax. When performed suboptimally, it may lead to serious complications. Validated checklists are central to teaching and assessing procedural skills and may result in improved health care quality. In this paper, we describe the development and content validation of a SBCT placement checklist.
Methods
A literature review across multiple medical databases and seminal textbooks was performed to identify all publications describing procedural steps involved in SBCT placement. No studies were identified that involved systematic development of a checklist for this purpose. After the first iteration of a comprehensive checklist (CAPS) based on literature review was developed, the modified Delphi technique involving a panel of nine multidisciplinary experts was used to modify it and establish its content validity.
Results
After four Delphi rounds, the mean expert‐rated Likert score across all checklist items was 6.85 ± 0.68 (out of 7). The final, 31‐item checklist had a high internal consistency (Cronbach's alpha = 0.846) with 95% of the responses (by nine experts across 31 checklist items) being a numerical score of 6 or 7.
Conclusions
This study reports the development and content validity of a comprehensive checklist for teaching and assessing SBCT placement. For purposes of demonstrating construct validity, this checklist should next be studied in the simulation and clinical setting.
INTRODUCTION
The insertion of small‐bore chest tubes (SBCTs) involving the modified Seldinger technique is frequently performed by a variety of clinicians when treating pleural effusion, hemothorax, or pneumothorax. An SBCT may be the preferred type of chest tube in many of these instances because, compared to large‐bore chest tubes (LBCTs), SBCTs have been associated with less patient discomfort. 1 , 2 Furthermore, according to one meta‐analysis, SBCTs may also be associated with lower complication rates and shorter hospital length of stay in the setting of pneumothorax. 3
SBCTs can nevertheless lead to several complications, with rates estimated from 5% to 15%, 4 , 5 , 6 particularly in cases of suboptimal insertion technique. These include infection; hemothorax, pneumothorax, and parenchymal lung injury; and injury to other organs including heart, diaphragm, and abdominal organs. 7 SBCTs are also prone to clogging, kinking, and dislodgement, risks that may be mitigated through certain procedural techniques. 8 A root cause analysis of two chest tube–related complications identified lack of familiarity with the procedural steps as a key area of weakness and identified key steps that were more prone to operator error. 9 Other studies have also identified key procedural steps as being associated with either higher success rates (e.g., use of ultrasound) or lower complication rates (e.g., considerations when choosing the entry site). 10
The traditional paradigm of procedural skill teaching comprising “see one, do one, teach one” has largely been replaced with a competency‐based framework that incorporates skills attainment, deliberate practice, and directed feedback. Procedural checklists, besides being a useful resource for teaching and learner assessment, have been shown to improve quality of health care and reduce complications. Haynes et al. 11 demonstrated mortality reduction following the use of a surgical safety checklist in noncardiac surgery, while both Santos et al. 12 and See et al. 13 showed that standardization of procedural steps involved in bedside pleural procedures can lower the risk of major procedural complications.
Previously, a group from Australia developed the TUBE‐iCOMPT checklist for all chest tubes placed using either the modified Seldinger technique or blunt dissection. 14 To our knowledge, there have been no validated checklists specifically for the insertion of SBCTs using the modified Seldinger technique. In this study, we developed and established the content validity of a SBCT insertion checklist that employed the modified Seldinger technique.
METHODS
Study design and setting
This study was granted exemption by the Thomas Jefferson University's Institutional Review Board (IRB Control # 10 E.48). In this multistep study, we initially performed a thorough review of published literature, then developed an evidence‐based draft checklist, and subsequently established its content validity through systematic expert feedback using the modified Delphi process.
Definition of SBCT
For purposes of this study, we defined SBCT as a chest tube sized ≤14 French that is placed using the modified Seldinger method.
Literature search and initial checklist development
A librarian (ECO) performed a comprehensive search of all published English‐language articles between 1950 and February 17, 2020, that described procedural steps involved in SBCT placement. Databases searched included Embase, PubMed, Cochrane, and Scopus. Emtree terms included “drainage catheter,” “checklist,” and “protocol.” Medical Subject Headings (MeSH) terms “chest tubes” and “checklist” were used in combination with keywords including “pigtail catheter,” “chest tube,” “Seldinger chest tube,” and “small‐bore chest tube” as well as “technique,” “checklist,” “best practice,” “protocol,” and various synonyms.
The literature review yielded 641 references. Three authors (MS, RH, and JD) reviewed all titles and abstracts (when available) for possible inclusion. Publications were included if they described procedural steps involved in SBCT placement, either in a narrative format or in the form of a checklist. Twenty‐seven articles were selected and reviewed by the same authors for publication of a relevant checklist. The references of all obtained articles were reviewed for possible additional articles. Ultimately, 17 studies were utilized for checklist development (Figure 1). No studies were identified that described systematic development and validation of a checklist for SBCT.
FIGURE 1.
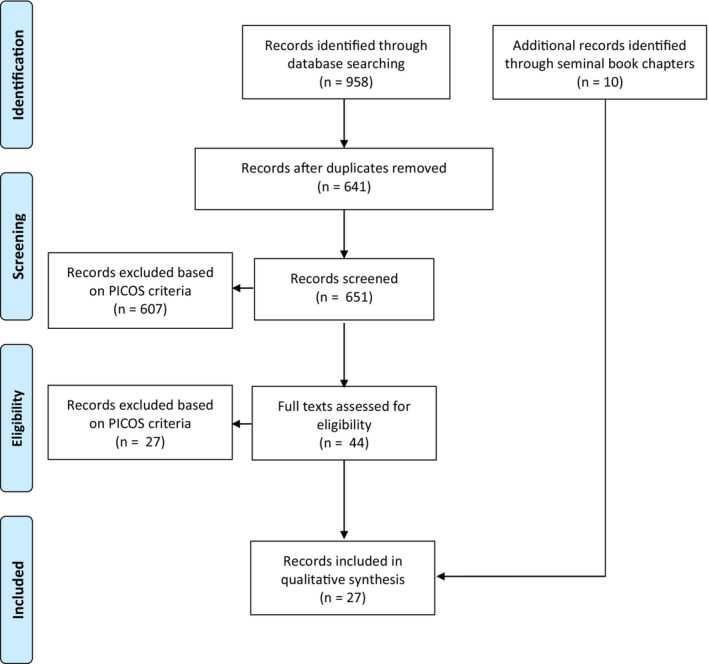
Process of identifying publications containing checklists or procedural steps used for SBCT placement. SBCT, small‐bore chest tube.
In addition, 10 seminal textbooks in the fields of medicine, surgery, emergency medicine, interventional pulmonology, thoracic surgery, and interventional radiology were reviewed for checklists or descriptions of procedural steps involved in SBCT placement (Appendix S1). Seminal textbooks were identified by the study investigators as most notable in their respective fields on a subjective basis.
Based on techniques described in the literature search results, the authors developed a 32‐item draft checklist, named Checklist for Assessing Placement of a SBCT (CAPS). Three authors (MS, RH, and JD) drafted the initial draft and presented it to the remainder of the study team, which reviewed and revised this draft for clarity.
Checklist validation using the modified Delphi process
The modified Delphi method, described in detail previously, was used to establish content validity of the SBCT insertion checklist. 15 Briefly, this entailed iterative consensus building among subject matter experts through multiple rounds of anonymized and pooled feedback on a series of draft checklists.
We identified nine experts in SBCT placement. Experts were nominated by the study investigators on the basis of their subjective reputation as strong clinicians in their fields with experience in performing and teaching this procedure. Experts were selected if they agreed to participate and met the a priori definition of “expert,” which entailed having performed or supervised >20 SBCT placements as an independent practitioner, including at least five within the preceding year. This threshold of 20 procedures was chosen in line with postgraduate training standards set for this procedure by a multisociety accreditation committee. 16 The nine experts represented diversity in specialty (interventional pulmonology, interventional radiology, emergency medicine, and thoracic surgery), institution/geographic location, and sex (Table 1). A diverse array of specialties was felt by the study investigators to be more likely in generating healthy debate and critique and less likely to result in confirmation bias as might be more likely among providers trained in the same way. The identities and specialties of other experts were kept confidential from each expert.
TABLE 1.
Baseline characteristics of Delphi experts.
| Reviewer | Area of clinical expertise | U.S. geographical region | Sex | Total SBCTs performed (lifetime) |
|---|---|---|---|---|
| 1 | Pulmonary and/or critical care | South | Male | 325 |
| 2 | Pulmonary and/or critical care | South | Female | 200 |
| 3 | Pulmonary and/or critical care | Midwest | Male | 200 |
| 4 | Pulmonary and/or critical care | West | Female | 500 |
| 5 | Emergency medicine | Northeast | Male | 25 |
| 6 | Emergency medicine | Northeast | Female | 45 |
| 7 | Thoracic surgery | Northeast | Male | 125 |
| 8 | Interventional radiology | Northeast | Male | 50 |
| 9 | Interventional radiology | Northeast | Male | 150 |
Abbreviation: SBCT, small‐bore chest tube.
Next, the draft checklist was presented to the group of independent experts. In Round 1, experts were individually invited to rate each checklist item on a 7‐point Likert‐type scale, where 1–3 represented “unimportant” steps, 4–6 represented “somewhat important” steps, and 7 represented a step that was mandatory for the procedure. Experts were allowed to insert free‐text comments wherever deemed appropriate.
Items receiving a mean of <4 were removed from the checklist. The checklist was modified by the authors based on the value and distribution of scores as well as any free‐text comments from the experts. The study team was blinded to the identity of the expert behind each comment; all communication with experts was performed by the Delphi checklist coordinator (JC) and all scores as well as comments were deidentified before presentation to the study team. Experts were blinded to each other's identity and did not get to view other scores or comments before submitting their own.
In subsequent Delphi rounds, the modified checklist was sent back to the same blinded experts for repeat review and feedback. This process was continued until there was consensus (defined as mean of >6 on the 7‐point scale) on all items, and there were no comments remaining unaddressed by the study team.
Statistical analysis
The average rating for each item was calculated using descriptive statistics. The internal consistency of the final checklist was determined using Cronbach's alpha. All statistics were performed using Microsoft Excel (Microsoft 365 Office version 2021).
RESULTS
The results of each Delphi round are illustrated in Table 2. In total, four Delphi rounds were carried out. Checklist items were added or modified based on aggregated Likert scores and in light of free‐text comments. Experts were also asked to vote on certain specific aspects. These included the exact timing of preprocedural timeout and whether to perform skin incision or guidewire insertion first. With regard to timeout, six (67%) felt that it should be done immediately after obtaining consent, two (22%) felt that it should be done after washing hands and before opening the kit, and one (11%) felt that it should be done immediately before first incision/needle insertion.
TABLE 2.
Results of each Delphi round.
| Item number | Delphi round 1 | Delphi round 2 | Delphi round 3 | Delphi round 4 | Final version of item | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean; median; SD | Modification | Mean; median; SD | Modification | Mean; median; SD | Modification | Mean; median; SD | Modification | ||
| 1. Obtains informed consent |
6.0 7.0 2.0 |
Added subtext: “Except in urgent cases” |
6.88 7.0 0.314 |
Modified to “May not be possible in emergent cases” |
6.77 7.0 0.682 |
N/A |
6.77 7.0 0.628 |
N/A | 1. Obtains informed consent
|
|
2. (Originally checklist item #3) Positions patient appropriately
|
6.55 7.0 0.831 |
Added to text: “in a supported manner” Cut from first subtext: “with arms resting on a table with a pillow” Cut from third subtext: “(with ipsilateral hand behind or above head if planning lateral approach)” Added fourth subtext: “Alternatively: supine oblique, as when performing procedure under CT guidance” |
6.88 7.0 0.314 |
Moved from Step #3 to Step #2 Modified first subtext to: “Sitting on edge of bed and leaning forward” |
6.88 7.0 0.314 |
N/A |
6.77 7.0 0.628 |
N/A | 2. Positions patient appropriately in a supported manner
|
|
3. (Originally checklist item #4) Inspects chest wall |
6.44 7.0 0.831 |
N/A |
6.33 7.0 1.56 |
Moved from Step #4 to Step #3 |
6.77 7.0 0.682 |
N/A |
6.55 7.0 0.831 |
N/A | 3. Inspects chest wall |
|
4B. (Originally checklist item #5) Identifies effusion or pneumothorax (as applicable) via ultrasound |
5.44 6.0 2.006 |
Added to text: “or CT” |
6.88 7.0 0.314 |
Moved from Step #5 to Step #4 |
7.0 7.0 0 |
Cut step from checklist |
(Cut from final checklist) Identifies effusion or pneumothorax (as applicable) via ultrasound or CT |
||
|
4. (Originally checklist item #6) Uses ultrasound as a guide to mark an appropriate site of entry
|
5.55 6.0 1.892 |
Modified to “Using ultrasound or CT as a guide, marks an appropriate site of entry” Cut “Ideally, an intercostal space one to two ribs below the upper level of fluid” |
6.44 7.0 0.955 |
Moved from Step #6 to Step #5 |
6.33 7.0 1.247 |
Moved from Step #5 to Step #4 Modified to “Using imaging (e.g., US or CT) as a guide …” |
6.44 7.0 1.571 |
N/A | 4. Using imaging (e.g., US or CT) as a guide, marks an appropriate site of entry |
|
5. (Originally checklist item #8) Opens kit |
6.22 7.0 1.872 |
N/A |
7.0 7.0 0 |
Moved from Step #8 to Step #6, before step “Washes hands” |
7.0 7.0 0 |
Moved from Step #6 to Step #5 |
7.0 7.0 0 |
N/A | 5. Opens kit |
|
6. (Originally checklist item #7) Washes hands |
6.22 7.0 1.872 |
N/A |
7.0 7.0 0 |
Swapped positioning to come after step “Opens kit” |
6.66 7.0 0.942 |
Moved from Step #7 to Step #6 |
6.66 7.0 0.942 |
N/A | 6. Washes hands |
|
7. (Originally checklist item #9) Applies cap, mask, sterile gown |
6.33 7.0 1.05 |
Modified to “Dons appropriate personal protective equipment” |
7.0 7.0 0 |
Moved from Step #9 to Step #8 |
6.77 7.0 0.682 |
Moved from Step #8 to Step #7 |
6.88 7.0 0.314 |
N/A | 7. Dons appropriate personal protective equipment |
|
8. (Originally checklist item #10) Applies sterile gloves |
6.66 7.0 0.942 |
N/A |
7.0 7.0 0 |
Moved from Step #10 to Step #9 |
7.0 7.0 0 |
Moved from Step #9 to Step #8 |
7.0 7.0 0 |
N/A | 8. Applies sterile gloves |
|
9. (Originally checklist item #11) Arranges material appropriately, including placing straightening catheter in pigtail |
6.11 7.0 1.286 |
N/A |
7.0 7.0 0 |
Moved from Step #11 to Step #10 Modified to “Arranges materials appropriately, including placing internal stiffener into pigtail catheter” |
6.88 7.0 0.314 |
Moved from Step #10 to Step #9 |
6.66 7.0 0.942 |
N/A | 9. Arranges materials appropriately, including placing internal stiffener into pigtail catheter |
|
10. (Originally checklist item #12) Preps over marked site and surrounding skin with chlorhexidine or appropriate alternative |
6.77 7.0 0.628 |
N/A |
7.0 7.0 0 |
Moved from Step #12 to Step #11 |
7.0 7.0 0 |
Moved from Step #11 to Step #10 |
7.0 7.0 0 |
N/A | 10. Preps over marked site and surrounding skin with chlorhexidine or appropriate alternative |
|
11. (Item did not exist in initial checklist) |
N/A | Created new item #13: “Applies sterile drape, leaving only the procedure site exposed” |
7.0 7.0 0 |
Moved from Step #13 to Step #12 |
6.88 7.0 0.314 |
Moved from Step #12 to Step #11 |
7.0 7.0 0 |
N/A | 11. Applies sterile drape, leaving only the procedure site exposed |
|
12. (Originally checklist item #2) Performs a preprocedure timeout immediately before procedure
|
6.77 7.0 0.628 |
Posed question to experts: “Should the step above (“time out”) be positioned as is or immediately after step 7 “Washes hands”? |
7.0 7.0 0 |
Moved from Step #2 to Step #13 Cut “doing procedure” Posed question to experts: “Should the step above (“time out”) be positioned as‐is? If not, after which step should it be placed?” |
7.0 7.0 0 |
Moved from Step #13 to Step #12 Modified to “verification of patient ID” Added text “(including laterality)” |
7.0 7.0 0 |
N/A | 12. Performs a preprocedure time out immediately before procedure
|
|
13. Reconfirms that puncture site is on the superior aspect of lower rib of the selected intercostal space
|
6.33 7.0 1.247 |
Moved from Step #13 to Step #14 |
6.44 7.0 0.955 |
Modified to “Confirms that the marked entry site is immediately above the lower rib bordering the selected intercostal space” |
6.22 7.0 1.314 |
Moved from Step #14 to Step #13 |
6.44 7 1.065 |
N/A | 13. Confirms that the marked entry site is immediately above the lower rib bordering the selected intercostal space |
14. Injects lidocaine at site of procedure
|
6.77 7.0 0.415 |
Moved from Step #14 to Step #15 |
7.0 7.0 0 |
Modified text to “Injects local anesthetic (for example, lidocaine) at the entry site” Modified subtext to three separate subtext points: “Using 25‐ to 22‐G needle, creates a superficial wheal” “Then injects deeper into skin, aspirating before each injection for evidence of blood or entry into pleura” “When pleural fluid or air is obtained, notes depth, and injects additional 2–3 mL of anesthetic to anesthetize the parietal pleura” |
6.66 7.0 0.942 |
Moved from Step #15 to Step #14 Changed subtext “injects additional 2–3 mL of anesthetic” to “injects additional anesthetic” |
7.0 7.0 0 |
Added to subtext point 3: “pulls back needle slightly” | 14. Injects local anesthetic (for example, lidocaine) at the entry site
|
15. After reconfirming position immediately above the rib, uses appropriate blade to make a superficial skin incision that is parallel to the rib
|
6.77 7.0 0.628 |
Moved from Step #15 to Step #16 |
7.0 7.0 0 |
Modified second subtext to “Keeps incision superficial, enabling entry of catheter through the epidermis without causing injury to deeper structures” |
6.66 7.0 0.942 |
Moved from Step #16 to Step #15 |
7.0 7.0 0 |
N/A | 15. After reconfirming positioning immediately above the rib, uses appropriate blade to make a superficial skin incision that is parallel to the rib
|
| 16. Attaches appropriate sized syringe to large hollow bore needle hub (typically, an 18‐G needle is used) and after reconfirming position immediately above the rib, introduces needle through the incision site |
6.22 7.0 1.474 |
Moved from Step #16 to Step #17 Added subtext “If using real‐time imaging guidance, use of a syringe may be omitted” |
6.66 7.0 0.94 |
Modified text to “Attaches appropriately sized syringe to the hub of a large hollow‐bore needle” |
6.66 7.0 0.942 |
Moved from Step #17 to Step #16 |
6.33 7.0 1.885 |
N/A | 16. Attaches appropriately sized syringe to the hub of a large hollow‐bore needle (typically, an 18‐G needle is used) and after reconfirming position immediately above the rib, introduces needle through the incision site
|
| 17. While inserting needle, continuously aspirates syringe to immediately recognize fluid or air return from pleural space |
6.0 7.0 2.0 |
Moved from Step #17 to Step #18 Added subtext “If using real‐time imaging guidance, this step may be omitted” |
6.66 7.0 0.94 |
N/A |
6.88 7.0 0.314 |
Moved from Step #18 to Step #17 |
7.0 7.0 0 |
N/A |
17. While inserting needle, continuously aspirates syringe in order to immediately recognize fluid or air return from pleural space
|
|
18. Removes syringe from needle hub while carefully maintaining position of needle
|
6.0 7.0 2.0 |
Moved from Step #18 to Step #19 Posed question to experts: “Should the subtext pertaining to ‘places gloved thumb over hub of needle’ be kept or removed?” Added subtext “If using real‐time imaging guidance, use of a syringe may be omitted” |
6.55 7.0 0.955 |
Cut subtext “Once syringe removed, places gloved thumb over hub of needle” |
7.0 7.0 0 |
Moved from Step #19 to Step #18 |
7.0 7.0 0 |
N/A | 18. Removes syringe from needle hub while carefully maintaining position of needle
|
|
19. Threads guidewire through hollow‐bore needle
|
6.44 7.0 1.065 |
Moved from Step #19 to Step #20 Modified first subtext to “The guidewire should be inserted at least several centimeters beyond the tip of the needle” Cut second subtext |
7.0 7.0 0 |
Modified text to “Threads guidewire through the hollow‐bore needle” Modified second subtext to “If resistance to guidewire insertion is encountered, stops and reconfirms placement of needle” |
7.0 7.0 0 |
Moved from Step #20 to Step #19 |
7.0 7.0 0 |
N/A | 19. Threads guidewire through the hollow‐bore needle
|
| 20. While continuously holding guidewire, removes hollow‐bore needle from site |
7.0 7.0 0 |
Moved from Step #20 to Step #21 |
7.0 7.0 0 |
Modified text to “While continuously holding guidewire, removes hollow‐bore needle” |
7.0 7.0 0 |
Moved from Step #21 to Step #20 |
7.0 7.0 0 |
N/A | 20. While continuously holding guidewire, removes hollow‐bore needle |
| 21. While continuously holding guidewire, inserts dilator with a clockwise/counterclockwise twisting motion over guidewire until an abrupt loss of resistance (i.e. “give”) is felt |
6.33 7.0 1.563 |
Moved from Step #21 to Step #22 Modified text to “While continuously holding guidewire, inserts dilator over guidewire until an abrupt loss of resistance (i.e. ‘give’) is felt.” Added subtext “Subsequently, using small back and forth movement (racking) of the guidewire, confirms that it is freely moving and not kinked.” |
6.55 7.0 0.955 |
Modified text to “While continuously holding guidewire, inserts dilator over guidewire” Added subtext “The appropriate depth of dilator placement may be determined using the previously noted depth in Step 15 and/or when an abrupt loss of resistance (i.e., ‘give’) is felt” |
6.88 7.0 0.314 |
Moved from Step #22 to Step #21 |
6.88 7.0 0.314 |
N/A | 21. While continuously holding guidewire, inserts dilator over guidewire
|
| 22. While continuously holding guidewire, removes dilator |
6.88 7.0 0.314 |
Moved from Step #22 to Step #23 |
6.88 7.0 0.314 |
N/A |
6.88 7.0 0.314 |
Moved from Step #23 to Step #22 |
6.88 7.0 0.314 |
N/A | 22. While continuously holding guidewire, removes dilator |
| 23. While continuously holding guidewire, inserts pigtail catheter (with straightening catheter in place) over the guidewire, stopping if any resistance is noticed |
6.88 7.0 0.314 |
Moved from Step #23 to Step #24 Added subtext “Keeps inserting until the tip is inside the pleura, then advances only the pigtail and not the straightening catheter” |
7.0 7.0 0 |
Modified text “straightening catheter” to “internal stiffener” Modified subtext “inserting” to “advancing” |
6.33 7.0 1.885 |
Moved from Step #24 to Step #23 |
7.0 7.0 0 |
N/A | 23. While continuously holding guidewire, inserts pigtail catheter (with internal stiffener in place) over the guidewire, stopping if any resistance is noticed.
|
| 24. Removes guidewire and straightening catheter together while placing finger/thumb tip over exposed hub |
6.875 7.0 0.330 |
Moved from Step #24 to Step #25 Modified text to “Removes the guidewire, and then, removes the straightening catheter” Posed question to experts: Should the text pertaining to “while placing finger/thumb tip over exposed hub” be kept or removed?” |
7.0 7.0 0 |
Modified text “straightening catheter” to “internal stiffener” |
7.0 7.0 0 |
Moved from Step #25 to Step #24 |
6.33 7.0 1.247 |
N/A | 24. Removes the guidewire and then removes the internal stiffener |
|
25. (Originally checklist item #26) Attaches catheter tubing to chest drain tubing and secures tightly via twisting motion.
|
7.0 7.0 0 |
Moved from Step #26 to Step #27 |
7.0 7.0 0 |
Moved from Step #27 to Step #26 |
7.0 7.0 0 |
Moved from Step #26 to Step #25 Modified first subtext “as desired” to “as appropriate” Added second subtext “Alternatively, attaches catheter tubing to a Heimlich valve” |
7.0 7.0 0 |
N/A | 25. Attaches catheter tubing to chest drain tubing and secures tightly via twisting motion.
|
|
26. (Originally checklist item #27) Secures chest tube in place using either a sterile suture or alternate device |
6.77 7.0 0.628 |
Moved from Step #27 to Step #28 |
6.66 7.0 0.666 |
Moved from Step #28 to Step #27 |
7.0 7.0 0 |
Moved from Step #27 to Step #26 |
7.0 7.0 0 |
N/A | 26. Secures chest tube in place using either a sterile suture or alternate device |
|
27. (Originally checklist item #25) Obtains a small amount of fluid for diagnostic workup if indicated, using the side/flushing port and a syringe (e.g., 60‐mL syringe) |
6.44 7.0 0.684 |
Moved from Step #25 to Step #26 Modified text to “Obtains fluid for diagnostic workup if indicated, using the side/flushing port (if available) and a syringe” Posed question to experts: “Should the above step take place as is, after the next step “Attaches catheter tubing to chest drain tubing and secures tightly via twisting motion,” OR after the following step: “Secures chest tube in place using either a sterile suture or alternate device?” |
6.66 7.0 0.942 |
Moved from Step #26 to Step #28 Modified text to “Obtains fluid for diagnostic workup if indicated, using the side/flushing port and a syringe (e.g., 60‐mL syringe)” |
7.0 7.0 0 |
Moved from Step #28 to Step #27 |
7.0 7.0 0 |
N/A | 27. Obtains fluid for diagnostic workup if indicated, using the side/flushing port and a syringe (e.g., 60‐mL syringe) |
| 28. Places a clear dressing over the catheter entry site |
6.22 6.0 0.785 |
Moved from Step #28 to Step #29 Modified to “Places a dressing over the catheter entry site” |
6.77 7.0 0.628 |
N/A |
6.88 7.0 0.314 |
Moved from Step #29 to Step #28 Modified to “Places a dressing at the catheter entry site” |
7.0 7.0 0 |
N/A | 28. Places a dressing at the catheter entry site |
|
28B. (Originally checklist item #29) Disposes of sharps appropriately |
6.88 7.0 0.314 |
Moved from Step #29 to Step #30 |
7.0 7.0 0 |
N/A |
7.0 7.0 0 |
Merged into item #29 “Cleans up” |
Merged into item #29 “Cleans up” (Disposes of sharps appropriately) |
||
|
29. (Originally checklist item #30) Cleans up |
6.22 7.0 1.872 |
Moved from Step #30 to Step #31 |
6.88 7.0 0.314 |
N/A |
6.33 7.0 1.885 |
Moved from Step #31 to Step #29 Added subtext “Disposes of sharps appropriately” |
7.0 7.0 0 |
N/A | 29. Cleans up
|
|
30. (Originally checklist item #31) Writes procedure note in appropriate space |
6.22 7.0 1.872 |
Moved from Step #31 to Step #32 |
7.0 7.0 0 |
Modified to “Writes procedure note” |
7.0 7.0 0 |
Moved from Step #32 to Step #30 |
6.77 7.0 0.628 |
N/A | 30. Writes procedure note |
|
31. (Originally checklist item #32) Orders a chest radiograph and interprets it |
5.88 7.0 1.852 |
Moved from Step #32 to Step #33 Modified to “Confirms appropriate catheter positioning via chest imaging” |
6.77 7.0 0.628 |
N/A |
7.0 7.0 0 |
Moved from Step #33 to Step #31 |
6.77 7.0 0.628 |
N/A | 31. Confirms appropriate catheter positioning via chest imaging |
Based on expert feedback, one item present in the original checklist (namely, identification of pleural effusion or pneumothorax via ultrasound or computed tomography [CT]) was removed from the final checklist to avoid redundancy; another item already referred to using ultrasound or CT to mark an appropriate site of entry. One other item (namely, sharps disposal) was merged into a preexisting separate item (namely, “cleans up”), whereas one item that was not present in the original version was added (namely, application of sterile drape following the skin prep).
In the first round of the Delphi process, the average score across all items was 6.42 ± 1.34. This increased to 6.85 ± 0.68 at the end of the fourth and last Delphi round. In the first round, 247 of 288 responses (by nine experts across 32 checklist items) were a numerical score of 6 or 7, representing 85.7% of all responses. This percentage increased to 94.9% in the fourth round. Furthermore, in line with our a priori benchmark, the percentage of checklist items receiving a mean score of >6 increased from 25/32 (78%) in round 1 to 31/31 (100%) in round 4. Following the fourth Delphi round, a consensus checklist was adopted by the author team with unanimous approval. This final, 31‐item checklist (Table 2 and Appendix S2) had high internal consistency (Cronbach's alpha = 0.846).
DISCUSSION
We present CAPS—a comprehensive checklist for insertion of SBCTs using the modified Seldinger technique—and hope that it will not only serve as a useful formative assessment tool to aid learner education and feedback but also provide a means for summative assessment of procedural competence. Through a rigorous process, we have established this checklist's high content validity, which indicates the completeness with which it encompasses all aspects of SBCT insertion. This provides a strong foundation for investigating the checklist's construct validity next, which would reflect its ability to accurately assess a subject's performance when inserting an SBCT.
Previously, a group from Australia developed the TUBE‐iCOMPT checklist for chest tube insertion. 14 The authors, evidently experts in chest tube insertion, developed this checklist for any chest tube placed using either the Seldinger technique (as is frequently done with SBCTs) or by blunt dissection (as more typical with LBCTs). To our knowledge, CAPS is the first procedural checklist on insertion of SBCTs using the modified Seldinger technique that was developed in a systematic, evidence‐based manner and subsequently validated through generation of blinded, multidisciplinary expert consensus using the modified Delphi technique.
Notably, during the content validation phase, we found that more than one Delphi round was required to achieve expert consensus on the various aspects of the CAPS checklist. These included the list of steps to follow, the specific details pertaining to each item, and the optimal sequence of steps required for sound conduct of this procedure.
One major item of debate was the timing of the procedural timeout. We respected the expert majority in developing the final checklist; however, we acknowledge that local or institutional protocols may vary in this aspect. The Joint Commission's Universal Protocol also leaves some room for interpretation by requiring that the timeout take place before starting the invasive procedure or making the incision. 17 In the operating room, a surgical timeout involves not just the surgeon but also the circulating nurse and other team members such as the anesthesiologist. There, the timeout is typically performed immediately before the surgeon makes the incision. A SBCT insertion, on the other hand, is more commonly performed outside of the operating room with a variable number of health care practitioners present in the room besides the proceduralist, if any at all. Therefore, depending on the urgency of the procedure and the availability of assistance, this timeout may potentially require some flexibility in terms of the specific timing (e.g., before the proceduralist washes their hands and dons sterile gloves). We suggest that, when administering this checklist, credit should be given for completing this task while allowing room for appropriate variability in terms of its exact timing.
Another variability in practice noted in our study was what qualified as appropriate personal protective equipment (PPE) for this procedure. This could conceivably vary depending on institutional policies. After the same was pointed out by the experts, we modified the checklist to include a more generic descriptor, “dons appropriate PPE.”
Similarly, expert consensus was to avoid prescribing an ideal site of entry relative to level of pleural fluid (i.e., one or two intercostal spaces below the upper level of fluid) as has been commonly prescribed for pleural fluid drainage. 18 Experts reported variable practice and lack of evidence to support such a recommendation. On the other hand, there was broad consensus on using imaging guidance as opposed to anatomic landmarks to choose the entry site, as is currently expected as the standard of care. 19 This was therefore incorporated into the final version of the checklist and would apply equally to all institutions, specialties, and practitioners.
Some experts recommended performing the scalpel incision prior to guidewire insertion; others noted that it could be performed after the guidewire was inserted. The rationale given for the former technique was to avoid accidentally cutting the guidewire. In the final Delphi round, there was broad consensus in favor of the former approach.
LIMITATIONS
This study has several limitations. Intrinsic bias among experts is possible. However, this possibility was minimized by presenting a literature‐based checklist as the starting instrument, selecting exerts from a wide range of institutions and across different specialties (Table 1) and using blinding during the modified Delphi process. While we did involve a diverse set of experts in terms of geography and training, it is possible that this checklist may not be generalizable to all settings. This checklist was designed keeping the novice learner in mind; experts may choose to depart from specific checklist items in certain situations. While this study demonstrates robust content validity of the new checklist, it does not inform the checklist's construct validity which would require further investigation involving subjects with varying levels of training and skill. Such a study would be expected to generate a cutoff (in terms of number of items correctly performed) correlating with each degree of performance or skill (e.g., novice, intermediate, expert, etc.). Finally, the feasibility of administering this 31‐item checklist (Appendix S2) would also require careful investigation, particularly at the bedside where the time it takes to be administered may have a greater bearing on its usability than in the simulation setting.
CONCLUSIONS
We report the first steps toward the development and validation of a comprehensive checklist for small‐bore chest tube insertion using the modified Seldinger technique. This checklist will likely be of use in formative training and summative assessment and as a quality improvement/quality assurance tool, though the same remains to be investigated. Our study provides content validity evidence for the checklist for assessing placement of a small‐bore chest tube checklist. Evidence of construct validity should be investigated next, including an examination of its performance in both simulated and real‐life clinical environments and its ability to discriminate proceduralists based on level of training and skill.
AUTHOR CONTRIBUTIONS
Majid Shafiq, Katherine Berg, Dale Berg, and Lee Ann Riesenberg conceived and designed the study. Majid Shafiq, Joshua Davis, Ronald Hall, Edward Jasper, and Emma C. O’Hagan were involved in literature review and initial development of the checklist. Majid Shafiq, Stefani Russo, Joshua Davis, Ronald Hall, Jared Calhoun, Edward Jasper, and Lee Ann Riesenberg were involved in checklist modification during the Delphi process. Majid Shafiq drafted the manuscript, and all authors contributed substantially to its revision. All authors take responsibility for the paper as a whole.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
Appendix S1:
Appendix S2:
ACKNOWLEDGMENTS
The authors thank all nine multidisciplinary experts for their indispensable participation in this project. The authors also thank Rosemarie Rippert for her administrative assistance during this project.
Shafiq M, Russo S, Davis J, et al. Development and content validation of the checklist for assessing placement of a small‐bore chest tube (CAPS) for small‐bore chest tube placement. AEM Educ Train. 2023;7:e10855. doi: 10.1002/aet2.10855
Accepted for presentation at the American Academy of Emergency Medicine's (AAEM) 29th Annual Scientific Assembly, New Orleans, LA, April 2023.
Supervising Editor: Dr. Victor Lee.
REFERENCES
- 1. Rahman NM, Pepperell J, Rehal S, et al. Effect of opioids vs NSAIDs and larger vs smaller chest tube size on pain control and pleurodesis efficacy among patients with malignant pleural effusion: the TIME1 randomized clinical trial. JAMA. 2015;314(24):2641‐2653. [DOI] [PubMed] [Google Scholar]
- 2. Kulvatunyou N, Erickson L, Vijayasekaran A, et al. Randomized clinical trial of pigtail catheter versus chest tube in injured patients with uncomplicated traumatic pneumothorax. Br J Surg. 2014;101(2):17‐22. [DOI] [PubMed] [Google Scholar]
- 3. Chang SH, Kang YN, Chiu HY, Chiu YH. A systematic review and meta‐analysis comparing pigtail catheter and chest tube as the initial treatment for pneumothorax. Chest. 2018;153(5):1201‐1212. [DOI] [PubMed] [Google Scholar]
- 4. Davies HE, Merchant S, McGown A. A study of the complications of small bore 'Seldinger' intercostal chest drains. Respirology. 2008;13(4):603‐607. [DOI] [PubMed] [Google Scholar]
- 5. Horsley A, Jones L, White J, Henry M. Efficacy and complications of small‐bore, wire‐guided chest drains. Chest. 2006;130(6):1857‐1863. [DOI] [PubMed] [Google Scholar]
- 6. Iepsen UW, Ringbæk T. Small‐bore chest tubes seem to perform better than larger tubes in treatment of spontaneous pneumothorax. Dan Med J. 2013;60(6):A4644. [PubMed] [Google Scholar]
- 7. Hallifax RJ, Psallidas I, Rahman NM. Chest drain size: the debate continues. Curr Pulmonol Rep. 2017;6(1):26‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Filosso PL, Sandri A, Guerrera F, et al. When size matters: changing opinion in the management of pleural space‐the rise of small‐bore pleural catheters. J Thorac Dis. 2016;8(7):E503‐E510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Broder JS, Al‐Jarani B, Lanan B, Brooks K. Pigtail catheter insertion error: root cause analysis and recommendations for patient safety. J Emerg Med. 2020;58(3):464‐472. [DOI] [PubMed] [Google Scholar]
- 10. Dammert P, Pratter M, Boujaoude Z. Safety of ultrasound‐guided small‐bore chest tube insertion in patients on clopidogrel. J Bronchol Interv Pulmonol. 2013;20(1):16‐20. [DOI] [PubMed] [Google Scholar]
- 11. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491‐499. [DOI] [PubMed] [Google Scholar]
- 12. Santos C, Gupta S, Baraket M, Collett PJ, Xuan W, Williamson JP. Outcomes of an initiative to improve inpatient safety of small bore thoracostomy tube insertion. Intern Med J. 2019;49(5):644‐649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. See KC, Jamil K, Chua AP, Phua J, Khoo KL, Lim TK. Effect of a pleural checklist on patient safety in the ultrasound era. Respirology. 2013;18(3):534‐539. [DOI] [PubMed] [Google Scholar]
- 14. Salamonsen MR, Bashirzadeh F, Ritchie AJ, Ward HE, Fielding DI. A new instrument to assess physician skill at chest tube insertion: the TUBE‐iCOMPT. Thorax. 2015;70(2):186‐188. [DOI] [PubMed] [Google Scholar]
- 15. Berg D, Berg K, Riesenberg LA, et al. The development of a validated checklist for thoracentesis: preliminary results. Am J Med Qual. 2013;28(3):220‐226. [DOI] [PubMed] [Google Scholar]
- 16. Mullon JJ, Burkart KM, Silvestri G, et al. Interventional pulmonology fellowship accreditation standards: executive summary of the Multisociety Interventional Pulmonology Fellowship Accreditation Committee. Chest. 2017;151(5):1114‐1121. [DOI] [PubMed] [Google Scholar]
- 17. Universal Protocol . The Joint Commission. Accessed February 26, 2022. https://www.jointcommission.org/standards/universal‐protocol/#93ad1844d85448d8ad293b4509ac61d7_2aad988d6aab4af59570a82a837d2215
- 18. Dezube R. How To Do Thoracentesis. Merck & Co., Inc. July 2022. Accessed February 26, 2022. https://www.merckmanuals.com/professional/pulmonary‐disorders/how‐to‐do‐pulmonary‐procedures/how‐to‐do‐thoracentesis [Google Scholar]
- 19. Havelock T, Teoh R, Laws D, Gleeson F. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65 Suppl 2:ii61‐ii76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1:
Appendix S2:


