Abstract
Canada and the USA are often compared for their markedly different approaches to health care despite cultural similarities and sharing the world’s longest international boundary. The period between the onset of the COVID-19 pandemic in January 2020 and the availability of a vaccine in December 2020 offers an ideal opportunity to compare subnational Canadian and American pandemic mortality. Preventing the spread of COVID-19 was through compliance with health orders and best practices; treatment was only available to those admitted to hospitals and whose lives were at risk. Using publicly available data from the Johns Hopkins University 2019 Novel Coronavirus Visual Dashboard, we seek to uncover if there were any similarities in Canadian provinces’ and American states’ monthly COVID-19 mortality per 100,000 people, building on a broader scientific push towards understanding the successes and failures of different health systems in the pandemic. The similar province and state cumulative COVID-19 mortality rate trajectories identified in our analyses do not amount to intuitive comparative jurisdictions which suggests the importance of identifying localized pandemic responses.
Keywords: Canada, COVID-19, Mortality, USA
Résumé
En dépit de leur proximité culturelle et de leur frontière commune, la plus longue au monde, les États-Unis et le Canada font souvent l’objet de comparaisons quant à leurs approches très différentes en matière de soins de santé. La période comprise entre le début de la pandémie de COVID-19 en janvier 2020 et la disponibilité d’un vaccin en décembre de la même année nous offre une occasion idéale de comparer la mortalité pandémique à l’échelle infranationale dans les deux pays. Au cours de cette période, la lutte contre la propagation de la COVID-19 s’est articulée autour du respect des ordonnances de santé et des pratiques exemplaires, les traitements n’étant réservés qu’aux personnes admises dans les hôpitaux dans un état critique. En utilisant les données du tableau de bord de la COVID-19 proposé par l’université John Hopkins, et en nous fondant sur une tendance scientifique plus large visant à comprendre les réussites et les échecs des différents systèmes de santé au cours de la pandémie, nous avons tenté de déceler des similitudes entre les provinces canadiennes et les états américains relativement au nombre de décès mensuel de la COVID-19 pour 100 000 habitants. Les trajectoires similaires des taux de mortalité cumulés liés à la COVID-19 dans les provinces et les états, observées dans nos analyses, ne constituent en aucun cas une comparaison intuitive entre les deux pays, ce qui souligne l’importance d’identifier les réponses locales à la pandémie.
Introduction
Canada and the USA are often compared for their markedly different approaches to health care despite cultural similarities and sharing the world’s longest international boundary (Blackwell et al., 2009; Pylypchuk & Sarpong, 2013; Sanmartin et al., 2006). The debate about whether health care is an inalienable public good—as in Canada—or more of a consumer choice—as in the US, in many ways, is innate to each country’s perspectives on social welfare and governance (Maioni, 2020; Quadagno, 2006; Raphael & Bryant, 2006; Ridic et al., 2012).
The COVID-19 pandemic laid bare the differences in public and private health care systems (Béland et al., 2021a, b; Combden et al., 2022; Unruh et al., 2022). Eight Canadian provinces’ COVID-19 responses were initially, and officially, led by medical doctors, except for Ontario and Quebec; 44 American states’ COVID-19 responses were run by governors or lay cabinet members except for Alabama, Hawaii, Indiana, Ohio, West Virginia, and Wyoming (authors’ analyses). Furthermore, in the early stages of the pandemic, Canada was among the world’s most successful countries in minimizing COVID-19 mortality while the USA was among the world’s least successful countries (Bilinski & Emanuel, 2020; Soneji et al., 2021). But the early and widespread availability of vaccines in late 2020 and through the spring of 2021 gave the USA a boost in its pandemic response because of its advantageous positioning in vaccine development and the supply chain (Wouters et al., 2021). Delays in receiving vaccines and the rise of the Delta variant led some under-resourced Canadian provincial health systems to effectively collapse—meaning that elective surgeries were cancelled, and intensive care units were unable to triage patients; pandemic management in Canada may not have been innately better than the USA simply due to universal health care access (McCullough, 2021). Until the pandemic is over, though, it will remain an open question—at the population level—as to whether private health care was more effective than public health care in combatting COVID-19.
While national trends are highly informative and crucial to evaluating the effectiveness of COVID-19 mitigation, there are rarely discussed, yet important, nuances in the subnational pandemic responses. Canadian provinces and US states have almost complete latitude to determine their public health policies and implementation strategies (Adeel et al., 2020); each country’s federal government can offer guidance and financial/logistical support, leading to fragmented policy under a national umbrella (Béland et al., 2021a, b). Thus, in both Canada and the USA, these secondary levels of jurisdiction offer ideal comparative groups. Given the markedly different national-level pandemic mortality rates, we examine whether there were any similarities between Canadian province and US state mortality, and, if so, to what extent and what can we ascertain?
The period between the onset of the COVID-19 pandemic in January 2020 and the availability of a vaccine in December 2020 offers an ideal opportunity to compare subnational Canadian and American pandemic mortality. All provinces and states started at zero COVID-19 deaths and without a vaccine or cure, as well as considerable autonomy in COVID-19 policy—an exceptional scenario for cross-border examination. We seek to uncover similarities in Canadian provinces’ and US states’ monthly COVID-19 mortality per 100,000 people, building on a broader scientific push towards understanding the successes and failures of different health systems in the pandemic.
Data and Methods
Within this brief report, we focus our efforts on each jurisdiction’s crude COVID-19 mortality rate—an imperfect marker of public health success, but the bedrock indicator of population health nonetheless (Etches et al., 2006). Our sources of Canadian and American COVID-19 mortality data are publicly available via the Johns Hopkins University 2019 Novel Coronavirus Visual Dashboard (Dong et al., 2020) operated by the Johns Hopkins University Center for Systems Science and Engineering (retrieved on April 9, 2021, from https://github.com/CSSEGISandData/COVID-19/tree/master/csse_covid_19_data/csse_covid_19_time_series). These data are a compilation of global and local sources of COVID-19 infection and deaths. They have also been updated as new and revised data become publicly available from vital statistics sources. Our analyses consist of descriptive comparisons of individual provincial versus state mortality. We included 6 of 10 Canadian provinces—Atlantic provinces formed a regional block with severe travel restrictions, leading to minimal COVID-19 mortality and thus incomparable to any US state or Canadian province. We also excluded Canada’s three territories—Yukon, Northwest Territories, and Nunavut—which are partially under federal control, and thus not sovereign like provinces (Cameron & White, 1995; Göcke, 2011; Marecic, 1999). We included all states in the contiguous US—the “Lower 48.” We excluded Hawaii and Alaska which were markedly different than other states as they were both only accessible to most Americans by airplane, with Hawaii also enacting a quarantine policy on arrival; the District of Columbia which is not fully under its own jurisdiction; and all US territories (such as Guam and Puerto Rico).
Our mortality indicators are (1) cumulative COVID-19 mortality by month per 100,000 and (2) non-cumulative monthly COVID-19 mortality per 100,000. The former measure is the additive number of COVID-19 deaths through the pandemic for each state or province then divided by the population and multiplied by 100,000; this measure provides an overall picture of which jurisdictions had the relatively highest and lowest mortality over time. The latter measure is the cumulative deaths at end of month minus the cumulative deaths at start of month then divided by the population and multiplied by 100,000 for each state or province; this measure provides an overall picture of how mortality changed monthly. To be conservative in our analyses, we included the small number of out-of-state deaths—potentially due to temporary migration, military service, or other possibilities—or deaths without specific dates within a month. To calculate these rates, population estimates for each province were incorporated, by our research team, into these data based on the 2016 Canadian Census (authors’ calculations; https://census.gc.ca/census-recensement/2016/index-eng.cfm) while each state’s population was already included in the JHU data via 2020 US census estimates.
In our results section, below, we present descriptive figures outlining select provincial and state cumulative and monthly COVID-19 mortality from January 2020 to the end of November 2020; provinces and states were chosen to show the most evident similarities. For visual simplicity, we only present data for the most similar provinces and states.
Results
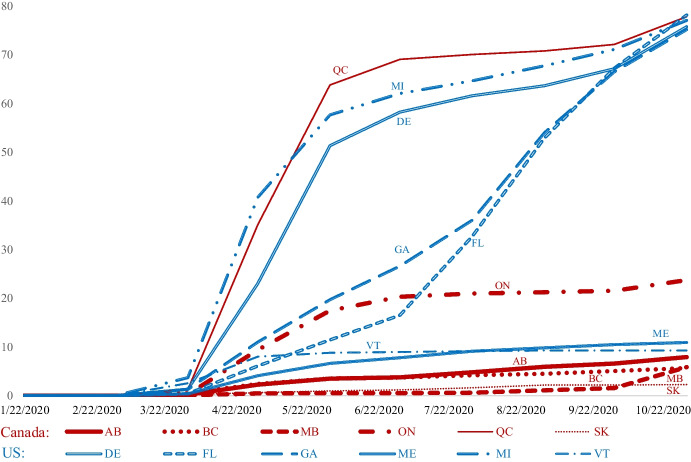
Figure 1, below, depicts the similarities between provinces and states for cumulative COVID-19 mortality by month per 100,000. Quebec (QC), like Michigan (MI) and Delaware (DE), experienced a sharp spike in mortality during the spring to early summer of 2020 followed by modest increases in mortality through November 2020; Georgia (GA) and Florida (FL) ended up with nearly identical cumulative COVID-19 mortality as Quebec but did not experience an initial spike. Ontario (ON) and Georgia had the same COVID-19 cumulative mortality trajectory in the late spring of 2020, but Ontario dramatically reduced the acceleration of its mortality rate, comparatively, by June. Vermont (VT) and Maine (ME) had the lowest cumulative COVID-19 mortality rates among all states and were comparable in their trajectories to Canada’s Western provinces of British Columbia (BC), Alberta (AB), Saskatchewan (SK), and Manitoba (MB).
Fig. 1.
Cumulative COVID-19 deaths per 100,000: January 1 to November 30, 2020
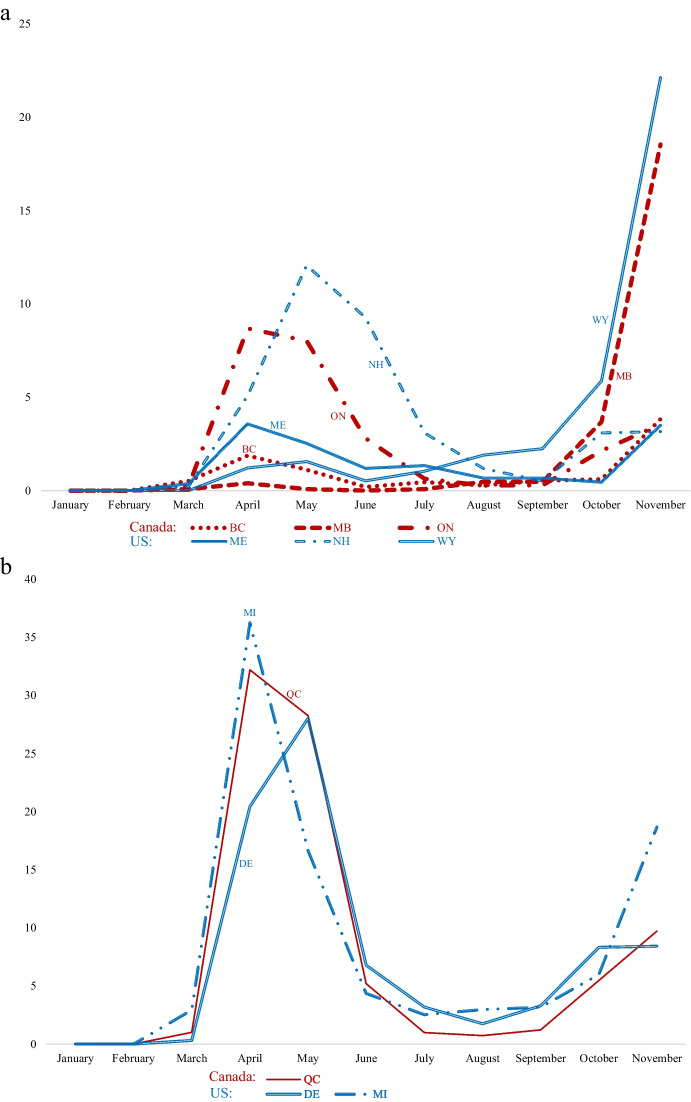
Figures 2a and b, below, depict the similarities between provinces and states for non-cumulative monthly COVID-19 mortality per 100,000. Most evidently, after months of consistently minimal mortality, it dramatically increased at nearly the same pace in October and November 2020 for Manitoba and Wyoming (WY). British Columbia and Maine managed to almost equally minimize COVID-19 mortality each month, only for both to experience a slight uptick in November 2020. After initially high rates of COVID-19 mortality in March, April, and May, Ontario and New Hampshire (NH) dramatically reduced their mortality rates over the summer until October 2020. Meanwhile, on a larger scale, Quebec, Michigan, and Delaware, once again tracked similarly in their monthly COVID-19 mortality rates—after steep increases in the spring of 2020, these jurisdictions experienced lower monthly mortality until early autumn, when it rose again.
Fig. 2.
a, b Non-cumulative monthly COVID-19 Deaths per 100,000: January 1 to November 30, 2020. Note: For visual clarity, the y-axis scale in Fig. 2b is different than the y-axis scale in Fig. 2a
Discussion
The similar provincial and state cumulative COVID-19 mortality rate trajectories shown here do not amount to intuitive comparative jurisdictions. Most provinces and states are dissimilar both in cumulative rates and monthly patterns of reductions in COVID-19 mortality, leading to the possibility, or perception, of randomness where similarities exist. For instance, Quebec had the same cumulative mortality rate—by November 2020—as Florida and Georgia, even though Quebec took comparatively extensive efforts to minimize COVID-19 prevention efforts; Florida had few statewide COVID-19 restrictions while Georgia limited local jurisdictions, like its largest city, Atlanta, to enact any public health measures that were more stringent than the lax ones at the state level. On the other end of the spectrum, Vermont and Maine—among the least populated and geographically small US states— had cumulative mortality rate paths akin to British Columbia and Alberta—two of Canada’s more populated, large provinces.
Identifying similarities in successes and failures between appropriate jurisdictional levels, via COVID-19 mortality, is an important macro-level step so that policymakers can see how their provincial or state responses to the pandemic stacked up against those in a different health system. A detailed policy-timeline analysis of similar provinces and jurisdictions would be a practical endeavor. Exploring the role of climate in COVID-19 prevention efforts might also be valuable (Chen et al., 2021): did the abilities of individuals in warmer, southern states, to spend more time outdoors in colder months create similar preventative circumstances as stricter COVID-19 policies in considerably colder northern states and provinces where people had to spend more time indoors? Explicitly factoring in population socio-demographic characteristics could also refine comparisons of Canadian and American health system’s successes in future work, given strong individual-level evidence of inequities in the pandemic (Czeisler et al., 2020; Etowa & Hyman, 2021; Hearne & Niño, 2022).
Of course, our research has its limitations. Due to space in this brief report format, we do not estimate excess mortality (McGrail, 2022) or case fatality, both of which are important to understanding national and subnational COVID-19 trends but require extensive estimating procedures and/or assumptions regarding the correct reporting of non-fatal cases (Rajgor et al., 2020; Wang et al., 2022). It is possible that the mortality patterns between provinces and states would look different. Additionally, we do not examine known COVID-19 infections in 2020, which could also add context to how provinces and states fared comparatively. Lastly, political meddling and/or lack of resources were widely known to contribute to varying data quality regarding COVID-19 infection and, potentially, mortality reporting; we do not systematically account for—nor are aware of a valid way to account for—differing levels of these measurement hindrances to get a clearer portrait of how health systems in provinces and states managed to limit mortality.
Conclusion
These mortality analyses importantly underscore the reality of an unexpected pandemic without widespread treatment and heavy reliance of citizens’ compliance with public health orders and best practices. With any luck, our research will encourage provincial and state health “autopsies” before the next novel coronavirus or infectious disease—without a known cure—inevitably emerges. At the very least, we hope that this research spurs more discussion of the costs and benefits of different types of medical systems between the two countries among those who can collectively make a difference. Elected officials, health care leaders, and implementation scientists have the capacity to investigate responses, learn from other systems, and engage with physicians, nurses, and the public to prepare for an even more robust response when the next major public health crisis occurs.
Acknowledgements
We would like to thank Erin Ware for critical comments on an early version of this paper and Emily Boyer for research assistance on Canada–USA differences in COVID-19 policies. We also appreciate being able to access this data repository for the 2019 Novel Coronavirus Visual Dashboard operated by the Johns Hopkins University Center for Systems Science and Engineering (JHU CSSE), also supported by ESRI Living Atlas Team and the Johns Hopkins University Applied Physics Lab (JHU APL).
Author Contribution
Tyler W. Myroniuk: conceptualization, original draft writing, revised draft writing, data analysis. Michelle Teti: conceptualization, revised draft writing. Enid Schatz: conceptualization, revised draft writing. Ifeolu David: conceptualization, revised draft writing.
Data Availability
Publicly available data sources are listed in the manuscript.
Declarations
Ethics Approval and Consent to Participate
N/A; not human subjects; public data.
Consent for Publication
N/A.
Competing Interests
The lead author, Tyler W. Myroniuk, is an editorial board member.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adeel AB, Catalano M, Catalano O, Gibson G, Muftuoglu E, Riggs T, Sezgin MH, Shvetsova O, Tahir N, VanDusky-Allen J, Zhao T, Zhirnov A. COVID-19 policy response and the rise of the sub-national governments. Canadian Public Policy. 2020;46(4):565–584. doi: 10.3138/cpp.2020-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Béland D, Dinan S, Rocco P, Waddan A. Social policy responses to COVID-19 in Canada and the United States: Explaining policy variations between two liberal welfare state regimes. Social Policy & Administration. 2021;55(2):280–294. doi: 10.1111/spol.12656. [DOI] [Google Scholar]
- Béland D, Marchildon GP, Medrano A, Rocco P. COVID-19, Federalism, and health care financing in Canada, the United States, and Mexico. Journal of Comparative Policy Analysis: Research and Practice. 2021;23(2):143–156. doi: 10.1080/13876988.2020.1848353. [DOI] [Google Scholar]
- Bilinski A, Emanuel EJ. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020;324(20):2100–2102. doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell DL, Martinez ME, Gentleman JF, Sanmartin C, Berthelot J-M. Socioeconomic status and utilization of health care services in Canada and the United States: Findings from a binational health survey. Medical Care. 2009;47(11):1136–1146. doi: 10.1097/MLR.0b013e3181adcbe9. [DOI] [PubMed] [Google Scholar]
- Cameron K, White G. Northern governments in transition: Political and constitutional development in the Yukon. Institute for Research on Public Policy; Distributed by Renouf Pub; 1995. [Google Scholar]
- Chen S, Prettner K, Kuhn M, Geldsetzer P, Wang C, Bärnighausen T, Bloom DE. Climate and the spread of COVID-19. Scientific Reports. 2021;11(1):9042. doi: 10.1038/s41598-021-87692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combden S, Forward A, Sarkar A. COVID-19 pandemic responses of Canada and United States in first 6 months: A comparative analysis. The International Journal of Health Planning and Management. 2022;37(1):50–65. doi: 10.1002/hpm.3323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler MÉ, Tynan MA, Howard ME, Honeycutt S, Fulmer EB, Kidder DP, Robbins R, Barger LK, Facer-Childs ER, Baldwin G, Rajaratnam SMW, Czeisler CA. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5–12, 2020. Morbidity and Mortality Weekly Report. 2020;69(24):751–758. doi: 10.15585/mmwr.mm6924e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etches V, Frank J, Ruggiero ED, Manuel D. Measuring population health: A review of indicators. Annual Review of Public Health. 2006;27(1):29–55. doi: 10.1146/annurev.publhealth.27.021405.102141. [DOI] [PubMed] [Google Scholar]
- Etowa J, Hyman I. Unpacking the health and social consequences of COVID-19 through a race, migration and gender lens. Canadian Journal of Public Health. 2021;112(1):8–11. doi: 10.17269/s41997-020-00456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Göcke K. Inuit self-government in the Canadian North: The next step in the Nunavut project. Zeitschrift Für Ausländisches Öffentliches Recht Und Völkerrecht. 2011;71(1):77–102. [Google Scholar]
- Hearne BN, Niño MD. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: Evidence from the COVID impact survey. Journal of Racial and Ethnic Health Disparities. 2022;9(1):176–183. doi: 10.1007/s40615-020-00941-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maioni A. Parting at the crossroads: The emergence of health insurance in the United States and Canada. Princeton University Press; 2020. [Google Scholar]
- Marecic CJ. Nunavut Territory: Aboriginal governing in the Canadian regime of governance. American Indian Law Review. 1999;24(2):275–295. doi: 10.2307/20070635. [DOI] [Google Scholar]
- McCullough, J. J. (2021). Opinion | What Alberta’s covid numbers tell us about the deficiencies of Canada’s health system. Washington Post. https://www.washingtonpost.com/opinions/2021/10/01/canada-alberta-covid-alabama-deficiencies-government-healthcare/. Accessed 3 Oct 2021
- McGrail K. Excess mortality, COVID-19 and health care systems in Canada. CMAJ. 2022;194(21):E741–E745. doi: 10.1503/cmaj.220337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pylypchuk Y, Sarpong EM. Comparison of health care utilization: United States versus Canada. Health Services Research. 2013;48(2pt1):560–581. doi: 10.1111/j.1475-6773.2012.01466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadagno J. One nation, uninsured: Why the U.S. has no national health insurance. Oxford University Press; 2006. [Google Scholar]
- Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. The Lancet Infectious Diseases. 2020;20(7):776–777. doi: 10.1016/S1473-3099(20)30244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael D, Bryant T. The state’s role in promoting population health: Public health concerns in Canada, USA, UK, and Sweden. Health Policy. 2006;78(1):39–55. doi: 10.1016/j.healthpol.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States, Germany and Canada. Materia Socio-Medica. 2012;24(2):112–120. doi: 10.5455/msm.2012.24.112-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanmartin C, Berthelot J-M, Ng E, Murphy K, Blackwell DL, Gentleman JF, Martinez ME, Simile CM. Comparing health and health care use in Canada and the United States. Health Affairs. 2006;25(4):1133–1142. doi: 10.1377/hlthaff.25.4.1133. [DOI] [PubMed] [Google Scholar]
- Soneji S, Beltrán-Sánchez H, Yang JW, Mann C. Population-level mortality burden from novel coronavirus (COVID-19) in Europe and North America. Genus. 2021;77(1):7. doi: 10.1186/s41118-021-00115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unruh L, Allin S, Marchildon G, Burke S, Barry S, Siersbaek R, Thomas S, Rajan S, Koval A, Alexander M, Merkur S, Webb E, Williams GA. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. 2022;126(5):427–437. doi: 10.1016/j.healthpol.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H., Paulson, K. R., Pease, S. A., Watson, S., Comfort, H., Zheng, P., Aravkin, A. Y., Bisignano, C., Barber, R. M., Alam, T., Fuller, J. E., May, E. A., Jones, D. P., Frisch, M. E., Abbafati, C., Adolph, C., Allorant, A., Amlag, J. O., Bang-Jensen, B., … Murray, C. J. L. (2022). Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–21. The Lancet, 399(10334), 1513–1536. 10.1016/S0140-6736(21)02796-3 [DOI] [PMC free article] [PubMed]
- Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. The Lancet. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available data sources are listed in the manuscript.