Abstract
Background:
The joint position sense (JPS) is an element of proprioception and defined as an individual’s ability to recognize joint position in space. The JPS is assessed by measuring the acuity of reproducing a predetermined target angle. The quality of psychometric properties of knee JPS tests after anterior cruciate ligament reconstruction (ACLR) is uncertain.
Purpose/Hypothesis:
The purpose of this study was to evaluate the test-retest reliability of a passive knee JPS test in patients who underwent ACLR. We hypothesized that the passive JPS test would produce reliable absolute error, constant error, and variable error estimates after ACLR.
Study Design:
Descriptive laboratory study.
Methods:
Nineteen male participants (mean age, 26.3 ± 4.4 years) who had undergone unilateral ACLR within the previous 12 months completed 2 sessions of bilateral passive knee JPS evaluation. JPS testing was conducted in both the flexion (starting angle, 0°) and the extension (starting angle, 90°) directions in the sitting position. The absolute error, constant error, and variable error of the JPS test in both directions were calculated at 2 target angles (30° and 60° of flexion) by using the angle reproduction method for the ipsilateral knee. The standard error of measurement (SEM), smallest real difference (SRD), and intraclass correlation coefficients (ICCs) with 95% Cis were calculated.
Results:
ICCs were higher for the JPS constant error (operated and nonoperated knee, 0.43-0.86 and 0.32-0.91, respectively) compared with the absolute error (0.18-0.59 and 0.09-0.86, respectively) and the variable error (0.07-0.63 and 0.09-0.73, respectively). The constant error of the 90°-60° extension test showed moderate to excellent reliability for the operated knee (ICC, 0.86 [95% CI, 0.64-0.94]; SEM, 1.63°; SRD, 4.53°), and good to excellent reliability for the nonoperated knee (ICC, 0.91 [95% CI, 0.76-0.96]; SEM, 1.53°; SRD, 4.24°).
Conclusion:
The test-retest reliability of the passive knee JPS tests after ACLR varied depending on the test angle, direction, and outcome measure (absolute error, constant error, or variable error). The constant error appeared to be a more reliable outcome measure than the absolute error and the variable error, mainly during the 90°-60° extension test.
Clinical Relevance:
As constant errors have been found reliable during the 90°-60° extension test, investigating these errors—in addition to absolute and variable errors—to reflect bias in passive JPS scores after ACLR is warranted.
Keywords: anterior cruciate ligament, joint position sense, proprioception, psychometric property, reliability
An anterior cruciate ligament (ACL) tear is a common devastating musculoskeletal injury, with an annual incidence rate of 68.6 isolated injuries per 100,000 person-years in the United States. 38 ACL injuries are managed either with rehabilitation alone or with surgery and rehabilitation. 37 However, approximately 20% of athletes who return to sport sustain a secondary ACL injury, regardless of management. 48
As with other knee joint structures (menisci, joint capsule, posterior cruciate and collateral ligaments, and surrounding tendons), 6,15 mechanoreceptors have been identified in the ACL, 1,13 suggesting a proprioceptive function for this ligament. 1 Proprioception is a term used to describe the sense of position and movement, as well as the sense of velocity, force, effort, and heaviness. 16,29,33 Proprioception plays a very important role, along with the other sensory systems, in executing motor tasks 16 throughout the process of anticipation (feedforward) before movement and reactive adaptation (feedback) during movement. 17,35
It is believed that ACL injury and ACL reconstruction (ACLR) affect knee proprioception, 20,34,43 which might be associated with knee instability, poor biomechanics, and impaired neuromuscular control, 8,9,18,29 and further contributing to an increased risk of reinjury and delayed return to play. 31 Therefore, addressing proprioception training during ACL rehabilitation and prevention programs may help to avoid these consequences. 7,8,10,18,29
The most commonly used submodalities to measure the sense of position and movement are joint position sense (JPS) and threshold to detect passive motion, respectively. 16,30,35,41,43 The JPS is defined as the individual’s ability to recognize joint position in space, 41 and it is assessed by measuring the acuity of reproducing a predetermined target angle. 20,35,41 Several variables can be manipulated to produce different protocols of knee JPS testing: (1) method of angle reproduction—active or passive; (2) direction of movement—extension or flexion; (3) demonstrating limb—ipsilateral or contralateral; (4) body position—lying, sitting, or standing; (5) measured range—starting angle and target angle; (6) weightbearing status—weightbearing or nonweightbearing; (7) testing instrument—eg, electrogoniometer or dynamometer; and (8) outcome measures—absolute error, constant error, or variable error. 16,43
There is a lack of consensus on which outcome measure to use while quantifying JPS acuity. The absolute error is the most commonly reported outcome measure in the literature. It provides the absolute amount of deviation of each reproduced angle from a target angle regardless of the direction of error and measures the overall performance accuracy. The constant error provides the amount and direction of deviation of each reproduced angle from a target angle and measures the performance bias (over- or undershooting the target angle). The variable error provides the difference between each reproduced angle and the individual’s mean error regardless of the score’s accuracy and measures the performance consistency. 39 Therefore, adding the constant error and the variable error to the commonly used absolute error when reporting the JPS error may augment the evaluation of an individual’s proprioceptive sense.
To quantify the JPS, clinicians must use clinical tools with a sufficient level of evidence to ensure their validity and reliability. The psychometric properties of JPS tests are not well-documented, 17 particularly after ACL injuries. 34,41,43 In their meta-analysis study in 2021, Strong et al 43 found a strong level of evidence, substantiating sufficient quality for known groups and discriminative validity of knee JPS tests, specifically the passive JPS tests. Nevertheless, they indicated an unknown level of evidence to substantiate the quality of other psychometric properties of knee JPS tests, including reliability. To our knowledge, only 2 studies have investigated the test-retest reliability of knee JPS tests (absolute error scores in the extension direction) in patients who underwent ACLR. 25,27 Both of these studies reported high test-retest reliability but had an “inadequate” risk-of-bias rating 43 based on their outcomes when using the COnsensus-based Standards for the Selection of health Measurement INstruments (COSMIN) risk of-bias checklist. 28
The purpose of this study was to evaluate the test-retest reliability of the absolute error, constant error, and variable error for a passive knee JPS test in the flexion and extension directions in patients after ACLR. It was hypothesized that these JPS tests would produce reliable absolute error, constant error, and variable error estimates in both directions after ACLR.
Methods
Study Design and Participant Recruitment
The study utilized a cross-sectional repeated-measures design. We adhered to the guidelines for reporting reliability and agreement studies 23 for designing and reporting this study. According to an a priori power analysis, we calculated that a minimum of 19 participants would be required to achieve an expected intraclass correlation coefficient (ICC) value of 0.9 and a minimal acceptable value of 0.7, with a 95% confidence interval (CI) for 2 times repeated test, given that α and β values were .05 and 0.20, respectively. 47 Thus, a convenience sample of 19 participants who were undergoing or had completed postoperative rehabilitation after ACLR was recruited between March and December 2021. Participants were active men aged between 21 and 35 years who had undergone a primary unilateral ACLR with a hamstring autograft during the past 12 months. Participants were excluded if they were within the first 3 months of postoperative rehabilitation; underwent a concomitant cartilage procedure and/or other ligament reconstruction; underwent other operations of the lower limbs within a year before the ACLR; and had knee pain, swelling, and/or fear of movement (indicated by a score of >37 on the Tampa Scale for Kinesiophobia 46 ) that prevented completion of the test. Ethical approval was obtained for the study protocol, and all participants signed a written informed consent before data collection.
Testing Procedure
The knee JPS was assessed using the Biodex system 4 dynamometer (Biodex Medical Systems). Criterion validity as well as trial-to-trial and day-to-day reliability of the Biodex dynamometer for position testing have demonstrated excellent correlations 11 (ICC, 0.99-1). A qualified male physical therapist (M.J.) assessed the participants’ eligibility, calibrated the dynamometer, provided a familiarization session, conducted the tests, and collected the data for both testing sessions for all participants.
At the time of recruitment, each eligible participant was evaluated to ensure their ability to participate in the study. Simultaneously, the participants’ characteristics and anthropometric data were collected. Further, other self-reported scores (numeric pain rating scale, 49 Tegner activity scale, 45 international knee documentation committee score, 36 and Tampa scale for kinesiophobia 22 ) were obtained to evaluate the participants’ self-perceived knee symptoms, 22,36,49 function, 36 and level of activity. 45 Thereafter, a familiarization session was conducted to demonstrate and explain the testing protocols to participants.
Two days after recruitment, each participant attended 2 testing sessions 5 days apart but at the same time of the day. Participants were asked to wear a blindfold to eliminate visual input during the tests and to wear shorts to avoid movement restriction. Participants were seated on the dynamometer chair, with their back supported on an 85° inclined back rest and the popliteal fossa placed approximately 5 cm from the chair, and the arms crossed on the chest. The thigh of the tested limb was secured to the chair by a strap. The dynamometer lever attachment was secured approximately 5 cm above the lateral malleolus. The dynamometer was calibrated according to the manufacturer’s guidelines.
The extension direction of the JPS test started by moving the participant’s knee passively by the physical therapist from the starting angle (90° of flexion) toward the target angle (30° of flexion or 60° of flexion, randomly ordered) (Figure 1, A-C). While the target angle was held for 5 seconds, 25,27 the participant was asked to memorize and remember this angle before the knee was returned to the same starting angle again passively by the physical therapist. Next, the dynamometer passively moved the knee toward extension at an angular velocity of 5 deg/s. 26 The participant was instructed to press the hold button when he felt that the target angle was reproduced (reproduced angle). Similarly, the flexion direction of the JPS test followed the same sequence, but the passive movements were from the starting angle (0° of flexion) toward the target angle (30° of flexion and 60° of flexion, randomly ordered) (Figure 1, D-F). Six trials 40 were repeated in an attempt to reproduce each target angle per direction, totaling 24 trials for each knee in each testing session. During each testing session, a random selection for the testing order—operated versus nonoperated limb; flexion versus extension direction; and 30° of flexion versus 60° of flexion target angle—was determined by using the Spin The Wheel–Random Picker mobile application (Version 2.5.9; Taurius Petraitis). Table 1 shows the details of the testing protocol.
Figure 1.
Top row: JPS test in extension. (A) Starting angle (90° of flexion). (B) Target angle (60° of flexion). (C) Target angle (30° of flexion). (B) and (C) were randomly ordered. Bottom row: JPS test in flexion. (D) Starting angle (0° of flexion). (E) Target angle (30° of flexion). (F) Target angle (60°of flexion). (E) and (F) were randomly ordered. JPS, joint position sense.
Table 1.
Variables of the Testing Protocol
| Variable | Protocol |
|---|---|
| Method of angle reproduction | Passive |
| Tested knee | Both operated and nonoperated |
| Weightbearing status | Nonweightbearing |
| Body position | Sitting |
| Testing instrument | Biodex dynamometer |
| Demonstrating limb | Ipsilateral |
| Direction of movement | Extension, flexion |
| Starting angle | 90° for extension, 0° for flexion |
| Target angles | 30° and 60°of flexion |
| Angular velocity | 5 deg/s |
| Memorization time for target angle | 5 s |
| No. of trials per target angle | 6 |
| No. of testing sessions | 2 |
| Time between sessions | 5 d |
| Outcome measures | Absolute error, constant error, and variable error |
Outcome Measures
The following formulas were used to calculate the mean absolute error and the mean constant error in flexion and extension, where RA is the reproduced angle, TA is the target angle, and n is the number of trials:
Variable error was calculated as follows:
where RAi is the score of the ith trial of interest and M is the mean reproduced angle of the complete set of trials. 39
Statistical Analysis
Data normality was tested using the Shapiro-Wilk test. The paired-samples t test was used to compare the results between both testing sessions. 3 Linear regression analyses were performed to assess proportional bias with the difference and mean of both tests used as dependent and independent variables, respectively. Test-retest reliability was judged with the ICC (3, k) (2-way mixed, average measure, absolute-agreement) in which the 95% CIs of the calculated ICCs were interpreted 21 as poor (<0.5), moderate (0.5 to <0.75), good (0.75 to <0.9), or excellent (0.9-1). The standard error of measurement (SEM) was calculated to quantify the measurement error using the following formula: SEM = SD×√(1-ICC), where SD is the mean standard deviation of both testing sessions. 3,5 The smallest real difference (SRD) measure was calculated to interpret the difference between the observed scores at 95% CI using the following formula: SRD95 = 1.96×SEM×√2. 4 All analyses were completed using SPSS (Version 21.0; IBM). The significance level was set at P < .05.
Results
Participant Characteristics
Nineteen male participants (mean age ± SD, 26.3 ± 4.4 years) completed both JPS testing sessions. The characteristics of these participants are provided in Table 2.
Table 2.
Participant Characteristics (N = 19 Male Participants) a
| Variable | Value |
|---|---|
| Age, mean ± SD, y | 26.3 ± 4.4 |
| BMI, mean ± SD, kg/m2 | 28.3 ± 4.6 |
| Operated limb, n (%) | |
| Dominant | 11 (58) |
| Nondominant | 8 (42) |
| Months between surgery and test, median (range) | 6.5 (3.1-11.2) |
| Self-reported rating scales, median (range) | |
| NPRS pain at rest b | 0 (0 -1) |
| NPRS pain worst b | 3 (1-7) |
| TAS c | 4 (3-7) |
| IKDC d | 72.4 (42.5-94.3) |
| TSK e | 25 (20-33) |
a BMI, body mass index; IKDC, International Knee Documentation Committee; NPRS, Numeric Pain Rating Scale; TAS, Tegner activity scale; TSK, Tampa Scale for Kinesiophobia.
b NPRS scores can range from 0 to 10, with higher scores indicating worse pain. 49
c TAS scores can range from 0 to 10, with higher scores indicating the ability to participate in more knee-demanding activities. 45
Test-Retest Reliability
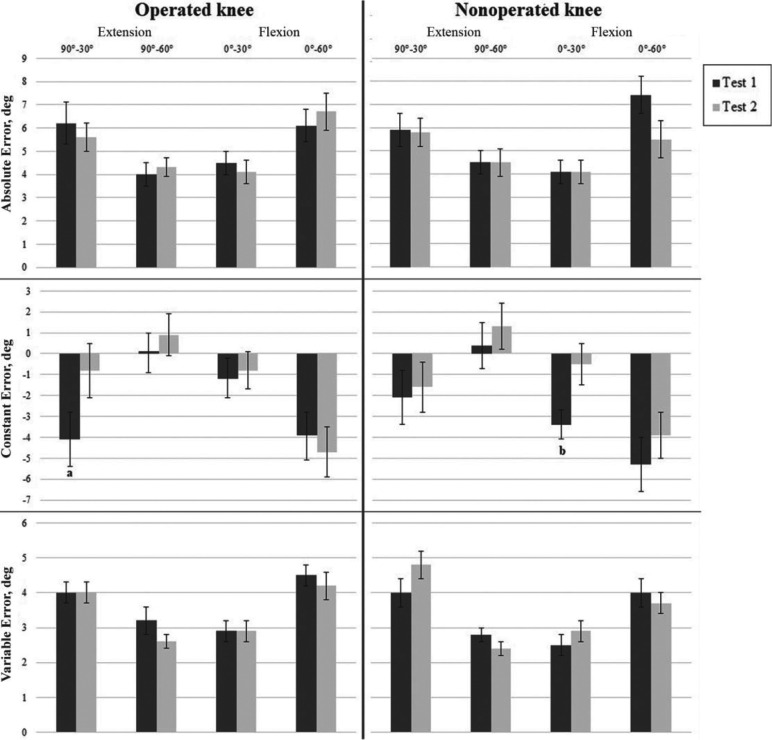
Figure 2 demonstrates the absolute error, constant error, and variable error scores of both JPS testing sessions. Regardless of the test angle and direction, the mean absolute error, constant error, and variable error scores for both tests were 5.2°, –1.8°, and 3.5°, respectively, for the operated knee and 5.2°, –1.9°, and 3.4°, respectively, for the nonoperated knee. Generally, participants had a tendency to undershoot the target angle in both knees, indicated by the negative constant error. A comparison between both tests revealed nonsignificant differences for absolute error and variable error scores, but only 2 constant error scores were found to be significantly greater in test 1 versus test 2: extension at 90°-30° in the operated knee (–4.1 ± 5.7 vs –0.8 ± 5.7, respectively; P = .048) and flexion at 0°-30° in the nonoperated knee (–3.4 ± 2.9 vs –0.5 ± 4.2, respectively; P = .005). Linear regression analyses showed no proportional bias for any of the scores obtained except for the variable error of the 90°-60° test in the operated knee (P = .009; β = 1.126).
Figure 2.
Comparison of the mean absolute error, constant error, and variable error between joint position sense tests 1 and 2 in the operated and nonoperated knees. Whiskers represent the SEM. a Significantly greater error in test 1 versus test 2 (P = .048). b Significantly greater error in test 1 versus test 2 (P = .005).
Reliability scores were in general higher for the constant error when compared with the absolute error and variable error. Looking at the 95% CIs, the constant error regarding the 90°-60° extension test showed moderate to excellent reliability for the operated knee (ICC, 0.86 [95% CI, 0.64-0.94]; SEM, 1.63°; SRD, 4.53°). The 90°-60° extension test was also more reliable for both the absolute error and constant error of the nonoperated knee, with moderate to excellent reliability for the absolute error (ICC, 0.86 [95% CI, 0.62-0.95]; SEM 0.94°; SRD, 2.60°), and good to excellent reliability for the constant error (ICC, 0.91 [95% CI, 0.76-0.96]; SEM, 1.53°; SRD, 4.24°). However, the 95% CIs for the absolute error, constant error, and variable error for almost all other target angles in either direction indicated poor to good reliability. Table 3 shows the ICCs and related values for the absolute error, constant error, and variable error.
Table 3.
ICC, SEM, and SRD Values for Absolute Error, Constant Error, and Variable Error of the JPS Test a
| Absolute Error | Constant Error | Variable Error | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ICC (95% CI) | SEM, deg | SRD, deg | ICC (95% CI) | SEM, deg | SRD, deg | ICC (95% CI) | SEM, deg | SRD, deg | |
| Operated knee | |||||||||
| Extension | |||||||||
| 90°-30° | 0.18 (0-0.69) | 2.98 | 8.27 | 0.43 (0-0.77) | 4.30 | 11.91 | 0.63 (0.02-0.86) | 0.77 | 2.12 |
| 90°-60° | 0.57 (0-0.83) | 1.32 | 3.65 | 0.86 (0.64-0.94) | 1.63 | 4.53 | 0.07 (0-0.64) | 1.27 | 3.51 |
| Flexion | |||||||||
| 0°-30° | 0.38 (0-0.77) | 1.71 | 4.75 | 0.80 (0.47-0.92) | 1.94 | 5.38 | 0.55 (0-0.83) | 0.93 | 2.58 |
| 0°-60° | 0.59 (0-0.84) | 2.01 | 5.56 | 0.53 (0-0.82) | 3.37 | 9.33 | 0.42 (0-0.78) | 1.22 | 3.39 |
| Nonoperated knee | |||||||||
| Extension | |||||||||
| 90°-30° | 0.09 (0-0.66) | 2.62 | 7.26 | 0.65 (0.06-0.87) | 3.25 | 9.01 | 0.73 (0.31-0.89) | 0.96 | 2.66 |
| 90°-60° | 0.86 (0.62-0.95) | 0.94 | 2.60 | 0.91 (0.76-0.96) | 1.53 | 4.24 | 0.12 (0-0.65) | 0.76 | 2.09 |
| Flexion | |||||||||
| 0°-30° | 0.29 (0-0.73) | 1.84 | 5.11 | 0.49 (0-0.79) | 2.56 | 7.09 | 0.28 (0-0.72) | 0.97 | 2.68 |
| 0°-60° | 0.35 (0-0.74) | 2.93 | 8.13 | 0.32 (0-0.74) | 4.33 | 11.99 | 0.09 (0-0.66) | 1.39 | 3.84 |
a Negative ICC values were replaced with zero. ICC, intraclass correlation coefficient; JPS, The joint position sense; SRD, smallest real difference.
Discussion
This study investigated the test-retest reliability of the absolute error, constant error, and variable error for passive knee JPS testing after ACLR. We found a wide range of ICCs, 95% CI, SEM, and SRD values depending on the knee JPS test angle, direction, and type of error (absolute error, constant error, or variable error). Nevertheless, ICCs were in general higher for the constant error compared with the absolute error and the variable error. Specifically, the constant error of the 90°-60° extension test showed moderate to excellent reliability for the operated knee (ICC, 0.86 [95% CI, 0.64-0.94]). The 90°-60° extension test also showed moderate to excellent reliability for the absolute error (ICC, 0.86 [95% CI, 0.62-0.95]), and good to excellent reliability for the constant error (ICC, 0.91 [95% CI, 0.76-0.96]) of the nonoperated knee.
Similar to our testing protocol, the other 2 studies that investigated test-retest reliability of the knee JPS tests after ACLR 25,27 used the same instrument (Biodex dynamometer), body position (sitting), and memorization time (5 seconds). In contrast, they evaluated JPS in the extension direction only. Also, both studies failed to report the time interval between the 2 testing sessions. Lee et al 25 employed the passive angle reproduction method of 1 target angle (45° knee flexion) starting from 90° knee flexion and repeated the procedure for 2 trials and demonstrated good reliability (ICC, 0.78). However, this study reported neither the angular velocity of the passive movement nor the 95% CI, SEM, and SRD values. Moezy et al 27 used the active angle reproduction method of 2 target angles (30° and 60° knee flexion) starting from 90° knee flexion and repeated the procedure for 5 trials per each target angle. For the operated knee, they reported good to excellent reliability during the 30° target angle (ICC 0.93 [95% CI 0.77-0.98, SEM 2.09°]) and excellent reliability during the 60° target angle (ICC 0.99 [95% CI 0.95-1.00, SEM 0.76°]). While for the nonoperated knee, they reported excellent reliability (ICC 0.99 [95% CI 0.95-1.00, SEM 1.33°] and 0.99 [95% CI 0.96-1.00, SEM 0.76°]) for both target angles (30° and 60°), respectively. . Therefore, variations in testing protocols and the lack of reporting of some important data help to explain the differences in reliability estimates when compared with our results. Moreover, comparisons of constant error and variable error estimates were precluded because both studies used absolute error as a single outcome measure when evaluating knee JPS.
The test-retest reliability of knee JPS tests has been studied in other pathological conditions than ACL injury. 12,24 However, comparable mixed reliability scores were provided, although the condition of interest and the testing protocols varied from our study. Fatoye et al 12 used a motorized device to evaluate knee JPS in a sitting position for children with hypermobility syndrome. They demonstrated poor to moderate reliability (ICC, 0.18-0.56) for the absolute error of passive angle reproduction tests of 2 target angles (10° and 25° of knee flexion) starting from 90° knee flexion. Kramer et al 24 reported moderate to good reliability (ICC, 0.58-0.79) and poor to moderate reliability (ICC, 0.42-0.63) of active angle reproduction tests, performed in sitting and standing positions, respectively, for patients with patellofemoral pain syndrome. In both positions, the absolute error was calculated by an electrogoniometer for the same target angles (15°, 30°, 45°, and 60° of flexion) starting from 75° of flexion during the sitting test as well as from full extension during the standing test.
Some authors investigated the test-retest reliability of knee JPS tests in healthy individuals. 32,44 In agreement with our results, they found varied ICC values despite the differences in the testing protocols. Olsson et al 32 found poor to good reliability scores (ICCs, 0.31-0.82 and 0.17-0.75) of active angle reproduction tests performed in sitting and prone positions, respectively. They used an electrogoniometer to calculate the absolute error for different target angles (in the sitting position: 30°, 50°, and 70° knee flexion; in the prone position: 40°, 70°, and 100° knee flexion) starting from 85° knee flexion in the sitting test and 15° knee flexion in the prone test. Similarly, Strong et al 44 reported mixed reliability scores of 2 novel active JPS tests performed in supine and standing positions. The authors used customized equipment and a motion capture system to calculate the absolute error, constant error, and variable error for 2 target angles (40° and 65°) starting from the knee extension position. During the supine test, they reported poor to excellent reliability for the absolute error (ICC 0.47 [95% CI 0.00-0.77] to 0.78 [95% CI 0.48-0.90]), and poor to good reliability for the variable error (ICC 0.00 [95% CI 0.00-0.54] to 0.64 [95% CI 0.14-0.85]). During the standing test, also they reported poor to excellent reliability for the absolute error (ICC 0.64 [95% CI 0.15-0.84] to 0.91 [95% CI 0.78-0.96]), and poor to good reliability for the variable error (ICC 0.24 [95% CI 0.00-0.67] to 0.65 [95% CI 0.22-0.85]). However, they did not report the reliability estimates of the constant error, which precludes comparisons with the corresponding reliability estimates of the passive JPS tests in our study.
In this study, we included men with Tegner scores 3 to 7 who had undergone ACLR in the previous 3 to 11 months to reflect a continuum of physical activity levels (light labor to certain competitive/recreational sports) and different stages of healing/recovery. Regardless of such differences, such a continuum would provide a wide range of knee JPS scores, which is desirable when investigating test-test reliability in the same patients using a repeated-measures design. The angular velocity used for passive JPS tests could determine the magnitude of errors; however, the present study aimed to assess the test-retest reliability of the observed values and not the magnitude of errors between limbs (operated vs nonoperated). The varied reliability scores in the present study can be attributed to the multiple angles, directions, and outcome measures that were utilized during the tests. Moreover, it is suggested that target angle memorization time affects knee JPS test reliability 42 ; thus, a longer memorization time for the target angle may allow more time for cognitive processing underlying the proprioception sense and may help to improve test reliability.
While a standardized method to evaluate knee JPS is yet to be ascertained, we used the passive angle reproduction method, as this method has previously been shown to discriminate between ACL-injured knees and asymptomatic knees to a greater extent than active JPS tests. 43 Additionally, because of the lack of consensus on which type of error to use as an outcome measure while quantifying knee JPS deficits, our study evaluated the absolute error, constant error, and variable error to comprehensively describe the patients’ proprioceptive performance in terms of accuracy (absolute error), bias (constant error), and consistency (variable error). To maintain consistency, only a male physical therapist conducted the testing protocol and assessed all participants. Because of the cultural barriers that prevent women from being assessed and tested by a male researcher for a research study in our study setting, only men were included in the study. Moreover, as our study included only young men with ACLR, the study findings may not be generalized to women, children, and older adults.
Finding a valid and reliable testing protocol for knee JPS assessment in patients with ACLR seems challenging, owing to the inconsistent testing procedures and the uncertain quality of the available research. 43,41 Also, some authors 14 have questioned the clinical relevance and ecological validity of quantifying knee JPS deficits because of their inconsistent correlations with functional outcomes after the surgery. Furthermore, they highlighted the need to develop new tests that may have the ability to value the significance of assessing the sensorimotor deficits after ACLR.
Conclusion
The test-retest reliability of passive knee JPS tests after ACLR ranged from poor to excellent depending on the test angle, direction, and outcome measure (absolute error, constant error, or variable error). The highest ICC values were generally evident for the JPS constant error, specifically the constant error of the 90°-60° extension test. Therefore, researchers need to be cautious while choosing passive JPS test parameters and related outcome measures (absolute error, constant error, and variable error). Future studies are warranted to ascertain standardized JPS tests and further investigate the psychometric properties of these tests after ACLR.
Acknowledgment
The authors thank Healthpoint Hospital for its assistance and support during this study.
Footnotes
Final revision submitted December 2, 2022; accepted December 13, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Institutional review board approval was obtained from Healthpoint Hospital (ref No. MF2467-2021-13).
References
References
- 1. Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–334. doi:10.1080/000164702320155356 [DOI] [PubMed] [Google Scholar]
References
- 2. Ahmed KM, Said HG, Ramadan EKA, Abd El-Radi M, El-Assal MA. Arabic translation and validation of three knee scores, Lysholm Knee Score (LKS), Oxford Knee Score (OKS), and International Knee Documentation Committee Subjective Knee Form (IKDC). SICOT J. 2019;5:6. doi:10.1051/sicotj/2018054 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 3. Atkinson G, Nevill AM. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26(4):217–238. doi:10.2165/00007256-199826040-00002 [DOI] [PubMed] [Google Scholar]
References
- 4. Beckerman H, Roebroeck ME, Lankhorst GJ, Becher JG, Bezemer PD, Verbeek ALM. Smallest real difference, a link between reproducibility and responsiveness. Qual Life Res. 2001;10(7):571–578. doi:10.1023/A:1013138911638 [DOI] [PubMed] [Google Scholar]
References
- 5. Bialocerkowski A, Klupp N, Bragge P. How to read and critically appraise a reliability article. Int J Ther Rehabil. 2010;17(3):114–120. doi:10.12968/ijtr.2010.17.3.46743 [Google Scholar]
References
- 6. Çabuk H, Kuşku Çabuk F. Mechanoreceptors of the ligaments and tendons around the knee. Clin Anat. 2016;29(6):789–795. doi:10.1002/CA.22743 [DOI] [PubMed] [Google Scholar]
References
- 7. Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res Sports Med. 2005;13(2):163–178. doi:10.1080/15438620590956197 [DOI] [PubMed] [Google Scholar]
References
- 8. Cronström A. Is poor proprioception associated with worse movement quality of the knee in individuals with anterior cruciate ligament deficiency or reconstruction? J Phys Ther Sci. 2018;30(10):1278–1283. doi:10.1589/jpts.30.1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 9. Dhillon MS, Kamal B, Prabhakar S. Differences among mechanoreceptors in healthy and injured anterior cruciate ligaments and their clinical importance. Muscles Ligaments Tendons J. 2012;2(1):38–43. [PMC free article] [PubMed] [Google Scholar]
References
- 10. Donnell-Fink LA, Klara K, Collins JE, et al. Effectiveness of knee injury and anterior cruciate ligament tear prevention programs: a meta-analysis. PLoS One. 2015;10(12):e0144063. doi:10.1371/journal.pone.0144063 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 11. Drouin JM, Valovich-McLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91(1):22–29. doi:10.1007/s00421-003-0933-0 [DOI] [PubMed] [Google Scholar]
References
- 12. Fatoye FA, Palmer ST, Macmillan F, Rowe PJ, van der Linden ML. Repeatability of joint proprioception and muscle torque assessment in healthy children and in children diagnosed with hypermobility syndrome. Musculoskelet Care. 2008;6(2):108–123. doi:10.1002/msc [DOI] [PubMed] [Google Scholar]
References
- 13. Gao F, Zhou J, He C, et al. A morphologic and quantitative study of mechanoreceptors in the remnant stump of the human anterior cruciate ligament. Arthroscopy. 2016;32(2):273–280. doi:10.1016/j.arthro.2015.07.010 [DOI] [PubMed] [Google Scholar]
References
- 14. Gokeler A, Benjaminse A, Hewett TE, et al. Proprioceptive deficits after ACL injury: are they clinically relevant? Br J Sports Med. 2012;46(3):180–192. doi:10.1136/bjsm.2010.082578 [DOI] [PubMed] [Google Scholar]
References
- 15. Gray JC. Neural and vascular anatomy of the menisci of the human knee. J Orthop Sports Phys Ther. 1999;29(1):23–30. doi:10.2519/jospt.1999.29.1.23 [DOI] [PubMed] [Google Scholar]
References
- 16. Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: a critical review of methods. J Sport Health Sci. 2016;5(1):80–90. doi:10.1016/j.jshs.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 17. Hillier S, Immink M, Thewlis D. Assessing proprioception: a systematic review of possibilities. Neurorehabil Neural Repair. 2015;29(10):933–949. doi:10.1177/1545968315573055 [DOI] [PubMed] [Google Scholar]
References
- 18. Jerosch J, Prymka M. Proprioception and joint stability. Knee Surg Sports Traumatol Arthrosc. 1996;4(3):171–179. doi:10.1007/BF01577413 [DOI] [PubMed] [Google Scholar]
References
- 19. Juweid M, Farah K, Hawamdeh Z, et al. Fear of movement/[re]injury among Arabic low back pain patients: establishing the validity of the Tampa Scale of Kinesiophobia–Arabic version. Myopain. 2015;23(3-4):134–142. doi:10.1080/24708593.2017.1303014 [Google Scholar]
References
- 20. Kim HJ, Lee JH, Lee DH. Proprioception in patients with anterior cruciate ligament tears: a meta-analysis comparing injured and uninjured limbs. Am J Sports Med. 2017;45(12):2916–2922. doi:10.1177/0363546516682231 [DOI] [PubMed] [Google Scholar]
References
- 21. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 22. Kori S, Miller R, Todd D. Kinesiophobia: a new view of chronic pain behavior. Pain Manag. 1990;3:35–43. [Google Scholar]
References
- 23. Kottner J, Audige L, Brorson S, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. Int J Nurs Stud. 2011;48(6):661–671. doi:10.1016/j.ijnurstu.2011.01.016 [DOI] [PubMed] [Google Scholar]
References
- 24. Kramer J, Handfield T, Kiefer G, Forwell L, Birmingham T. Comparisons of weight-bearing and non-weight-bearing tests of knee proprioception performed by patients with patello-femoral pain syndrome and asymptomatic individuals. Clin J Sport Med. 1997;7(2):113–118. doi:10.1097/00042752-199704000-00007 [DOI] [PubMed] [Google Scholar]
References
- 25. Lee DH, Lee JH, Ahn SE, Park MJ. Effect of time after anterior cruciate ligament tears on proprioception and postural stability. PLoS One. 2015;10(9):e0139038. doi:10.1371/journal.pone.0139038 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 26. Li L, Ji ZQ, Li YX, Liu WT. Correlation study of knee joint proprioception test results using common test methods. J Phys Ther Sci. 2016;28(2):478–482. doi:10.1589/jpts.28.478 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 27. Moezy A, Olyaei G, Hadian M, Razi M, Faghihzadeh S. A comparative study of whole body vibration training and conventional training on knee proprioception and postural stability after anterior cruciate ligament reconstruction. Br J Sports Med. 2008;42(5):373–378. doi:10.1136/bjsm.2007.038554 [DOI] [PubMed] [Google Scholar]
References
- 28. Mokkink LB, de Vet HCW, Prinsen CAC, et al. COSMIN Risk of Bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1171–1179. doi:10.1007/s11136-017-1765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 29. Nagai T, Allison KF, Schmitz JL, Sell TC, Lephart SM. Sports Medicine: Conscious proprioception assessments in sports medicine: How individuals perform each submodality?. Dover DE: SM Group Ebooks; 2016. Accessed November 29, 2020. http://www.smgebooks.com/sports-medicine/chapters/SMD-16-04.pdf. [Google Scholar]
- 30. Nagai T, Schilaty ND, Strauss JD, Crowley EM, Hewett TE. Analysis of lower extremity proprioception for anterior cruciate ligament injury prevention: current opinion. Sports Med. 2018;48(6):1303–1309. doi:10.1007/s40279-018-0889-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 31. Nagelli C V, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47(2):221–232. doi:10.1007/s40279-016-0584-z [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 32. Olsson L, Lund H, Henriksen M, Rogind H, Bliddal H, Danneskiold-Samsøe B. Test-retest reliability of a knee joint position sense measurement method in sitting and prone position. Adv Physiother. 2004;6(1):37–47. doi:10.1080/14038190310009894 [Google Scholar]
References
- 33. Proske U, Gandevia SC. The proprioceptive senses: their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev. 2012;92(4):1651–1697. doi:10.1152/physrev.00048.2011 [DOI] [PubMed] [Google Scholar]
References
- 34. Relph N, Herrington L, Tyson S. The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy. 2014;100(3):187–195. doi:10.1016/j.physio.2013.11.002 [DOI] [PubMed] [Google Scholar]
References
- 35. Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: basic science and principles of assessment and clinical interventions. Man Ther. 2015;20(3):368–377. doi:10.1016/j.math.2015.01.008 [DOI] [PubMed] [Google Scholar]
References
- 36. Rossi MJ, Lubowitz JH, Guttmann D. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2002;30(1):152. doi:10.1177/03635465020300011301 [DOI] [PubMed] [Google Scholar]
References
- 37. Sanders JO, Brown GA, Murray J, Pezold R, Sevarino KS. Treatment of anterior cruciate ligament injuries. J Am Acad Orthop Surg. 2016;24(8):e81–e83. doi:10.5435/JAAOS-D-16-00154 [DOI] [PubMed] [Google Scholar]
References
- 38. Sanders T, Maradit Kremers H, Bryan A, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. doi:10.1177/0363546516629944 [DOI] [PubMed] [Google Scholar]
References
- 39. Schmidt R, Lee T. Motor Control and Learning: A Behavioral Emphasis. 5th ed. Human Kinetics ; 2011. [Google Scholar]
References
- 40. Selfe J, Callaghan M, McHenry A, Richards J, Oldham J. An investigation into the effect of number of trials during proprioceptive testing in patients with patellofemoral pain syndrome. J Orthop Res. 2006;24(6):1218–1224. doi:10.1002/jor.20127 [DOI] [PubMed] [Google Scholar]
References
- 41. Smith TO, Davies L, Hing CB. A systematic review to determine the reliability of knee joint position sense assessment measures. Knee. 2013;20(3):162–169. doi:10.1016/j.knee.2012.06.010 [DOI] [PubMed] [Google Scholar]
References
- 42. Springer S, Kelman D, Brand M, Gottlieb U. Knee position sense: does the time interval at the target angle affect position accuracy? J Phys Ther Sci. 2017;29(10):1760–1765. doi:10.1589/jpts.29.1760 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 43. Strong A, Arumugam A, Tengman E, Röijezon U, Häger CK. Properties of knee joint position sense tests for anterior cruciate ligament injury: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(6):23259671211007878. doi:10.1177/23259671211007878 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 44. Strong A, Srinivasan D, Häger CK. Development of supine and standing knee joint position sense tests. Phys Ther Sport. 2021;49:112–121. doi:10.1016/j.ptsp.2021.02.010 [DOI] [PubMed] [Google Scholar]
References
- 45. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res.1985;198:43–49. [PubMed] [Google Scholar]
References
- 46. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62(3):363–372. doi:10.1016/0304-3959(94)00279-N [DOI] [PubMed] [Google Scholar]
References
- 47. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–110. doi:10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.0.CO;2-E [DOI] [PubMed] [Google Scholar]
References
- 48. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. doi:10.1177/0363546515621554 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 49. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi:10.1111/j.1365-2702.2005.01121.x [DOI] [PubMed] [Google Scholar]