Key Points
Question
What is the prevalence of statin use for primary prevention of atherosclerotic cardiovascular disease (ASCVD) by race and ethnicity according to 10-year risk of ASCVD?
Findings
In this cross-sectional analysis of the National Health and Nutrition Examination Surveys representing 39.4 million US adults, Black and Hispanic participants had significantly lower statin use than White participants. Having health insurance or a routine location for health care were significantly associated with increased statin use across race and ethnicity groups.
Meaning
The findings in this study indicate that racial and ethnic disparities in the use of statins for primary prevention across all strata of ASCVD risk are associated with poor access to care among individuals of self-reported Black and Hispanic race and ethnicity.
This cross-sectional study evaluates statin use for primary prevention of atherosclerotic cardiovascular disease in the US by 10-year risk and by race and ethnicity.
Abstract
Importance
The burden of atherosclerotic cardiovascular disease (ASCVD) in the US is higher among Black and Hispanic vs White adults. Inclusion of race in guidance for statin indication may lead to decreased disparities in statin use.
Objective
To evaluate prevalence of primary prevention statin use by race and ethnicity according to 10-year ASCVD risk.
Design, Setting, and Participants
This serial, cross-sectional analysis performed in May 2022 used data from the National Health and Nutrition Examination Survey, a nationally representative sample of health status in the US, from 2013 to March 2020 (limited cycle due to the COVID-19 pandemic), to evaluate statin use for primary prevention of ASCVD and to estimate 10-year ASCVD risk. Participants aged 40 to 75 years without ASCVD, diabetes, low-density lipoprotein cholesterol levels 190 mg/dL or greater, and with data on medication use were included.
Exposures
Self-identified race and ethnicity (Asian, Black, Hispanic, and White) and 10-year ASCVD risk category (5%-<7.5%, 7.5%-<20%, ≥20%).
Main Outcomes and Measures
Prevalence of statin use, defined as identification of statin use on pill bottle review.
Results
A total of 3417 participants representing 39.4 million US adults after applying sampling weights (mean [SD] age, 61.8 [8.0] years; 1289 women [weighted percentage, 37.8%] and 2128 men [weighted percentage, 62.2%]; 329 Asian [weighted percentage, 4.2%], 1032 Black [weighted percentage, 12.7%], 786 Hispanic [weighted percentage, 10.1%], and 1270 White [weighted percentage, 73.0%]) were included. Compared with White participants, statin use was lower in Black and Hispanic participants and comparable among Asian participants in the overall cohort (Asian, 25.5%; Black, 20.0%; Hispanic, 15.4%; White, 27.9%) and within ASCVD risk strata. Within each race and ethnicity group, a graded increase in statin use was observed across increasing ASCVD risk strata. Statin use was low in the highest risk stratum overall with significantly lower rates of use among Black (23.8%; prevalence ratio [PR], 0.90; 95% CI, 0.82-0.98 vs White) and Hispanic participants (23.9%; PR, 0.90; 95% CI, 0.81-0.99 vs White). Among other factors, routine health care access and health insurance were significantly associated with higher statin use in Black, Hispanic, and White adults. Prevalence of statin use did not meaningfully change over time by race and ethnicity or by ASCVD risk stratum.
Conclusions and Relevance
In this study, statin use for primary prevention of ASCVD was low among all race and ethnicity groups regardless of ASCVD risk, with the lowest use occurring among Black and Hispanic adults. Improvements in access to care may promote equitable use of primary prevention statins in Black and Hispanic adults.
Introduction
Statins have been shown to be safe and effective in the prevention of atherosclerotic cardiovascular disease (ASCVD),1 which is the leading cause of death among US adults.2 ASCVD and lack of access to cardiology specialists disproportionately affects non-Hispanic Black (hereafter, Black) and Hispanic adults compared to non-Hispanic White (hereafter, White) adults.2,3 For primary prevention of ASCVD, the 2018 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Management of Blood Cholesterol1 recommends statin treatment among those with diabetes, low-density lipoprotein cholesterol (LDL-C) values (190 mg/dL or greater; to convert millimoles per liter, multiply by 0.0259), or 10-year predicted ASCVD risk of 5% to less than 20% with risk enhancers or 20% or greater regardless of risk enhancers. The ACC and AHA endorse the use of pooled cohort equations (PCE) to calculate 10-year predicted ASCVD risk using age, sex, blood pressure, cholesterol, diabetes, smoking status, hypertension treatment, and race and ethnicity parameters.1,4 The use of PCE to guide statin initiation for primary prevention was first introduced in the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol.4 The PCE model includes Black race as consideration, showing higher risk of ASCVD in Black vs non-Black individuals with identical profiles.5 Thus, the PCE-guided approach to statin initiation for primary prevention should promote greater use of statins for primary prevention among Black individuals.6,7
Prior reports demonstrate racial disparities in underuse of statins for secondary prevention among Black and Hispanic patients.8,9 Studies evaluating statin use in primary prevention populations have been limited to single centers or diabetes-only cohorts or do not include temporal trends or current 10-year ASCVD risk categorization.10,11 National-level patterns and temporal trends in statin use for the broader primary prevention population across racial and ethnic groups are not known. This is particularly relevant considering the growing burden of ASCVD and worsening racial disparities in cardiovascular health factors.12,13 To quantify these gaps, we evaluated prevalence of statin use for primary prevention of ASCVD by race and ethnicity according to PCE-predicted 10-year ASCVD risk strata among participants in the National Health and Nutrition Examination Survey (NHANES), a nationally representative sample of health status in the US, between January 2013 and March 2020.
Methods
Data Source and Study Population
The protocols, methodology, and data for NHANES are publicly available.14 Briefly, the National Center for Health Statistics of the US Centers for Disease Control and Prevention surveys participants identified in the US via a stratified multistage probability sampling design.15 These 2-year cross-sectional surveys can be combined and weighted to provide accurate prevalence estimates representative of the noninstitutionalized US population.15 The current analysis pooled participants from 3 cycles: 2013 to 2014, 2015 to 2016, and 2017 to March 2020 (the 2019 to 2020 cycle was combined with the previous cycle and stopped early due to the coronavirus pandemic).16 Data were analyzed in May 2022. The protocol for each cycle was approved by the National Center for Health Statistics ethics review board, and participants provided written informed consent. All proportions presented use appropriate NHANES sample weights, as recommended by NHANES reporting guidelines.17
Data Collection
Data were collected by trained interviewers who administered standardized questionnaires in participants’ homes, followed by physical, anthropomorphic, and laboratory measurements in mobile examination centers. Data on age, sex, race and ethnicity, marital status, number of individuals in the household, household income, education, health insurance status, access to routine health care location, smoking status, hypertension, heart failure, and chronic kidney disease were obtained by self-report. Pill bottle review validated self-reported medication use in the past 30 days and included statins and antihypertensive medications for the current analysis. Blood pressure (average of 3 measurements), height, and weight were measured by trained individuals according to a standardized protocol. Urine and blood laboratory samples were collected during mobile examinations. Fasting triglyceride, LDL-C, fasting blood glucose, and hemoglobin A1c levels were also collected.
Independent Variable and Covariates
NHANES data collection requires individuals to select among the following categories for race and ethnicity: Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and other race, including multiracial. For the current analysis, participants were categorized as Asian, Black, or White based on self-identification as non-Hispanic Asian, non-Hispanic Black, and non-Hispanic White, respectively. Participants were categorized as Hispanic ethnicity based on self-identification as Mexican American or other Hispanic. Participants who self-identified as other race (including multiracial) were not included due to limited sample size. Details on other covariates are in the eMethods in Supplement 1. Ten-year predicted ASCVD risk was calculated using the PCE and divided into the following risk strata: 5% to less than 7.5%, 7.5% to less than 20%, and 20% or greater based on the 2018 ACC/AHA guidelines recommendation for increased statin-derived benefit.1,4 Because the PCE does not incorporate ethnicity, the equations for White race were applied to Asian and Hispanic participants.4 Clinical factors were categorized as ASCVD risk, body mass index (BMI), and chronic kidney disease status, whereas social determinants of health (SDOH) were defined as education, having a routine location for health care, and health insurance.
Study Population
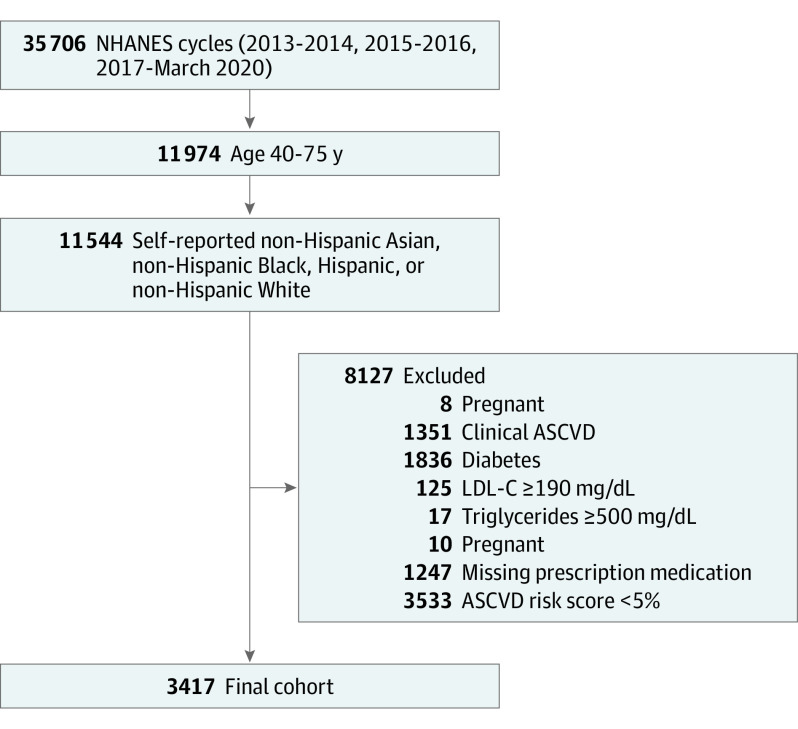
The current analysis assessed 11 536 NHANES participants aged 40 through 75 years who self-identified as Asian, Black, Hispanic, or White for inclusion. The selected age range was specified based on 2018 ACC/AHA guideline recommendations for applying the PCE.1,4 Participants were excluded if they met the following criteria: pregnant (n = 8), clinical ASCVD (self-reported prior myocardial infarction, prior stroke, or angina; n = 1351), diabetes (self-report of diagnosis or told to take insulin or oral antidiabetics, hemoglobin A1c >6.5% [to convert to proportion of total hemoglobin, multiply by 0.01], or fasting blood glucose >126 mg/dL [to convert to mmol/L, multiply by 0.0555]; n = 1836), LDL-C 190 mg/dL or greater (n = 125), triglyceride level 500 mg/dL or greater (to convert to mmol/L, multiply by 0.0113; n = 17), missing prescription data (n = 10), missing at least 1 component for PCE calculation (n = 1247), and 10-year predicted ASCVD risk less than 5% (n = 3533). The final analytic sample included 3417 NHANES participants (Figure 1), representing 39.4 million US adults after application of weight-based sampling.
Figure 1. Flow Diagram of Inclusion and Exclusion Criteria.
ASCVD indicates atherosclerotic cardiovascular disease; LDL-C, low-density lipoprotein cholesterol; NHANES, National Health and Nutrition Examination Surveys.
Outcome
The primary outcome was prevalence of statin use, defined by interviewer pill bottle review. The following generic or brand-name medications were included: atorvastatin, cerivastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin.
Statistical Analysis
Baseline characteristics of each ASCVD risk stratum were calculated using NHANES sampling weights and compared between each race and ethnicity. Differences in baseline characteristics were calculated for participants according to ASCVD risk stratum by race and ethnicity.
For the primary analysis, Poisson regression with adjustment for NHANES cycle was used to determine the association of race and ethnicity and ASCVD risk stratum (independent variables) with statin use (outcome variable). Given the frequency of statin use (>10%), prevalence ratios were calculated via Poisson regression with robust standard errors.18 Additionally, the proportional use of statins across NHANES cycles was compared within each ASCVD risk and race and ethnicity stratum using logistic regression.
Multivariate-adjusted Poisson regression models with robust error variance were constructed to identify significant clinical and SDOH factors associated with statin use within each race and ethnicity group. These race and ethnicity-specific models enabled the estimation of the prevalence ratios (PRs) and 95% CIs for statin use associated with each covariate of interest. Based on previously published literature, the clinical and SDOH factors considered for the multivariate models included ASCVD risk (as assessed by PCE), BMI (calculated as weight in kilograms divided by height in meters squared), chronic kidney disease, education status, having a routine location for health care, and health insurance.19,20 Variables included in PCE calculations were not included in the analysis to avoid collinearity, as ASCVD risk was included in the model. Interaction between ASCVD risk and the NHANES cycle was analyzed in each race and ethnicity stratum. Other SDOH factors, such as marital status and household food insecurity, were either missing in the 2019 to March 2020 model or had variable survey response rates due to the COVID-19 pandemic and were therefore not included in the primary analysis. Sensitivity analyses were conducted to evaluate the association of these SDOH factors (ie, marital status and household food insecurity) with statin use by constructing additional multivariable-adjusted Poisson regression models in the subset with available data. Sensitivity analyses were also conducted by substituting the ASCVD risk category with the individual components of the PCE risk score in the fully adjusted model. A sensitivity analysis was also performed using adjusted high-density lipoprotein cholesterol (HDL-C) and total cholesterol levels for individuals who reported taking statins by multiplying total cholesterol levels by a factor of 1.36 and HDL-C levels by a factor of 0.93 to estimate untreated levels for calculating the PCE risk. The adjustment factors were based on the previously reported treatment effect of statins on total cholesterol and HDL-C with a mean reduction of 27% in total cholesterol and a mean increase of 7% in HDL-C.21,22,23
Finally, the prevalence of statin use among race and ethnicity subgroups was evaluated across demographic and SDOH domain subgroups using unadjusted Poisson regression models (eMethods in Supplement 1). All analyses were performed with a significance threshold of P < .05 in R version 4.1.3 (R Foundation).
Results
Baseline Characteristics
The mean (SD) age was 61.8 (8.0) years. Of 3417 included participants, 1289 were women, and 2128 were men, yielding an estimated 14.9 million (37.8%) female participants and 24.5 million (62.2%) male participants. By self-report, 329 participants were Asian (weighted percentage, 4.2%), 1032 were Black (weighted percentage, 12.7%), 786 were Hispanic (weighted percentage, 10.1%), and 1270 were White (weighted percentage, 73.0%). The proportion of participants with a 10-year predicted ASCVD risk of 5% to less than 7.5% was 31.0%, 7.5% to less than 20% was 58.3%, and 20% or greater was 10.7% (Table 1; eTable 1 in Supplement 1). The median (IQR) predicted 10-year ASCVD risk was 10.1% (7.4-14.2), 10.3% (7.2-15.1), 9.2% (6.6-14.2), and 9.6% (6.9-15.0) in Asian, Black, Hispanic, and White participants, respectively. ASCVD risk 20% or greater was found for 12.2% of Asian participants, 11.9% of Black participants, 9.6% of Hispanic participants, and 10.6% of White participants.
Table 1. Characteristics of US Adults Aged 40 to 75 Years by Race and Ethnicity and Stratified by 10-Year Predicted Risk of Atherosclerotic Cardiovascular Disease (ASCVD), National Health and Nutrition Examination Survey 2013 to March 2020.
| Characteristic | % (95% CI) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5% to <7.5% | P valuea | 7.5% to <20% | P valuea | ≥20% | P valuea | ||||||||||
| Asian | Black | Hispanic | White | Asian | Black | Hispanic | White | Asian | Black | Hispanic | White | ||||
| Age, y | |||||||||||||||
| 40-49 | 16.7 (10.3-25.9) | 35.4 (29.3-42.1) | 24.8 (18.8-32.0) | 11.6 (8.9-15.1) | <.001 | 6.3 (4.2-9.3) | 10.2 (7.6-13.5) | 8.6 (4.3-16.5) | 3.8 (2.5-5.8) | <.001 | NAb | 1.2 (0.2-8.5) | NAb | 1.5 (0.2-10.7) | .02 |
| 50-59 | 50.8 (41.6-60.0) | 44.6 (37.6-51.8) | 51.1 (43.1-59.1) | 49.3 (44.8-53.7) | 21.4 (15.6-28.6) | 40.0 (35.3-44.9) | 29.0 (24.3-34.3) | 19.9 (16.1-24.4) | 6.0 (1.8-17.9) | 17.9 (11.9-26.1) | 10.4 (4.3-23.2) | 3.0 (0.8-10.2) | |||
| 60-69 | 31.1 (25.0-37.9) | 19.1 (14.9-24.1) | 24.1 (18.9-30.2) | 37.7 (32.2-43.6) | 54.2 (47.1-61.3) | 37.6 (32.8-42.7) | 48.1 (43.4-52.8) | 54.8 (50.1-59.4) | 28.5 (16.0-45.6) | 45.6 (36.3-55.2) | 24.7 (17.0-34.4) | 26.9 (18.7-37.0) | |||
| 70-75 | 1.4 (0.2-8.8) | 1.0 (0.3-3.1) | - | 1.3 (0.6-3.1) | 18.0 (12.3-25.6) | 12.2 (10.0-14.9) | 14.2 (11.0-18.3) | 21.4 (18.1-25.1) | 65.4 (48.6-79.1) | 35.3 (25.8-46.2) | 64.9 (53.0-75.2) | 68.6 (59.8-76.3) | |||
| Female | 41.1 (33.4-49.3) | 42.8 (35.9-50.0) | 32.9 (26.3-40.3) | 43.3 (36.7-50.0) | .12 | 37.3 (29.4-45.8) | 41.1 (37.4-45.0) | 29.2 (24.7-34.2) | 37.8 (33.8-41.9) | .02 | 23.1 (12.3-39.1) | 37.5 (26.6-49.9) | 28.8 (19.5-40.3) | 26.6 (19.3-35.3) | .31 |
| Male | 58.9 (50.7-66.6) | 57.2 (50.0-64.1) | 67.1 (59.7-73.7) | 56.7 (50.0-63.3) | 62.7 (54.2-70.6) | 58.9 (55.0-62.6) | 70.8 (65.8-75.3) | 62.2 (58.1-66.2) | 76.9 (60.9-87.7) | 62.5 (50.1-73.4) | 71.2 (59.7-80.5) | 73.4 (64.7-80.7) | |||
| > HS education | 13.9 (7.4-24.8) | 13.0 (9.3-18.0) | 35.0 (27.7-43.2) | 8.7 (5.9-12.8) | <.001 | 23.3 (16.9-31.2) | 20.5 (17.0-24.5) | 42.1 (36.1-48.3) | 5.4 (3.9-7.3) | <.001 | 33.5 (20.6-49.4) | 27.5 (21.0-35.0) | 50.6 (36.3-64.8) | 14.5 (8.8-22.9) | <.001 |
| Routine location for health care | 81.9 (72.7-88.5) | 89.9 (84.4-93.6) | 80.3 (74.0-85.3) | 90.2 (86.5-93.0) | <.001 | 86.3 (79.5-91.1) | 89.7 (87.3-91.7) | 77.0 (72.2-81.2) | 91.3 (89.3-93.0) | <.001 | 94.1 (82.2-98.2) | 89.1 (82.9-93.2) | 85.1 (75.4-91.5) | 94.9 (88. 8,97.7) | .02 |
| Health insurance | 88.4 (79.4-93.8) | 82.2 (77.3-86.2) | 79.3 (71.3-85.5) | 88.9 (82.9-93.0) | .05 | 88.8 (83.5-92.5) | 85.3 (81.3-88.6) | 75.0 (70.3-79.2) | 92.7 (90.3-94.6) | <.001 | 94.4 (82.9-98.3) | 85.4 (77.1-91.1) | 88.9 (81.3-93.7) | 96.7 (91.9-98.7) | <.001 |
| Body mass indexc | |||||||||||||||
| Underweight | 1.9 (0.5-7.6) | 0.9 (0.1-6.3) | 0.9 (0.2-3.8) | 1.4 (0.4-5.2) | <.001 | 2.4 (1.1-5.4) | 2.1 (1.1-3.9) | NAb | 0.8 (0.3-1.9) | <.001 | NAb | 0.7 (0.1-5.1) | 0.9 (0.1-6.8) | 1.5 (0.5-4.6) | .13 |
| Normal weight | 50.3 (39.0-61.6) | 14.8 (10.5-20.5) | 8.8 (5.3-14.2) | 18.2 (13.3-24.3) | 45.8 (39.1-52.6) | 20.4 (17.3-23.8) | 15.8 (12.3-20.1) | 20.6 (16.8-24.9) | 44.7 (27.7-62.9) | 23.6 (17.7-30.7) | 14.1 (8.2-23.2) | 18.8 (13.5-25.6) | |||
| Overweight | 35.9 (26.3-46.8) | 28.4 (22.9-34.5) | 42.7 (34.7-51.2) | 40.1 (33.6-47.0) | 41.6 (34.9-48.8) | 28.5 (24.4-32.9) | 43.6 (38.5-48.8) | 36.4 (32.4-40.7) | 40.6 (25.3-58.0) | 37.5 (30.7-44.8) | 42.3 (31.3-54.1) | 41.1 (32.6-50.3) | |||
| Obese | 11.9 (5.9-22.6) | 55.9 (49.5-62.1) | 47.6 (39.5-55.8) | 40.3 (35.0-45.8) | 10.2 (7.2-14.1) | 49.1 (44.2-54.0) | 40.6 (35.2-46.4) | 42.2 (37.7-46.8) | 14.8 (4.9-36.6) | 38.2 (30.2-46.9) | 42.7 (30.1-56.2) | 38.5 (29.8-48.1) | |||
| Comorbidities | |||||||||||||||
| Hypertension | 53.3 (41.4-64.7) | 54.5 (47.5-61.3) | 39.1 (32.1-46.5) | 44.6 (38.4-50.9) | .04 | 64.9 (56.8-72.2) | 76.6 (73.5-79.5) | 58.4 (52.3-64.3) | 60.0 (55.8-64.1) | <.001 | 84.4 (68.6-93.1) | 96.6 (90.2-98.9) | 85.2 (76.0-91.3) | 81.8 (72.7-88.4) | .01 |
| Chronic kidney disease | 11.1 (5.5-21.2) | 13.0 (9.1-18.4) | 7.0 (4.6-10.4) | 9.6 (6.9-13.1) | .27 | 12.1 (8.5-17.0) | 20.7 (17.3-24.5) | 15.6 (11.7-20.7) | 20.2 (16.8-24.1) | .11 | 35.1 (20.6-52.9) | 31.2 (23.7-39.9) | 30.2 (21.6-40.6) | 27.0 (20.1-35.3) | .66 |
| Heart failure | 0.7 (0.1-4.8) | 3.7 (1.9-7.2) | 0.7 (0.2-2.7) | 0.5 (0.1-1.5) | <.001 | 0.4 (0.0-2.9) | 2.2 (1.1-4.4) | 0.6 (0.2-2.1) | 1.2 (0.6-2.3) | .16 | 1.8 (0.2-12.0) | 4.7 (1.9-11.2) | 3.3 (0.7-15.0) | 2.0 (0.6-6.2) | .53 |
| Current smoking | 11.0 (5.7-20.2) | 24.1 (18.1-31.2) | 26.6 (19.6-35.0) | 23.0 (17.0-30.2) | .30 | 18.0 (13.5-23.5) | 34.7 (31.0-38.5) | 28.2 (24.0-32.8) | 22.2 (18.7-26.2) | <.001 | 12.7 (5.2-27.9) | 56.4 (48.3-64.1) | 20.2 (12.5-30.9) | 25.4 (20.5-31.1) | <.001 |
| Laboratory values | |||||||||||||||
| Total cholesterol, median (95% CI), mg/dLd | 206 (194-220) | 196 (191-203) | 206 (197-215) | 202 (197-206) | .13 | 203 (193-215) | 194 (191-198) | 203 (198-209) | 200 (196-204) | <.001 | 196 (177-220) | 200 (187-210) | 207 (191-224) | 201 (190-209) | .64 |
| LDL-C, median (95% CI), mg/dLd,e | 110 (93-130) | 114 (104-127) | 126 (123-131) | 122 (115-128) | .01 | 127 (116-135) | 112 (107-120) | 126 (122-136) | 118 (115-124) | .01 | NAb | 115 (99-132) | 112 (102-139) | 121 (103-135) | .71 |
| HDL-C, median (95% CI), mg/dLd | 49 (47-54) | 56 (53-60) | 46 (43-49) | 51 (49-53) | <.001 | 50 (46-55) | 53 (52-55) | 44 (43-48) | 51 (50-53) | <.001 | 51 (47-57) | 52 (49-57) | 47 (43-51) | 48 (46-53) | <.001 |
| Triglycerides, median (95% CI), g/dLe,f | 111 (83-169) | 78 (72-89) | 112 (102-123) | 104 (88-126) | <.001 | 111 (99-138) | 80 (74-85) | 116 (105-133) | 110 (99-122) | <.001 | NAb | 79 (66-115) | 113 (83-228) | 109 (98-155) | .03 |
| HbA1c, median (95% CI), %g | 5.7 (5.6-5.8) | 5.7 (5.7-5.8) | 5.6 (5.5-5.8) | 5.5 (5.5-5.6) | <.001 | 5.8 (5.8-6.0) | 5.8 (5.8-5.9) | 5.6 (5.6-5.7) | 5.6 (5.6-5.7) | <.001 | 5.9 (5.8-6.3) | 5.8 (5.8-6.0) | 5.7 (5.7-5.9) | 5.7 (5.7-5.9) | .01 |
| Mean SBP, median (95% CI), mm Hg | 128 (123-134) | 128 (126-130) | 127 (126-131) | 124 (123-126) | <.001 | 134 (130-136) | 135 (134-137) | 133 (131-136) | 128 (126-130) | <.001 | 153 (142-161) | 152 (150-157) | 144 (139-153) | 140 (137-144) | <.001 |
| Taking ≥ 1 antihypertensive agent | 37.8 (26.8-50.3) | 38.5 (32.7-44.6) | 22.5 (17.4-28.6) | 33.2 (26.7-40.3) | .03 | 45.6 (36.1-55.3) | 58.7 (54.1-63.1) | 39.3 (34.2-44.6) | 44.8 (40.5-49.2) | <.001 | 60.2 (44.1-74.4) | 80.0 (70.5-87.0) | 66.1 (55.6-75.2) | 68.5 (59.8-76.1) | .12 |
| 10-y ASCVD risk, median (95% CI), %c | 6.1 (6.0-6.4) | 6.2 (6.0-6.4) | 6.0 (5.8-6.2) | 6.1 (6.0-6.2) | .84 | 11.0 (10.5-11.5) | 11.7 (11.2-12.0) | 11.2 (10.6-11.9) | 11.7 (11.1-12.4) | .12 | 23.0 (21.4-28.8) | 24.5 (23.3-26.3) | 23.9 (22.7-25.6) | 23.3 (22.9-23.8) | .20 |
Abbreviations: HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; HS, high school; LDL-C, low-density lipoprotein cholesterol; NA, not applicable; SBP, systolic blood pressure.
P values are calculated by χ2, analysis of variance, or Kruskal-Wallis for categorical, parametric numeric, and nonparametric numeric variables, respectively.
Sample sizes less than 30 were not reported due to unstable estimates.
Calculated as weight in kilograms divided by height in meters squared and categorized as underweight (<18.5 kg/m2), normal weight (18.5 to <25 kg/m2), overweight (25 to <30 kg/m2), and obese (≥30 kg/m2).
To convert to mmol/L, multiply by 0.0259.
Triglyceride and LDL-C sampling calculations were completed using a fasting subsample weight in 1542 adults with available data.
To convert to mmol/L, multiply by 0.0113.
To convert to proportion of total hemoglobin, multiply by 0.01.
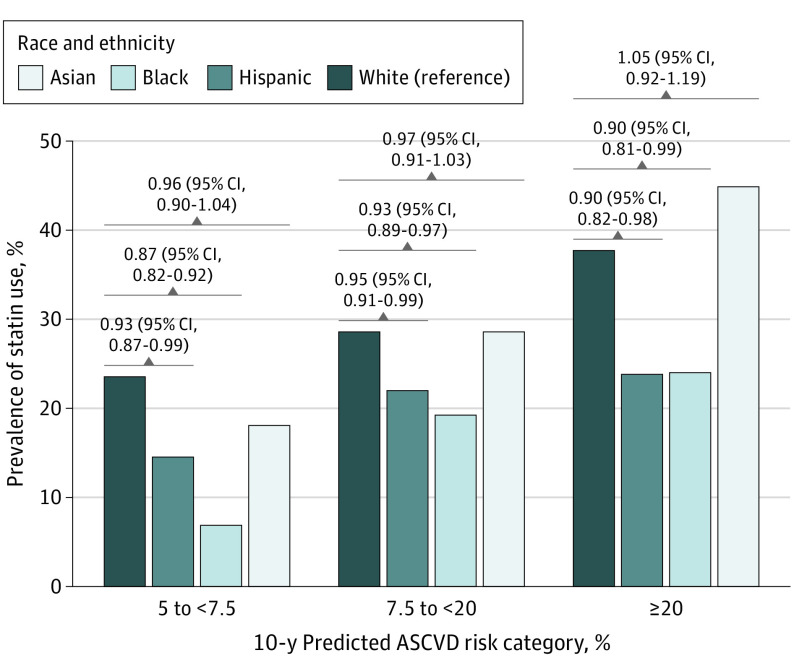
Prevalence of Statin Use by Race and Ethnicity and 10-Year Predicted ASCVD Risk Strata
Overall, the prevalence of statin use was 25.5% (95% CI, 23.3-27.9). Statin use was significantly lower among Black and Hispanic participants vs White participants in the overall cohort (20.0% vs 27.9%, P < .001, and 15.4% vs 27.9%, P < .001, respectively), as well as across each ASCVD risk strata (Figure 2). There was no difference in overall statin use between Asian and White participants (25.5% vs 27.9%; PR, 0.98; 95% CI, 0.94-1.02; P = .38) or within each ASCVD risk strata (Figure 2). Within each race and ethnicity group, a graded increase in the prevalence of statin use was observed across ASCVD risk strata (Figure 2). However, the use of statins in the highest risk strata (ASCVD risk ≥20%) remained low overall and was significantly lower among Black participants (23.8%; PR, 0.90; 95% CI, 0.82-0.98) and Hispanic participants (23.9%; PR, 0.90; 95% CI, 0.81-0.99) compared with White participants (37.6%; reference group). In the sensitivity analysis using adjusted levels of total cholesterol and HDL-C among individuals receiving statin therapy, statin use patterns across different race and PCE risk-based subgroups was similar to that observed in the primary analysis (eFigure in Supplement 1).
Figure 2. Prevalence of Statin Use Among Participants in the 2013-March 2020 National Health and Nutrition Examination Surveys Meeting Criteria for Primary Prevention Based on Predicted 10-Year Risk of Atherosclerotic Cardiovascular Disease (ASCVD).
Data represented as prevalence ratios with 95% CIs.
Temporal Trends in Prevalence of Statin Use Across Race and Ethnicity and Risk Strata
The prevalence of statin use was lower among Black and Hispanic participants compared with Asian and White participants across all survey cycles and ASCVD risk strata (Figure 3). No significant differences in prevalence of statin use over time were noted in any race and ethnicity stratified by ASCVD risk strata.
Figure 3. Temporal Trends in Prevalence of Statin Use Among Participants in the 2013-March 2020 National Health and Nutrition Examination Surveys (NHANES) Meeting Criteria for Primary Prevention.
Data represented as odds ratios and 95% CIs with NHANES cycle 2013-2014 as the reference cycle.
Factors Associated With Prevalence of Statin Use
In adjusted analyses, among clinical factors, higher ASCVD risk strata had significantly greater prevalence of statin use across each race and ethnicity group. BMI 30 or greater (vs less than 30) was also significantly associated with greater use of statins among Asian participants (PR, 1.11; 95% CI, 1.00-1.23), Black participants (PR, 1.09; 95% CI, 1.03-1.15), and White participants (PR, 1.07; 95% CI, 1.01-1.13), but not among Hispanic participants (PR, 0.94; 95% CI, 0.96-1.12) (Table 2). Among SDOH factors, access to routine health care and health insurance were both significantly associated with greater statin use among Black, Hispanic, and White participants in the fully adjusted model (Table 2; eTable 4 in Supplement 1). Having a routine location for health care was associated with greater statin use for Asian participants (PR, 1.22; 95% CI, 1.11-1.34), but health insurance was not (PR, 0.99; 95% CI, 0.84-1.17) (Table 2). In sensitivity analyses among the subset of participants with data on other SDOH factors, marital status and food insecurity were not associated with statin use (eTable 4 in Supplement 1). In the sensitivity analysis assessing each component of PCE instead of ASCVD risk estimate, taking at least 1 antihypertensive was the sole component associated with increased statin use across all race and ethnicity groups (eTable 2 in Supplement 1).
Table 2. Factors Associated With Prevalence of Statin Use by Race and Ethnicity, National Health and Nutrition Examination Survey (NHANES) 2013 to March 2020.
| Characteristic | Multivariable-adjusted prevalence ratio (95% CI)a | |||
|---|---|---|---|---|
| Asian | Black | Hispanic | White | |
| 10-y ASCVD risk strata | ||||
| 5%-<7.5% | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 7.5%-<20% | 1.06 (0.97-1.14) | 1.12 (1.06-1.17) | 1.04 (0.99-1.10) | 1.03 (0.98-1.09) |
| ≥20% | 1.22 (1.07-1.39) | 1.16 (1.07-1.26) | 1.11 (1.03-1.21) | 1.10 (1.01-1.19) |
| NHANES cycle | ||||
| 2013-2014 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2015-2016 | 1.03 (0.92-1.16) | 1.03 (0.97-1.10) | 0.95 (0.89-1.01) | 0.94 (0.89-0.99) |
| 2017-Mar 2020 | 1.05 (0.94-1.17) | 1.02 (0.96-1.08) | 0.96 (0.91-1.01) | 0.95 (0.90-1.00) |
| < HS education (yes vs no) | 0.95 (0.84-1.07) | 0.99 (0.95-1.04) | 0.99 (0.92-1.08) | 1.03 (0.95-1.13) |
| Routine location for health care (yes vs no) | 1.22 (1.11-1.34) | 1.15 (1.10-1.21) | 1.22 (1.16-1.28) | 1.17 (1.10-1.24) |
| Health insurance (yes vs no) | 0.99 (0.84-1.17) | 1.14 (1.09-1.19) | 1.24 (1.19-1.28) | 1.20 (1.14-1.25) |
| Body mass indexb | ||||
| Underweight | 0.91 (0.80-1.03) | 0.87 (0.82-0.93) | 0.81 (0.78-0.85) | 0.81 (0.76-0.87) |
| Normal weight | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Overweight | 1.06 (0.96-1.16) | 0.99 (0.92-1.07) | 1.04 (0.98-1.10) | 1.03 (0.97-1.09) |
| Obese | 1.11 (1.00-1.23) | 1.02 (0.95-1.10) | 1.07 (1.01-1.14) | 1.07 (1.01-1.13) |
| Chronic kidney diseasec | 0.99 (0.88-1.11) | 1.01 (0.95-1.08) | 1.01 (0.95-1.07) | 0.99 (0.94-1.05) |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; HS, high school.
The multivariable-adjusted model included 10-year predicted ASCVD risk stratum, NHANES cycle, education, having a routine location for health care, health insurance status, body mass index category, and chronic kidney disease. Interaction between 10-year ASCVD risk and NHANES cycle was tested with P > 10.
Calculated as weight in kilograms divided by height in meters squared, categorized as underweight (<18.5 kg/m2), normal weight (18.5 to <25 kg/m2), overweight (25 to <30 kg/m2), and obese (≥30 kg/m2).
Chronic kidney disease was defined by self-report or an estimated glomerular filtration rate of less than 60 mL/min/1.73 m2 using the Chronic Kidney Disease Epidemiology Collaboration equation24 or a urinary albumin-to-creatinine ratio greater than 30 mg/g.
Statin Use Across SDOH Subgroups
Analyses of statin use prevalence by race and ethnicity stratified by demographic and SDOH categories were qualitatively similar to that observed in the overall population, with lower statin use among Black and Hispanic participants compared with Asian and White participants (eTable 3 in Supplement 1). Among NHANES participants with health insurance, prevalence of statin use was lower in Black and Hispanic participants than in White participants.
Discussion
In this cross-sectional study of a nationally representative sample of US adults with an indication for statin therapy for primary prevention based on 10-year ASCVD risk, prevalence of statin use was low overall across all NHANES cycles, risk categories, and race and ethnicity strata. There were marked disparities in statin use by race and ethnicity groups, such that Black and Hispanic adults had the lowest use rates across all risk strata compared with White adults. Higher ASCVD risk strata were associated with greater statin use with each race and ethnicity group. Among SDOH factors, lack of a routine health care location and health insurance were significantly associated with a lower prevalence of statin use across all race and ethnicity groups evaluated. These findings demonstrate the persistent racial and ethnic disparities in guideline-recommended statin use for primary prevention among at-risk adults and represent an opportunity to advance pharmacoequity in primary prevention.25
Prior studies from single health care systems and community health care networks demonstrated underuse of statins for primary prevention among Black and Hispanic (vs White) patients receiving care in a health care setting.10,11,26 In 1 study,10 among 33 298 primary prevention patients of a large academic health care system with an indication for statin use, the odds of statin prescription were 62% lower among Black adults with an ASCVD risk 7.5% or greater and 36% lower among Black adults with diabetes compared to White adults with similar characteristics. Likewise, in a study of 32 440 adults with diabetes from the Community Health Applied Research Network database,11 statin prescription rates were lower among adults who identified as belonging to a race or ethnicity group other than White. The current analysis adds to these observations and demonstrates existing racial and ethnic disparities in statin use for primary prevention in a nationally representative cohort of community-dwelling adults that persisted over time. While we observed greater use of statins among individuals with higher ASCVD risk for each race and ethnicity group, the overall use of statins in the highest ASCVD risk group remained low with disproportionately lower rates among Black and Hispanic adults and no meaningful improvement over time. These findings highlight the persistent implementation gap and disparity in statin use for primary prevention in individuals at high risk.
Health disparities, such as those observed in the current study, are multifactorial and include the effects of current and historical structural and interpersonal racism.27 A higher burden of adverse SDOH has been found to be associated with health inequities.27,28 Consistent with our findings, SDOH factors, such as health insurance and access to care, have been previously identified as being associated with appropriate statin use.19,29,30 Potential mechanisms or manifestations of systemic racism that could impact racial disparities in primary prevention statin use could arise from patient factors, such as trust in health care and pharmaceutical companies; health system factors, such as clinician bias and differential quality of care; structural factors, such as neighborhood deprivation and pharmacy access; and insurance factors, such as limited coverage and unaffordable drug costs.31 Together, these findings suggest that existing inequities in access to preventive care may be associated with the underuse of statins across races and ethnicity groups.
Our study findings have important public health implications. First, the estimated absolute risk difference in predicted ASCVD risk between Black and White adults (2.4% higher risk among Black patients) does not translate to greater statin treatment rates in Black vs White adults.5 The treatment gap is much wider than the predicted risk gap. Interventions aimed at improving access to prescription medications are critical to alleviate disparities. While overall statin use has increased over time, likely due to generic availability and expansion of health care access, we did not observe an increase in statin use for primary prevention.32,33,34 This may be related to persisting gaps in awareness, diagnosis, and access to care. Prior NHANES analyses report poorer awareness of hypertension and hyperlipidemia among Black and Hispanic participants vs White participants.35,36,37 To meet the goals of the Million Hearts initiative38 to prevent 1 million ASCVD events by 2027, efforts are needed to improve awareness and screening for ASCVD risk factors and access to evidence-based preventive therapies, specifically among those who self-identify as Black or Hispanic.
The strengths of the present study include standardized collection of data and the generalization of the study sample to the national population. Additionally, the detailed pill bottle review allowed for an accurate measure of realistic medication use behaviors. The exclusion of secondary prevention populations allowed us to ascribe statin use to ASCVD risk rather than a competing indication, although temporal associations between diagnosis and medication use could not be ascertained in the cross-sectional design.
Limitations
This study has some noteworthy limitations. Due to the limited sample size and NHANES questionnaire assessment, homogenization of Hispanic ethnicity was used in this analysis. Homogenizing this group of US adults fails to discern notable differences, such as the increased prevalence of cardiovascular risk factors observed among Puerto Rican and Cuban adults.39,40 Additionally, the study only assessed 4 categories of race and ethnicity and excluded other race and ethnicity groups, such as Alaskan Native, Native American, and multiracial. While sample weighting ensures accurate estimates, small sample sizes existed for Asian participants within the ASCVD subgroups; therefore, estimates for Asian statin use may be unstable and interpreted with caution. Furthermore, the PCE differentiates predicted ASCVD risk based on self-identification as Black and categorizes all other races and ethnicities as non-Black. The reliance on Black vs non-Black racial distinction in the PCE fails to capture the environmental context that leads to health disparities and differential treatment of cardiovascular disease prevention for adults of any race or ethnicity other than White.41,42 Similarly, self-report data in the NHANES survey may be subject to limitations of recall bias and underreporting. It is plausible that minor previous ASCVD events, such as transient ischemic attacks or peripheral artery disease, may be underreported, leading to the misidentification of secondary prevention statin use for primary prevention. Moreover, the calculation of PCE among individuals taking statin therapy is likely to underestimate their 10-year ASCVD risk prior to statin initiation, leading to some degree of misclassification in the PCE risk groups. However, in the sensitivity analysis using corrected levels of total cholesterol and HDL-C among individuals reporting statin use for estimate of PCE, the pattern of statin use across different race- and PCE risk–based groups was similar to that observed in the primary analysis. Data on prior statin use, copayment, statin intolerance, and dose are not available in NHANES, which would have allowed us to further evaluate the clinical appropriateness of statin use among those who receive statin therapy vs those who do not.
Conclusions
In the current analysis of NHANES participants from 2013 through March 2020 with a guideline indication for statin use for primary prevention, prevalence of statin use was substantially lower among Black and Hispanic participants compared to White participants. Overall, prevalence of statin use was low among Asian, Black, Hispanic, and White participants, particularly among those with an ASCVD risk 20% or greater. However, access to health care and health insurance were significantly associated with statin use and offer modifiable barriers to improve statin use. The significant differences in prevalence of statin use observed in this study, despite high ASCVD risk, highlight the importance of identifying intervenable factors to reduce cardiovascular health inequities.
eMethods
eTable 1. Characteristics of US Adults Aged 40-75 by Race and Ethnicity and 10-year ASCVD Risk, NHANES 2013-March 2020
eTable 2. Sensitivity Analysis of Individual PCE Factors Associated with Prevalent Statin Use by Race and Ethnicity, NHANES 2013-March 2020
eTable 3. Association of Race and Ethnicity and Prevalent Statin Use within Levels of Demographics and Social Determinants of Health, NHANES 2013-2018
eTable 4. Association of Social Determinants of Health in Fully Adjusted Models within Race and Ethnicity, NHANES 2013-March 2020
eFigure. Sensitivity Analysis for Prevalent Statin Use Among NHANES 2013-2020 Participants Meeting Criteria for Primary Prevention Based on Statin-adjusted Predicted 10-year ASCVD Risk
Data sharing statement
References
- 1.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;139(25):e1082-e1143. doi: 10.1161/CIR.0000000000000625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Centers for Disease Control and Prevention . Leading causes of death and injury. Published February 10, 2022. Accessed May 10, 2022. https://www.cdc.gov/injury/wisqars/LeadingCauses.html
- 3.Eberly LA, Richterman A, Beckett AG, et al. Identification of racial inequities in access to specialized inpatient heart failure care at an academic medical center. Circ Heart Fail. 2019;12(11):e006214. doi: 10.1161/CIRCHEARTFAILURE.119.006214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25)(suppl 2):S49-S73. doi: 10.1161/01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 5.Vasan RS, van den Heuvel E. Differences in estimates for 10-year risk of cardiovascular disease in Black versus White individuals with identical risk factor profiles using pooled cohort equations: an in silico cohort study. Lancet Digit Health. 2022;4(1):e55-e63. doi: 10.1016/S2589-7500(21)00236-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393-e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez CJ, Allison M, Daviglus ML, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States. Circulation. 2014;130(7):593-625. doi: 10.1161/CIR.0000000000000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pokharel Y, Gosch K, Nambi V, et al. Practice-level variation in statin use among patients with diabetes: insights from the PINNACLE registry. J Am Coll Cardiol. 2016;68(12):1368-1369. doi: 10.1016/j.jacc.2016.06.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minhas AMK, Ijaz SH, Javed N, et al. National trends and disparities in statin use for ischemic heart disease from 2006 to 2018: insights from National Ambulatory Medical Care survey. Am Heart J. 2022.252:60-69. doi: 10.1016/j.ahj.2022.05.015 [DOI] [PubMed] [Google Scholar]
- 10.Dorsch MP, Lester CA, Ding Y, Joseph M, Brook RD. Effects of race on statin prescribing for primary prevention with high atherosclerotic cardiovascular disease risk in a large healthcare system. J Am Heart Assoc. 2019;8(22):e014709. doi: 10.1161/JAHA.119.014709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akhabue E, Rittner SS, Carroll JE, et al. Implications of American College of Cardiology/American Heart Association (ACC/AHA) cholesterol guidelines on statin underutilization for prevention of cardiovascular disease in diabetes mellitus among several US networks of community health centers. J Am Heart Assoc. 2017;6(7):e005627. doi: 10.1161/JAHA.117.005627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Virani SS, Alonso A, Aparicio HJ, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254-e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 13.Chobufo MD, Singla A, Rahman EU, Michos ED, Whelton PK, Balla S. Temporal trends in atherosclerotic cardiovascular disease risk among U.S. adults. analysis of the National Health and Nutrition Examination Survey (NHANES), 1999-2018. Eur J Prev Cardiol. 2022;29(18):2289-2300. doi: 10.1093/eurjpc/zwac161 [DOI] [PubMed] [Google Scholar]
- 14.US Centers for Disease Control and Prevention . National health and nutrition examination survey. Published March 28, 2022. Accessed April 11, 2022. https://www.cdc.gov/nchs/nhanes/index.htm
- 15.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1. 2013;(56):1-37. https://www.cdc.gov/nchs/data/series/sr_01/sr01_056.pdf [PubMed] [Google Scholar]
- 16.Akinbam L, Chen TC, Davy O, et al. National Health and Nutrition Examination Survey, 2017–March 2020 Prepandemic File: Sample Design, Estimation, and Analytic Guidelines. National Center for Health Statistics; 2022, doi: 10.15620/cdc:115434 [DOI] [PubMed] [Google Scholar]
- 17.US Centers for Disease Control and Prevention . NHANES survey methods and analytic guidelines. Accessed February 15, 2023. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx
- 18.Knol MJ, Duijnhoven RG, Grobbee DE, Moons KGM, Groenwold RHH. Potential misinterpretation of treatment effects due to use of odds ratios and logistic regression in randomized controlled trials. PLoS One. 2011;6(6):e21248. doi: 10.1371/journal.pone.0021248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mefford MT, Rosenson RS, Deng L, et al. Trends in statin use among US adults with chronic kidney disease, 1999-2014. J Am Heart Assoc. 2019;8(2):e010640. doi: 10.1161/JAHA.118.010640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens. 2021;34(7):707-717. doi: 10.1093/ajh/hpab011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edwards JE, Moore RA. Statins in hypercholesterolaemia: a dose-specific meta-analysis of lipid changes in randomised, double blind trials. BMC Fam Pract. 2003;4:18. doi: 10.1186/1471-2296-4-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benn M, Watts GF, Tybjaerg-Hansen A, Nordestgaard BG. Familial hypercholesterolemia in the danish general population: prevalence, coronary artery disease, and cholesterol-lowering medication. J Clin Endocrinol Metab. 2012;97(11):3956-3964. doi: 10.1210/jc.2012-1563 [DOI] [PubMed] [Google Scholar]
- 23.Bucholz EM, Rodday AM, Kolor K, Khoury MJ, de Ferranti SD. Prevalence and predictors of cholesterol screening, awareness, and statin treatment among US adults with familial hypercholesterolemia or other forms of severe dyslipidemia (1999-2014). Circulation. 2018;137(21):2218-2230. doi: 10.1161/CIRCULATIONAHA.117.032321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levey AS, Stevens LA, Schmid CH, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612. Medline: doi: 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Essien UR, Dusetzina SB, Gellad WF. A Policy prescription for reducing health disparities-achieving pharmacoequity. JAMA. 2021;326(18):1793-1794. doi: 10.1001/jama.2021.17764 [DOI] [PubMed] [Google Scholar]
- 26.Nanna MG, Navar AM, Zakroysky P, et al. Association of patient perceptions of cardiovascular risk and beliefs on statin drugs with racial differences in statin use: insights from the Patient and Provider Assessment of Lipid Management registry. JAMA Cardiol. 2018;3(8):739-748. doi: 10.1001/jamacardio.2018.1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384(8):768-773. doi: 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Havranek EP, Mujahid MS, Barr DA, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873-898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 29.Schroff P, Gamboa CM, Durant RW, Oikeh A, Richman JS, Safford MM. Vulnerabilities to health disparities and statin use in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. J Am Heart Assoc. 2017;6(9):e005449. doi: 10.1161/JAHA.116.005449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wirtz VJ, Kaplan WA, Kwan GF, Laing RO. Access to medications for cardiovascular diseases in low- and middle-income countries. Circulation. 2016;133(21):2076-2085. doi: 10.1161/CIRCULATIONAHA.115.008722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chalasani R, Krishnamurthy S, Suda KJ, Newman TV, Delaney SW, Essien UR. Pursuing pharmacoequity: determinants, drivers, and pathways to progress. J Health Polit Policy Law. 2022;47(6):709-729. doi: 10.1215/03616878-10041135 [DOI] [PubMed] [Google Scholar]
- 32.Salami JA, Warraich H, Valero-Elizondo J, et al. National trends in statin use and expenditures in the US adult population from 2002 to 2013: insights from the medical expenditure panel survey. JAMA Cardiol. 2017;2(1):56-65. doi: 10.1001/jamacardio.2016.4700 [DOI] [PubMed] [Google Scholar]
- 33.Sumarsono A, Lalani HS, Vaduganathan M, et al. Trends in utilization and cost of low-density lipoprotein cholesterol-lowering therapies among Medicare beneficiaries: an analysis from the Medicare Part D database. JAMA Cardiol. 2021;6(1):92-96. doi: 10.1001/jamacardio.2020.3723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sumarsono A, Lalani H, Segar MW, et al. Association of Medicaid expansion with rates of utilization of cardiovascular therapies among Medicaid beneficiaries between 2011 and 2018. Circ Cardiovasc Qual Outcomes. 2021;14(1):e007492. doi: 10.1161/CIRCOUTCOMES.120.007492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26(1):60-69. doi: 10.1161/01.HYP.26.1.60 [DOI] [PubMed] [Google Scholar]
- 36.Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment, and control in US Adults: trends in the hypertension control cascade by population subgroup (National Health and Nutrition Examination Survey, 1999-2016). Am J Epidemiol. 2019;188(12):2165-2174. doi: 10.1093/aje/kwz177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Centers for Disease Control and Prevention . Disparities in screening for and awareness of high blood cholesterol—United States, 1999–2002. Accessed May 11, 2022. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5405a2.htm
- 38.US Centers for Disease Control and Prevention . Million hearts. Published June 14, 2022. Accessed June 27, 2022. https://millionhearts.hhs.gov/index.html
- 39.Qato DM, Lee TA, Durazo-Arvizu R, et al. Statin and aspirin use among Hispanic and Latino adults at high cardiovascular risk: findings from the Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc. 2016;5(4):e002905. doi: 10.1161/JAHA.115.002905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuehn BM. Better risk assessment tools needed for Hispanic or Latino patients. Circulation. 2019;139(18):2186-2187. doi: 10.1161/CIRCULATIONAHA.119.040938 [DOI] [PubMed] [Google Scholar]
- 41.Vyas DA, James A, Kormos W, Essien UR. Revising the atherosclerotic cardiovascular disease calculator without race. Lancet Digit Health. 2022;4(1):e4-e5. doi: 10.1016/S2589-7500(21)00258-2 [DOI] [PubMed] [Google Scholar]
- 42.Flores Rosario K, Mehta A, Ayers C, et al. Performance of the pooled cohort equations in hispanic individuals across the United States: insights from the Multi-Ethnic Study of Atherosclerosis and the Dallas Heart Study. J Am Heart Assoc. 2021;10(9):e018410. doi: 10.1161/JAHA.120.018410 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eTable 1. Characteristics of US Adults Aged 40-75 by Race and Ethnicity and 10-year ASCVD Risk, NHANES 2013-March 2020
eTable 2. Sensitivity Analysis of Individual PCE Factors Associated with Prevalent Statin Use by Race and Ethnicity, NHANES 2013-March 2020
eTable 3. Association of Race and Ethnicity and Prevalent Statin Use within Levels of Demographics and Social Determinants of Health, NHANES 2013-2018
eTable 4. Association of Social Determinants of Health in Fully Adjusted Models within Race and Ethnicity, NHANES 2013-March 2020
eFigure. Sensitivity Analysis for Prevalent Statin Use Among NHANES 2013-2020 Participants Meeting Criteria for Primary Prevention Based on Statin-adjusted Predicted 10-year ASCVD Risk
Data sharing statement