Abstract
The World Trade Center disaster and its recovery work involved a range of hazardous occupational exposures that have not been fully characterized but that can be reasonably assumed to have the potential to cause mucosal inflammation, preferentially (but not exclusively) in the upper airway. A high prevalence of rhinosinusitis and upper airway disease (UAD) symptoms was reported by several early surveys. Clinical studies demonstrated objective, clinically significant, and persistent chronic perennial rhinosinusitis and UAD—with or without seasonal exacerbation—in a large proportion of patients. Demonstration of an association between UAD and available exposure indicators has been limited. Atopy seemed to be associated with increased UAD symptom severity and to be a risk factor for upper, but not lower, airway disease. World Trade Center-related UAD is considered an irritant-induced disease but not, in many cases, of acute onset. No data thus far suggest an increased upper airway cancer incidence.
Keywords: Occupational medicine, Rhinitis, Sinusitis, Inhalation injury, Atopy, Allergy, Pharyngitis, Laryngitis, Reflux disease
Introduction
The terrorist attacks on the World Trade Center (WTC) on September 11, 2001 (9/11) released a large amount of dust, smoke, and combustion products into the air of New York City [1, 2]. Smoldering fires continued until mid-December 2001, making it the longest-lasting urban fire in this country’s recorded history. The characterization of the released toxicants at the WTC site is incomplete, particularly for those released during the first few hours or days after the attack and for volatile components. The ensuing 9.5-month rescue, recovery, and service restoration endeavor exposed tens of thousands of rescue, recovery, and service restoration workers and volunteers to the pollutants released at the WTC site. Chemical analyses of samples of settled WTC dust collected 4 days after the disaster demonstrated that it was very alkaline (pH, 9.2–11.5), in all likelihood due to the large amount of pulverized cement and other basic construction materials [1, 2]. More than 98% of those settled dust particles had an aerodynamic diameter exceeding 10 μm (respirable), and contained—in addition to cement—cellulose, glass fibers, asbestos, lead, polycyclic aromatic hydrocarbons, polychlorinated biphenyls, and other potentially hazardous materials [1]. Studies of settled dust inside buildings surrounding the WTC (which had to be disturbed during clean-up) showed similar characteristics to those observed outdoors [3]. In contrast to those studies, a study of suspended particles indicated 1) a higher proportion of fine (inhalable) particles (PM2.5) in October 2001 (16%–86% of total dust) and April 2002 (7%–85% of total dust); 2) a higher concentration of fine particles near the center of the WTC disaster site, with a decreasing gradient toward its periphery; and 3) a decrease in concentrations of total dust and fine particles between those two time points [4]. The reported limited availability, adequacy, and/or use of protective respiratory equipment in all likelihood enhanced the respiratory hazard [4-7]. Other hazardous occupational exposures included ergonomic and psychological stressors.
From the limited knowledge of the inhaled particles and gases at the WTC disaster site briefly summarized above, and in consideration of hydrosolubility and particle size characteristics, the estimation was that many of them were irritants capable of causing inflammatory mucosal changes, with the upper airway as their primary target [8, 9]. No significant allergen exposures were generally expected in this setting, although allergic pathways could be enhanced indirectly by the proinflammatory effect of those irritants [10].
Early surveys reported a high prevalence of symptoms of chronic rhinosinusitis and upper airway mucosal inflammation among rescue and clean-up workers in relation to their exposures at the WTC site [11]. In this article, we summarize the findings of those surveys and correlate them with those in the very few clinical studies that have been reported thus far.
Symptom Survey–based Studies
Several published studies have estimated upper and/or lower airway disease (UAD and LAD, respectively) symptom prevalence among WTC workers. UAD generally includes any combination of rhinitis, sinusitis, pharyngitis, and laryngitis. Although some of the symptoms included in the survey questionnaires may be characteristic of some of those disease entities (e.g., nasal obstruction and anterior discharge, hoarseness, sore throat), others can be shared (e.g., posterior discharge by rhinitis and sinusitis) or be completely nonspecific (e.g., cough by several UADs and LADs [12]).
One of the earliest symptom-based surveys was conducted at the screening and monitoring program for the New York City firefighters [13]. Levels of exposure to WTC dust and smoke were predetermined to be high for the 16% of the population who arrived on the day of the attack, moderate for the 69% who arrived within the first 48 h of the attack, low for the 13% who arrived 3–7 days after the attack, and none for the 2% who were not present at the WTC site within 2 weeks of the terrorist attack. A case definition of WTC cough was established clinically and administratively as “-a persistent cough that developed after exposure to the site and was accompanied by respiratory symptoms severe enough that required medical leave for at least 4 weeks” [13]. Only 332 (3.3%) of the screened firefighters met that WTC cough case definition and were further investigated. After the collapse, the most common UAD symptom among those 332 firefighters was sore throat, reported by 82%, 74%, and 80% of the 332 firefighters in the high-, moderate-, and low-exposure groups, respectively. Nasal congestion and nasal drip were also commonly reported, the former by 51%, 56%, and 47%, and the latter by 39%, 42%, and 33% within the corresponding three exposure level groups. Unlike cough (which can be a symptom of UAD and LAD), these UAD symptom prevalences did not seem to correlate with the predetermined exposure levels.
A related symptom survey among 362 New York City firefighters conducted between October 1 and October 5, 2001, included a comparison group of WTC-unexposed firefighters. Of the WTC firefighters surveyed, 78% reported any UAD symptom, 54% reported sore throat, and 40% reported nasal congestion. Firefighters who arrived closer to the time of the WTC collapse had a statistically significant higher prevalence ratio of UAD symptoms compared with the unexposed firefighters, controlling for age and tobacco use. Multivariate analysis found exposure duration exceeding 7 days to be the only significant predictor of UAD [7].
A survey of a convenience sample of 1,138 non-firefighting rescue and clean-up workers and volunteers participating in a screening program between July 16 and December 31, 2002, provided an early picture of the adverse respiratory health effects of the WTC disaster, and attempted to distinguish incident from prevalent symptoms [6]. It revealed that 487 (42.8%) individuals had a previous history of UAD symptoms before 9/11, which worsened in 250 (51.3%) of them after their WTC-related work. The report also found that UAD symptoms were incident and persistent in 565 (50%) of the screened workers. The most common incident UAD symptoms experienced while working at the WTC site were throat irritation (44.2%), blowing nose more than usual (35.7%), and stuffy nose (35.1%). Those symptoms persisted until the time of the survey in 22.6%, 18%, and 23.2% of the workers, respectively.
Three smaller surveys covering a narrower range of occupational categories reported similar findings. The first was a symptom survey of 183 WTC recovery workers (in only five occupational categories) conducted in December 2001 [14]. Nasal congestion, sore throat, and hoarseness (the only three UAD symptoms investigated) were reported by 52%, 43%, and 44% of the workers, respectively. The incidence of those UAD symptoms exceeded that of LAD symptoms (cough, phlegm, and wheeze). The incidence of new or additional UAD, but not of LAD, symptoms seemed to be higher in patients who admitted to having at least one of those symptoms before they began working at the WTC. The second study was a survey of a convenience sample of 96 male ironworkers who arrived at the WTC site between September 11 and September 15, 2001, and worked at the WTC for varying lengths of time until February 8, 2002. The survey was conducted 5 months after 9/11 [15]. Of the 96 ironworkers, 74 (77.1%) had one or more respiratory symptoms, and 50 (52.1%) complained of sinus symptoms. The most commonly reported symptom was cough (64.6%), for which early exposure seemed to be the most reliable predictor. Only one of the ironworkers reported having sinus disease before working at the WTC disaster site. The third study, a survey of 240 police officers from the Emergency Services Unit, was completed in January 2002 [16]. Although it focused primarily on LAD, it also revealed that 89 (37.1%) and 24 (10%) police officers reported having rhinitis and sinusitis, respectively.
Rhinosinusitis and UAD symptom persistence between 2001 and 2005 was surveyed longitudinally in a study of New York City firefighters [17]. Before 9/11, frequent sore throat was reported by 3.2% of firefighters, and frequent rhinosinusitis symptoms by 4.4%. By year 1 after 9/11, symptom prevalence had increased 10-fold for UAD symptoms, with sore throat as the most commonly reported (62.4%). The latter decreased to 36% by year 2 and remained stable (37%) by year 4. In contrast, the prevalence of frequent rhinosinusitis symptoms remained high from year 1 (45.1%) to year 4 (47.8%) after 9/11.
Rhinosinusitis and UAD have been notably unexplored in the New York City Department of Health WTC Health Registry, the largest ongoing symptom-based survey of WTC-related adverse health effects [18].
Clinical Studies
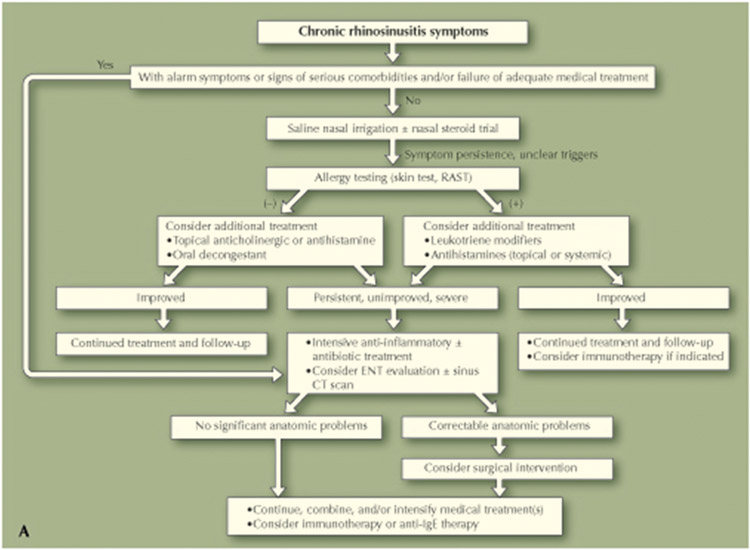
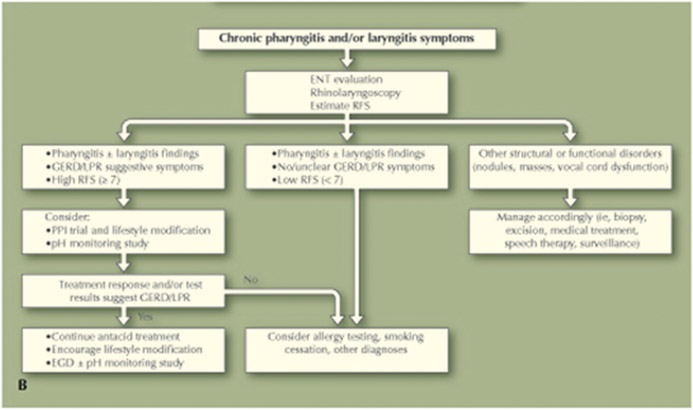
Detailed clinical studies were conducted at the WTC Health Effects Treatment Program (WTC HETP) at the Mount Sinai Medical Center in New York City. The WTC HETP was established in January 2003 to diagnose and treat the adverse health effects in WTC-exposed rescue, recovery, clean-up, and service restoration workers [19••]. The largest study was based on the clinical (and in ~40% of the patients, rhinolaryngoscopic) findings among 554 workers from the broadest possible spectrum of occupations at the WTC site who were sequentially evaluated during the first year of the program and treated and observed for 3 years. UAD was defined as the presence of at least three symptoms of perennial rhinitis, atopic or not, lasting more than 8 weeks. Symptoms and signs of sinusitis, pharyngitis, or laryngitis were evaluated by means of sinus CT scans and a comprehensive physical examination of the head and neck, including rhinolaryngoscopy. The reflux finding score was used to describe and quantitate laryngopharyngitis changes by endoscopy [20]. WTC-relatedness was presumed when the UAD symptoms arose while at or within 6 months of leaving the WTC site and was assessed within 1 year of patients’ first clinical evaluation. Structural abnormalities precluded an occupational causative attribution only if they were severe and thus deemed capable of accounting for all or most of the patients’ symptoms. Other competing causes of nonallergic rhinosinusitis were investigated and excluded [21]. If rhinosinusitis symptoms were preexistent, a substantial aggravation (e.g., from a single season to perennial and severe) was required for attribution. Figure 1a and b show the algorithms used to evaluate and treat patients with rhinosinusitis and laryngopharyngitis symptoms. Of the presumed WTC-related disease categories presented in the study, UAD clearly was the most prevalent (78.5%), consisting of rhinitis in all patients and very frequently associated with sinusitis, pharyngitis, and/or laryngitis. The most frequent disease presentation (29.8% of the patients) was a triad of UAD, LAD, and gastroesophageal reflux disease. The latter was almost invariably manifested with laryngopharyngeal symptoms and laryngopharyngoscopic inflammatory changes.
Fig. 1.
Clinical diagnostic and treatment algorithms for individuals with chronic rhinosinusitis (a) and laryngopharyngitis symptoms (b). EGD esophagogastroduodenoscopy; ENT ear, nose, and throat; GERD gastroesophageal reflux disease; LPR laryngopharyngeal reflux; RAST radioallergosorbent test; RFS reflux finding score
In a related study of 168 WTC HETP patients, the prevalence of presumably WTC-related UAD did not seem to vary by occupation, whereas that of LAD and pulmonary functional abnormalities did [22]. The role of atopy as a risk factor for presumably WTC-related UAD and LAD was examined in a second related study. Atopy was determined in 136 former WTC workers by radioallergosorbent test, skin prick test, or both. Atopy was present in 54.4% (74 of 136) of the workers tested, a prevalence similar to that of the general population in the United States. Bivariate analysis suggested that atopy was associated with higher WTC-related UAD and LAD symptom severity. Multivariate logistic regression analyses indicated that atopy was a risk factor for WTC-related UAD, but not LAD, after adjusting for age, sex, smoking, early arrival at the WTC site, and having a diagnosis of asthma before September 11, 2001. Ethnic background was not associated with atopic status, but immigrants (mostly first-generation) seemed significantly less likely to be atopic [23••]. Given the high prevalence among HETP workers of rhinitis [19••] and snoring (which are well known to be associated [24]), an exploratory study (n = 100) was conducted to examine the association of WTC-related UAD and WTC occupational exposure variables with obstructive sleep apnea (OSA) [25]. Neither association reached statistical significance. There seemed to be a trend toward increased severity of OSA with increased WTC occupational exposure duration that improved (but still did not reach statistical significance) after adjustment for competing risk factors in multivariate analysis. The possible association among UAD, gastroesophageal reflux disease, and OSA is still the subject of considerable research and speculation [26-28]. Further exploration of this issue may be warranted, although this study suggested that if WTC-related UAD or occupational exposures proved to be contributory to the development of OSA in this population, they would be weaker predictors than other risk factors, both highly prevalent among WTC workers, and strongly predictive of OSA (like male sex and excessive weight) [25]. Further studies with better subcategorization of UAD, a larger patient sample, and more detailed assessment of multiple potential risk factors may be warranted.
Lastly, the same detailed clinical HETP investigations allowed the documentation of the laryngopharyngitis that frequently characterizes WTC-related UAD. WTC-related reflux disorders were clinically diagnosed in 57.6% of the HETP patient population, and their manifestations were noted to almost invariably include laryngopharyngitis [19••]. WTC-related reflux disorders shared with LAD the apparent association with early arrival at the WTC [19••] and seemed to associate more clearly with LAD diagnoses and pulmonary functional abnormalities than with psychiatric diagnoses [29]. Another clinical study reported on the frequent observation of spirometric inspiratory flow limitation (suggestive of dynamic upper airway obstruction) and on a small case series of vocal cord dysfunction among these workers [30]. The latter could conceivably result from direct toxicant injury [31, 32] or indirectly from the highly prevalent comorbidities in these patients of rhinosinusitis (with chronic posterior nasal discharge [33]), reflux-related laryngopharyngitis [29, 34], and/or psychological illness [35].
Treatment and Medicolegal Aspects
The medical treatment of occupational rhinosinusitis includes, first and foremost, removal from the inciting exposure [36]. There are several excellent reviews on the treatment of chronic rhinosinusitis [37, 38••]. The WTC HETP diagnosis and treatment algorithms (Fig. 1a and b) were developed by the authors (Drs. de la Hoz and Shohet) for the WTC HETP occupational physicians to have a readily accessible guideline tailored to the specificities of the WTC-exposed population, and based on the best available published medical evidence at the time.
In the case of the former WTC rescue and recovery workers, prevention was aimed at post-WTC occupational exposures, which were considerable for many occupations (e.g., firefighters, demolition and construction laborers, construction trade workers, ironworkers, welders). Additionally, those occupations almost always require the use of protective respiratory equipment, for which rhinosinusitis and UAD can be an obstacle. For the roughly 50% of workers who were actively employed 2 years after ending their WTC work (de la Hoz, unpublished data), WTC HETP physicians used medical treatment, reduced exposure, and/or vocational retraining to maintain the workers’ productivity to the extent possible.
The medicolegal classification of these workers’ chronic rhinosinusitis and UAD was based on the clinical parameters described in the previous section. Objective testing specifically for occupational rhinosinusitis remains imperfect, nonstandardized, and generally unavailable [36], and certainly would have been nonapplicable to the WTC workers whose condition was deemed irritant induced and their inciting occupational exposure not reproducible. Comorbidities (particularly lower airway, psychological, and musculoskeletal diseases [19••]) added considerably to or overshadowed the occupational UAD-related disability.
Conclusions
The WTC disaster and its recovery work involved a range of hazardous occupational exposures that have not been (and may never be) fully characterized. What is known about the characteristics of settled dust samples suggests that those exposures included a predominance of respirable, hydrosoluble, and alkaline particles, which can be reasonably assumed to have the potential to cause mucosal inflammation preferentially (but not exclusively) in the upper airway. Compared with the settled dust studies, a limited air sampling study reported a larger proportion of inhalable (PM2.5) particles but also suggested a concentration gradient from the center of the WTC pile to its periphery and from the first to the third and last trimester of the recovery work.
The results from several early symptom surveys clearly suggested a high prevalence of rhinosinusitis and UAD. The clinical studies, which included examination (often endoscopic) of the upper airway, demonstrated objective, clinically significant, and persistent chronic perennial rhinosinusitis and UAD, with or without seasonal exacerbation, in a large proportion of patients. On the other hand, and unlike the situation with LAD, almost no study to date has documented a clear association between UAD and several exposure indicators (like early arrival at the WTC site, exposure to the dust from the collapse of the towers, total exposure duration, and occupation). Atopy—considered a preexisting, genetically determined characteristic—seemed to be associated with increased UAD symptom severity, which is in agreement with what controlled exposure research study results would predict [39, 40]. Atopy also seemed to be a risk factor for what seems to be WTC-related, irritant-induced UAD, but not for LAD. With respect to the former, previously published reports are very scarce, and their results mixed [36, 41]. With respect to the latter, however, the lack of association with atopic status does not seem surprising [42].
A remarkable clinical observation is that the symptoms of rhinosinusitis and UAD appeared in many of the workers rather insidiously over the course of weeks to months at the WTC site, and in many patients up to 6 months after ceasing their exposure(s). This finding places WTC-related UAD in the category of irritant induced but not, in many cases, of acute onset, and this characteristic is analogous to what has been observed with WTC-related LAD [19••]. It is also of interest to note that the increased incidence rate of presumed WTC-related asthma returned to the expected population baseline rate about 6 months after the official end of the recovery effort [43], corroborating a posteriori the occupational attribution criterion used at the HETP. Unfortunately, those investigators did not include rhinitis and UAD in their studies.
The limited correlation of UAD with exposure variables is in agreement with the relatively scarce previously reported literature on irritant-induced rhinosinusitis [41]. It is conceivable that the continued resuspension of predominantly larger settled dust particles during the rescue, debris removal, and clean-up efforts constantly reexposed workers regardless of their arrival time, occupation, exposure duration, or distance from the pile.
Another remarkable finding with the presumed WTC-related UAD (in comparison to other reported irritant-induced UAD series) is the prominence of laryngopharyngitis, documented in the clinical studies to an unprecedented level. Laryngopharyngitis frequently overshadowed rhinosinusitis, contributed to the symptom of cough (and many others), may at least partially explain the frequent finding of increased dynamic upper airway resistance and inspiratory flow limitation by spirometry, and in some cases manifested as vocal cord dysfunction [30]. Laryngopharyngitis in many cases probably resulted from direct toxicant- induced generalized upper airway inflammatory mucosal injury. As noted previously, gastroesophageal reflux disorders were diagnosed in more than 50% of the workers evaluated, and their manifestations almost invariably included laryngopharyngitis [19••]. The possibility that reflux disorders and related laryngopharyngitis may have also been a subclinically preexistent and a postexposure local injury predisposing and/or amplifying factor deserves further consideration [19••].
Given the exposure to carcinogens at the WTC site, the development of neoplastic diseases is an area of concern. No conclusive data thus far suggest an increased cancer incidence, but adequate long-term follow-up is clearly needed.
WTC-related UAD significantly impacted the quality of life and ability to work of those workers whose occupations often involved dust and irritant exposures and required the ability to wear personal respiratory protective equipment. Together with the other temporally related physical and psychological comorbidities, and social dislocation, the WTC experience underscores the need for a comprehensive, integrated, and multidisciplinary approach to address the complex needs of disaster victims [22] and for ongoing monitoring efforts to ensure adequate follow-up and long-latency disease surveillance and detection.
Acknowledgments
The publication of this work was made possible by the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health (CDC/NIOSH) cooperative agreement no. U10 OH008225. The contents of this article are the sole responsibility of the authors and do not necessarily represent the official views of the CDC/NIOSH. The work described in this article was done before October 2006, when the WTC HETP had been funded by the following philanthropic organizations: the American Red Cross, the September 11 Fund, the Robin Hood Foundation, and the Bear Stearns Charitable Foundation.
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
Rafael E. de la Hoz, Department of Preventive Medicine, Mount Sinai School of Medicine, Box 1059, One Gustave L. Levy Place, New York, NY 10029, USA
Michael R. Shohet, Department of Otolaryngology and Head and Neck Surgery, Mount Sinai School of Medicine, Box 1189, One Gustave L. Levy Place, New York, NY 10029, USA
Jeffrey M. Cohen, Department of Preventive Medicine, Mount Sinai School of Medicine, Box 1059, One Gustave L. Levy Place, New York, NY 10029, USA
References
Papers of particular interest, published recently, have been highlighted as:
•• Of major importance
- 1.Lioy PJ, Weisel C, Millette JR, et al. : Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in Lower Manhattan after the collapse of the WTC 11 September 2002 Environ Health Perspect 2002, 110:703–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGee JK, Chen LC, Cohen MD, et al. : Chemical analysis of World Trade Center fine particulate matter for use in toxicologic assessment. Environ Health Perspect 2003, 111:972–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Offenberg JH, Eisenreich SJ, Chen LC, et al. : Persistent organic pollutants in the dusts that settled across Lower Manhattan after September 11, 2001. Environ Sci Technol 2003, 37:502–508. [DOI] [PubMed] [Google Scholar]
- 4.Geyh AS, Chillrud S, Williams DL, et al. : Assessing truck driver exposure at the World Trade Center disaster site: personal and area monitoring for particulate matter and volatile organic compounds during October 2001 and April 2002. J Occup Environ Hyg 2005, 2:179–193. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention: Use of respiratory protection among responders at the World Trade Center—New York City, September 2001. MMWR Morb Mortal Wkly Rep 2002. 51:6–8. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention: Physical health status of World Trade Center rescue and recovery workers and volunteers—New York City, July, 2002–August, 2004. MMWR Morb Mortal Wkly Rep 2004, 53:807–812. [PubMed] [Google Scholar]
- 7.Feldman DM, Baron SL, Bernard BP, et al. : Symptoms, respiratory use, and pulmonary function changes among New York City firefighters responding to the World Trade Center disaster. Chest 2004, 125:1256–1264. [DOI] [PubMed] [Google Scholar]
- 8.Shusterman D: Toxicology of nasal irritants. Curr Allergy Asthma Rep 2003, 3:258–265. [DOI] [PubMed] [Google Scholar]
- 9.Wallingford KM, Snyder EM: Occupational exposures during the World Trade Center disaster response. Toxicol Ind Health 2001, 17:247–253. [DOI] [PubMed] [Google Scholar]
- 10.Diaz-Sanchez D, Tsien A, Casillas A, et al. : Enhanced nasal cytokine production in human beings after in vivo challenge with diesel exhaust particles. J Allergy Clin Immunol 1996, 98:114–123. [DOI] [PubMed] [Google Scholar]
- 11.Berríos-Torres SI, Greenko JA, Phillips M, et al. : World Trade Center rescue worker injury and illness surveillance, New York, 2001. Am J Prev Med 2003, 25:79–87. [DOI] [PubMed] [Google Scholar]
- 12.Irwin RS, Madison JM: The diagnosis and treatment of cough. N Engl J Med 2000, 343:1715–1721. [DOI] [PubMed] [Google Scholar]
- 13.Prezant DJ, Weiden M, Banauch GI, et al. : Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med 2002, 347:806–815. [DOI] [PubMed] [Google Scholar]
- 14.Herbstman JB, Frank R, Schwab M, et al. : Respiratory effects of inhalation exposure among workers during the clean-up effort at the World Trade Center disaster site. Environ Res 2005, 99:85–92. [DOI] [PubMed] [Google Scholar]
- 15.Skloot G, Goldman M, Fischler D, et al. : Respiratory symptoms and physiologic assessment or ironworkers at the World Trade Center disaster site. Chest 2004, 125:1248–1255. [DOI] [PubMed] [Google Scholar]
- 16.Salzman SH, Moosavy FM, Miskoff JA, et al. : Early respiratory abnormalities in emergency services police officers at the World Trade Center site. J Occup Environ Med 2004, 46:113–122. [DOI] [PubMed] [Google Scholar]
- 17.Webber MP, Gustave J, Lee R, et al. : Trends in respiratory symptoms of firefighters exposed to the World Trade Center disaster: 2001–2005. Environ Health Perspect 2009, 117:975–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farfel M, DiGrande L, Brackbill R, et al. : An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health 2008, 85:880–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.••. de la Hoz RE, Shohet MR, Chasan R, et al. : Occupational toxicant inhalation injury: the World Trade Center (WTC) experience. Int Arch Occup Environ Health 2008, 81:479–485. This is the largest clinical study published to date that characterizes the different diseases that account for the symptoms reported by former WTC site workers.
- 20.Belafsky PC, Postma GN, Koufman JA: The validity and reliability of the reflux finding score (RFS). Laryngoscope 2001, 111:1313–1317. [DOI] [PubMed] [Google Scholar]
- 21.Settipane RA, Lieberman P: Update on nonallergic rhinitis. Ann Allergy Asthma Immunol 2001, 86:494–508. [DOI] [PubMed] [Google Scholar]
- 22.de la Hoz RE, Hill S, Chasan R, et al. : Health care and social issues of immigrant rescue and recovery workers at the World Trade Center site. J Occup Environ Med 2008, 50:1329–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.••. de la Hoz RE, Shohet MR, Wisnivesky JP, et al. : Atopy and upper and lower airway disease among former World Trade Center workers and volunteers. J Occup Environ Med 2009, 51:992–995. This was a study of a commonly investigated potential risk factor for occupational airway diseases.
- 24.Young T, Finn L, Palta M: Chronic nasal congestion at night is a risk factor for snoring in a population-based cohort study. Arch Intern Med 2001, 161:1514–1519. [DOI] [PubMed] [Google Scholar]
- 25.de la Hoz RE, Aurora RN, Landsbergis P, et al. : Snoring and obstructive sleep apnea among former World Trade Center rescue workers and volunteers. J Occup Environ Med 2010, 52:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNicholas WT: The nose and OSA: variable nasal obstruction may be more important in pathophysiology than fixed obstruction. Eur Respir J 2008, 32:3–8. [DOI] [PubMed] [Google Scholar]
- 27.Zanation AM, Senior BA: The relationship between extraesophageal reflux (EER) and obstructive sleep apnea (OSA). Sleep Med Rev 2005, 9:453–458. [DOI] [PubMed] [Google Scholar]
- 28.Redolfi S, Yumino D, Ruttanaumpawan P, et al. : Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med 2009, 179:241–246. [DOI] [PubMed] [Google Scholar]
- 29.de la Hoz RE, Christie J, Teamer J, et al. : Reflux symptoms and disorders and pulmonary disease in former World Trade Center rescue and recovery workers and volunteers. J Occup Environ Med 2008, 50:1351–1354. [DOI] [PubMed] [Google Scholar]
- 30.de la Hoz RE, Shohet MR, Bienenfeld LA, et al. : Vocal cord dysfunction in former World Trade Center (WTC) rescue and recovery workers. Am J Ind Med 2008, 51:161–165. [DOI] [PubMed] [Google Scholar]
- 31.Perkner JJ, Fennelly KP, Balkissoon R, et al. : Irritant-associated vocal cord dysfunction. J Occup Environ Med 1998, 40:136–143. [DOI] [PubMed] [Google Scholar]
- 32.Allan PF, Abouchahine S, Harvis L, et al. : Progressive vocal cord dysfunction subsequent to a chlorine gas exposure. J Voice 2006, 20:291–296. [DOI] [PubMed] [Google Scholar]
- 33.Irwin RS, Pratter MR, Holland PS, et al. : Postnasal drip causes cough and is associated with reversible upper airway obstruction. Chest 1984, 85:346–352. [DOI] [PubMed] [Google Scholar]
- 34.Williams AN, Simon RA, Woessner KM: Sinusitis and chronic progressive exercise- induced cough and dyspnea. Allergy Asthma Proc 2008, 29:669–675. [DOI] [PubMed] [Google Scholar]
- 35.Brown TM, Merritt WD, Evans DL: Psychogenic vocal cord dysfunction masquerading as asthma. J Nerv Ment Dis 1988, 176:308–310. [DOI] [PubMed] [Google Scholar]
- 36.Moscato G, Vandenplas O, Van Wijk G, et al. : Occupational rhinitis. Allergy 2008, 63:969–980. [DOI] [PubMed] [Google Scholar]
- 37.Long A, McFadden C, DeVine D, et al. : Management of Allergic and Nonallergic Rhinitis. AHRQ Evidence Report/Technology Assessment, No. 54. Rockville, MD: Agency for Healthcare Research and Quality; 2002 [PMC free article] [PubMed] [Google Scholar]
- 38.••. Wallace DV, Dykewicz MS, Bernstein DI, et al. : The diagnosis and management of rhinitis. J Allergy Clin Immunol 2008, 122: S1–S84. This is an authoritative, comprehensive, and up-to-date guideline on the diagnosis and treatment of rhinitis.
- 39.Shusterman D, Murphy MA, Balmes J: Influence of age, gender, and allergy status on nasal reactivity to inhaled chlorine. Inhal Toxicol 2003, 15:1179–1189. [DOI] [PubMed] [Google Scholar]
- 40.Shusterman D, Tarun A, Murphy MA, et al. : Seasonal allergic rhinitic and normal subjects respond differentially to nasal provocation with acetic acid vapor. Inhal Toxicol 2005, 17:147–152. [DOI] [PubMed] [Google Scholar]
- 41.Siracusa A, Desrosiers M, Marabini A: Epidemiology of occupational rhinitis: prevalence, aetiology and determinants. Clin Exp Allergy 2000, 30:1519–1534. [DOI] [PubMed] [Google Scholar]
- 42.Mapp CE, Boschetto P, Maestrelli P, et al. : Occupational asthma. Am J Respir Crit Care Med 2005, 172:280–305. [DOI] [PubMed] [Google Scholar]
- 43.Brackbill RM, Hadler JL, DiGrande L, et al. : Asthma and posttraumatic stress symptoms 5–6 years following exposure to the World Trade Center terrorist attack. JAMA 2009, 302:502–516. [DOI] [PubMed] [Google Scholar]