Abstract
Background:
Bariatric endoscopy has emerged for non-surgical treatment of obesity, providing a treatment option for weight loss and associated comorbidities. Outcomes of endoscopic sleeve gastroplasty (ESG) of 12 months have been published by our team and there is a need for longer follow-up period understanding the effects of ESG techniques.
Aim:
This report emphasises on weight loss pattern in follow-up time points and monitors the post-procedure improvement in comorbidities with minimum 4-year follow-up of patients undergoing ESG at a single academic centre in India.
Subjects and Methods:
This was a prospective cohort study. All procedures were performed by the same surgeon. Patients with a body mass index of >30 kg/m2 (or >27 with comorbidities) underwent ESG for treatment of obesity. Patients were systematically followed yearly after their procedure. Data collected on the primary outcome and secondary outcomes were analysed and presented.
Results:
612 patients (69.3% female) with a mean age of 40.70 ± 12.66 years and mean body mass index of 34.30 ± 5.05 kg/m2 underwent ESG. Out of 612 patients, follow-up rates for a 1-2-3 and 4 years were 93.1%, 90.2%, 81.7% and 81.9%, respectively. The mean percentage total body weight loss was 18.19% (95% confidence interval [CI]: 17.72–18.57) and %EWL was 49.30% (95% CI: 48.91–49.68) with 90% of participants-maintaining a percentage of total weight loss of ≥5% and 70% of patients maintaining an EWL of ≥25% at 4 years, respectively. Resolution/improvement of comorbidities was 51.2% cases of T2DM, 65.8% cases of hypertension, 73.6% cases of dyslipidaemia and 89.9% remission were in obstructive sleep apnoea. No patient required an emergency intervention, and there was no mortality or significant morbidity.
Conclusions:
This study shows acceptable results with ESG at 4 years in our unit. Regular monitoring by a multidisciplinary nurtures weight loss, resolution or improvement of comorbidities and improvement of quality of life with low perioperative complications. There is a need for more reports with this approach to determine the amount and duration of weight loss outcome and medical intervention.
Keywords: Bariatrics, endoscopic sleeve gastroplasty, endoscopy, obesity, weight loss
INTRODUCTION
Obesity has become a public health concern affecting different age groups in worldwide and reducing quality of life.[1] The most effective method for controlling obesity and metabolic disorder is bariatric surgery, which is more effective than diet and exercise or pharmacologic approaches.[2] In spite of that, the giant majority of qualifying patients never undergo bariatric surgery, given matters with access and cost and fear of its related with real and perceived morbidity associated with surgery.[3]
Recently, bariatric endoscopy has emerged for non-surgical treatment of obesity, providing a treatment option for weight loss and associated comorbidities.[4] In 2008, Fogel et al. and 2010 Brethauer et al.[5,6] showed the viability of endoscopic gastric volume reduction for the management of obesity using a superficial endoscopic suturing device that mimicked vertical banded gastroplasty surgical anatomy. In 2013, Abu Dayyeh et al. verified the viability of creating a full endoscopic sleeve gastroplasty (ESG) that decreases the entire stomach through creation of a small-diameter sleeve along the lesser curvature of the stomach.[7] Since then, clinical experiences with ESG have been published. Existing data, including our earlier published report, suggest an average percentage of total weight loss (%TWL) of 10%–20% at 6 months to 1 year after ESG.[8–11] Given the relatively recent adoption of ESG by bariatric surgeon, there is a lack of data on its long-term effectiveness beyond 1 year after the procedure. In this paper, we provide 4-year outcomes after ESG in cohort of patients with obesity. Numerous factors may affect a patient’s outcome in long term. The main objective of this study is to assess the weight loss pattern (such as %TWL and %EWL) in follow-up time points and monitor the post-procedure adverse events (AEs). Secondary outcomes included post-procedure hospital length of stay as well as resolution or improvement of comorbidities within 90 days.
SUBJECTS AND METHODS
Patients and study design
All patients who underwent ESG were prospectively enrolled in our database. This study is a part of longitudinal study conducted at high volume centre of a prospectively maintained cohort data. The institutional ethical committee (Hospital centre and University) approved this study (SAIMS/IEC/2019/56) and was registered at clinical trials registry-India (REF/2019/07/027153). The inclusion criteria for undergoing ESG procedure included body mass index (BMI) of >30 kg/m2 (or >27 with comorbidities). Written informed consent was obtained from all patients. All patients were restricted to a full liquid diet for the first 2 weeks after the procedure, then advanced to a modified bariatric diet for four additional weeks as previously described.
Endoscopic sleeve gastroplasty procedure
Procedure has described in prior published reports by our group.[10]
Data collection
Patient’s demographic (age, sex, weight loss requirement), clinical (comorbidities), anthropometric (weight, height), treatment (operation duration) and post-operative outcome (weight loss, comorbidities remission, early complications, post-operative ESG concerns) data were prospectively documented (electronic health-care records). Baseline and follow-up examinations included assessment of weight and height as before, with BMI calculated as weight in kilograms divided by the square of height in meters. Weight measurements were performed at the baseline before the procedure, as well as during scheduled follow-up visits at 1, 3, 6, 12 and 24 months after the procedure. Afterward, patients were encouraged to continue to have a minimum of yearly follow-up visits (including video and phone calls) and to follow the prescribed diet.
Study endpoint
The primary study endpoint included present follow-up and %TWL or percentage of excess weight loss (%EWL) and post-procedure adverse events (Ads): Nausea, constipation, abdominal pain and generalised weakness. Secondary outcomes included post-procedure hospital length of stay as well as resolution/improvement of comorbidities.
Statistical analysis
Descriptive analyses of the variables were carried out using the test of proportions for qualitative variables and measurements of central tendency (mean) and measures of dispersion (standard deviation) for quantitative variables. To assess demographic variables (i.e., age, height, gender, initial weight and BMI etc.) we used Student’s test for independent samples (continuous variables) and Chi squared test (qualitative variables) to contributed better response rates. We used Student’s test for independent samples (continuous variables) and Chi-squared test (qualitative variables). The analysis included using the starting weight as covariate for %TWL and 95% confidence interval (CI) was used for comparing the responder rate. All P values presented are two-tailed, and statistical significance was defined a priori as P < 0.05. Data analysis was done using IBM SPSS Statistics 20; IBM, Armonk, NY, USA.
RESULTS
In total, 612 patients were included in the analysis; females were dominant 424 (69.3%). Baseline characteristic of the study cohorts is summarised in Table 1. Patients had a mean age of 40.70 ± 12.65 years and mean BMI of 34.30 ± 5.05 kg/m2. Among total 612 patients, all patients were eligible for 2-year follow-up. And out of 612, 570 patients were eligible for 3rd-year follow-up and 310 patients were eligible for the 4th-year follow-up time points representing a 1-, 2-,3 and 4-year follow-up rate of 570 (93.1%), 552 (90.2%), 466 (81.7%) and 254 (81.9%), respectively [Figure 1]. None of the patients had a history of prior balloon placement or bariatric surgery. Out of all, 271 (44.2%) were diabetic (T2DM), 366 (59.8%) had hypertension (HTN), 446 (72.8%) had obstructive sleep apnoea (OSA) and 410 (67%) had dyslipidaemia (DLP) [Table 1].
Table 1.
Patient characteristics of 612 patients
| Characteristic | Total (n=612), n (%) |
|---|---|
| Age (years) | 40.70±12.66 |
| Height (m) | 160.96±15.48 |
| Gender (female) | 424 (69.3) |
| Weight (kg) | 90.37±16.61 |
| BMI (kg/m2) | 34.30±5.05 |
| Diabetes | 271 (44.2) |
| Hypertension | 366 (59.8) |
| Sleep apnoea | 446 (72.8) |
| Dyslipidaemia | 410 (67.0) |
BMI: Body mass index
Figure 1.
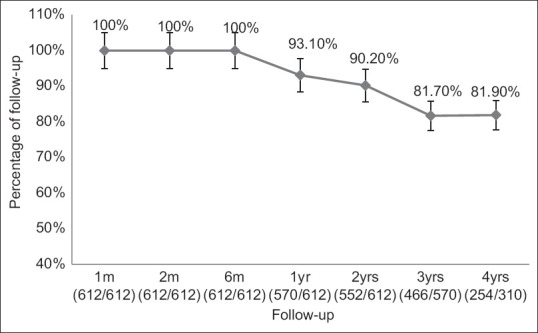
Follow-up pattern
Primary outcome
Percentage of total weight loss
At 6 months, mean %TWL was 12.6% (95% CI: 9.28–19.06, P < 0.001) with 575 patients and 94% of patients achieved ≥5% TWL. At 1 year, mean %TWL was 21.20% (95% CI: 20.81–21.59, P < 0.001) with 558 and 98% of patients achieved ≥5% TWL, respectively. At 2 years, mean %TWL was 20.05% (95% CI: 19.61–20.48, P < 0.001) with 513 and 93% of patients achieved ≥5% TWL, respectively. At 3 years, mean %TWL was 18.74% (95% CI: 18.31–19.12, P < 0.001) with 425 and 91% of patients maintained ≥5% TWL, respectively. At 4 years, mean %TWL was 18.19% (95% CI: 17.72-18.57, P < 0.001) with 229 and 90% of patients maintained ≥5% TWL, respectively. Patients %TWL at their nadir weight after ESG had a mean of 18.9% (95% CI: 18.5–19.3). Patients’ mean weight gain after nadir was 3.5 Kg until the end of the follow-up period (95% CI: 3.1–3.3 Kg) [Table 2].
Table 2.
Weight loss observation during follow-up
| F/W | P | TWL | EWL | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| 95% CI | %TWL | ≥5% TWL (%) | 95% CI | %EWL | ≥25% EWL (%) | ||
| 1 month | 0.001 | 9.28-9.45 | 9.41±1.66 | 92 | 35.93-36.72 | 36.34±2.12 | 87 |
| 3 months | 0.001 | 12.90-13.66 | 13.28±4.80 | 94 | 39.82-40.68 | 40.24±2.34 | 90 |
| 6 months | 0.001 | 18.31-19.06 | 18.68±4.52 | 97 | 53.26-54.06 | 53.68±4.53 | 90 |
| 1 year | 0.001 | 20.81-21.59 | 21.20±4.70 | 98 | 56.51-57.30 | 56.92±6.54 | 92 |
| 2 years | 0.001 | 19.61-20.48 | 20.05±5.23 | 93 | 54.03-54.80 | 54.42±4.45 | 80 |
| 3 years | 0.001 | 18.31-19.12 | 18.74±4.06 | 91 | 50.71-51.48 | 51.10±4.61 | 70 |
| 4 years | 0.001 | 17.72-18.57 | 18.19±5.02 | 90 | 48.91-49.68 | 49.30±3.22 | 70 |
| Nadir | 0.001 | 17.61-19.71 | 18.9±6.23 | 90 | 49.81-50.51 | 50.20±3.6 | 70 |
TWL: Total weight loss, %TWL: Percentage of TWL, EWL: Excess weight loss, %EWL: Percentage of EWL, CI: Confidence interval, F/W: Follow-up
Percentage of excess weight loss (%EWL)
We have described briefly the %EWL in Table 2 as at 1-year mean %EWL was 56.9% (95% CI: 56.51–57.30, P < 0.001) with 513 and 90% of patients achieved ≥25% EWL. At 2 years, mean %EWL was 54.4% (95% CI: 54.03–54.80, P < 0.001) with 442 and 80% of patients maintained ≥25% EWL. At 3 years, mean %EWL was 50.1% (95% CI: 49.71–50.08, P < 0.001) with 327 and 70% of patients maintained ≥25% EWL. At 4 years, mean %EWL was 49.3% (95% CI: 48.91–49.68, P < 0.001) with 177 and 70% of patients maintained ≥25% EWL. Patients %EWL at their nadir weight after ESG had a mean of 57.2% (95% CI: 56.8–57.5).
Adverse events
Immediate post-operative complications include 217 (35.45%) patients with nausea, 108 (17.6%) with vomiting, 75 (12.25%) with bloating, 284 (46.4%) with abdominal pain and 16 (2.6%) with generalised weakness, respectively, shown in Table 3 but there was no adverse serious event.
Table 3.
Post-operative complications
| AEs | n (%) |
|---|---|
| Nausea | 217 (35.45) |
| Vomiting | 108 (17.6) |
| Bloating | 75 (12.25) |
| Abdominal pain | 284 (46.4) |
| Generalised weakness | 16 (2.6) |
AEs: Adverse events
Secondary outcome
The mean duration of surgery was 61.96 ± 2.1 min (range, 45.2–121.1) and hospital stay were 3 days (range, 2–4 days). Resolution/improvement of comorbidities was as follows: 121 of 236 (51.2%) cases of T2DM, 216 of 328 (65.8%) cases of HTN, 410 of 302 (73.6%) cases of DLP and OSA were in 401 (89.9%) remission [Figure 2].
Figure 2.
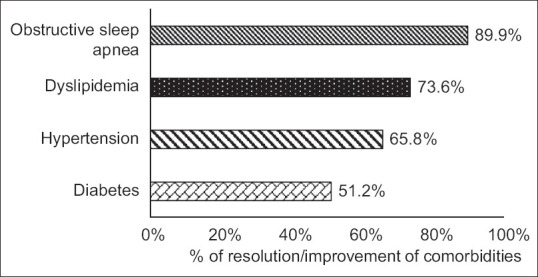
Resolution/improvement of comorbidities
Out of all 41 patients, 6.7% were readmitted for assessment. 22 (3.6%) underwent revision or redo ESG during the study period, 2 of whom had completed 1 year of follow-up. Nineteen patients (3.1%) were revised to sleeve gastrectomy and underwent the revision after 12 months of primary ESG, due to weight regain. There were no clinical signs that necessitated further evaluation. No patient required an emergency intervention, and there was no mortality or significant morbidity.
DISCUSSION
Our results suggest that ESG is safe and effective, with durable long-term results for at least up to 4 years after the procedure. We found an average 18.19% TWL and 49.30% EWL at 4 years after the procedure. Maximum (21% TWL) weight loss is generally achieved by 1 year after the procedure, after which patients tend to regain about 10% of their lost weight. Our weight loss outcomes showed ESG to be highly effective at promoting weight loss from 1st month to up to 4 years with 90% patients consistently maintaining a ≥5% TWL or more. It is proving that ESG procedure is one of the widely available options giving its safety and short to long-term effectiveness.
There is a lack of data on its long-term effectiveness beyond 2 years after the ESG procedure. To the best of our knowledge, this is the first large single-centre cohort study of patients with obesity from India, presenting our outcome data for up to 4 years after ESG. Earlier studies, including reports from our own group, had shown that ESG is safe and effective for up to 1 year after the procedure, and young age and female gender are related to better outcomes.[10] In a previous report on 42 patients who underwent ESG at our centre, we reported a %TWL of 19.94 ± 4.89 at 1 year after the procedure.[10] A similar study by Lopez-Nava et al. in 2017 reported a %TWL of 18.6% at 2 years after ESG.[12] A recent multicentre international study on 193 patients reported a %TWL of 15% at 1 year after the procedure,[13] and a recent meta-analysis of studies published between 2016 and 2019 reported a %TWL of 17.2% (95% CI; 14.6–19.7) at 18–24 months.[14] Compared to these results, we have been able to show for the first time that weight loss after ESG is consistently maintaining with an average %TWL of nearly 18.9% at the end of the follow-up. Importantly, we were able to show that patient’s weight is largely stable from 2 to 4 years after the procedure, a promising finding regarding long-term effectiveness of ESG even beyond 4 years. It is important to note that 90% of participants maintained a %TWL of ≥5%, and 70% of patients maintained an EWL of ≥25% at 4 years. These weight loss results with a number needed to treat of 1.1 to reach %TWL of 5% or more at long term are clinically significant according to earlier studies proving improvement in obesity-related comorbidities such as insulin resistance and T2DM, DLP and HTN with %TWL of 5% or more.[15] In our cohort, we found resolution/improvement of comorbidities; 51.2% in T2DM, 65.8% in HTN, 73.6% in DLP and OSA were in 89.9% remission.
Regarding safety data, the majority of our patients experienced at least one minor AEs among which abdominal pain and nausea were the most common; they were treated conservatively and symptoms were resolved during the hospital stay. Nonetheless, there were no serious AEs and no need for any further interventional procedures. These findings are in accordance with most previous studies, except for slightly lower rates of abdominal pain and nausea. Although we found rates of 46% and 35%, respectively, some articles show rates of up to 80% for each of these symptoms.[16–20] The long-term durability of ESG, our results suggest that ESG is safe, with no severe or fatal AEs in our cohort, consistent with the available literature.[16]
Furthermore, in our study, post-procedural pharmacotherapy in these patients was able to prevent further weight gain but did not lead to significant additional weight loss. Similarly, we were able to show that only 5 (0.8%) patients underwent revision or redo during the study period. In our cohort, 2 (0.3%) patients were revised to sleeve gastrectomy and underwent the revision after 12 months of primary ESG, due to weight regain and 3 (0.4%) patients had reversal redo-ESG. It is important to recognise that obesity is considered a multifactorial disease with a strong genetic component, and patients cannot truthfully expect a one-time treatment to be successful without a comprehensive and multidisciplinary post-procedural care plan, including nutritional, psychiatric and endocrinology care. Finally, we found that ESG is effective and safe at promoting weight loss in an Indian population during the study period. Promising outcomes and development of new endoscopic techniques allow the large academic centres to play an increasingly important role in the management of obesity. These findings are important regarding planning and standardisation of ESG training, both during a therapeutic or bariatric endoscopy fellowship, as well as for independent gastroenterologists who would like to add ESG to their practice, to ensure safety and reproducible outcomes.[17]
Our study limitation is bounded due to the deficit of a control group, and since we have an absolute follow-up rate of 93% in the 1st year, 90% in the 2nd year, 81% in the 3rd year and 81% in the 4th year, respectively, there is still possibility/potential for differential loss to follow-up to influence the findings. Moreover, the results which we are providing represent practice at an academic centre with a consequential/remarkable experience in bariatric endoscopy where patients are tremendously motivated (about 70% self-paying) and are also supervised by a devoted multidisciplinary team, and hence, our outcomes might not be straightly generalisable to further settings. In conclusion, we showed that ESG can be a reliable and effective procedure acceptable to patients. Significant weight loss occurs during without mortality or major morbidity. However, long-term follow-up appears to be associated with weight gain. Regular monitoring by a multidisciplinary team is a key measure to success, we think that renewed weight gain can be partially prevented by close clinical follow-up. There is a need for long-term follow-up of large randomised controlled studies to define the indications for ESG.
CONCLUSION
Our results suggest that ESG is safe and effective for treatment of obesity, with reliable long-term results for at least up to four years after the procedure. Regular monitoring by a multidisciplinary team improves the quality of life with low perioperative complications. This procedure should be considered as a reliable option for treatment of obesity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Our Institute would like to acknowledge Dr Manoel Galvao Neto, joined our Institute as Clinical Director-Dept Bariatric Endoscopy for his valuable guidance and support.
REFERENCES
- 1.Rønningen R, Wammer AC, Grabner NH, Valderhaug TG. Associations between lifetime adversity and obesity treatment in patients with morbid obesity. Obes Facts. 2019;12:1–13. doi: 10.1159/000494333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, et al. Bariatric surgery versus non-surgical treatment for obesity:A systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f5934. doi: 10.1136/bmj.f5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ASGE Bariatric Endoscopy Task Force. Sullivan S, Kumar N, Edmundowicz SA, Abu Dayyeh BK, Jonnalagadda SS, Larsen M, et al. ASGE position statement on endoscopic bariatric therapies in clinical practice. Gastrointest Endosc. 2015;82:767–72. doi: 10.1016/j.gie.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 4.Abu Dayyeh BK, Thompson CC. Obesity and bariatrics for the endoscopist:New techniques. Therap Adv Gastroenterol. 2011;4:433–42. doi: 10.1177/1756283X11398737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fogel R, De Fogel J, Bonilla Y, De La Fuente R. Clinical experience of transoral suturing for an endoluminal vertical gastroplasty:1-year follow-up in 64 patients. Gastrointest Endosc. 2008;68:51–8. doi: 10.1016/j.gie.2007.10.061. [DOI] [PubMed] [Google Scholar]
- 6.Brethauer SA, Chand B, Schauer PR, Thompson CC. Transoral gastric volume reduction for weight management:Technique and feasibility in 18 patients. Surg Obes Relat Dis. 2010;6:689–94. doi: 10.1016/j.soard.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty:A potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530–5. doi: 10.1016/j.gie.2013.04.197. [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Nava G, Galvao M, Bautista-Castaño I, Fernandez-Corbelle JP, Trell M. Endoscopic sleeve gastroplasty with 1-year follow-up:Factors predictive of success. Endosc Int Open. 2016;4:E222–7. doi: 10.1055/s-0041-110771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopez-Nava G, Galvão MP, da Bautista-Castaño I, Jimenez A, De Grado T, Fernandez-Corbelle JP. Endoscopic sleeve gastroplasty for the treatment of obesity. Endoscopy. 2015;47:449–52. doi: 10.1055/s-0034-1390766. [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Jain S, Mathur W, Kosta S, Neto MG, Brunaldi VO, et al. Endoscopic sleeve gastroplasty is an effective and safe minimally invasive approach for treatment of obesity:First Indian experience. Dig Endosc. 2020;32:541–6. doi: 10.1111/den.13508. [DOI] [PubMed] [Google Scholar]
- 11.Sharaiha RZ, Kedia P, Kumta N, DeFilippis EM, Gaidhane M, Shukla A, et al. Initial experience with endoscopic sleeve gastroplasty:Technical success and reproducibility in the bariatric population. Endoscopy. 2015;47:164–6. doi: 10.1055/s-0034-1390773. [DOI] [PubMed] [Google Scholar]
- 12.Lopez-Nava G, Sharaiha RZ, Vargas EJ, Bazerbachi F, Manoel GN, Bautista-Castaño I, et al. Endoscopic sleeve gastroplasty for obesity:A multicenter study of 248 patients with 24 months follow-up. Obes Surg. 2017;27:2649–55. doi: 10.1007/s11695-017-2693-7. [DOI] [PubMed] [Google Scholar]
- 13.Barrichello S, Hourneaux de Moura DT, Hourneaux de Moura EG, Jirapinyo P, Hoff AC, Fittipaldi-Fernandez RJ, et al. Endoscopic sleeve gastroplasty in the management of overweight and obesity:An international multicenter study. Gastrointest Endosc. 2019;90:770–80. doi: 10.1016/j.gie.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, Adam A, Neto MG, Badurdeen D, et al. Efficacy and safety of endoscopic sleeve gastroplasty:A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2020;18:1043–53. doi: 10.1016/j.cgh.2019.08.022. e4. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–6. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Storm AC, Abu Dayyeh BK. Endoscopic sleeve gastroplasty for obesity:Defining the risk and reward after more than 1600 procedures. Gastrointest Endosc. 2019;89:1139–40. doi: 10.1016/j.gie.2019.02.025. [DOI] [PubMed] [Google Scholar]
- 17.Shahnazarian V, Ramai D, Sarkar A. Endoscopic bariatric therapies for treating obesity:A learning curve for gastroenterologists. Transl Gastroenterol Hepatol. 2019;4:16. doi: 10.21037/tgh.2019.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharaiha RZ, Hajifathalian K, Kumar R, Saunders K, Mehta A, Ang B, et al. Five-year outcomes of endoscopic sleeve gastroplasty for the treatment of obesity. Clin Gastroenterol Hepatol. 2021;19:1051–7. doi: 10.1016/j.cgh.2020.09.055. e2. [DOI] [PubMed] [Google Scholar]
- 19.Li P, Ma B, Gong S, Zhang X, Li W. Efficacy and safety of endoscopic sleeve gastroplasty for obesity patients:a meta-analysis. Surg Endosc. 2020;34:1253–60. doi: 10.1007/s00464-019-06889-6. [DOI] [PubMed] [Google Scholar]
- 20.Carr P, Keighley T, Petocz P, Blumfield M, Rich GG, Cohen F, et al. Efficacy and safety of endoscopic sleeve gastroplasty and laparoscopic sleeve gastrectomy with 12+months of adjuvant multidisciplinary support. BMC Prim Care. 2022;23:26. doi: 10.1186/s12875-022-01629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


