Abstract
Background.
Some personality characteristics have previously been associated with an increased risk for psychiatric disorder. Longitudinal studies are required in order to tease apart temporary (state) and enduring (trait) differences in personality among individuals with bipolar disorder (BD). This study aimed to determine whether there is a characteristic personality profile in BD, and whether associations between BD and personality are best explained by state or trait effects.
Method.
A total of 2247 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder study completed the NEO Five-Factor Inventory administered at study entry, and at 1 and 2 years.
Results.
Personality in BD was characterized by high neuroticism (N) and openness (O), and low agreeableness (A), conscientiousness (C) and extraversion (E). This profile was replicated in two independent samples, and openness was found to distinguish BD from major depressive disorder. Latent growth modeling demonstrated that manic symptoms were associated with increased E and decreased A, and depressed symptoms with higher N and lower E, A, C and O. During euthymic phases, high N and low E scores predicted a future depression-prone course.
Conclusions.
While there are clear state effects of mood on self-reported personality, personality variables during euthymia predict future course of illness. Personality disturbances in extraversion, neuroticism and openness may be enduring characteristics of patients with BD.
Keywords: Bipolar disorder, extraversion, NEO-FFI, neuroticism, personality
Introduction
Trait theories of personality propose lifelong, stable dimensions distributed as a continuum in the population. Current research suggests five high-level traits: neuroticism (N), extraversion (E), openness to experience (O), agreeableness (A) and conscientiousness (C) (Goldberg, 1993; McCrae & Costa, 1997), which are found across all cultures (McCrae & Terracciano, 2005).
For some traits, extreme scores confer an increased likelihood of a psychiatric diagnosis. High neuroticism and low extraversion are associated with a range of disorders (Eysenck & Rachman, 1965), including social phobia and agoraphobia (Solyom et al. 1986; Trull & Sher, 1994), psychosis (Van Os & Jones, 2001) and post-traumatic stress disorder (Cox et al. 2004a). Elevated neuroticism scores are common among patients with major depressive disorder (MDD) (Hirschfeld & Klerman, 1979; Trull & Sher, 1994; Enns & Cox, 1997), including pre-morbidly (Rodgers, 1990; Furukawa et al. 1998), and among their healthy relatives (Maier et al. 1992; Modell et al. 2003), suggesting that neuroticism and depression may share genetic influences (e.g. Rietschel et al. 2008). Extraversion-related traits may differentiate bipolar and unipolar affective disorders (Akiskal et al. 1983, 2006). Comparisons of groups of individuals with common psychiatric diagnoses including mood and anxiety disorders confirm widespread, but often subtle, differences in personality profile (e.g. Rector et al. 2002). A recent study comparing personality across a range of internalizing disorders found that individuals with bipolar disorder (BD; n=87) scored significantly higher than a large sample of community controls in neuroticism, openness and conscientiousness, and in general had notably higher extraversion and openness scores than other diagnostic groups (Rector et al. 2002; Tackett et al. 2008). While these associations between normal personality and DSM-IV Axis I diagnoses may be of great theoretical and etiological importance, much of the present literature is based on studies assessing relatively few individuals (Young et al. 1995; Bagby et al. 1997; Heerlein et al. 1998; Jain et al. 1999).
Associations between personality traits and psychiatric disorders may occur for several reasons, including ‘scarring’ of personality by mood episodes, shared genetic risk for personality and disorder, or methodological artifacts such as overlapping items in symptom and personality rating scales (Shea et al. 1996; Duggan et al. 2003; Foster & MacQueen, 2008). The relationship between personality and symptoms is particularly complex in BD because personality scores can be affected by mood state (Kendell & DiScipio, 1968; Reich et al. 1987) and by residual symptoms present even during euthymic states (Katz & McGuffin, 1987; Sauer et al. 1997). In addition, personality may modify the effects of psychiatric symptoms and affect the course of illness (Heerlein et al. 1998; Lozano & Johnson, 2001).
BD is a condition in which hypotheses about personality and mental health present unique challenges. Separating the influences of mood-related state and underlying trait effects requires that personality be assessed during periods of active symptoms and euthymia. In this study, we assessed mood and personality repeatedly in large BD samples. We predicted that personality in BD would be characterized by higher neuroticism and extraversion than population means, and that individuals with BD and MDD would differ on some traits. Second, we predicted significant ‘ state ’ effects: mood at the time of assessment would explain significant variation in personality scores. Third, we predicted ‘ trait ’ effects of personality on illness course, i.e. enduring, biologically based individual differences that are not due to current symptoms and that differ between manic-prone and depression-prone individuals. We investigated the associations between personality and predominant polarity because of recent evidence that predominant polarity affects clinical features of BD, including delay before diagnosis, type of mood episode and age at illness onset, duration of illness and suicide attempts (Rosa et al. 2008).
Method
Subjects
The Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study comprised a number of randomized controlled trials incorporated into a large, multi-site, naturalistic study of outcome in BD (Sachs et al. 2003). Patients eligible for STEP-BD were 15 years or over and met DSM-IV criteria for bipolar I or II disorders, cyclothymia, BD not otherwise specified (NOS), or schizo-affective disorder (manic or bipolar subtype). Written informed consent was obtained from patients aged 18 years or over and written assent and parent or guardian consent was obtained for patients aged 15–17 years. The study was approved by Institutional Review Boards of participating institutions.
Initial analyses were conducted in a subset of individuals that participated in the STEP-genetic repository (STEP-GRP) and completed a personality assessment (n=980 of 2089). Replication of results from STEP-GRP was subsequently attempted in two further samples. The first comprised a non-overlapping STEP-BD sample (n=1267) with identical recruitment and inclusion criteria. These individuals took part in the STEP-BD standard care pathway (STEP-SCP) but not the STEP-GRP. The second group [the Massachusetts General Hospital (MGH) sample] was a convenience sample of 203 individuals aged 18 years or over who met DSM-IV criteria for MDD or BD I or II as previously described (Simon et al. 2003) for whom NEO Five-Factor Inventory (NEO-FFI) personality scores were available. An overview of the three samples and the analysis framework is given in Fig. 1.
Fig. 1.
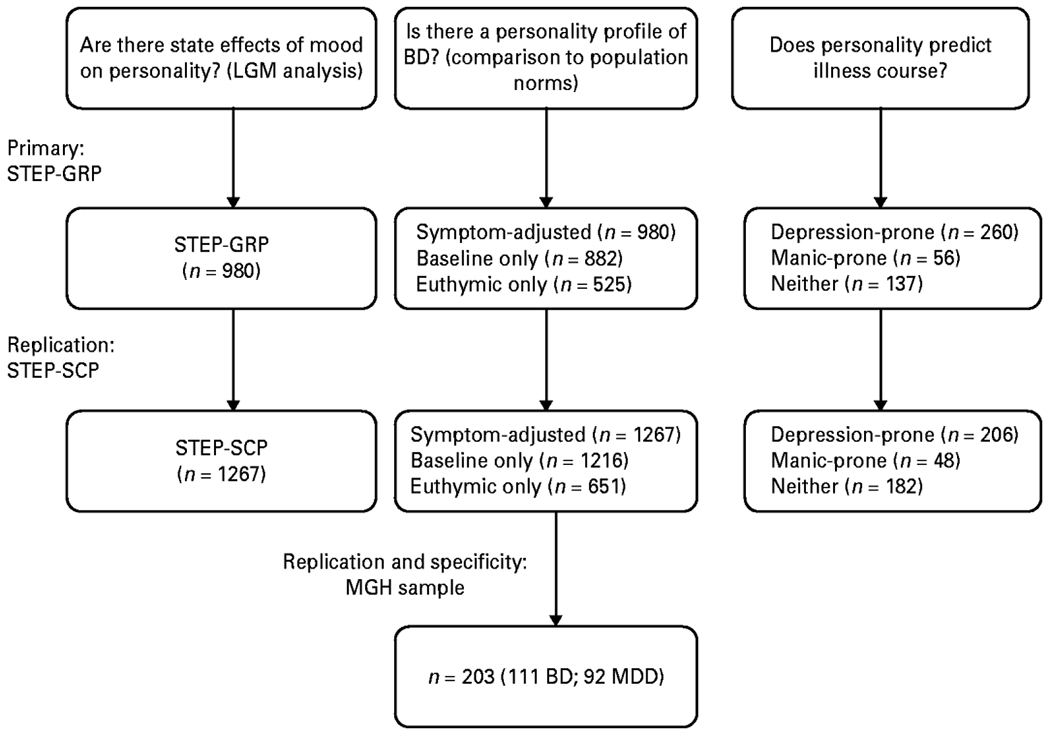
Analytic framework and samples used to investigate personality in bipolar disorder (BD). LGM, Latent growth model; STEP-GRP, Systematic Treatment Enhancement Program genetic repository ; STEP-SCP, STEP standard care pathway; MGH, Massachusetts General Hospital ; MDD, major depressive disorder.
Personality assessment: the revised NEO-FFI
Personality was assessed using the NEO-FFI (Costa & McCrae, 1992), a 60-item self-report with each item rated on a five-point scale. (The NEO-FFI was administered at the initiation of the STEP-BD study in both STEP-GRP and STEP-SCP cohorts, but was subsequently eliminated from the assessment package so is available for only a subset of each cohort.) Twelve items assess each of five personality dimensions: neuroticism (N), the tendency to experience negative affect; extraversion (E), a tendency towards energy, positive emotions, and stimulation-seeking; conscientiousness (C), a tendency towards self-discipline and dutiful behavior; openness to experience (O), sometimes described as intellectual curiosity ; and agreeableness (A), a tendency to be co-operative and compassionate. Scores were converted to sex-adjusted t scores with a (normative) mean of 50 and a standard deviation of 10 using normative data provided in the professional manual (Costa & McCrae, 1992). NEO-FFI was completed at entry, and at 1 and 2 years. For all analyses, patients were included only if a clinical rating of mood was available within 30 days of personality assessment; where more than one was available, the temporally closest was used.
In the MGH sample, NEO-FFI scores were collected on a single occasion and again converted to t scores using adult normative data (Costa & McCrae, 1992).
Clinical assessments
STEP-BD included a comprehensive battery of clinician- and self-report assessments (Sachs et al. 2003). Clinicians completed the Affective Disorders Evaluation (Sachs, 1990) at study entry and the Young Mania Rating Scale (YMRS; Young et al. 1978) and Montgomery–Asberg Depression Rating Scale (MADRS; Montgomery & Asberg, 1979) at every clinical assessment. Current clinical state was determined at each contact throughout the trial using the Clinical Monitoring Form (CMF) for mood disorders (Sachs et al. 2002) which incorporates the Structured Clinical Interview for DSM-IV (SCID-IV; First et al. 1996) current mood modules and rates frequency and intensity of mood states (Sachs et al. 2002). The CMF determines a categorical clinical status, defined as mania/hypomania if the patient is experiencing three or more symptoms of mood elevation, depression if they are experiencing five or more depressive symptoms, and euthymia if they are currently experiencing two or less symptoms (at no more than moderate levels). Observations where patients were in mixed or partially recovered states were excluded from these analyses (although the time spent in those states was included in measures of follow-up and mood state duration). Clinical state was used to determine the number of days spent depressed, manic/hypomanic and euthymic during the study. After initial assessment, whenever a patient was observed in the same mood state at two consecutive assessments, the number of days between those assessments was counted towards the ‘ tally ’ for that mood state. Where mood state changed between assessments, half of the days between were ascribed to one mood state and half to the other. Intervals between assessments were censored such that the maximum duration ascribed to a mood state prior to, or after, an assessment was 60 days. Individuals were defined as ‘depression-prone’ if they spent more days depressed than manic during the study period, as ‘manic-prone’ if they spent more days manic than depressed, and as ‘no predominant mood’ if they either spent an equal number of days depressed and manic, or if they were euthymic throughout the study period. A follow-up of >180 days between the first and last assessment was required in order to describe illness course; individuals with <180 days of follow-up were excluded from analyses concerning illness course.
In the MGH sample, diagnosis and current mood episode (no active episode, depressed, manic/hypomanic, or mixed) were established using the SCID-IV.
Statistical analysis
State effects of mood on personality
To establish the effects of varying mood states on repeated assessments of personality, we employed a latent growth model (LGM) approach. LGMs are rooted in a structural equation modeling framework (Meredith & Tisak, 1990) and use latent growth factors to account for dependency among repeat observations. The model comprised MADRS and YMRS symptom scores and sex-adjusted t scores for each personality dimension at each time point. Symptom scores were treated as time-varying covariates and simultaneously regressed on each personality trait at that time point. Individual patterns of personality scores throughout the study were summarized by two parameters: an intercept, reflecting an individual-specific symptom-adjusted score, and a slope, reflecting the mean rate of change over time. We assumed that variation in personality scores in this study would be predominantly due to individual differences in underlying (trait) personality and to (state) mood effects. Since personality is relatively stable during adulthood (Ferguson, 2010), we assumed that, relative to these other sources of variation, the effects of repeated self-report and of ageing would be small and would affect all individuals approximately equally; for these reasons, we fixed the slope term to be equal between individuals.
Model estimation was performed with Mplus 5.0 software (www.statmodel.com) and reported with maximum-likelihood parameter estimates and robust standard errors returned by the estimator=mlr option. Application of the Expectation-Maximization (EM) algorithm allowed inclusion of all available data, including patients with partially incomplete data assuming a missing at random mechanism (Rubin, 1987) which is robust to missingness contingent on variables (e.g. personality scores) contained within the model. Model fit was evaluated using the comparative fit index (CFI), Tucker–Lewis index (TLI) and Steiger’s root mean square error of approximation (RMSEA). Recommended values are RMSEA<0.06, and CFI and TLI>0.95 (Hu & Bentler, 1999).
Determination of personality in BD
To determine whether there was a characteristic personality profile in BD, we compared personality t scores from the first assessment completed by STEP-GRP patients when in a euthymic state with norms for the adult US population (mean=50, s.d.=10) (Costa & McCrae, 1992), using one-sample t tests. We then attempted to replicate this using scores from the first euthymic assessment for patients in the STEP-SCP sample.
To assess the specificity of the personality profile to BD disorder, t tests were used to compare the BD and MDD groups from the MGH sample on each personality factor. To prevent concurrent mood from confounding associations between personality and diagnosis we assessed the effects of diagnosis only in individuals in depressed or euthymic episodes using analysis of variance (ANOVA) with two factors [diagnosis (BD, MDD) and current mood episode (euthymic, depressed)].
Associations between personality and illness course
We assessed associations between euthymic personality scores and groups defined by prospective illness course using one-way ANOVA. Where significant differences were found, post hoc pairwise t tests with Bonferroni corrections were employed. Even during defined periods of euthymia, some residual mood symptoms were present, potentially confounding associations between outcome and personality. Therefore, we used multinomial logistic regressions to test whether personality predicted illness course when residual mood symptoms (measured by the YMRS and MADRS) were included in the model as a continuous covariate. Analyses predicted manic-prone or depression-prone status as categorical outcomes with ‘no predominant polarity ’ used as the reference category, with each personality factor (separately), YMRS and MADRS scores from the closest clinical assessment to the euthymic personality assessment as predictors. Initial analyses were completed in STEP-GRP and replication was attempted using identical methods in STEP-SCP.
Results
State effects of mood on personality
Personality assessment and clinical rating were available for 980 STEP-GRP participants : 641 (65%) with a diagnosis of bipolar I ; 272 (28%) with bipolar II ; 56 (6%) with bipolar NOS; and 11 (1%) with schizoaffective disorder, bipolar type. Compared with the remainder of the STEP-GRP cohort, this sample was older [mean age 44.5 (s.d.=12.6) versus 40.8 (s.d.=12.9) years, t=−6.65, degrees of freedom (df)=2087, p<0.001] and women were over-represented (61% v. 54%, χ2=10.4, df=1, p=0.001). The mean number of clinical state assessments available for each participant was 24.6 (s.d.=16.7, range 1–110), completed over a mean period of 1004 days (s.d.=445, range 0–2021 days).
These 980 individuals underwent 1529 personality assessments; 882 (90% of sample) at baseline, 428 (44%) at 12 months, and 219 (22%) at 24 months. The LGM showed a reasonable fit to the data (CFI=0.94, TLI=0.90, RMSEA=0.04) and explained the majority of variance in personality scores (r2 between 0.61 and 0.83 for each trait at each time point). Of the five traits, only neuroticism showed evidence for significant change over time (mean change = −2.37 points per year, s.e.=0.41, p<0.001).
Estimated effects of mood state on personality were largely consistent across assessments (see Table 1) although some effects were significant only at the first time point, where minimal missing data maximized statistical power to detect the effect. Depression was associated with increased neuroticism, and decreased extraversion, and conscientiousness at all time points, and with decreased agreeableness and openness at some time points. Manic symptoms were associated with increased extraversion at each assessment and with decreased agreeableness at baseline only. Mania had no reliable effect on neuroticism, openness or conscientiousness (Table 1).
Table 1.
State effects of MADRS depression and YMRS mania scores on NEO-FFI personalitya
| STEP-GRP |
STEP-SCP |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
12 Months |
24 Months |
Baseline |
12 Months |
24 Month |
|||||||
| β | p | β | p | β | p | β | p | β | p | β | p | |
| Depression | ||||||||||||
| Neuroticism | 0.16 | <0.001 | 0.27 | <0.001 | 0.38 | <0.001 | 0.20 | <0.001 | 0.25 | <0.001 | 0.37 | <0.001 |
| Extraversion | −0.23 | <0.001 | −0.25 | <0.001 | −0.20 | 0.002 | −0.22 | <0.001 | −0.27 | <0.001 | −0.28 | <0.001 |
| Openness | −0.09 | 0.02 | −0.02 | n.s | −0.11 | 0.04 | −0.10 | 0.007 | −0.09 | n.s | −0.04 | n.s |
| Agreeableness | −0.11 | 0.02 | −0.07 | n.s | −0.09 | n.s | −0.09 | 0.03 | −0.07 | n.s | −0.24 | <0.001 |
| Conscientiousness | −0.15 | 0.004 | −0.19 | <0.001 | −0.26 | <0.001 | −0.19 | <0.001 | −0.27 | <0.001 | −0.21 | 0.02 |
| Mania | ||||||||||||
| Neuroticism | 0.14 | n.s | −0.06 | n.s | 0.01 | n.s | 0.00 | n.s | −0.06 | n.s | −0.03 | n.s |
| Extraversion | 0.18 | 0.03 | 0.26 | 0.006 | 0.28 | 0.02 | 0.05 | n.s | 0.10 | 0.04 | 0.17 | 0.02 |
| Openness | 0.06 | n.s | −0.05 | n.s | 0.10 | n.s | 0.05 | n.s | 0.07 | n.s | 0.17 | 0.01 |
| Agreeableness | −0.19 | 0.02 | −0.08 | n.s | 0.06 | n.s | −0.08 | n.s | −0.08 | n.s | 0.13 | 0.047 |
| Conscientiousness | −0.05 | n.s | 0.06 | n.s | 0.20 | n.s | 0.00 | n.s | 0.02 | n.s | −0.03 | n.s |
MADRS, Montgomery–Asberg Depression Rating Scale; YMRS, Young Mania Rating Scale; NEO-FFI, NEO Five-Factor Inventory; STEP-GRP, Systematic Treatment Enhancement Program genetic repository; STEP-SCP, STEP standard care pathway; n.s., non-significant.
Regression coefficients (β) and p values reflect incremental change of one symptom point on personality factor scores.
In STEP-SCP participants, personality and clinical assessments were available for 1267 patients (41% male) with diagnoses of bipolar I (n=858, 68%), bipolar II (n=316, 25%), bipolar NOS (n=73, 6%) and schizo-affective disorder, bipolar type (n=18, 1%). These 1267 individuals underwent 1598 personality assessments; 1216 (96% of sample) at baseline, 272 (21%) at 12 months, and 110 (9%) at 24 months. As before, the LGM showed a reasonable fit to the STEP-SCP data (CFI=0.94, TLI=0.90, RMSEA=0.03) and explained the majority of variance in personality scores at each time point (r2 between 0.62 and 0.85). Neuroticism again decreased over time (mean change=−2.49 points per year, s.e.=0.55, p<0.001), and, openness also decreased over time (mean change=−1.39 points per year, s.e.=0.55, p=0.01). State effects on personality scores in STEP-SCP participants were consistent with STEP-GRP results (Table 1). As before, depressed symptoms were associated with increased N and decreased E, O, A and C. Manic symptoms were generally not associated with personality scores, although there were moderately consistent associations with increased extraversion.
Personality scores of patients with BD
Baseline, symptom-adjusted and euthymic personality scores of STEP-GRP and STEP-SCP participants can be seen in Fig. 2.
Fig. 2.
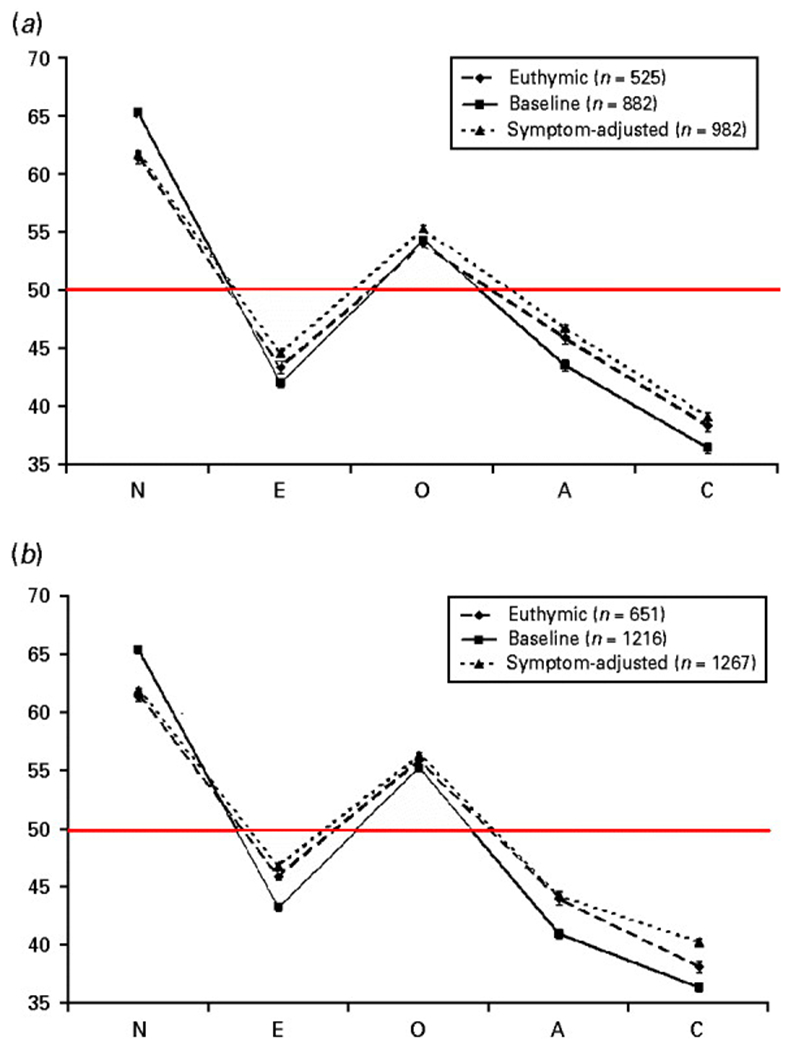
The personality profile of bipolar disorder. (a) Systematic Treatment Enhancement Program genetic repository (STEP-GRP) participants (total n=982); (b) STEP standard care pathway (STEP-SCP) participants (total n=1267). Data are NEO Five-Factor Inventory (NEO-FFI) t scores where available from study entry (–■–, n=882 and n = 1216), assessment during euthymic state (--◆--, n=525 and n=651), and symptom-adjusted scores (⋯▲⋯ n=982 and n=1267) from structural equation models. Values are means, with standard errors represented by vertical bars. —, Population mean=50 (s.d.=10) (Costa & McCrae, 1992). N, Neuroticism; E, extraversion; O, openness to experience; A, agreeableness; C, conscientiousness.
A personality assessment was completed during a euthymic state by 525 of 980 (54%) STEP-GRP patients. Compared with population norms (Costa & McCrae, 1992), the STEP-GRP euthymic state scores deviated on every factor, reporting higher neuroticism (mean t score 61.4, s.d. = 11.6) and openness (mean t score 53.9, s.d.=11.0), and lower extraversion (mean t score 43.4, s.d.=11.6), agreeableness (mean t score 46.0, s.d.=12.3) and conscientiousness (mean t score 38.4, s.d.=13.0) (t tests at 524 df, all p<0.001).
In STEP-SCP participants, personality assessment was available during a euthymic state for 651 (51%) patients. The results replicated those found in STEP-GRP participants, with scores again differing from population norms on every trait and in the same direction as STEP-GRP (all p<0.001).
Specificity of the bipolar profile
NEO-FFI scores were obtained in an independent group of patients with BD (n=111) and MDD (n=92), the MGH sample (Simon et al. 2003). These two diagnostic groups did not differ in mean age [BD=40.2 (s.d.=12.2) years, MDD=41.2 (s.d.=12.3) years, t=−0.60, df=202, p=0.21] or in the proportion of females [BD 52 (50.5%), MDD 56 (50.5%), χ2=0.61, df 1, p=0.44]. t Tests showed that the BD and MDD groups did not differ on N, E, A or C but differed significantly on openness (t=−2.12, df = 202, p=0.02, see Fig. 3). A two-factor ANOVA limited to individuals in depressed or euthymic mood states revealed an effect of diagnosis on openness (F=4.69, df=1, 169, p=0.03), and no significant effect of mood state (F=0.16, df=1, 169, p=0.68). In contrast, current mood state had significant effects on extraversion (F=21.2, df=1, 169, p<0.001), agreeableness (F=4.08, df=1, 169, p=0.045) and neuroticism (F=15.1, df=1, 169, p<0.001), while diagnosis did not. Conscientiousness was not significantly associated with either mood state or diagnosis.
Fig. 3.
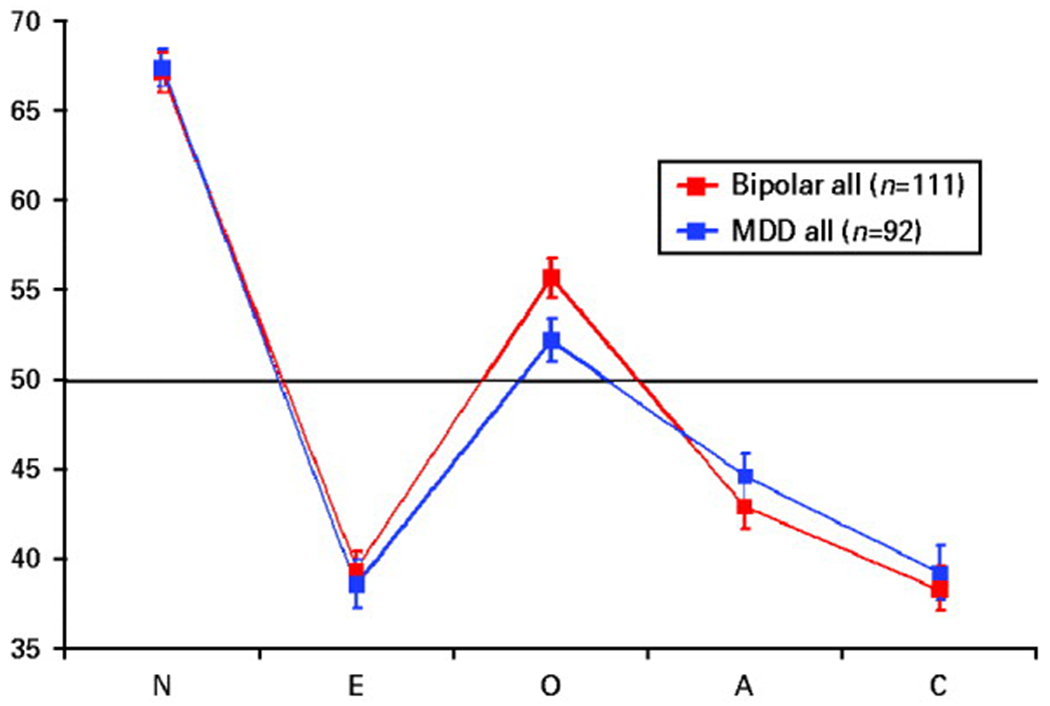
NEO Five-Factor Inventory (NEO-FFI) personality scores (t scores) in an independent sample of 203 individuals with mood disorders: bipolar disorder ( , all n=111); major depressive disorder (–■–, all n=92). Values are means, with standard errors represented by vertical bars. —, Population mean=50 (s.d.=10) (Costa & McCrae, 1992). N, Neuroticism; E, extraversion; O, openness to experience; A, agreeableness; C, conscientiousness. Groups differ only in O (t=−2.12, df=202, p=0.02).
, all n=111); major depressive disorder (–■–, all n=92). Values are means, with standard errors represented by vertical bars. —, Population mean=50 (s.d.=10) (Costa & McCrae, 1992). N, Neuroticism; E, extraversion; O, openness to experience; A, agreeableness; C, conscientiousness. Groups differ only in O (t=−2.12, df=202, p=0.02).
Associations between personality and illness course
The longitudinal nature of STEP-BD allowed us to examine whether euthymic personality predicted the prospective course of illness. A euthymic personality assessment was available for 453 STEP-GRP individuals whose illness course could be categorized. Of these, 56 (12%) were defined as manic-prone, 260 (57%) as depression-prone, and 137 (30%) patients showed no predominant mood (136 were euthymic throughout the study; one participant reported an equal number of days manic and depressed). The three groups differed significantly from each other in the proportion of days spent manic [manic-prone, mean 11 (s.d.=0.09) days; depression-prone, mean 0.01 (s.d.=0.03) days; no predominant mood, mean 0.00 (s.d.=0.00) days; F=162, df=2, 50, p<0.001], and the proportion of days spent depressed [manic-prone, mean 0.03 (s.d.=0.04) days; depression-prone, mean 0.14 (s.d.=0.12) days; no predominant mood, mean 0.00 (s.d.=0.00) days; F=116, df=2, 450, p<0.001].
Sex-adjusted personality t scores were compared between depression-prone, manic-prone, and equal polarity groups, using one-way ANOVA (Fig. 4). Openness, conscientiousness and agreeableness did not differ between groups. Neuroticism and extraversion differed significantly (neuroticism, F=14.3, df=2, 450, p<0.001; extraversion, F=10.3, df=2, 450, p<0.001). Post-hoc t tests showed that higher extraversion scores were associated with a manic-prone course compared with a depression-prone course, and neuroticism scores were higher and extraversion scores lower in depression-prone individuals than those with no predominant mood.
Fig. 4.
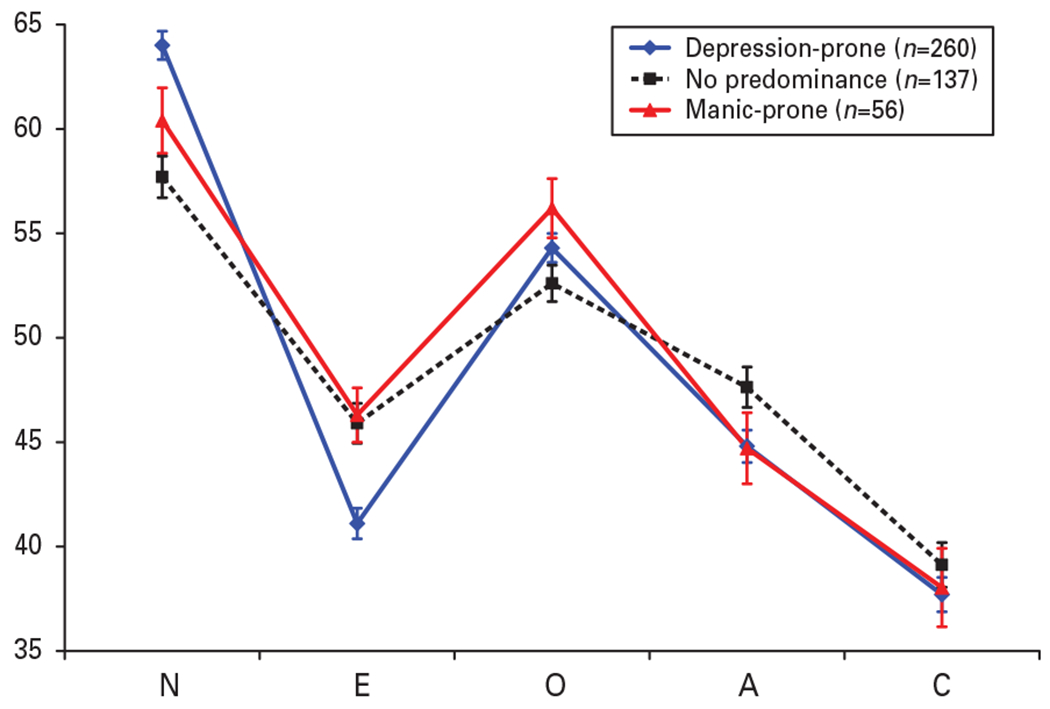
NEO Five-Factor Inventory (NEO-FFI) personality scores (t scores) during euthymic state among 453 individuals with depression-prone (–◆–, n=260), manic-prone ( , n=56) or no predominant mood (--■--, n=137) bipolar disorder (Systematic Treatment Enhancement Program genetic repository participants). Scores are unadjusted for residual symptoms. Values are means, with standard errors represented by vertical bars. N, Neuroticism ; E, extraversion ; O, openness to experience ; A, agreeableness ; C, conscientiousness. Significant differences exist between groups in N (F1=4.3, df=2, 450, p<0.0001) and E (F1=0.3, df=2, 450, p=0.0001).
, n=56) or no predominant mood (--■--, n=137) bipolar disorder (Systematic Treatment Enhancement Program genetic repository participants). Scores are unadjusted for residual symptoms. Values are means, with standard errors represented by vertical bars. N, Neuroticism ; E, extraversion ; O, openness to experience ; A, agreeableness ; C, conscientiousness. Significant differences exist between groups in N (F1=4.3, df=2, 450, p<0.0001) and E (F1=0.3, df=2, 450, p=0.0001).
Because residual symptoms during euthymic states might confound associations between euthymic personality and illness course, we used multinomial logistic regression to control for residual manic and depressed symptoms. Compared with individuals with no predominant mood, elevated neuroticism and decreased extraversion predicted a depression-prone course, and increased openness a manic-prone course (see Appendix Table 1).
We attempted to replicate the associations between personality and illness course in STEP-SCP. A euthymic personality assessment and illness course categorization was available for 436 individuals. Of these, 48 (11%) were defined as manic-prone, 206 (47%) as depression-prone, and 182 (42%) patients were euthymic throughout their participation (n=181) or reported an equal number of days manic and depressed (n=1). As in STEP-GRP, elevated neuroticism and decreased extraversion predicted a depression-prone course. In addition, lower conscientiousness scores were associated with a depression-prone course. No personality factor significantly predicted a manic-prone course (Appendix Table 1).
Discussion
To our knowledge, this is the largest analysis of the relationship between personality and BD. The longitudinal nature of STEP-BD with repeated personality assessments allowed us to examine three key questions: (1) is there a distinct personality profile associated with BD; (2) are associations between personality and BD due to state mood effects; and (3) are there associations between personality and illness course?
BD was associated with a distinct personality profile comprising high neuroticism and openness, and low extraversion, conscientiousness and agreeableness. This profile was replicated in two independent samples, suggesting that this profile may reflect a liability for affective disorder. Furthermore, we saw no difference in scores on any trait between patients with bipolar I, bipolar II and bipolar NOS diagnoses.
Although we did not compare personality across a full range of psychiatric disorders, comparisons within the MGH sample demonstrated that patients with BD had higher NEO openness scores than patients with MDD. These findings suggest that openness is an enduring marker differentiating individuals at risk for mania or hypomania from those at risk for other affective disorders. Some (Bagby et al. 1996; Nowakowska et al. 2005) but not all (Bagby et al. 1997; Jain et al. 1999) previous studies have reported elevated openness in BD.
Longitudinal assessment of mood and personality allowed us to quantify state effects of mood on personality. We found associations between depression and increased neuroticism and decreased extraversion, conscientiousness and openness, whereas mania was associated only with increased extraversion. These effects were largely consistent across time. The existence of such ‘ state ’ effects could be interpreted as reflecting the inherent limitations of the self-report method, or alternatively as reflecting genuine, though temporary, mood-driven fluctuations in personality (Reich et al. 1987; Santor et al. 1997). It is interesting that decreases in neuroticism were paralleled by decreases in openness, suggesting that decreases in worry, negative affect, or pessimism do not bring about increases in openness or novelty seeking.
These state effects do not fully account for personality differences between bipolar patients and controls (Clark et al. 2003). Personality measures show high test–retest reliabilities in psychiatric populations, similar to those seen in healthy controls (Kleifield et al. 1994; Kentros et al. 1997). Whereas personality differences are ameliorated by successful treatment of symptoms, personality scores during treatment trials show both absolute change and high test–retest correlations within individuals, such that changes in symptoms and personality correlate only modestly (Santor et al. 1997). Moreover, these differences in bipolar and other affective disorders exist prior to illness onset (Rodgers, 1990; Lauer et al. 1997) and the effects of prodromal (Fava & Kellner, 1991) or residual symptoms (Katz & McGuffin, 1987; Sauer et al. 1997) cannot account for them. In keeping with other studies of patients in remission (Hirschfeld & Klerman, 1979; Cox et al. 2004b), our samples differed widely from normative data on every trait during euthymia, particularly in neuroticism and conscientiousness, where mean difference was greater than one standard deviation. All three BD samples, as well as the depressed group, showed below-average extraversion scores, in contrast to previous studies which suggested elevated scores on extraversion-related traits in BD (Akiskal et al. 1983; Young et al. 1995). Results presented here suggest that while extraversion is elevated during mania it remains below average in BD patients during euthymic periods, perhaps due to ongoing experiences of depression or irritability.
Further evidence that the personality differences associated with BD are enduring traits was provided by differences in euthymic personality among patients who subsequently experienced manic-prone and depression-prone courses of illnesses. Some of these group differences may be attributable to residual symptoms present during apparently euthymic states. We controlled for these residual symptoms by covarying for depression and mania while analysing associations between personality and subsequent mood states. These covariance analyses do not reduce the significant associations between personality and patients’ predominant mood states.
Our results fit with a body of research suggesting that neuroticism is a non-specific predictor of mental disorder (Middeldorp et al. 2005). Since neuroticism is stable over the life course (Wray et al. 2007) while symptoms change markedly within individuals (Colman et al. 2007), neuroticism may be a better predictor of the lifetime vulnerability to depression than any single symptom measurement. Neuroticism captures aspects of personality that go beyond depression, such as worrying, which may be enduring characteristics that are separate from the experience of low mood (Duggan et al. 2003). Moreover, our analyses follow much previous research in suggesting that N and E are the personality traits most associated with risk for psychopathology, and that openness may be the trait most related to mania. Conscientiousness and agreeableness, though also affected in BD, may ultimately be less relevant to ‘external’ clinical validators of illness course.
The study was limited by methodological assumptions including the accuracy of self-reported personality. The NEO-FFI may not capture all personality variation relevant to BD. However an informant-based measure would have been difficult to administer and perhaps also unnecessary: even during depressed states, patients’ self-reports of personality do not differ widely from those of informants (Bagby et al. 1998). Second, we defined our illness-course groups by predominant mood episode, prospectively through clinical observations. While the accuracy of this allocation has limitations, there are advantages of the prospective design including reduced problems with recall accuracy. Third, for pragmatic reasons and to minimize missing data we included personality assessments that were conducted within 30 days of clinical assessments, although the usual delay was much shorter than this 30-day maximum. Nonetheless, this delay between assessments might introduce random error in the association between personality and symptoms among patients with rapid changes in mood state. For example, patients with high openness scores during euthymia could have switched to hypomania during the lag interval between the symptom and personality assessments. Fourth, we cannot rule out effects of treatment, selection for a specialty treatment program or co-morbid anxiety or personality disorders, which may conceivably affect personality profile. Fifth, many patients were missing from the later personality assessments. The EM model estimator used for the mplus analyses are robust against the influence of any missingness related to the five personality traits; nonetheless, we cannot exclude the possibility that other unmeasured factors may have influenced missingness and thus increased the error in the model. Despite these limitations, the consistency of results across three BD samples suggests that our results can be generalized. Finally, a significant limitation of the study is the reliance on normative data rather than a demographically matched healthy comparison group with which to directly compare scores. It is possible that a proportion of the difference in scores between our BD group and those polled for the normative data reflect cohort effects or regional differences.
Knowing that there are associations between BD and personality traits does not define their direction of causality. Attempts to experimentally manipulate mood and measure the corresponding effect on personality have largely failed to invoke personality changes (Masters & Furman, 1976) but these studies suffer limitations of sample size and magnitude of mood effects. This study cannot differentiate between the possibility that BD and personality traits have shared genetic causes and the ‘scarring ’ hypothesis, i.e. that prior illness episodes change personality. Testing this would require repeated assessment of personality and psychopathology in longitudinal designs, establishing baseline personality before onset of illness and following personality change in individuals who do and do not develop bipolar spectrum disorders (Rodgers, 1990; Van Os & Jones, 2001). These studies have not been conducted in BD, in comparison with a substantial high-risk literature assessing personality and psychopathology in MDD (Mulder, 2002). An alternative approach would be to use genetic methods to examine the genetic correlation between personality profiles and BD. For example, twin studies have documented shared genetic determinants of personality traits (especially neuroticism and extraversion) with anxiety disorders and MDD (Hettema et al. 2006; Kendler et al. 2006; Bienvenu et al. 2007; Kendler & Myers, 2010). The availability of genomewide association analysis (GWAS) also provides an opportunity to examine the shared genetic risk factors underlying personality and psychiatric disorder. For example, aggregate results from a GWAS analysis of schizophrenia were recently shown to account for a significant proportion of the polygenic contribution to BD (Purcell et al. 2009). Similar cross-phenotype analyses between BD and personality profiles could be used to estimate the proportion of phenotypic overlap that is attributable to genetic predisposition (as opposed to scarring). To date, no such twin or molecular genetic analyses of BD and personality have been reported; our results suggest that such studies could be valuable for dissecting the etiology of the association between BD and personality reported here.
In sum, we demonstrated that patients with BD can be distinguished from population norms and from patients with MDD on select personality variables, notably openness and neuroticism. State effects of mood on personality are considerable but do not fully explain personality profiles in BD. Moreover, personality during euthymia is predictive of future mood course, suggesting that personality disturbances are enduring markers of the illness process. Future research should examine whether these profiles are a direct consequence of the underlying neurobiological (genetic, or environmental) causes of BD.
Supplementary Material
Appendix Table 1. Associations between NEO-FFI personality scores [mean (s.e.) t scores] during euthymic state and depression-prone and manic-prone courses of bipolar disorder
Multinomial categorical regression coefficients (B) and standard errors (s.e.) reflect predictive effect of personality score on illness course, compared with individuals showing no predominant mood.
Acknowledgements
We are grateful to the following individuals: T. Croudace and G. Hammond for Mplus advice, and K. Todd-Brown for assistance in data handling. The STEP-BD project was funded in whole or in part with federal funds from the National Institute of Mental Health (NIMH), National Institutes of Health (NIH), under contract N01-MH-80001 to G.S. (principal investigator), M. E. Thase (co-principal investigator) and M. S. Bauer (co-principal investigator). Active STEP-BD sites and principal investigators included: Baylor College of Medicine (L. B. Marangell); Case University (J. R. Calabrese); Massachusetts General Hospital and Harvard Medical School (A.A.N.); Portland Veterans Affairs Medical Center (P. Hauser); Stanford University School of Medicine (T. A. Ketter); University of Colorado Health Sciences Center (M. Thomas); University of Massachusetts Medical Center (J. Patel); University of Oklahoma College of Medicine (M. D. Fossey); University of Pennsylvania Medical Center (L. Gyulai); University of Pittsburgh Western Psychiatric Institute and Clinic (M. E. Thase); University of Texas Health Science Center at San Antonio (C. L. Bowden). Collection of DNA from consenting participants in STEP-BD was supported by N01-MH-80001 (G.S., principal investigator). We thank B. Rosen-Sheidley and L. Silfies for their assistance with this effort.
Declaration of Interest
This work was also supported by NIH grants MH079799 and MH063445 (J.W.S.) and MH63420 (V.L.N.). Collection of data from the MGH sample was supported by a grant from Millennium Pharmaceuticals to J.W.S. and J.F.R. ; J.H.B. was supported by the University of Cambridge Parke-Davis Exchange Fellowship.
References
- Akiskal HS, Hirschfeld RM, Yerevanian BI (1983). The relationship of personality to affective disorders. Archives of General Psychiatry 40, 801–810. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Kilzieh N, Maser JD, Clayton PJ, Schettler PJ, Traci Shea M, Endicott J, Scheftner W, Hirschfeld RM, Keller MB (2006). The distinct temperament profiles of bipolar I, bipolar II and unipolar patients. Journal of Affective Disorders 92, 19–33. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Bindseil KD, Schuller DR, Rector NA, Young LT, Cooke RG, Seeman MV, McCay EA, Joffe RT (1997). Relationship between the five-factor model of personality and unipolar, bipolar and schizophrenic patients. Psychiatry Research 70, 83–94. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Rector NA, Bindseil K, Dickens SE, Levitan RD, Kennedy SH (1998). Self-report ratings and informants’ ratings of personalities of depressed outpatients. American Journal of Psychiatry 155, 437–438. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Young LT, Schuller DR, Bindseil KD, Cooke RG, Dickens SE, Levitt AJ, Joffe RT (1996). Bipolar disorder, unipolar depression and the Five-Factor Model of personality. Journal of Affective Disorders 41, 25–32. [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Hettema JM, Neale MC, Prescott CA, Kendler KS (2007). Low extraversion and high neuroticism as indices of genetic and environmental risk for social phobia, agoraphobia, and animal phobia. American Journal of Psychiatry 164, 1714–1721. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, Jarrett RB (2003). Separate personality traits from states to predict depression. Journal of Personality Disorders 17, 152–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Ploubidis GB, Wadsworth ME, Jones PB, Croudace TJ (2007). A longitudinal typology of symptoms of depression and anxiety over the life course. Biological Psychiatry 62, 1265–1271. [DOI] [PubMed] [Google Scholar]
- Costa PTJ, McCrae RR (1992). Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Psychological Assessment Resources Inc.: Odessa, FL. [Google Scholar]
- Cox BJ, MacPherson PS, Enns MW, McWilliams LA (2004a). Neuroticism and self-criticism associated with posttraumatic stress disorder in a nationally representative sample. Behavioral Research and Therapy 42, 105–114. [DOI] [PubMed] [Google Scholar]
- Cox BJ, McWilliams LA, Enns MW, Clara IP (2004b). Broad and specific personality dimensions associated with major depression in a nationally representative sample. Comprehensive Psychiatry 45, 246–253. [DOI] [PubMed] [Google Scholar]
- Duggan C, Milton J, Egan V, McCarthy L, Palmer B, Lee A (2003). Theories of general personality and mental disorder. British Journal of Psychiatry 181 (Suppl. 44), S19–S23. [DOI] [PubMed] [Google Scholar]
- Enns MW, Cox BJ (1997). Personality dimensions and depression : review and commentary. Canadian Journal of Psychiatry 42, 274–284. [DOI] [PubMed] [Google Scholar]
- Eysenck HJ, Rachman S (1965). Dimensions of personality, pp. 14–28. In The Causes and Cures of Neurosis. Robert R. Knapp: San Diego, CA. [Google Scholar]
- Fava GA, Kellner R (1991). Prodromal symptoms in affective disorders. American Journal of Psychiatry 148, 823–830. [DOI] [PubMed] [Google Scholar]
- Ferguson CJ (2010). A meta-analysis of normal and disordered personality across the life span. Journal of Personality and Social Psychologil 98, 659–667. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer RI, Gibbon M, Williams JBW (1996). Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. American Psychiatric Press Inc.: Washington, DC. [Google Scholar]
- Foster JA, MacQueen G (2008). Neurobiological factors linking personality traits and major depression. Canadian Journal of Psychiatry 53, 6–13. [DOI] [PubMed] [Google Scholar]
- Furukawa T, Hori S, Yoshida S, Tsuji M, Nakanishi M, Hamanaka T (1998). Premorbid personality traits of patients with organic (ICD-10 F0), schizophrenic (F2), mood (F3), and neurotic (F4) disorders according to the five-factor model of personality. Psychiatry Research 78, 179–187. [DOI] [PubMed] [Google Scholar]
- Goldberg LR (1993). The structure of phenotypic personality traits. American Psychologist 48, 26–34. [DOI] [PubMed] [Google Scholar]
- Heerlein A, Richter P, Gonzalez M, Santander J (1998). Personality patterns and outcome in depressive and bipolar disorders. Psychopathology 31, 15–22. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS (2006). A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry 163, 857–864. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Klerman GL (1979). Personality attributes and affective disorders. American Journal of Psychiatry 136, 67–70. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM (1999). Cutoff criteria for fit indices in covariance structure analysis: conventional versus new alternatives. Structural Equation Modeling 6, 1–55. [Google Scholar]
- Jain U, Blais MA, Otto MW, Hirshfeld DR, Sachs GS (1999). Five-factor personality traits in patients with seasonal depression : treatment effects and comparisons with bipolar patients. Journal of Affective Disorders 55, 51–54. [DOI] [PubMed] [Google Scholar]
- Katz R, McGuffin P (1987). Neuroticism in familial depression. Psychological Medicine 17, 155–161. [DOI] [PubMed] [Google Scholar]
- Kendell RE, DiScipio WJ (1968). Eysenck personality inventory scores of patients with depressive illnesses. British Journal of Psychiatry 114, 767–770. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL (2006). Personality and major depression : a Swedish longitudinal, population-based twin study. Archives of General Psychiatry 63, 1113–1120. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J (2010). The genetic and environmental relationship between major depression and the five-factor model of personality. Psychological Medicine 40, 801–806. [DOI] [PubMed] [Google Scholar]
- Kentros M, Smith TE, Hull J, McKee M, Terkelsen K, Capalbo C (1997). Stability of personality traits in schizophrenia and schizoaffective disorder : a pilot project. Journal of Nervous and Mental Disease 185, 549–555. [DOI] [PubMed] [Google Scholar]
- Kleifield EI, Sunday S, Hurt S, Halmi KA (1994). The effects of depression and treatment on the Tridimensional Personality Questionnaire. Biological Psychiatry 36, 68–70. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Bronisch T, Kainz M, Schreiber W, Holsboer F, Krieg JC (1997). Pre-morbid psychometric profile of subjects at high familial risk for affective disorder. Psychological Medicine 17, 355–362. [DOI] [PubMed] [Google Scholar]
- Lozano BE, Johnson SL (2001). Can personality traits predict increases in manic and depressive symptoms? Journal of Affective Disorders 63, 103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier W, Lichtermann D, Minges J, Heun R (1992). Personality traits in subjects at risk for unipolar major depression : a family study perspective. Journal of Affective Disorders 24, 153–164. [DOI] [PubMed] [Google Scholar]
- Masters JC, Furman W (1976). Effects of affective states on noncontingent outcome expectancies and beliefs in internal or external control. Developmental Psychology 12, 481–482. [Google Scholar]
- McCrae RR, Costa PT Jr. (1997). Personality trait structure as a human universal. American Psychologist 52, 509–516. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Terracciano A (2005). Universal features of personality traits from the observer’s perspective: data from 50 cultures. Journal of Personality and Social Psychology 88, 547–561. [DOI] [PubMed] [Google Scholar]
- Meredith W, Tisak J (1990). Latent curve analysis. Psychometrika 55, 107–122. [Google Scholar]
- Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI (2005). The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychological Medicine 35, 611–624. [DOI] [PubMed] [Google Scholar]
- Modell S, Huber J, Holsboer F, Lauer CJ (2003). The Munich Vulnerability Study on Affective Disorders: risk factors for unipolarity versus bipolarity. Journal of Affective Disorders 74, 173–184. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry 134, 382–389. [DOI] [PubMed] [Google Scholar]
- Mulder RT (2002). Personality pathology and treatment outcome in major depression: a review. American Journal of Psychiatry 159, 359–371. [DOI] [PubMed] [Google Scholar]
- Nowakowska C, Strong CM, Santosa CM, Wang PW, Ketter TA (2005). Temperamental commonalities and differences in euthymic mood disorder patients, creative controls, and healthy controls. Journal of Affective Disorders 85, 207–215. [DOI] [PubMed] [Google Scholar]
- Purcell SM, Wray NR, Stone JL, Visscher PM, O’Donovan MC, Sullivan PF, Sklar P (2009). Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460, 748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector NA, Hood K, Richter MA, Bagby RM (2002). Obsessive-compulsive disorder and the five-factor model of personality : distinction and overlap with major depressive disorder. Behavioral Research and Therapy 40, 1205–1219. [DOI] [PubMed] [Google Scholar]
- Reich J, Noyes R Jr., Hirschfeld R, Coryell W, O’Gorman T (1987). State and personality in depressed and panic patients. American Journal of Psychiatry 144, 181–187. [DOI] [PubMed] [Google Scholar]
- Rietschel M, Beckmann L, Strohmaier J, Georgi A, Karpushova A, Schirmbeck F, Boesshenz KV, Schmal C, Burger C, Jamra RA, Schumacher J, Hotels S, Kumsta R, Entringer S, Krug A, Markov V, Maier W, Propping P, Wust S, Kircher T, Nothen MM, Cichon S, Schulze TG (2008). G72 and its association with major depression and neuroticism in large population-based groups from Germany. American Journal of Psychiatry 165, 753–762. [DOI] [PubMed] [Google Scholar]
- Rodgers B (1990). Behaviour and personality in childhood as predictors of adult psychiatric disorder. Journal of Child Psychology and Psychiatry 31, 393–414. [DOI] [PubMed] [Google Scholar]
- Rosa AR, Andreazza AC, Kunz M, Gomes F, Santin A, Sanchez-Moreno J, Reinares M, Colom F, Vieta E, Kapczinski F (2008). Predominant polarity in bipolar disorder : diagnostic implications. Journal of Affective Disorders 107, 45–51. [DOI] [PubMed] [Google Scholar]
- Rubin DB (1987). Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons, Inc.: NY. [Google Scholar]
- Sachs GS (1990). Use of clonazepam for bipolar affective disorder. Journal of Clinical Psychiatry 51 (Suppl.), 31–34; discussion 50–53. [PubMed] [Google Scholar]
- Sachs GS, Guille C, McMurrich SL (2002). A clinical monitoring form for mood disorders. Bipolar Disorders 4, 323–327. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, Lavori P, Lebowitz B, Rudorfer M, Frank E, Nierenberg AA, Fava M, Bowden C, Ketter T, Marangell L, Calabrese J, Kupfer D, Rosenbaum JF (2003). Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biological Psychiatry 53, 1028–1042. [DOI] [PubMed] [Google Scholar]
- Santor DA, Bagby RM, Joffe RT (1997). Evaluating stability and change in personality and depression. Journal of Personality and Social Psychology 73, 1354–1362. [DOI] [PubMed] [Google Scholar]
- Sauer H, Richter P, Czernik A, Ludwig-Mayerhofer W, Schochlin C, Greil W, von Zerssen D (1997). Personality differences between patients with major depression and bipolar disorder – the impact of minor symptoms on self-ratings of personality. Journal of Affective Disorders 42, 169–177. [DOI] [PubMed] [Google Scholar]
- Shea MT, Leon AC, Mueller TI, Solomon DA, Warshaw MG, Keller MB (1996). Does major depression result in lasting personality change? American Journal of Psychiatry 153, 1404–1410. [DOI] [PubMed] [Google Scholar]
- Simon NM, Smoller JW, Fava M, Sachs G, Racette SR, Perlis R, Sonawalla S, Rosenbaum JF (2003). Comparing anxiety disorders and anxiety-related traits in bipolar disorder and unipolar depression. Journal of Psychiatric Research 37, 187–192. [DOI] [PubMed] [Google Scholar]
- Solyom L, Ledwidge B, Solyom C (1986). Delineating social phobia. British Journal of Psychiatry 149, 464–470. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Quilty LC, Sellbom M, Rector NA, Bagby RM (2008). Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: the context of personality structure. Journal of Abnormal Psychology 117, 812–825. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ (1994). Relationship between the five-factor model of personality and axis I disorders in a nonclinical sample. Journal of Abnormal Psychology 103, 350–360. [DOI] [PubMed] [Google Scholar]
- Van Os J, Jones PB (2001). Neuroticism as a risk factor for schizophrenia. Psychological Medicine 31, 1129–1134. [DOI] [PubMed] [Google Scholar]
- Wray NR, Birley AJ, Sullivan PF, Visscher PM, Martin NG (2007). Genetic and phenotypic stability of measures of neuroticism over 22 years. Twin Research and Human Genetics 10, 695–702. [DOI] [PubMed] [Google Scholar]
- Young LT, Bagby RM, Cooke RG, Parker JD, Levitt AJ, Joffe RT (1995). A comparison of Tridimensional Personality Questionnaire dimensions in bipolar disorder and unipolar depression. Psychiatry Research 58, 139–143. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA (1978). A rating scale for mania: reliability, validity and sensitivity. British Journal of Psychiatry 133, 429–435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table 1. Associations between NEO-FFI personality scores [mean (s.e.) t scores] during euthymic state and depression-prone and manic-prone courses of bipolar disorder
Multinomial categorical regression coefficients (B) and standard errors (s.e.) reflect predictive effect of personality score on illness course, compared with individuals showing no predominant mood.


