ABSTRACT
The World Health Organization defines healthy ageing as ‘the process of developing and maintaining the functional ability that enables well-being in older age’. This functional ability is the characteristic of the individual’s own physical and mental status influenced by the environmental and socio-economic factors. Preoperative preparation of the elderly patients includes functional assessment to identify preexisting cognitive impairment or cardio-pulmonary reserve, frailty, nutrition, polypharmacy and anti-coagulation issues. Intraoperative management includes anaesthetic mode and pharmacology, monitoring, intravenous fluid and transfusion management, lung protective ventilation and hypothermia. Postoperative checklist includes perioperative analgesia, postoperative delirium and cognitive dysfunction.
Key words: Aged, frailty, geriatric assessment, perioperative care
INTRODUCTION
Advances in modern healthcare have improved the life expectancy of the population and quality of life of the elderly. With more number of aged people getting admitted for various surgeries, anaesthetising these patients has become a challenge and has laid the foundation to a new subspeciality. Geriatric patients represent a vulnerable group at higher perioperative risk.[1] Hence, a standard perioperative approach needs to be adopted in the geriatric patient with the help of a multidisciplinary team. The primary goal should be not just survival but to provide an optimal quality of life after the surgical procedure. The various physiological changes seen in the elderly and the complications associated with these during anaesthesia and the recent advances for a comprehensive and safe practice in geriatric anaesthesia are discussed in this article.
PHYSIOLOGICAL CHANGES IN THE ELDERLY AND THEIR ANAESTHETIC IMPLICATIONS[2–4]
Central nervous system
Ageing is associated with a progressive decrease in brain mass with increased ventricular size. The cerebral blood flow, cerebral metabolic rate and electrical activity remain unchanged. The neurotransmitter functions suffer due to decreased number of receptors (acetylcholine, dopamine, noradrenaline, 5-hydroxytryptamine). Hence, there is a decrease in minimum alveolar concentration (approximately 6% by every decade) with increased sensitivity to general anaesthetic drugs. Due to decreased Schwann cells, there is an increase in the exposed nerve root distance which increases block sensitivity. There is decrease in the epidural space due to narrowing of the spinal canal. Dural permeability also increases leading to exaggerated effects during epidural blockade.
Cardiovascular system
Anaesthetic agents in elderly individuals remove the baseline sympathetic tone. They directly depress the myocardial and vascular smooth muscle contraction and diminish the baroreceptor reflex leading to unpredictable responses. The changes in the vascular compliance, myocyte death and receptor responsiveness decrease the reserve and adaptability to alterations during major surgical procedures. Vascular ageing occurs with loss of elasticity of vessels and stiffened arteries. Subsequently, pressure in the aortic root increases during late systole resulting in ventricular hypertrophy and impaired diastolic filling. The venous compliance decreases and the stiff veins are unable to ‘buffer’ changes in blood volume leading to exaggerated changes in cardiac filling pressure during volume shifts and increased susceptibility to hypovolaemia.
In the heart, progressive myocyte death is seen with increasing age. There is reduced number of sinoatrial nodal cells with fibrotic infiltration of conduction system. Ventricular hypertrophy may also be secondary to cardiac muscle cell death. Ventricular contraction may be impaired due to incomplete relaxation during diastole secondary to myocardial fibrosis. Diastolic dysfunction is the most common cause of heart failure with preserved ejection fraction in those more than 75 years of age. Diastolic filling depends on high left atrial pressure and atrial kick. Hence, tachycardia and atrial fibrillation are not well tolerated. There is a narrow range between inadequate filling pressure and fluid overload (preload sensitive). Other changes such as decreased beta-receptor responsiveness are also observed.
Respiratory system
The elderly have altered respiratory mechanics and less efficient gas exchange. The intrapleural pressure increases because of increased lung compliance, stiff thorax, decreased height and calcification of vertebrae and diaphragmatic flattening. There is a decrease in central nervous system (CNS) responsiveness that causes blunted response to hypoxia and hypercapnia. While the vital capacity reduces, there is an increase in residual volume (reduced elastic recoil 5–10% per decade), functional residual capacity (FRC), dead space and closing capacity (CC). CC surpasses the FRC leading to ventilation/perfusion (V/Q) mismatch and shunting. Limited maximal expiratory flow rate response is seen during exercise. Additionally, there is a reduction in the forced expiratory volume in one second (FEV1) (6-10%per decade) and FEV1/FRC. Blunting of hypoxic pulmonary vasoconstrictive reflex occurs with a decrease in pulmonary capillary bed and increase in pulmonary artery pressure (30%) and pulmonary vascular resistance (80%).
Decreased efficiency of gas exchange occurs due to breakdown of elastin connections between connective tissue and alveolar tissue. Poor tethering of lung tissue to airways permits atelectasis and increases risk of hypoxia and pneumonia. The smaller airways collapse under anaesthesia, increasing shunting and dead space. Preoxygenation before anaesthesia takes longer time due to decrease in partial pressure of arterial oxygen (PaO2) by approximately 0.4 mmHg/year. [PaO2 = 100 -(0.4 x age in years) mmHg].
Airway management in the elderly patient is complicated due to diminished receptor sensitivity. Stimulus threshold for vocal cord closure is increased with blunted cough, laryngeal and pharyngeal reflexes. A weak gag reflex with loss of oesophageal-gastric sphincter tone predisposes the elderly to an increased risk of aspiration.
Changes in other systems
In the kidneys, glomerulosclerosis occurs leading to decreased glomerular filtration after 40 years of age, i.e., 10% decrease per decade. The drug clearance is decreased owing to reduced renal blood flow. Serum creatinine is a poor indicator of underlying renal function due to decreased muscle mass. Reduced sodium conservation owing to reduced renin aldosterone activity with raised anti-diuretic hormone leads to hyponatraemia and hyperkalaemia. Certain endocrine abnormalities such as hypocalcaemia, osteoporosis, subclinical hypothyroidism with raised thyroid stimulating hormone can be seen.
Significant changes are seen in the haematological, musculoskeletal, gastrointestinal system and the skin. Anaemia occurs due to immunosenescence, reduced bone marrow production and spleen size, stem cells ageing and erythropoietin resistance. Decreased muscle mass and bone density, osteoarthritis, osteomalacia, rheumatoid arthritis, gout, degenerative joint disease and loss of disc along with fragile skin, decreased skin elasticity and decreased subcutaneous fat predispose the elderly to injuries during surgical positioning. They are also prone for pressure ulcer due to dehydration, poor circulation and nutrition. Care during positioning and padding and securing a proper venous access are crucial. Progressive deficit in ability to sense heat and cold and reduced ability to generate heat (reduced muscle mass for shivering thermogenesis) and dissipate heat make them prone for hypothermia. This is further complicated by impaired non-shivering thermogenesis due to decreased brown fat.
Increased gastric acid secretion is seen in the elderly. Decreased colonic motility leads to faecal impaction and constipation. Hepatic tissue loss is approximately 40% by 80 years of age and leads to delayed drug metabolism.
PHARMACOLOGICAL CHANGES AND ANAESTHETIC IMPLICATIONS[2,3]
There is reduced receptor number, increased receptor sensitivity and postreceptor transduction in the brain. Hence, geriatric patients have increased sensitivity to anaesthetic drugs. Hepatic metabolism and renal drug clearance is also affected. There is rapid equilibration with the peripheral compartment due to decreased total body water, and hence less dose of drug is required. In the central compartment, there is decreased lean body mass and albumin, causing raised peak concentration and slower redistribution. Increased body fat accounts for slow equilibration leading to prolonged drug actions [Table 1].
Table 1.
Pharmacokinetic and pharmacodynamic properties of drugs in geriatric patients
| Drug | Pharmacokinetic | Pharmacodynamic |
|---|---|---|
| Thiopentone (85%reduction), Etomidate | Decreased initial volume of distribution (Vd). decreased clearance (half-life 13-25 h versus 6-12 h in young) | |
| Propofol, midazolam | Decreased clearance | Increased brain sensitivity |
| Morphine (morphine-6 glucuronide) | Decreased clearance | Reduced renal clearance Increased brain sensitivity |
| Fentanyl, sufentanil, alfentanil | Increased brain sensitivity | |
| Remifentanil | Reduced central compartment volume | Increased brain sensitivity |
| Neuromuscular blockers | Prolonged action of drug undergoing hepatic metabolism Dose unchanged | |
| Neostigmine | Dose unchanged | More cardiac adverse effects |
Dose reduction is universally observed over all the range of drugs. Thiopental causes profound drop in blood pressure due to peripheral vasodilatation with blunted baroreceptor reflex. Elimination is delayed (half-life is 13–25 hours compared to 6–12 hours in the young). Hence, 25–75% dose reduction should be done in geriatrics. Propofol causes greater blood pressure fall than thiopental; hence, titrated doses are recommended. However, there is less postanaesthetic mental impairment. A 30–40% reduction in bolus and infusion dose is advised (induction dose 1.2–1.7 mg/kg). Etomidate is desirable as it is haemodynamically stable; however, 50% dose reduction is needed. V/Q mismatch leads to reduced rate of action of inhalational agents. However, a reduced cardiac output leads to rapid onset of action. Increased volume of distribution leads to prolonged recovery with highly lipid soluble agents (isoflurane 7 minutes). Lower lipid solubility as with sevoflurane, desflurane is preferred as there is rapid depth control and faster emergence (desflurane 5.4 minutes). Minimum alveolar concentration of all inhalational agents is reduced by 6% per decade after 40 years of age.
Senile motor neuron degeneration with muscle atrophy predisposes these patients to motor weakness and exaggerated effects of muscle relaxants. Senile cyclic guanosine 3’,5’- monophosphate deficiency and atypical extra-junctional acetylcholine receptor proliferation is seen leading to risk of prolonged and/or residual neuromuscular blockade resulting in adverse postoperative respiratory events (hypoxia, airway obstruction). Increased sensitivity to succinylcholine can be due to reduced cholinesterase levels. Sugammadex can be used to avoid delayed recovery.
COMMON PERIOPERATIVE COMPLICATIONS IN GERIATRIC POPULATION
Elderly patients require cautious care and support perioperatively. The multiple comorbid conditions, decreased functional status, decreased respiratory reserve, frailty, neurocognitive decline, limitations in mobility and polypharmacy place them at greater risk.[1]
Cardiopulmonary complications
The diminished cardiopulmonary reserve leads to exaggerated decline in blood pressure during induction. Beta-blocked receptors, baroreceptor dysfunction and decreased response to angiotensin II fail to counteract hypovolaemia. A retrospective study of 8441 individuals undergoing general surgery published in 2018 showed that age ≥65 years is an important predictor of major adverse cardiac events like atrial fibrillation and myocardial infarction.[5]
Postoperative pulmonary complications (PPCs) increase with increasing age. In patients undergoing non-cardiac surgery, the rates of PPC are 14% in those aged ≥65 years.[6] Postoperative hypoxaemia may occur in 20–60% of these patients. Apnoea with interrupted breathing, after administration of narcotics, and postoperative pulmonary aspiration due to decreased cough and swallowing reflexes, along with pulmonary infections and atelectasis, are commonly observed. Elderly patients have higher incidence of postoperative sleep apnoea.
Central nervous system complications
In individuals ≥65 years, the prevalence of dementia is 5–8%.[4] Data from a retrospective cohort published in 2014 showed that geriatric population with hip fractures and preexisting dementia were associated with increased hazard ratio (2.49), risk of higher mortality and poor prognosis.[7] Preexisting cognitive impairment is a predictor of postoperative delirium (POD).[1] Postoperative cognitive impairment leads to decreased pulmonary hygiene and ambulation further leading to morbidity in the form of pneumonia, deep vein thrombosis and stroke. The impairments are perceived in mood, memory, behaviour and motor function.
Postoperative delirium and postoperative cognitive dysfunction
Postoperative cognitive impairment affects 5–50% of geriatric patients comprising of POD and postoperative cognitive dysfunction (POCD). Delirium is acute progressive alteration in cognitive function lasting for few days to few weeks. Prevalence of POD is 10%. In POCD, there is deterioration from baseline in cognitive neuropsychological functioning lasting for months or years. Incidence of POCD is 79% at 7 days and 12.7% at 3 months in non-cardiac surgery.[1] Aetiological factors include drug interactions, alcohol abuse, electrolyte abnormalities, longer duration of anaesthesia, postoperative infections, second operations and respiratory problems. No difference between regional and general anaesthesia is noticed in the incidence of POCD. Certain randomised controlled trials have compared propofol and sevoflurane and found that sevoflurane increased the incidence of POCD at 7 days and 9 months.[8] POCD carries an increased risk of death at 1 year after surgery.[9]
The pathogenesis involves neuroinflammation, micro-emboli and neuronal death. This leads to cholinergic dysfunction. Recent evidence says that the use of bispectral index (BIS) monitoring to adjust anaesthetic doses to achieve a BIS value between 40 and 60 or using auditory evoked potential monitoring reduces cognitive dysfunction at 3 months postoperatively.[10] A meta-analysis of four studies showed no correlation between depth of anaesthesia and POCD.[11] Dexmedetomidine is recognised to have neuroprotective effects and reduces POCD by preventing inflammation, providing good analgesia and CNS protection. In a meta-analysis by Yang W et al.,[12] which included use of dexmedetomidine within general anaesthesia, POCD at day 7 was lower in the treatment group. There are few studies which provide evidence for the protective effect of ketamine and the non-steroidal anti-inflammatory drug parecoxib against POCD; however, the quality of evidence is low and is limited by few number of randomised controlled trials.[13]
Bone cement implantation syndrome
Femoral neck fractures comprise 50% of geriatric hip fractures. In a study done by Tsai et al.,[14] it was noted that the cemented group had higher mortality than the uncemented group. Male gender, older age and higher score on comorbidity index (≥1) were independent determinants of increased mortality. Bone cement implantation syndrome occurs due to release of cement monomers into the circulation during cementing. It occurs 4–6 minutes after cementing leading to hypotension and desaturation. Some recent studies have investigated the role of emboli formed, complement activation and histamine release. Bone cement can directly inhibit the myocardium leading to arrhythmias. Due to the decreased cardiopulmonary reserve in the elderly, there is risk of greater morbidity and mortality.
Other complications
Elderly patients are vulnerable to hypothermia due to decreased basal metabolic rate and anaesthesia-induced altered thermoregulatory mechanisms. Hypothermia can lead to coagulopathy, increased blood loss, cardiac ischaemia, arrhythmias, poor wound healing and long hospital stay. As elderly have degenerative diseases, giving an epidural and spinal is technically difficult. They are susceptible to fractures and dislocations while positioning. Polypharmacy leads to high rate of adverse drug reactions due to multiple interactions and decreased renal and hepatic reserve. Frailty and poor nutrition are associated with increased length of hospital stay and assisted living postoperatively for a long time.
GUIDELINES TO IMPROVE PATIENT SAFETY IN GERIATRIC AGE GROUP
With recent evidence published on preoperative screening of elderly patients for frailty and post operative cognitive disorders, the perioperative management in the elderly has witnessed a paradigm shift by the introduction of safer alternatives and algorithmic approach to already existing practices for improved safety in the entire perioperative period.[15,16] The newer concepts and modalities in the field of geriatric age group are emerging.
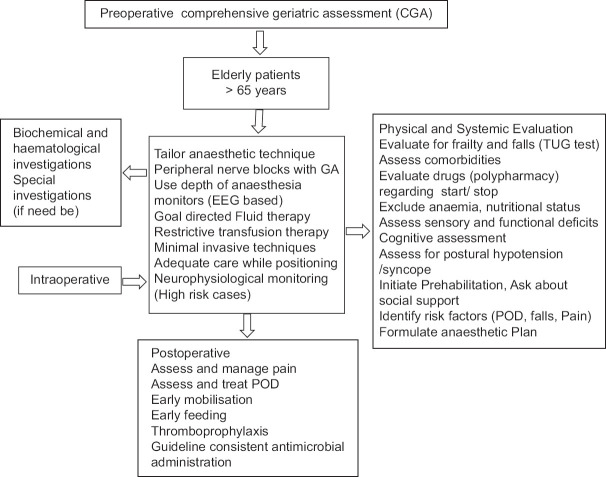
Comprehensive geriatric assessment
The primary focus is to delineate and mitigate the multiple negative factors in the preoperative period and tailor an anaesthetic approach for better patient-oriented outcome measures. The perioperative management of elderly patients (PriME) recommendations has proposed a multidisciplinary comprehensive geriatric assessment (CGA) model encompassing the physical, functional, psychological and social concerns, to frame decisions for favourable clinical outcomes and functionality in the elderly [Figure 1].[17] The home-based and in-hospital models for CGA have been incorporated and demonstrated to yield better results than the posthospital discharge programmes, in hospital-based as well as outpatient CGA consultation.[18] Elderly patients exhibiting timed up and go test result duration >20 seconds must undergo a CGA evaluation. The former is a screening test to evaluate propensity to fall and is a reliable and strong mortality indicator.[19]
Figure 1.
Comprehensive geriatric assessment. GA – general anaesthesia, EEG – electroencephalogram, TUG – timed up and go. POD – postoperative day
Frailty assessment
Since frailty is a strong predictor of adverse postoperative outcomes, the American College of Surgeons National Surgical Quality Improvement Program/American Geriatrics Society (ACS NSQIP/AGS) advocates critical assessment by using multiparametric frailty scales.[20,21] It is also recommended to initiate multimodal prehabilitation and assessment of functional and sensory deficits in the immediate preoperative period.[22,23]
Airway management
Difficulty in mask ventilation and risk of aspiration will require second generation laryngeal mask airway over conventional mask ventilation. Preoxygenation is mandatory. Limited range of neck movements may necessitate the use of a flexible fibreoptic bronchoscope.
Role of neuraxial/regional/peripheral blockade
Despite the conflict of preference between general and neuraxial anaesthesia, the guidelines recommend the use of the latter over the former in the elderly, wherever possible.[24] Peripheral nerve blocks (PNBs) exhibit opioid-sparing effect, provide adequate analgesia, risk reduction in postoperative complications especially pneumonia, improved mobility and reduced costs. Use of PNB should be considered in patients with underlying comorbidities, which also obviates the need for stringent monitoring and thus leads to better resource utilisation in this subset of patients.[25] Therefore, regional anaesthesia should be employed in the intraoperative and in the postoperative period as a part of multimodal analgesic techniques and use of ultrasound is advocated for higher success and safety.
Opioid-free anaesthesia and enhanced recovery after surgery
Opioid-free anaesthesia has shown a beneficial impact on postoperative delirium in the recent clinical trial.[26] The enhanced recovery after surgery (ERAS) protocols have also been extended to the elderly. These focus on preoperative carbohydrate loading, goal-directed fluid therapy and patient blood management system with restrictive transfusion strategy (haemoglobin <8 gm/dl).
Neurophysiological monitoring
Since sensory deficits have been reported to be the most common cause of disability in the age group of >60 years, use of intraoperative neurophysiological monitoring with somatosensory evoked potentials, transcranial electrical stimulation and free-run electromyography (EMGs)/triggered EMG has been advocated.[27] It is recommended to monitor the depth of anaesthesia guided by the use of electroencephalogram based monitoring systems (BIS or entropy) to avoid deeper levels of sedation and also monitor cerebral desaturation by regional cerebral oximetry in the high-risk elderly population.
Assessment of pain in the elderly
Numerical rating scale or verbal descriptors are used as aids for pain assessment in the cognitively intact elderly patient. Pain in Advanced Dementia (PAINAD) and Doloplus-2 scales may be employed in patients with underlying cognitive impairment. An innovative electronic pain assessment tool, integrating automated facial expression analysis with clinical behavioural indicators, has recently been introduced and has indicated excellent inter-rater reliability in patients with dementia. The current recommendations underline the importance of structured pain education implementation amongst the healthcare providers for the geriatric age group.[28]
SUMMARY
Elderly patients represent a vulnerable patient group at higher perioperative risk. Treatment concepts should include extensive preoperative assessment, structured intraoperative procedures and postoperative in-patient treatment pathway with adequate pain relief. Optimal perioperative treatment requires close inter-disciplinary, inter-professional and cross-sectional collaboration to minimise unwanted postoperative outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lim BG, Lee IO. Anesthetic management of geriatric patients. Korean J Anaesthesiol. 2020;73:8–29. doi: 10.4097/kja.19391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brocklehurst JC, Fillit HM, Rockwood K, Woodhouse KW. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 7th ed. Ch. 13-23. Philadelphia, PA: Saunders/Elsevier; 2016. pp. 82–144. [Google Scholar]
- 3.Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega RA, et al. 8th ed. Ch. 34. Philadelphia, PA: Wolters Kluwer; 2021. Anesthesia for older Patients. Clinical Anesthesia; pp. 932–52. [Google Scholar]
- 4.Butterworth JF IV, Mackey DC, Wasnick JD, editors. Morgan and Mikhail's Clinical Anesthesiology. 7th ed. Ch. 43. United Sates: McGraw Hill; 2022. pp. 1488–510. Ch 43. [Google Scholar]
- 5.Acheampong D, Guerrier S, Lavarias V, Pechman D, Mills C, Inabnet W, et al. Risk factors contributing to cardiac events following general and vascular surgery. Ann Med Surg. 2018;33:16–23. doi: 10.1016/j.amsu.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manku K, Bacchetti P, Leung JM. Prognostic significance of postoperative in-hospital complications in elderly patients. I. Long-term Survival. Anaesth Analg. 2003;96:583–9. doi: 10.1097/00000539-200302000-00051. [DOI] [PubMed] [Google Scholar]
- 7.Seitz DP, Gill SS, Gruneir A, Austin PC, Anderson GM, Bell CM, et al. Effects of dementia on postoperative outcomes of older adults with hip fractures:A population-based study. J Am Med Dir Assoc. 2014;15:334–41. doi: 10.1016/j.jamda.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 8.Qiao Y, Feng H, Zhao T, Yan H, Zhang H, Zhao X. Postoperative cognitive dysfunction after inhalational anesthesia in elderly patients undergoing major surgery:The influence of anesthetic technique, cerebral injury and systemic inflammation. BMC Anesthesiol. 2015;15:154. doi: 10.1186/s12871-015-0130-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS the ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110:548–55. doi: 10.1097/ALN.0b013e318195b569. [DOI] [PubMed] [Google Scholar]
- 10.Punjasawadwong Y, Chau-In W, Laopaiboon M, Punjasawadwong S, Pin-On P. Processed electroencephalogram and evoked potential techniques for amelioration of postoperative delirium and cognitive dysfunction following non-cardiac and non-neurosurgical procedures in adults. Cochrane Database Syst Rev. 2018;5:CD011283. doi: 10.1002/14651858.CD011283.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu X, Jin X, Yang S, Xia Y. The correlation of the depth of anesthesia and postoperative cognitive impairment:A meta-analysis based on randomized controlled trials. J Clin Anesth. 2018;45:55–9. doi: 10.1016/j.jclinane.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Yang W, Kong LS, Zhu XX, Wang RX, Liu Y, Chen LR. Effect of dexmedetomidine on postoperative cognitive dysfunction and inflammation in patients after general anaesthesia:A PRISMA-compliant systematic review and meta-analysis. Medicine. 2019;98:e15383. doi: 10.1097/MD.0000000000015383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brodier EA, Cibelli M. Postoperative cognitive dysfunction in clinical practice. BJA Educ. 2021;21:75–82. doi: 10.1016/j.bjae.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai M, Ng YY, Chen W, Tsai S, Wu S. The effects of cement fixation on survival in elderly patients with hip hemiarthroplasty:A nationwide cohort study. BMC Musculoskeletal Disord. 2019;20:628. doi: 10.1186/s12891-019-3013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olotu C, Weimann A, Bahrs C, Schwenk W, Scherer M, Kiefmann R. The perioperative care of older patients—time for a new, interdisciplinary approach. Dtsch Arztebl Int. 2019;116:63–9. doi: 10.3238/arztebl.2019.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgeli R, Scholtz K, Kurth J, Treskatsch S, Neuner B, Koch S, et al. Perioperative management of elderly patients with gastrointestinal malignancies:The contribution of Anesthesia. Visc Med. 2017;33:267–74. doi: 10.1159/000475611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aceto P, Antonelli Incalzi R, Bettelli G, Carron M, Chiumiento F, Corcione A, et al. Perioperative Management of Elderly patients (PriME):Recommendations from an Italian intersociety consensus. Aging Clin Exp Res. 2020;32:1647–73. doi: 10.1007/s40520-020-01624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan S, Ip KY, Irwin MG. Peri-operative optimisation of elderly and frail patients:A narrative review. Anaesthesia. 2019;74(S1):80–9. doi: 10.1111/anae.14512. [DOI] [PubMed] [Google Scholar]
- 19.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 20.Cuvillon P, Lefrant JY, Gricourt Y. Considerations for the use of local anesthesia in the frail elderly:Current perspectives. Local Reg Anesth. 2022;15:71–5. doi: 10.2147/LRA.S325877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal perioperative management of the geriatric patient:A Best practices guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg. 2016;222:930–47. doi: 10.1016/j.jamcollsurg.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 22.Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M, et al. Guidelines for enhanced recovery after lung surgery:Recommendations of the Enhanced Recovery After Surgery (ERAS ®) Society and the European Society of Thoracic Surgeons (ESTS) Eur J Cardiothorac Surg. 2019;55:91–115. doi: 10.1093/ejcts/ezy301. [DOI] [PubMed] [Google Scholar]
- 23.Levett DZH, Jack S, Swart M, Carlisle J, Wilson J, Snowden C, et al. Perioperative cardiopulmonary exercise testing (CPET):Consensus clinical guidelineson indications, organization, conduct, and physiological interpretation. Br J Anaesth. 2018;120:484–50. doi: 10.1016/j.bja.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 24.Memtsoudis SG, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin EM, et al. Anaesthetic care of patients undergoing primary hip and knee arthroplasty:Consensus recommendations from the International Consensus on Anaesthesia-Related Outcomes after Surgery group (ICAROS) based on a systematic review and meta-analysis. Br J Anaesth. 2019;123:269–87. doi: 10.1016/j.bja.2019.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures:A Cochrane review. Anesth Analg. 2018;126:1695–704. doi: 10.1213/ANE.0000000000002489. [DOI] [PubMed] [Google Scholar]
- 26.Luchting, Benjamin Azad, Shahnaz Christina. Pain therapy for the elderly patient:Is opioid-free an option? Curr Opin Anesthesiol. 2019;32:86–91. doi: 10.1097/ACO.0000000000000675. [DOI] [PubMed] [Google Scholar]
- 27.Palanca BJA, Avidan MS, Wildes TS, Ju Y-E, Ching S. Electroencephalography and delirium in the postoperative period. Br J Anaesth. 2017;119:294–307. doi: 10.1093/bja/aew475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schofield P. The assessment of pain in older people:UK National Guidelines. Age Ageing. 2018;47:i1–22. doi: 10.1093/ageing/afx192. [DOI] [PMC free article] [PubMed] [Google Scholar]