ABSTRACT
Airway management is a core skill essential for anaesthesiologists and health care providers involved in resuscitation and acute care of patients. Advancements in airway management are continuously evolving. This narrative review highlights the recent advancements with respect to innovations, tools, techniques, guidelines, and research in both technical and non-technical aspects of airway management. These include nasal endoscopy, virtual endoscopy, airway ultrasound, video endoscopes, supraglottic airways with enhanced protection against aspiration, hybrid devices, and the use of artificial intelligence and telemedicine, the utility of which has increased in recent times, thereby improving success with airway management and enhancing patient safety. There has been an increasing emphasis on peri-intubation oxygenation strategies to reduce complications in patients with a physiologically difficult airway. Recent guidelines for difficult airway management and preventing unrecognised oesophageal intubation are available. Large multicentre airway data collection helps us examine airway incidents, aetiology, and complications to expand our knowledge and give us insights for change in practice.
Key words: Intubation, technology, ventilation
INTRODUCTION
Airway management is a core skill essential for anaesthesiologists and health care providers involved in resuscitation and acute care of patients. Not surprisingly, it is the subject of much research and innovation to facilitate efficiency in the procedure and enhance patient safety. There has been an exponential rise in publications on management of difficult airways, especially in the last few years, in anaesthesia literature.[1] The coronavirus disease 2019 (COVID-19) pandemic has led to a paradigm shift in airway management, with the recognition of unique challenges and the use of additional measures to avoid transmission of infection to health care workers while ensuring patient safety.[2] There has been a recent focus on the management of physiologically difficult airways, in addition to anatomical difficulty.[3] This narrative review highlights the recent advancements with respect to innovations, tools, techniques, guidelines, and research in both technical and non-technical aspects of airway management. Lower airway management and ventilation strategies have not been covered.
METHODS
A literature search was conducted on PubMed and Cochrane Database of Systematic Reviews using the following keywords: airway, airway management, intubation, supraglottic devices, recent advances, technology, oxygenation, airway guidelines. The search included guidelines, review articles, clinical trials, observational studies, and meta-analyses published from 2017 to 2022. Based on articles selected initially, a manual search was conducted using cross-references to identify articles not captured in the initial search, including those of historic value.
AIRWAY ASSESSMENT
Assessment for anatomical difficulty
A combination of careful history-taking, general examination, and focused airway examination using specific tests and imaging is commonly used to predict a difficult airway. The history of a previous difficult airway is most important to consider. The use of nasal endoscopy, virtual endoscopy, ultrasound, and artificial intelligence (AI) has emerged in recent times for difficult airway assessment and management.
Tests for airway assessment
The most commonly used tests are the Mallampati test, mouth opening test, thyromental distance, sternomental distance, upper lip bite test (ULBT), and the Wilson risk score. Screening tests should have high sensitivities. A Cochrane review comparing the diagnostic accuracy of various commonly used tests for predicting a difficult airway found all investigated tests to have relatively low sensitivities with high variability. Among the tests examined, the ULBT showed the most favourable diagnostic accuracy.[4] The ULBT, a short hyomental distance, retrognathia, or a combination of findings based on the Wilson score were found to be the best predictors of a difficult tracheal intubation in a recent systematic review. No risk factor or physical finding was found that consistently ruled out a difficult intubation.[5] Taken together, one can conclude that although a variety of tests are helpful in identifying a potentially difficult airway, they should be interpreted with caution as they have not proved to be good screening tests. Among the screening tests, the ULBT seems to be the best predictor of difficulty.
Nasal endoscopy
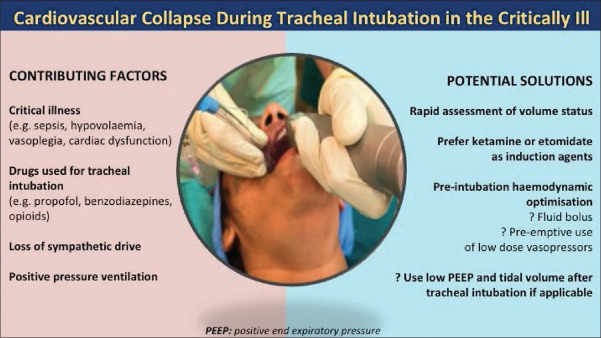
Nasendoscopy is used to assess the upper airway and trachea and is useful for planning both tracheal intubation and extubation.[6] Assessment of airway narrowing, distortion, presence of infectious pathology, laryngeal tumours, or upper airway oedema can be easily performed in awake patients prior to airway management, usually in the sitting position. An example is the nasal endoscopic view of carcinoma of the glottis with subglottic extension [Figure 1]. Nasal endoscopy also facilitates examination of devices in place including supraglottic airways, tracheal tubes, and tracheostomy tubes, thus making it useful for extubation or device manipulation.
Figure 1.
Nasal endoscopic view of carcinoma of the glottis with subglottic extension
Virtual endoscopy
This is a radiological simulation of the airway anatomy from the oropharynx up to the carina. A 3D ‘fly-through’ video is created using computed tomography (CT) images reconstructed to create the airway anatomy. This improves our interpretation of 2D CT scan images and helps us to better identify a difficult airway to make an appropriate airway plan.[7] Virtual endoscopy improves the diagnostic accuracy of airway pathology when compared with CT scan alone and leads to more conservative and potentially safer airway management strategies in patients with head and neck pathology.[8]
Role of ultrasound
The use of point-of-care ultrasound (POCUS) imaging is rising in airway management. POCUS facilitates quick and real-time assessment of the airway, which can be learned with minimal training.[9]
A tongue thickness greater than 6.1 cm has been shown to be an independent predictor of difficult tracheal intubation.[10] The distance from skin to epiglottis (DSE) is the most measured and studied test to predict a difficult laryngoscopy. A DSE >2–2.5 cm is a predictor of difficult laryngoscopy.[11] A recent systematic review showed that airway ultrasound metrics were associated with difficult laryngoscopy in three domains: anterior tissue thickness, anatomical position, and oral space.[12]
Other ultrasonographic assessments include dynamic assessment of the vocal cords, which is useful in the assessment of stridor and vocal cord palsy. Assessment of the subglottic diameter has been shown to be superior to the formula used in estimating tracheal tube size in children. Gastric POCUS can be used to reliably estimate the volume of gastric contents. Ultrasound has a high diagnostic capability in confirming tube position. In an oesophageal intubation, there is a ‘double tract sign’ with two air-filled structures. This evaluation can be further supported by thoracic ultrasonography to check the absence of bilateral lung sliding.[9]
Preoperative surface marking of the cricothyroid membrane prior to an anticipated difficult intubation or as a real-time procedural guidance is the most commonly recommended application of airway ultrasound and has a higher success rate than palpation.[13] While performing tracheostomy, ultrasound is a useful tool to assess the diameter of the trachea and any overlying vessels at the proposed insertion site.
Though ultrasound examination is performed quickly, the results are dependent on the operator. Further training and studies are needed for better standardisation. Combining clinical and ultrasound assessments may form an accurate screening tool for difficult laryngoscopy in the future.[12]
Artificial intelligence to predict a difficult airway
An AI model was created based on deep learning, using 16 facial images of patients classified according to expected difficulty in tracheal intubation. The AI model was able to recognise expected difficulty in tracheal intubation with 80.5% accuracy and an area under the curve of 0.864 (confidence interval 95%, 0.731–0.969).[14] Other studies have used machine learning to perform a facial analysis to detect morphological features related to difficult airways.[15]
THE PHYSIOLOGICALLY DIFFICULT AIRWAY
A physiologically difficult airway is one in which physiological alterations in the patient increase the risk of cardiorespiratory and other complications during tracheal intubation.[3,16] These physiological derangements may be due to acute illness, pre-existing disease, the effects of anaesthetic agents, and positive pressure ventilation. This risk is especially recognised in critically ill patients but can also occur in healthy patients who have physiological alterations such as pregnant, obese, and paediatric patients.
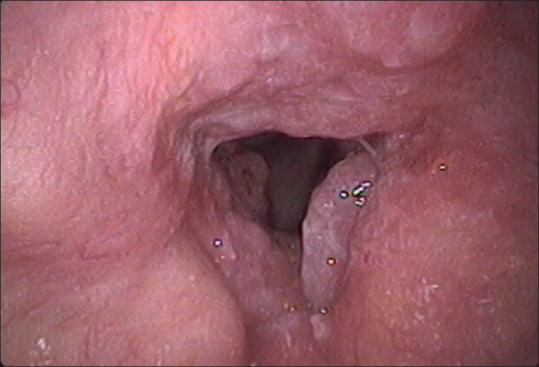
In the International Observational Study to Understand the Impact and Best Practices of Airway Management in Critically Ill Patients (INTUBE), which included 2964 critically ill patients undergoing tracheal intubation, at least one major adverse peri-intubation event was observed in 45.2% of patients. The predominant complication was cardiovascular instability (42.6% of patients), followed by severe hypoxaemia (9.3%) and cardiac arrest (3.1%).[17] A subanalysis of the study identified propofol use for induction as a modifiable intervention significantly associated with cardiovascular instability.[18] Common practices such as administration of a fluid bolus prior to tracheal intubation to prevent hypotension have not shown benefit. The role of pre-emptive use of low-dose vasopressors is currently under investigation.[19] Common contributing factors for cardiovascular collapse along with potential solutions are being currently investigated [Figure 2].
Figure 2.
Cardiovascular collapse during tracheal intubation in the critically ill: contributing factors and potential solutions. (The author Dr Sheila Myatra has taken prior permission for reproduction of this figure created by her from Elsevier and the Editor in Chief of ACCPM)
The focus of airway evaluation and management has traditionally been on anatomical factors that make airway management difficult. Recognition of the high incidence of complications in this vulnerable group of patients has emphasised the need for physiological optimisation and adoption of strategies to avoid complications during tracheal intubation.
PREOXYGENATION AND APNOEIC OXYGENATION
Preoxygenation is used to increase oxygen reserves prior to anaesthetic induction and tracheal intubation to prevent the onset of critical hypoxaemia during periods of apnoea. There has been a recent focus on optimising preoxygenation using non-invasive ventilation (NIV) or high-flow nasal oxygen (HFNO), continuing nasal oxygen during attempts at tracheal intubation, considering gentle mask ventilation during rapid sequence intubation (RSI), and the use of NIV/HFNO post extubation, especially in high-risk patients.[20] These include patients for RSI, with limited oxygen reserves (critically ill, paediatric, pregnant, and obese patients) and when a difficult airway is anticipated.
The pressure support and positive end-expiratory pressure applied during NIV keep the lungs open during the entire respiratory cycle, decrease intrapulmonary shunting and thereby increase safe apnoea time (time to desaturation following neuromuscular blockade). Apnoeic oxygenation can further extend the duration of safe apnoea. By increasing the flow rate to 15 L/min through a nasal cannula (NO DESAT: nasal oxygen during efforts at securing a tube), near 100% inspired oxygen concentration (FiO2) can be obtained due to the decreased oxygen demands of the apnoeic state. However, this method will not have a significant effect on carbon dioxide (CO2) levels.[21] Transnasal humidified rapid insufflation ventilatory exchange (THRIVE), which provides 100% oxygen at flow rates up to 70 L/min, is a method of apnoeic oxygenation and ventilation that can prolong the safe apnoea time longer than NO DESAT, without much rise in CO2 levels and thereby reduce the time pressure during airway management.[22] This is especially useful during the management of difficult airways, rapid sequence inductions, and management of morbidly obese patients. THRIVE can be used for pre-oxygenation and continued during tracheal intubation. HFNO has also been recommended to optimise oxygenation during shared airway procedures, awake tracheal intubation, and in spontaneously breathing patients receiving intravenous anaesthesia.[23,24]
In the landmark Preventing Hypoxaemia with Manual Ventilation during Endotracheal Intubation (PREVENT) trial, critically ill patients were randomised to receive bag-mask ventilation from induction to laryngoscopy or no ventilation during RSI. Bag-mask ventilation reduced the incidence of severe hypoxaemia by more than half without any increase in the incidence of pulmonary aspiration.[25] Therefore, the risk/benefit of gentle mask ventilation during RSI must be carefully assessed in patients at high risk of desaturation. Post-extubation support with NIV and HFNO in patients at high risk of reintubation has shown reduced reintubation rates.[26]
NEWER TOOLS AND TECHNIQUES FOR AIRWAY MANAGEMENT
Supraglottic airway devices (SADs)
SADs with enhanced protection against aspiration
To further protect against gastric aspiration, the self-sealing Baska maskÔ was introduced. During positive pressure ventilation, the cuff seal apposes to the glottis incrementally to augment the seal pressure with increasing airway pressure. Along with this, it has been equipped with a gastric reflux high-flow suction clearance system.[27] Another inclusion is the LMA protectorÔ. Distinct from other SADs, it contains two gastric drainage channels and a pharyngeal chamber to drain the gastric contents. Additionally, it is equipped with a colour-coded cuff pressure indicator for continuous intracuff pressure monitoring.[28]
SADs enabling tracheal intubation using a flexible bronchoscope
Tracheal intubation using a flexible bronchoscope through SADs can be achieved through a majority of newer SADs, which allow an adequate diameter tracheal tube to be inserted through the device. The most recent addition is the LMA BlockbusterÔ. Along with the dual safety and superior seal, it comes with a customised Parker tipped, wire reinforced tube.[29] While managing a difficult airway, the importance of tracheal intubation through SADs using a flexible bronchoscope has been emphasised by recent airway guidelines.
Adjuncts for tracheal intubation
MADgic atomisers
The newer range of atomising devices includes MADgic LMAÔ and LMA MAD NasalÔ that not only topicalise the oral, nasal, pharyngeal, and laryngeal tissues but also help keep the airway open.
Optical viewing stylets
Newer variants of optical stylets use complementary metal oxide semiconductor video chips at the distal opening of the stylet with an inbuilt screen monitor or an attachment for smartphones for viewing the airway structures during intubation. These include Trachway intubating styletÔ, Stylet ViuÔ, AinCa Video StyletÔ, C-MAC Video Stylet,Ô and the VivaSight SLÔ.[30]
Robotic endoscope-automated laryngeal imaging for tracheal intubation
This is a video-endoscopic stylet used to guide tracheal intubation. The bending motion of the tip of the endoscope can be controlled manually or automatically towards the glottis. The prototype, operating in automated mode, uses a recorded glottic image that resembles anatomic airway images in the electronic databases to steer the endoscope tip into the trachea to facilitate tracheal intubation.[31]
Videolaryngoscopes
The improvement and decrease in cost of miniature video camera chips and light-emitting diode sources have triggered an explosion of videolaryngoscopes. The Vie Scope™ has a closed circular tube with a bevelled end, similar to the Miller-shaped laryngoscope blade, that is transparent and illuminated. It allows direct visualisation of the glottis and aids endotracheal intubation using a bougie.[32] The infrared red intubation system (IRRIS) consists of a small infrared light source placed on the anterior cervical surface and over the cricothyroid membrane. The device emits infrared red light through the skin of the patient to the subglottic space. Then, a videolaryngoscope that does not filter that wavelength is placed in the airway. The videoscope displays a bright light emerging from the glottis which guides the passage.[33]
Video endoscopes
The COVID-19 pandemic has fuelled the shift from reusable to single-use bronchoscopes enabled with a battery light source and an in-built monitor. New variants have been added to the already established scopes.
Hybrid devices
These include devices with features of two or more traditional airway equipment. The total track VLMÔ combines the features of a videolaryngoscope and intubating laryngeal mask airway. An interesting option of picture-in-picture imaging to combine videolaryngoscope and video-bronchoscope capability into a single unit is currently available in GlideScope CoreÔ and CMACÔ.
Transnasal humidified rapid insufflation ventilatory exchange
This has been discussed in the beginning of this article.
Vision-guided supraglottic airway device insertions
There has been a recent focus on real-time, vision-guided insertion of SADs to ensure optimal placement. The Video Laryngeal Mask™ and SafeLM™ video laryngeal mask are available for use. The main advantages of these devices are that they can be easily inserted under direct vision, reduce airway damage, facilitate tracheal intubation through the SAD, have recording capability, and have the ability to detach the SAD from the scope once placed, thereby facilitating reuse of the videoscope.[34]
Video-assisted intubation with a flexible bronchoscope
The use of a flexible bronchoscope has traditionally been considered as the gold standard device for anticipated difficult airway with limited use in unanticipated difficult airway algorithms. The combined video-assisted flexible bronchoscopic intubation offers a scope for extending its use in both elective and rescue scenarios.
Telemedicine technology for tracheal intubation
Use of teleguidance in medicine in not new. It was explored during the COVID-19 pandemic as a means to reduce exposure to the airway provider. A scoping review that assessed teleguided technology for tracheal intubation found that it facilitated intubation as effectively as supervision by an individual without further complications. It also facilitates progressive autonomy for airway trainees.[35] However, clinical studies are necessary to fully understand the benefits and limitations of this technology.
CONFIRMATION OF TRACHEAL INTUBATION
Quick and correct placement of a tracheal tube is indispensable during airway management to avoid complications. There are several ways through which tracheal tube placement can be confirmed, but each has its own limitations. Clinical examination has been the traditional form of teaching. However, auscultation and observation of chest wall movement are unreliable.[36]
The 2022 American Society of Anesthesiologists (ASA) guidelines for difficult airway management recommend confirmation of tracheal intubation using waveform capnography.[36–39] Undetected oesophageal intubation continues to occur, leading to increased morbidity and mortality. None of these guidelines focus specifically on preventing unrecognised oesophageal intubation. Therefore, a consensus guideline from the Project for Universal Management of Airways (PUMA)—a global multidisciplinary group of airway experts and major international airway societies—was developed for providing comprehensive recommendations for preventing unrecognised oesophageal intubation.[40]
The PUMA guidelines recommend the routine use of a videolaryngoscope, if feasible, and encourages verbalisation of the view obtained by the airway operator during laryngoscopy. The guidelines recommend confirmation of tracheal intubation placement using sustained end-tidal carbon dioxide as the gold standard while meeting the following criteria: (1) rise in amplitude during exhalation and fall during inspiration; (2) increasing or consistent amplitude over at least seven breaths; (3) peak amplitude more than 1 kPa (7.5 mmHg) above baseline; and (4) clinically appropriate reading.[40] The guideline recommends default tube removal when sustained exhaled CO2 cannot be detected. If tube removal is considered dangerous, then urgent exclusion of oesophageal intubation using alternative techniques is recommended. These include repeat laryngoscopy (preferably videolaryngoscopy) and one of the following: flexible bronchoscopy, ultrasound or the use of oesophageal detector devices, along with evaluation of other causes of inability to detect CO2. The guideline recommends against using clinical examination to exclude oesophageal intubation. The tube should be removed if sustained exhaled CO2 cannot be achieved, oesophageal placement cannot be excluded, or the oxygen saturation drops at any point before restoring sustained exhaled CO2. The guidelines also emphasise the use of various strategies to address cognitive bias and deterioration in the performance of an individual or team under stressful situations.[40]
HUMAN FACTOR CONSIDERATIONS
Though clinical abilities and technical proficiencies are essential for successful airway management, non-technical skills are equally important.[41] Human factors involve considering the impact of aspects of the individual, environment, processes, and culture on human performance.[42] Poor human factors have contributed to 40% of reported cases, as per the 4th National Audit Project (NAP4) of the Royal College of Anaesthetists.[43]
The ASA guidelines outline human factors relevant to difficult airway management as practitioner factors (knowledge, training, complacency, stressors, team dynamics, team decision-making, debriefing, etc.) and external factors such as those related to the patient (including difficult airway, infection risk, aspiration risk), environment (including equipment, monitoring, personal protective equipment), and institution (including culture, staffing, protocols, supervision, support).[37] A study that looked at the prevalence and commonality of human factors in airway guidelines found that they were well represented, with work systems and processes featured more than user and patient outcome measurements.[42] Human factors are an evolving area in airway management. Further considerations are necessary for future guideline development.
The lesser incidence of airway complications limits our continued learning process. Therefore, regular practice of these skills by means of focussed airway workshops and simulation-based training programmes are important.[44] Cognitive aids such as the Vortex approach may be useful in these settings.[45] Equipment layout has been identified as a key element that may aid airway management, particularly in critical situations. Chrimes et al.[46] outlined key principles for incorporating human factors into airway trolley design and implementation to enhance team performance.
GUIDELINES FOR DIFFICULT AIRWAY MANAGEMENT
Three guidelines for difficult airway management have been published in recent times.[23,37,39] The 2022 ASA difficult airway guidelines emphasise awareness of the passage of time and limiting the number of attempts with different airway devices. The novel content includes a pre-airway management decision-making tool and an awake airway management algorithm.[37] Novel content in the Canadian guidelines include recommendations for the use of videolaryngoscope to facilitate all tracheal intubations and that all institutions designate an airway lead to help with airway-related protocols, training, and quality reviews.[39] The Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults are comprehensive and evidence-based that can help in the preparation and practical performance of ATI.[23] The PUMA group is working on the development of a single set of evidence-based airway management guidelines that can be applied universally.[47]
LARGE DATABASES AND MULTICENTRE OBSERVATIONAL STUDIES
The aim of large airway data collection is to examine airway incidents, aetiology, and complications in order to inform and expand our knowledge on the subject and give us insights into changes in practice. An example is the NAP4 from the United Kingdom which has provided important insights into airway management complications for practice change.[43] The INTUBE study highlights the high incidence of complications during tracheal intubation in the critically ill, with identification of haemodynamic collapse being the most frequent, along with insights into practice change and future research.[17] The Airway App demonstrates the feasibility of using smartphone technology to capture emergency front-of-neck airway experiences internationally.[48] Although information generated from such large databases have the potential of aiding safer future care, there are several practical hurdles for execution that need to be addressed. These include creating a robust registry, patient confidentiality, standardisation of the clinical data collected, access across health care systems, maintenance, and cost implications.
SUMMARY
Advancements in airway management are continuously evolving. They include a range of newer tools and strategies aimed at improving success in airway management and enhancing patient safety. Nasal endoscopy, virtual endoscopy, airway ultrasound, video endoscopy, supraglottic airways with enhanced protection against aspiration, hybrid devices, and the use of AI and telemedicine have increased utility in airway assessment and management. There has been increasing emphasis on peri-intubation oxygenation and non-technical skills and strategies to reduce complications in patients with a physiologically difficult airway. Large multicentre airway data analysis gives us insights into practice change. Recent guidelines for difficult airway management and preventing unrecognised oesophageal intubation are available. The penetration and impact of these guidelines on patient outcomes will need to be evaluated in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.García-Aroca MÁ, Pandiella-Dominique A, Navarro-Suay R, Alonso-Arroyo A, Granda-Orive JI, Anguita-Rodríguez F, et al. Analysis of production, impact, and scientific collaboration on difficult airway through the web of science and scopus (1981-2013) Anesth Analg. 2017;124:1886–96. doi: 10.1213/ANE.0000000000002058. [DOI] [PubMed] [Google Scholar]
- 2.Patwa A, Shah A, Garg R, Divatia JV, Kundra P, Doctor JR, et al. All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID-19 pandemic. Indian J Anaesth. 2020;64(Suppl 2):S107–15. doi: 10.4103/ija.IJA_498_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myatra SN, Divatia JV, Brewster DJ. The physiologically difficult airway:An emerging concept. Curr Opin Anaesthesiol. 2022;35:115–21. doi: 10.1097/ACO.0000000000001102. [DOI] [PubMed] [Google Scholar]
- 4.Roth D, Pace NL, Lee A, Hovhannisyan K, Warenits AM, Arrich J, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev. 2018;5:CD008874. doi: 10.1002/14651858.CD008874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Detsky ME, Jivraj N, Adhikari NK, Friedrich JO, Pinto R, Simel DL, et al. Will this patient be difficult to intubate?:The rational clinical examination systematic review. JAMA. 2019;321:493–503. doi: 10.1001/jama.2018.21413. [DOI] [PubMed] [Google Scholar]
- 6.Rosenblatt W, Ianus AI, Sukhupragarn W, Fickenscher A, Sasaki C. Preoperative endoscopic airway examination (PEAE) provides superior airway information and may reduce the use of unnecessary awake intubation. Anesth Analg. 2011;112:602–7. doi: 10.1213/ANE.0b013e3181fdfc1c. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad I, Keane O, Muldoon S. Enhancing airway assessment of patients with head and neck pathology using virtual endoscopy. Indian J Anaesth. 2017;61:782–6. doi: 10.4103/ija.IJA_588_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Boghdadly K, Onwochei DN, Millhoff B, Ahmad I. The effect of virtual endoscopy on diagnostic accuracy and airway management strategies in patients with head and neck pathology:A prospective cohort study. Can J Anaesth. 2017;64:1101–10. doi: 10.1007/s12630-017-0929-6. [DOI] [PubMed] [Google Scholar]
- 9.Adi O, Kok MS, Wahab SFA. Focused airway ultrasound:An armamentarium in future airway management. J Emerg Crit Care Med. 2019;3:31. [Google Scholar]
- 10.Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth. 2017;118:601–9. doi: 10.1093/bja/aex051. [DOI] [PubMed] [Google Scholar]
- 11.Carsetti A, Sorbello M, Adrario E, Donati A, Falcetta S. Airway ultrasound as predictor of difficult direct laryngoscopy:A systematic review and meta-analysis. Anesth Analg. 2022;134:740–50. doi: 10.1213/ANE.0000000000005839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhargava V, Rockwell NA, Tawfik D, Haileselassie B, Petrisor C, Su E. Prediction of difficult laryngoscopy using ultrasound:A systematic review and meta-analysis. Crit Care Med. 2023;51:117–26. doi: 10.1097/CCM.0000000000005711. [DOI] [PubMed] [Google Scholar]
- 13.Kristensen MS, Teoh WH, Rudolph SS. Ultrasonographic identification of the cricothyroid membrane:Best evidence, techniques, and clinical impact. Br J Anaesth. 2016;117:i39–48. doi: 10.1093/bja/aew176. [DOI] [PubMed] [Google Scholar]
- 14.Hayasaka T, Kawano K, Kurihara K, Suzuki H, Nakane M, Kawamae K. Creation of an artificial intelligence model for intubation difficulty classification by deep learning (convolutional neural network) using face images:An observational study. J Intensive Care. 2021;9:1–14. doi: 10.1186/s40560-021-00551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuendet GL, Schoettker P, Yüce A, Sorci M, Gao H, Perruchoud C, et al. Facial image analysis for fully automatic prediction of difficult endotracheal intubation. IEEE Trans Biomed Eng. 2016;63:328–39. doi: 10.1109/TBME.2015.2457032. [DOI] [PubMed] [Google Scholar]
- 16.Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sales JC. The physiologically difficult airway. West J Emerg Med. 2015;16:1109–17. doi: 10.5811/westjem.2015.8.27467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russotto V, Myatra SN, Laffey JG, Tassistro E, Antolini L, Bauer P. Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA. 2021;325:1164–72. doi: 10.1001/jama.2021.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russotto V, Tassistro E, Myatra SN, Parotto M, Antolini L, Bauer P, et al. Peri-intubation cardiovascular collapse in patients who are critically ill:Insights from the INTUBE study. Am J Respir Crit Care Med. 2022;206:449–58. doi: 10.1164/rccm.202111-2575OC. [DOI] [PubMed] [Google Scholar]
- 19.Myatra SN, Russotto V, Bellani G, Divatia JV. A fluid bolus before tracheal intubation in the critically ill does not prevent peri-intubation cardiovascular collapse:Time to consider alternatives? Anaesth Crit Care Pain Med. 2022;41:101158. doi: 10.1016/j.accpm.2022.101158. doi:10.1016/j.accpm.2022.101158. [DOI] [PubMed] [Google Scholar]
- 20.De Jong A, Casey JD, Myatra SN. Focus on noninvasive respiratory support before and after mechanical ventilation in patients with acute respiratory failure. Intensive Care Med. 2020;46:1460–3. doi: 10.1007/s00134-020-06100-8. [DOI] [PubMed] [Google Scholar]
- 21.Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–75. doi: 10.1016/j.annemergmed.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE):A physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015;70:323–9. doi: 10.1111/anae.12923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020;75:509–28. doi: 10.1111/anae.14904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Booth AWG, Vidhani K, Lee PK, Thomsett CM. SponTaneous Respiration using IntraVEnous anaesthesia and Hi-flownasal oxygen (STRIVE Hi) maintains oxygenation and airway patency during management of the obstructed airway:An observational study. Br J Anaesth. 2017;118:444–51. doi: 10.1093/bja/aew468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Casey JD, Janz DR, Russell DW, Vonderhaar DJ, Jofe AM, Dischert KM, et al. Bag-mask ventilation during tracheal intubation of critically Ill adults. N Engl J Med. 2019;380:811–21. doi: 10.1056/NEJMoa1812405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thille AW, Muller G, Gacouin A, Coudroy R, Decavele M, Sonneville R. Effect of postextubation highfow nasal oxygen with noninvasive ventilation versus high-fow nasal oxygen alone on reintubation among patients at high risk of extubation failure:A randomized clinical trial. JAMA. 2019;322:1465–75. doi: 10.1001/jama.2019.14901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Priya H, Sripriya R, Ravishankar M, Karthikeyan P, Charulatha R. Baska Mask is non-inferior to tracheal tube in preventing airway contamination during controlled ventilation in elective nasal surgeries:A randomised controlled trial. Indian J Anaesth. 2021;65:586–92. doi: 10.4103/ija.IJA_237_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan LZ, An Tan DJ, Seet E. Laryngeal mask airway Protector™for intubation and extubation in thyroid surgeries:A case report. Indian J Anaesth. 2018;62:545–8. doi: 10.4103/ija.IJA_43_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Endigeri A, Ganeshnavar A, Varaprasad B, Shivanand YH, Ayyangouda B. Comparison of success rate of BlockBuster® versus Fastrach® LMA as conduit for blind endotracheal intubation:A prospective randomised trial. Indian J Anaesth. 2019;63:988–94. doi: 10.4103/ija.IJA_396_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matek J, Kolek F, Klementova O, Michalek P, Vymazal T. Optical devices in tracheal intubation-state of the art in 2020. Diagnostics (Basel) 2021;11:575. doi: 10.3390/diagnostics11030575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biro P, Hofmann P, Gage D, Boehler Q, Chautems C, Braun J, et al. Automated tracheal intubation in an airway manikin using a robotic endoscope:A proof of concept study. Anaesthesia. 2020;75:881–6. doi: 10.1111/anae.14945. [DOI] [PubMed] [Google Scholar]
- 32.Ecker H, Kolvenbach S, Stranz S, Herff H, Wetsch WA. Comparison of the novel VieScope with conventional and video laryngoscope in a difficult airway scenario –A randomized, controlled simulation trial. BMC Emerg Med. 2021;21:90. doi: 10.1186/s12873-021-00484-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kristensen MS. Infrared Red Intubation System (IRRIS) guided flexile videoscope assisted difficult airway management. Acta Anaesthesiol Scand. 2017;1:7. doi: 10.1111/aas.13016. [DOI] [PubMed] [Google Scholar]
- 34.Van Zundert AAJ, Gatt SP, Van Zundert TCRV, Kumar CM, Pandit JJ. Features of new vision incorporated third generation video laryngeal mask airways. J Clin Monit Comput. 2022;36:921–8. doi: 10.1007/s10877-021-00780-3. [DOI] [PubMed] [Google Scholar]
- 35.Levin BS, Chang MG, Bittner EA. Teleguidance technology for endotracheal intubation:A scoping review. Crit Care Explor. 2021;3:e0582. doi: 10.1097/CCE.0000000000000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–52. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 37.Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136:31–81. doi: 10.1097/ALN.0000000000004002. [DOI] [PubMed] [Google Scholar]
- 38.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Law JA, Duggan LV, Asselin M, Baker P, Crosby E, Downey A, et al. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway:Part 1. Difficult airway management encountered in an unconscious patient. Can J Anaesth. 2021;68:1373–404. doi: 10.1007/s12630-021-02007-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chrimes N, Higgs A, Hagberg CA, Baker PA, Cooper R, Greif R, et al. Preventing unrecognized oesophageal intubation:A consensus guideline from the Project for Universal Management of Airways and international airway societies. Anaesthesia. 2022;77:1395–415. doi: 10.1111/anae.15817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radhakrishnan B, Katikar MD, Myatra SN, Gautam PL, Vinayagam S, Saroa R. Importance of non-technical skills in anaesthesia education. Indian J Anaesth. 2022;66:64–9. doi: 10.4103/ija.ija_1097_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Edelman DA, Duggan LV, Lockhart SL, Marshall SD, Turner MC, Brewster DJ. Prevalence and commonality of non-technical skills and human factors in airway management guidelines:A narrative review of the last 5 years. Anaesthesia. 2022;77:1129–36. doi: 10.1111/anae.15813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cook TM, Woodall N, Frerk C Fourth National Audit Project. Major complications of airway management in the UK:Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1:Anaesthesia. Br J Anaesth. 2011;106:617–31. doi: 10.1093/bja/aer058. [DOI] [PubMed] [Google Scholar]
- 44.Myatra SN, Kalkundre RS, Divatia JV. Optimizing education in difficult airway management:Meeting the challenge. Curr Opin Anaesthesiol. 2017;30:748–54. doi: 10.1097/ACO.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 45.Chrimes N. The Vortex:A universal “high-acuity implementation tool”for emergency airway management. Br J Anaesth. 2016;117(Suppl 1):i20–7. doi: 10.1093/bja/aew175. [DOI] [PubMed] [Google Scholar]
- 46.Chrimes N, Bradley WPL, Gatward JJ, Weatherall AD. Human factors and the “next generation”airway trolley. Anaesthesia. 2019;74:427–33. doi: 10.1111/anae.14543. [DOI] [PubMed] [Google Scholar]
- 47.Chrimes N, Higgs A, Law JA, Baker PA, Cooper RM, Greif R, et al. Project for universal management of airways - Part 1:Concept and methods. Anaesthesia. 2020;75:1671–82. doi: 10.1111/anae.15269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duggan LV, Lockhart SL, Cook TM, O'Sullivan EP, Dare T, Baker PA. The Airway App:Exploring the role of smartphone technology to capture emergency front-of-neck airway experiences internationally. Anaesthesia. 2018;73:703–10. doi: 10.1111/anae.14247. [DOI] [PubMed] [Google Scholar]