Abstract
BACKGROUND
Turning may be particularly challenging for stroke patients leading to decreased mobility and increased functional restriction. Timed up and go instrumentation using a simple technology in the clinical context could allow for the collection of both traditional and potentially more discriminatory variables in turning ability.
AIM
Determine whether the speed turning metrics obtained by a single inertial sensor are suitable for differentiating between stroke patients with varying levels of mobility and disability.
DESIGN
Cross-sectional study.
SETTING
Outpatients setting.
POPULATION
Chronic stroke patients.
METHODS
A total of 48 chronic stroke patients and 23 healthy controls were included. Stroke patients were divided in two groups based on the total iTUG score: an impaired mobility (> 20 seconds) and an available mobility (<20 seconds) group. All subjects performed an instrumented Timed Up and Go (iTUG) wearing a single IMU sensor on the lower back. Time of subcomponents of the timed up and go test and kinematic parameters of turning were quantified. Other clinical outcomes were: 10 meters walk test, Functional Ambulation Categories Scale (FAC), the Rivermead Mobility Index (RMI), Modified Rankin Scale and the Saltin–Grimby Physical Activity Level Scale (SGPALS).
RESULTS
There were significant differences (P<0.01) in iTUG phases and turning speeds among groups. Low to strong significant correlations were found between measures derived from the turning speeds and clinical measures. The area under the curve (AUC) of Receiver Operating Characteristic (ROC) turning speeds was demonstrated to be able to discriminate (AUC: 0.742-0.912) from available to impaired stroke patients.
CONCLUSIONS
This study provides evidence that turning speeds during timed up and go test are accurate measures of mobility and capable of discriminating stroke patients with impaired mobility from those with normal mobility.
CLINICAL REHABILITATION IMPACT
The turning metrics are related to impairment and mobility in chronic stroke patients; hence they are important to include during clinical evaluation and may assist in creating a customized strategy, assess potential treatments, and effectively organize recovery.
Key words: Stroke, Mobility limitation, Physical functional performance
Different degrees of turns, starting from a standing posture or while walking, occur naturally during daily activities, and the capacity to turn is crucial to an individual’s quality of life. Turning is more complex and demanding than linear gait as it requires additional neural resources to plan and coordinate postural transitions, coupling between the balance and gait control systems, and spatial coordination between limbs.1 This is especially true for stroke patients who have significant physical and cognitive impairments that affect their ability to turn safely and can predispose them to an abnormal turning pattern and limitation of activities. In fact, turning may be particularly challenging for stroke patients and it has been demonstrated that stroke patients need a greater number of steps and amount of time to complete turns.2 Moreover, turning impairment is associated with an increased risk of falling and falls are eight times more likely to occur while turning than when going straight forward.3 As such, turning assessments may be more sensitive to evaluating mobility than gait assessments alone.
The Timed-Up-and-Go (TUG) is a simple performance test commonly used to assess functional mobility in stroke patients and could provide some information about turning movement. In fact, the patient was asked to stand up from a seated position, walk 3 meters, turn around 180°, walk back 3 meters, turn around 180° and sit back down again. It is a simple test, easy to administer, fast and with excellent intra and inter-rater reliability, a good convergent validity, and sensitivity to detect small changes, making it a valid instrument to monitor stroke patients who can walk.4 The score is given by the total time the patient takes to complete the task. Indeed, the TUG combines different mobility functions and the different subcomponents of TUG are complex activities on their own. The use of whole time as an outcome metric for the TUG has one disadvantage: it combines the trial’s overall performance into a single measure, making it harder to distinguish between individual components’ performance. In recent decades, technological improvements have coincided with the need to improve the parameterization of the TUG test, leading to the development of an instrumented version of the test (iTUG). Timed up and go instrumentation could include an accelerometer, gyroscope, optoelectronic system, and motion-sensing camera. Due to their small size and wearability, inertial sensors have recently become easier and less expensive to use in rehabilitative settings, allowing for reliable quantification of iTUG turning subcomponents.5 The reliability and validity of the iTUG using different types of sensors and settings have already been demonstrated in different populations like community-dwelling older adults,6-8 patients with Parkinson’s Disease,9, 10 Multiple Sclerosis11 or Stroke12, 13 or other neurological condition,14 obese women15 and children with cerebral palsy.16
Few studies investigated the 180° turning in stroke subjects: spatiotemporal and kinematic parameters were evaluated by mean of an optoelectronic motion capture system, body-fixed inertial sensors or cameras.17-19 Other studies investigating whether the iTUG turning parameters are able to discriminate between falls and non-fallers founded than iTUG was unable to improve fall risk classification.7, 20 Finally, recent studies have investigated 360 ° turns with both inertial sensor and force plates, as everyday activities involve varying degrees of turning, from slight to complete turns.21, 22
We recognize the significance of these turning metrics, thus we would investigate parameters like average and peak angular speed during a 180° turn while performing an iTUG test with a single inertial sensor on the lower back. We expected that stroke patients would take longer to turn and have a slower turn speed than healthy people. Furthermore, we wanted to see if these speed metrics can distinguish between stroke patients with varying levels of mobility and disability, providing clinicians with a better understanding of their patients’ ability to turn. Thus, the aim of this study was to quantitatively categorize two separate mobility groups using cut-off values of speed turning in chronic stroke patients. Our hypothesis is that turning speed measurements during iTUG with a single inertial sensor on the lower back could lead to a viable and sensitive screening tool for identifying stroke patients with various degrees of mobility impairment.
Materials and methods
Study design and participants
The study was a cross-sectional study following the STrengthening The Reporting of OBservational studies in Epidemiology (STROBE) guideline23 in the conduct and reporting of the study.
We included outpatients admitted to the Department of Physical Medicine and Rehabilitation, OORR Foggia, Italy from January to October 2021. Inclusion criteria were: 1) age over 18 years; 2) single unilateral stroke with hemiparesis at least 6 months prior to enrolment in the study; 3) ability to walk 10 meters independently/without assistance with the possible use of walking aids or orthoses; 4) non-use of Botulinum toxin type A for lower limb spasticity <4 months prior to study entry; 5) ability to provide informed consent and follow instructions. Participants were excluded if there was any additional concomitant neurological disease such as neurodegenerative disease or dementia or musculoskeletal condition that could have influenced performance in the test procedures.
Age-matched healthy subjects were also recruited and volunteered as the control group. The selection criteria for the controls were ambulatory with no history of musculoskeletal or neurological injuries.
The study was approved by the board of local ethics committee of University Hospital “Policlinico-Ospedali Riuniti”, Foggia, Italy (n136/CE/2021), and all participants provided written consent to participate. All procedures were carried out according to the latest version of the Declaration of Helsinki.
iTUG
The iTUG was performed by the participants in a quiet room. Instructions were provided to the patients using TUG Test: the patient sits in the chair (46 cm high) with armrests, walks for 3 meters at a comfortable speed along a ribbon placed on the ground, turns around and goes back up, walks the path in the opposite direction, turns around again and sits down.24 Orthosis and assistive device typically used in community by each participant were permitted.
No restrictions were given about the turning side and participants could turn spontaneously on both sides. Each subject completed three trials with a 30 seconds rest period between each trial. The best result out of the three was considered for the analysis.
The iTUG tests were performed using a wearable inertial sensor (G-Sensor®, BTS Bioengineering S.p.A., Garbagnate Milanese, Milan, Italy) placed to the lower back of participants (second lumbar vertebra) with an elastic band. The sensor has a weight of 37gr and dimension of 70x40x18mm and was composed of a triaxial accelerometer 16 bit/axes (sensor range, 2 g), a triaxial magnetometer 13 bit (1200 T), and a triaxial gyroscope 16 bit/axes (sensor range, 2000/s). The signals were sampled at a frequency of 100 Hz and transmitted via Bluetooth to a laptop computer for acquisition and processing using a dedicated software package (BTS®G- Studio, BTS Bioengineering, Italy). The total iTUG time was determined, as well as the following subcomponents: sit to stand, forward motion, mid turning, return gait, end turning, and stand to sit. Duration of test (seconds), duration of the single subcomponents (seconds), the peak angular velocity (PA °/s) and the average angular velocity (AA °/s) during mid turning around the cone and end turning before sitting were calculated.
Previous studies reported an overall good-to excellent test–retest reliability for most parameters considered in the present study.10, 25
Clinical measures
Participant characteristics and the variables of interest were assessed at baseline by the same experienced physicians. The following evaluations were performed:
10 meters walk test (10mwt): The walking velocity (m/s) to walk straight 10 m with 2 m of acceleration and 2 m of deceleration at their comfortable walking pace with the subject’s usual shoes was calculated. Aids were permitted when needed. The mean of three trials was calculated.26
Rivermead Mobility Index (RMI): a unidimensional questionnaire that includes 15 items related to bed mobility, transfers, walking, stairs use, and running. All items are rated in a yes/no format with positive responses scoring a 1 for a maximal RMI score of 15.27
Modified Rankin Scale (mRS): a single-item disability rating scale that measures functional independence in daily activities. The scale measures disability using a grading system that ranges from zero (no disability) to five (severe disability).28
Saltin-Grimby Physical Activity Level Scale (SGPALS): a self-reported questionnaire with 4 different levels of activity from sedentary (level one) to regular vigorous physical activities (level four).29
Functional Ambulation Categories scale (FAC): a 6-point (0-5) scale that measures the need for support during ambulation from inability (0 points) to independence in walking (5 points).30
Statistical analysis
We performed a descriptive statistic to estimate frequency of all variables. Quantitative variables were reported as mean±standard deviation. Ordinal variables were reported with median and range. We performed the Shapiro-Wilk test for distribution. Pearson Chi-square test or Fisher test were performed for categorical variables and Mann u Whitney or Kruskal Wallis for continuous variables to compare demographic characteristics and functional outcomes. Accordingly, we used a non-parametric Kruskal-Wallis test and a post hoc analysis with Bonferroni correction to compare mobility available, impaired and healthy into each phase of iTUG. Eta square was computed to analyze the effect size where 0 indicates no relationship and 1 indicates a perfect relationship. Spearman rho correlation test was used to examine the relationship between total time of iTUG, average angular (AA) speed, Peak angular (PA) speed and demographic characteristics and other evaluation measures. Correlation was considered excellent if >0,70, moderate if between 0,50 and 0,69 and poor if correlation coefficients <0.49.31
The cut off values of AA and PA speed during MT and ET between the mobility impaired and mobility available groups were determined by analyzing the receiver operating characteristics (ROC). Sensitivity and specificity with confidence interval (CI 95%) and positive/negative likelihood ratio (LR +/LR -), were also determined.
An area under the curve (AUC) value of 0,9 and greater indicates high discrimination, 0.7–0.9 indicates moderate discrimination, 0.5-0.7 indicates low discrimination, and 0,5 and less indicates a non-significant discrimination. The Youden Index was used to find out the optimal cut off. Likelihood ratio was calculated to determine the accuracy i.e. the probability to discriminate mobility groups by means of these cut off. The data were analyzed through IBM SPSS version 26 (IBM Corp, Armonk, USA) and MedCalc version 19 statistical software. The level of statistical significance was set at P<0.05.
Sample size
We calculated that an adequate sample size for ROC analyses with AUC>0.740 and P<0.5 as a null hypotesis (Type I error 0.05 and; type II error of 0.20; ratio negative/positive of 1.3) was 44.
Data availability
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
Results
Forty-eight stroke patients were included in this study (22 female and 26 male), mean age 60.87±11.46 years. Based on total TUG time we divided stroke populations into two subgroups: mobility impaired who performed >20 seconds and mobility available who completed in ≤20 seconds. Twenty-three healthy subjects (13 male and 10 female), aged 60.95±13.10 years, with no history of walking and/or cognitive impairments, served as controls. All demographic characteristics and functional outcomes are described in Table I.
Table I. —Subject characteristic and functional outcomes.
| Mobility impaired N.=27 |
Mobility available N.=21 |
Healthy N.=23 |
P value | |
|---|---|---|---|---|
| Age (mean±SD) years | 61.22±11.82 | 60.42±11.26 | 60.5±13.10 | 0.586 |
| Gender (M/F) | 14/13 | 13/8 | 12/10 | 0.448 |
| Height (mean±SD) cm | 164.48±7.22 | 167.14±10.98 | 165.86±9.2 | 0.761 |
| Weight (mean±SD) Kg | 70.22±12.88 | 75.47±15.99 | 73.27±13.70 | 0.348 |
| BMI (mean±SD) Kg/m2 | 25.88±3.88 | 26.99±5.10 | 26.65±4.67 | 0.805 |
| Type of stroke (Hemorrhagic/Ischemic) | 12/15 | 9/12 | - | 0.912 |
| Side (left/right) | 15/12 | 7/14 | - | 0.125 |
| Time since stroke (mean±SD) years | 3.11±4.57 | 3.04±4.44 | - | 0.568 |
| 10 mwt (mean±SD) m/s | 0.45±0.18 | 0.85±0.25 | - | 0.001 |
| mRS (median) Min/Max | 3 (2/4) | 2 (1/4) | - | 0.001 |
| FAC (median) Min/ Max | 3 (3/4) | 4 (3/5) | - | 0.001 |
| SGPALS (median) Min/Max | 1 (1/2) | 2 (1/3) | - | 0.001 |
| RMI | 7 (5/9) | 11 (6/14) | - | 0.001 |
| Aid-Orthosis (no/yes) | 13/14 | 20/1 | - | 0.001 |
SGPALS: Saltin–Grimby Physical Activity Level Scale; FAC: functional ambulation categories; mRS: modified Rankin scale; 10 mwt: 10 meter walk test; RMI: Rivermead mobility index; PA: peak angular; AA: average angular.
No differences were found among demographic characteristics. Significant differences were found between two subgroups of stroke patients in all clinical outcomes (P<0.05).
A Kruskal-Wallis test showed significant differences among mobility impaired, mobility available and healthy populations. Pairwise comparisons indicated that the healthy population performed significantly better than mobility impaired and mobility available while mobility available performed significantly better than impaired except for sit to stand and stand to sit phases where non-significant differences (low effect size) were found. Table II reports mean values of each iTUG phases, significance with effect size, mid/end turning speeds and pairwise comparisons with Bonferroni corrections.
Table II. —Kruskal-Wallis Test with pairwise comparisons of iTUG parameters between groups with a Bonferroni Correction.
| iTUG | Mobility available mean±SD |
Mobility impaired mean±SD |
Healthy mean±SD |
P value (effect size) | P* impaired- available | P* impaired- healthy | P* available- healthy |
|---|---|---|---|---|---|---|---|
| Duration (s) | 15.19±2.87 | 31.72±10.97 | 9.13±1.60 | <0.001 (0.86) | <0.001 | <0.001 | 0.003 |
| Sit to Stand (s) | 1.55±0.50 | 1.95±0.74 | 1.08±0.26 | <0.001 (0.34) | 0.377 | <0.001 | 0.004 |
| Forward Gait (s) | 2.96±0.92 | 9.36±4.56 | 1.83±0.44 | <0.001 (0.80) | <0.001 | <0.001 | 0.020 |
| Mid Turning (s) | 3.60±1.19 | 5.75±2.34 | 1.87±0.62 | <0.001 (0.69) | 0.009 | <0.001 | 0.001 |
| Return Gait (s) | 2.67±0.71 | 8.22±4.81 | 1.63±0.48 | <0.001 (0.75) | <0.001 | <0.001 | 0.012 |
| End Turning (s) | 2.57±0.68 | 4.36±1.92 | 1.39±0.52 | <0.001 (0.68) | 0.007 | <0.001 | 0.001 |
| Stand to Sit (s) | 1.82±0.54 | 2.08±0.89 | 1.34±0.31 | <0.001 (0.20) | 1 | <0.001 | 0.014 |
| Average angular speed (°/s) MT | 53.79±17.67 | 33.11±12.37 | 89.90±9.49 | <0.001 (0.69) | 0.007 | <0.001 | 0.001 |
| Peak angular speed MT (°/s) | 117.41±37.37 | 83.05±23.11 | 168.18±42.00 | <0.001 (0.58) | 0.014 | <0.001 | 0.004 |
| Average angular speed (°/s) ET | 62.37±17.69 | 34.91±11.69 | 118.51±35.88 | <0.001 (0.76) | 0.001 | <0.001 | 0.002 |
| Peak angular speed (°/s) ET | 133.55±42.97 | 85.77±19.73 | 212.15±46.34 | <0.001 (0.68) | 0.003 | <0.001 | 0.002 |
P*: adjusted p-value based on Bonferroni’s correction; significance value: P<0.05. MT: mid turning; ET: end turning; s: seconds; SD: standard deviation.
Turning speeds demonstrate low to strong relationships with other outcome measures in our stroke population as shown in Table III. Conversely, non-significant relationship was found with patients’ demographic characteristics (P>0.05).
Table III. —Spearman rho correlations between turning speed parameters and functional outcomes.
| AA Speed MT | PA Speed MT | AA Speed ET | PA Speed ET | |
|---|---|---|---|---|
| SGPALS | 0.416* | 0.329* | 0.615** | 0.600** |
| FAC | 0.503** | 0.396* | 0.656** | 0.650** |
| mRS | -0.527** | -0.460** | -0.773** | -0.594** |
| 10 mwt | 0.656** | 0.591** | 0.625** | 0.534** |
| RMI | 0.595** | 0.540** | 0.769** | 0.712** |
*significance value P<0.05; **significance value P<0.001.ITUG: instrumented timed up and go; SGPALS: Saltin–Grimby Physical Activity Level Scale; FAC: functional ambulation categories; mRS: modified Rankin scale; 10 mwt: 10 meter walk test; RMI: Rivermead mobility index; PA: peak angular; AA: average angular; MT: mid turning; ET: end turning.
ROC curves were constructed for turning speed in mid turning and end turning (Figure 1). Table IV shows the Area under the curve (AUC) with the optimal cut-off point of the average and peak speed of mid turning and end turning of iTUG. Each cut-off demonstrated moderate to high discriminance (AUC: 0.742-0.912) from available to impaired stroke patients. The optimal sensitivity and specificity, the positive and negative likelihood ratios are also reported in Table IV.
Figure 1.
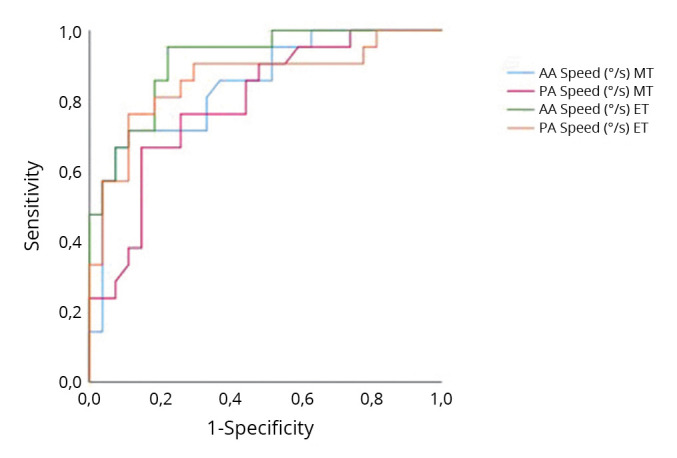
—Receiving operating characteristics curves (ROC) for turning speed in mid turning (MT) and end turning (ET).
Table IV. —The AUC. sensitivity. specificity and likelihood ratio for each turning speed parameters to detect the mobility subgroup of stroke patients.
| AUC | cut-off (°/s) | Sensitivity % (95% CI) | Specificity % (95% CI) | +LR | -LR | |
|---|---|---|---|---|---|---|
| AA Speed MT | 0.844 | 41.9 | 88.89 (70.8-97.6) | 71.43 (43-85.4) | 2.67 | 0.17 |
| PA Speed MT | 0.792 | 101.5 | 85.19 (66.3-95.8) | 66.67 (43-85.4) | 2.56 | 0.22 |
| AA Speed ET | 0.912 | 39.1 | 77.78 (57.7-91.4) | 95.24 (76.2-99.9) | 10.11 | 0.54 |
| PA Speed ET | 0.859 | 102.2 | 88.89 (70.8-97.6) | 76.19 (52.8-91.8) | 3.42 | 0.24 |
AUC: area under the curve; PA: peak angular; AA: average angular; MT: mid turning; ET: end turning; CI: confidence interval; LR: likelihood ratio.
Discussion
This study aimed to investigate whether the speed of 180-degree turning task explored during an instrumented TUG test using a single wearable sensor could be used to identify stroke patients from healthy controls and to define two separate mobility groups among stroke patients. Overall, our data suggest that information from an inertial sensor placed on the lower back can effectively describe changes in mobility.
In line with previous findings,17, 19, 32, 33 all iTUG measures (total duration, subtasks duration, AA and PA speed of turning) showed significant differences between healthy controls and stroke patients. As expected, stroke patients take substantially longer to complete the entire task and all the subtasks. Furthermore, at both mid and end turning, stroke patients have lower average and PA speeds. Poor neuromuscular control, gait asymmetry, lower limb weakness, poor capacity to manage postural balance, loss of coordination, visual impairments, fear of falling, and possibly attention deficiencies, all of which are frequent in stroke patients, can explain this difference.2
Due to difficulties in performing turns, stroke patients may avoid 180-degree turns resulting in decreased mobility and increased functional restriction. In fact, turning is a fundamental component of mobility as it occurs frequently during daily tasks and turning assessments may be more sensitive to mobility disability than gait assessment alone.
Mobility is a domain of the Activities and Participations component of the International Classification of Functioning Disability and Health (ICF) framework and because its multidimensional characteristic and complex interaction of bio-psychosocial variables, choosing a measure of mobility might be difficult for clinicians. TUG is a widely used measure of mobility in older people and neurological populations, including stroke patients, with excellent intra and inter-rater reliability, good convergent validity, and sensitivity to detect small changes, making it a valid instrument to monitor stroke patients who can walk.4 When assessing mobility, we should consider two constructs: “capacity” as the highest level of functioning that a person can reach, typically evaluated in laboratory or hospital settings; and “performance” as what an individual does in his current environment. Both of the two constructs influenced the physical activity levels, another crucial aspect in disability management and progression. In fact, it should be noted that the levels of physical activity in people with stroke are lower than those of controls and do not appear to meet the guidelines.34 People who have had a stroke spend long periods inactive and sedentary throughout all stages following stroke, particularly during the acute phase. Our data are in line with the literature showing a discrepancy between capacity and performance:35 in our sample 76% of participants were limited or non-limited community ambulators and only 23% were house ambulators; by contrast the majority (60.4% of patients) were mostly sedentary or inactive; 29.2% performed light physical activity and only 10.4% performed regular physical activity. Inactivity may be a key confounder when assessing the level of disability and mobility in chronic stroke patients, this component should be considered both during the assessment and the rehabilitation process. Furthermore, increasing physical activity and developing standardized activity targets may be beneficial for rehabilitation therapy at all stages of stroke recovery.36, 37 Clearly, the goal must be to promote capacity for improvement in actual performance, and in order to effectively plan rehabilitation and compare different interventions, a thorough understanding of the nature and severity of mobility and turning difficulties among chronic stroke patients is required.
Recently, there is growing interest in the comprehension and detailed knowledge of the turning characteristics in stroke patients. Abdolli et al.21 found that stroke patients were slower and turned 360° with a reduced angular velocity but a greater range of trunk motions than age-matched controls. Chen et al.38 investigated the role of the trunk in the 180° rotation, evaluating the activation pattern of the extensor and flexor trunk muscles throughout the task and discovered that stroke patients had more trunk muscle activity and a unique activation pattern than healthy controls. The author interpreted this as a means to compensate for the inadequate motor control of the lower limb and to promote stability. Furthermore, Liang et al.39 observed that a reduction in trunk flexibility, strength, and motor control could affect stroke turning performance, particularly when turning toward the paretic side. Exploration of the turning characteristics in stroke patients may aid in the development of a specialized approach with the objective to assess various interventions and organize rehabilitation effectively. Exploring the turning characteristics in stroke patients may help design a tailored approach, evaluate various interventions and efficiently organize rehabilitation. For this purpose, we offered a simple and quick parameter, such as turning speed, available by a single inertial sensor.
Importantly, our study revealed that stroke patients with a major mobility impairment turned with a longer duration and with a less speed than the stroke patients with a lower mobility impairment. As in previous studies,24, 40 stroke patients were divided into two groups according to the total time taken to perform the TUG test: the mobility-available group, which completes the TUG in equal or less than 20 seconds and is considered “independent mobile,” and the mobility-impaired group, which takes more than 20 seconds to complete the iTUG and generally requires assistance with basic activities. All the analysed iTUG metrics show a significant difference between the two groups, with the exception of sit to stand and stand to sit duration. In particular, the mobility-available individuals take 3.60±1.19 s and 2.57±0.68 s to complete the mid turn and the end turn, whereas the mobility impaired individuals take 5.75±2.34 s and 4.36±1.92 s. Moreover, the turning speed parameters, such as AA and PA speed during mid and turning, showed a significant difference. All this confirms the hypothesis that was raised at the beginning of this study: iTUG turning speed appears a reliable tool in classifying groups with different mobility.
Therefore, we calculated the cut-off value of AA speed and PA speed that could be used as a reference point to estimate the mobility level. Specifically, the values are 41.9 °/s and 39.1°/s for AA speed in mid and end turning respectively, and 101.5 °/s and 102.2 °/s for PA speed in mid and end turning respectively showed a moderate to high accuracy in classifying mobility groups as available or impaired. Among the parameters, AA speed end turning was the one with the highest accuracy (0.912 AUC) and a good specificity (95.24%) and sensitivity (77.78%).
Our study also found that speed turning is associated with all the functional outcomes related to disability, ambulation category, physical activity level and mobility. These findings suggested that turning speed could be a helpful clinical metric and a valid tool for classifying stroke patients globally. Moreover, the results of the correlation analysis suggest that gait speed, as assessed by the 10mwt, played a relevant role in turning performance, consistent with what is reported in literature. Walking speed just before and during turning may influenced axial coordination and rotation41, 42 and turning at a slow pace may hamper medio lateral stability in older adults.43
Limitations of the study
We acknowledge that this study has limitations. First, the sample size was limited: a larger sample of chronic stroke patients would be more representative and would allow the results to be more generalizable and broadly applied. Second, the use of a single sensor is not without risks: a comparison to the gold standard technique (optoelectronic system) is advisable to confirm the results. The test may be affected by several factors, including changes in sensor inclination during walking and differences in sensor placements. Third, the design of the study did not allow for correlation of these parameters with the presence or absence of falls risk and the response to various interventions.
Further research should investigate the potential of the iTUG and speed turning parameters to stratify and monitor the stroke patients over time, to assess the response and benefits to various therapeutic interventions and to identify which stroke patients are at risk of falling.
Conclusions
Our findings suggest that placing a sensor on the lower back and measuring the average and PA speeds during the turning transition can provide information related to disability and mobility in stroke patients. Evaluation of mobility in people who have had a stroke is crucial in clinical settings for a variety of reasons, including making an accurate diagnosis, planning the treatment technique for each particular patient, and evaluating the effectiveness of rehabilitation. The iTUG turning speed has the potential to provide clinically helpful information by objectively monitoring a patient’s mobility after a stroke.
References
- 1.Herman T, Giladi N, Hausdorff JM. Properties of the ‘timed up and go’ test: more than meets the eye. Gerontology 2011;57:203–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20484884&dopt=Abstract https://doi.org/ 10.1159/000314963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lam T, Luttmann K. Turning capacity in ambulatory individuals poststroke. Am J Phys Med Rehabil 2009;88:873–83, quiz 884–6, 946. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19893383&dopt=Abstract 10.1097/PHM.0b013e3181bc0ddf [DOI] [PubMed]
- 3.Hyndman D, Ashburn A, Stack E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil 2002;83:165–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11833018&dopt=Abstract 10.1053/apmr.2002.28030 [DOI] [PubMed] [Google Scholar]
- 4.Hafsteinsdóttir TB, Rensink M, Schuurmans M. Clinimetric properties of the Timed Up and Go Test for patients with stroke: a systematic review. Top Stroke Rehabil 2014;21:197–210. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24985387&dopt=Abstract 10.1310/tsr2103-197 [DOI] [PubMed] [Google Scholar]
- 5.Porciuncula F, Roto AV, Kumar D, Davis I, Roy S, Walsh CJ, et al. Wearable Movement Sensors for Rehabilitation: A Focused Review of Technological and Clinical Advances. PM R 2018;10(Suppl 2):S220–32. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30269807&dopt=Abstract 10.1016/j.pmrj.2018.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mangano GR, Valle MS, Casabona A, Vagnini A, Cioni M. Age-related changes in mobility evaluated by the timed up and go test instrumented through a single sensor. Sensors (Basel) 2020;20:719. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32012930&dopt=Abstract 10.3390/s20030719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jackson K, Sample R, Bigelow K. Use of an Instrumented Timed Up and Go (iTUG) for Fall Risk Classification. Sensors 2019;36:354–65. [Google Scholar]
- 8.Sample RB, Kinney AL, Jackson K, Diestelkamp W, Bigelow KE. Identification of key outcome measures when using the instrumented timed up and go and/or posturography for fall screening. Gait Posture 2017;57:168–71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28645093&dopt=Abstract 10.1016/j.gaitpost.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 9.Van Uem JM, Walgaard S, Ainsworth E, Hasmann SE, Heger T, Nussbaum S, et al. Quantitative timed-up-and-go parameters in relation to cognitive parameters and health- related quality of life in mild-to-moderate Parkinson’s disease. PLoS One 2016;11:e0151997. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27055262&dopt=Abstract 10.1371/journal.pone.0151997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kleiner AF, Pacifici I, Vagnini A, Camerota F, Celletti C, Stocchi F, et al. Timed Up and Go evaluation with wearable devices: validation in Parkinson’s disease. J Bodyw Mov Ther 2018;22:390–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29861240&dopt=Abstract https://doi.org/ 10.1016/j.jbmt.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 11.Hershkovitz L, Malcay O, Grinberg Y, Berkowitz S, Kalron A. The contribution of the instrumented Timed-Up-and-Go test to detect falls and fear of falling in people with multiple sclerosis. Mult Scler Relat Disord 2019;27:226–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30415024&dopt=Abstract 10.1016/j.msard.2018.10.111 [DOI] [PubMed] [Google Scholar]
- 12.Vernon S, Paterson K, Bower K, McGinley J, Miller K, Pua YH, et al. Quantifying individual components of the timed up and go using the kinect in people living with stroke. Neurorehabil Neural Repair 2015;29:48–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24743227&dopt=Abstract 10.1177/1545968314529475 [DOI] [PubMed] [Google Scholar]
- 13.Hollands KL, Agnihotri D, Tyson SF. Effects of dual task on turning ability in stroke survivors and older adults. Gait Posture 2014;40:564–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25086799&dopt=Abstract 10.1016/j.gaitpost.2014.06.019 [DOI] [PubMed] [Google Scholar]
- 14.Caronni A, Sterpi I, Antoniotti P, Aristidou E, Nicolaci F, Picardi M, et al. Criterion validity of the instrumented Timed Up and Go test: A partial least square regression study. Gait Posture 2018;61:287–93. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29413799&dopt=Abstract 10.1016/j.gaitpost.2018.01.015 [DOI] [PubMed] [Google Scholar]
- 15.Cimolin V, Cau N, Malchiodi Albedi G, Aspesi V, Merenda V, Galli M, et al. Do wearable sensors add meaningful information to the Timed Up and Go test? A study on obese women. J Electromyogr Kinesiol 2019;44:78–85. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30551006&dopt=Abstract 10.1016/j.jelekin.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 16.Newman MA, Hirsch MA, Peindl RD, Habet NA, Tsai TJ, Runyon MS, et al. Carolinas Trauma Network Research Group . Use of an instrumented dual-task timed up and go test in children with traumatic brain injury. Gait Posture 2020;76:193–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31862669&dopt=Abstract 10.1016/j.gaitpost.2019.12.001 [DOI] [PubMed] [Google Scholar]
- 17.Wüest S, Massé F, Aminian K, Gonzenbach R, de Bruin ED. Reliability and validity of the inertial sensor-based Timed “Up and Go” test in individuals affected by stroke. J Rehabil Res Dev 2016;53:599–610. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27898161&dopt=Abstract 10.1682/JRRD.2015.04.0065 [DOI] [PubMed] [Google Scholar]
- 18.Faria CD, Paula de Carvalho-Pinto B, Nadeau S, Teixeira-Salmela LF. 180° turn while walking: characterization and comparisons between subjects with and without stroke. J Phys Ther Sci 2016;28:2694–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27821916&dopt=Abstract 10.1589/jpts.28.2694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonnyaud C, Pradon D, Vuillerme N, Bensmail D, Roche N. Spatiotemporal and Kinematic Parameters Relating to Oriented Gait and Turn Performance in Patients with Chronic Stroke. PLoS One 2015;10:e0129821. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26091555&dopt=Abstract 10.1371/journal.pone.0129821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zou TE, Liang PJ, Lee SC. Turning duration and steps predict future falls in poststroke hemiplegic individuals: A preliminary cohort study. Top Stroke Rehabil 2021;28:33–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32397952&dopt=Abstract 10.1080/10749357.2020.1760644 [DOI] [PubMed] [Google Scholar]
- 21.Abdollahi M, Kuber PM, Shiraishi M, Soangra R, Rashedi E. Kinematic Analysis of 360° Turning in Stroke Survivors Using Wearable Motion Sensors. Sensors (Basel) 2022;22:385. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35009931&dopt=Abstract 10.3390/s22010385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soangra R, Krishnan V, John J, Rashedi E, McKenzie A. Comparison of 360° Turn Cycles among Individuals after Stroke and Healthy Older Adults. Phys Ther Fac Artic Res 2021;11. 10.3390/app11073202 [DOI]
- 23.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. ; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17941715&dopt=Abstract 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=1991946&dopt=Abstract 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 25.De Ridder R, Lebleu J, Willems T, De Blaiser C, Detrembleur C, Roosen P. Concurrent Validity of a Commercial Wireless Trunk Triaxial Accelerometer System for Gait Analysis. J Sport Rehabil 2019;28:jsr.2018-0295. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30747572&dopt=Abstract 10.1123/jsr.2018-0295 [DOI] [PubMed]
- 26.Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the stroke population. Stroke 1995;26:982–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7762050&dopt=Abstract 10.1161/01.STR.26.6.982 [DOI] [PubMed] [Google Scholar]
- 27.Hsieh CL, Hsueh IP, Mao HF. Validity and responsiveness of the rivermead mobility index in stroke patients. Scand J Rehabil Med 2000;32:140–2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11028799&dopt=Abstract 10.1080/003655000750045497 [DOI] [PubMed] [Google Scholar]
- 28.Quinn TJ, Dawson J, Walters MR, Lees KR. Reliability of the modified Rankin Scale: a systematic review. Stroke 2009;40:3393–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19679846&dopt=Abstract 10.1161/STROKEAHA.109.557256 [DOI] [PubMed] [Google Scholar]
- 29.Grimby G, Börjesson M, Jonsdottir IH, Schnohr P, Thelle DS, Saltin B. The “Saltin-Grimby Physical Activity Level Scale” and its application to health research. Scand J Med Sci Sports 2015;25(Suppl 4):119–25. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26589125&dopt=Abstract 10.1111/sms.12611 [DOI] [PubMed] [Google Scholar]
- 30.Mehrholz J, Wagner K, Rutte K, Meissner D, Pohl M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch Phys Med Rehabil 2007;88:1314–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17908575&dopt=Abstract 10.1016/j.apmr.2007.06.764 [DOI] [PubMed] [Google Scholar]
- 31.Tomczak M, Tomczak E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci 2014;1:19–25. [Google Scholar]
- 32.Hollands KL, Hollands MA, Zietz D, Wing AM, Wright C, van Vliet P. Kinematics of turning 180 ° during the timed up and go in stroke survivors with and without falls history. Neurorehabil Neural Repair 2010;24:358–67. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19822720&dopt=Abstract 10.1177/1545968309348508 [DOI] [PubMed] [Google Scholar]
- 33.Barrois RP, Ricard D, Oudre L, Tlili L, Provost C, Vienne A, et al. Observational Study of 180° Turning Strategies Using Inertial Measurement Units and Fall Risk in Poststroke Hemiparetic Patients. Front Neurol 2017;8:194. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28555124&dopt=Abstract 10.3389/fneur.2017.00194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Billinger SA, Arena R, Bernhardt J, Eng JJ, Franklin BA, Johnson CM, et al. American Heart Association Stroke Council ; Council on Cardiovascular and Stroke Nursing; Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Clinical Cardiology. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:2532–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24846875&dopt=Abstract 10.1161/STR.0000000000000022 [DOI] [PubMed] [Google Scholar]
- 35.Flury D, Massé F, Paraschiv-Ionescu A, Aminian K, Luft AR, Gonzenbach R. Clinical value of assessing motor performance in postacute stroke patients. J Neuroeng Rehabil 2021;18:102. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34167546&dopt=Abstract 10.1186/s12984-021-00898-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fini NA, Holland AE, Keating J, Simek J, Bernhardt J. How Physically Active Are People Following Stroke? Systematic Review and Quantitative Synthesis. Phys Ther 2017;97:707–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28444348&dopt=Abstract 10.1093/ptj/pzx038 [DOI] [PubMed] [Google Scholar]
- 37.English C, Manns PJ, Tucak C, Bernhardt J. Physical activity and sedentary behaviors in people with stroke living in the community: a systematic review. Phys Ther 2014;94:185–96. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24029302&dopt=Abstract https://doi.org/ 10.2522/ptj.20130175 [DOI] [PubMed] [Google Scholar]
- 38.Chen IH, Liang PJ, Chiu VJ, Lee SC. Trunk Muscle Activation Patterns During Standing Turns in Patients With Stroke: An Electromyographic Analysis. Front Neurol 2021;12:769975. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34858317&dopt=Abstract 10.3389/fneur.2021.769975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liang PJ, Chiu VJ, Teng YC, Chiu HL, Lee SC. Turning difficulties after stroke and its relationship with trunk function. Eur J Phys Rehabil Med 2021;57:859–65. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34042411&dopt=Abstract 10.23736/S1973-9087.21.06841-6 [DOI] [PubMed] [Google Scholar]
- 40.Lee K, Lee D, Hong S, Shin D, Jeong S, Shin H, et al. The relationship between sitting balance, trunk control and mobility with predictive for current mobility level in survivors of sub-acute stroke. PLoS One 2021;16:e0251977. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34351943&dopt=Abstract 10.1371/journal.pone.0251977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Singh H, Sanders O, McCombe Waller S, Bair WN, Beamer B, Creath RA, et al. Relationship Between Head-Turn Gait Speed and Lateral Balance Function in Community-Dwelling Older Adults. Arch Phys Med Rehabil 2017;98:1955–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28610969&dopt=Abstract 10.1016/j.apmr.2017.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Forsell C, Conradsson D, Paquette C, Franzén E. Reducing gait speed affects axial coordination of walking turns. Gait Posture 2017;54:71–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28273601&dopt=Abstract https://doi.org/ 10.1016/j.gaitpost.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 43.Conradsson D, Paquette C, Franzén E. Medio-lateral stability during walking turns in older adults. PLoS One 2018;13:e0198455. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29870557&dopt=Abstract https://doi.org/ 10.1371/journal.pone.0198455 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.


