Abstract
BACKGROUND
Neck pain is associated with decreased health-related quality of life, decreased work productivity, and increased visits to health care providers.
AIM
The aim of this study was to assess the effectiveness of “Global Postural Re-education” (GPR) versus a neck specific exercise (SE) program on neck pain, disability, cervical range of movement, postural stability, and activity of the superficial cervical flexor muscles.
DESIGN
A parallel-group and single-blinded clinical trial.
SETTING
Community interventions.
POPULATION
Fifty women with non-specific chronic neck pain (NSCNP).
METHODS
Participants were randomly assigned to one of the two intervention groups (GPR [N.=25] or SE [N.=25]). Both interventions consisted of eight sessions of ~40 minutes duration, performed twice a week, for four weeks. Outcomes included neck pain intensity and disability, cervical range of motion (CROM), postural sway, and activity of the superficial neck flexor muscles during a cranio-cervical flexion test (CCFT). All outcomes were assessed twice before the intervention and immediately following eight treatment sessions over four weeks.
RESULTS
Both interventions were equally effective in reducing neck pain (P<0.001, ŋp2=0.770) and disability (P<0.001, ŋp2=0.306), improving neck mobility (P<0.001, 0.385≤ŋp2≤0.623, for all measurements) and decreasing the activity of the superficial cervical flexor muscles (P>0.001). Neither intervention altered postural sway.
CONCLUSIONS
Our results revealed that GPR and SE induced significant positive results in all measures apart from postural stability but with no difference between the interventions.
CLINICAL REHABILITATION IMPACT
“Global Postural Re-education” (GPR) and neck SE interventions are equally effective in reducing neck pain and disability, and improving neck mobility in women with NSCNP. Overall, this study indicates that GPR and SE interventions can be used to effectively manage patients with NSCNP.
Key words: Neck pain, Exercise, Electromyography, Postural balance
Neck pain is a highly prevalent musculoskeletal disorder and is one of the major contributors to the global burden of disability.1 Neck pain is most common in middle age, with women being affected more than men.2 The course of neck pain has a favourable prognosis for most people. Nonetheless, one-third of people still present low-grade symptoms or pain recurrence one year after treatment, often leading to chronic pain.3 Neck pain is associated with decreased health-related quality of life, decreased work productivity, and increased visits to health care providers,3 resulting in enormous costs for society.1, 3
Although neck pain can be caused by traumatic events (e.g., fracture, whiplash-associated disorder) or inflammatory disorders, most people present with non-specific neck pain as it cannot be attributed to specific causes.3-5 Nevertheless, non-specific neck pain can be accompanied by a myriad of neuromuscular and biomechanical changes including reduced range, smoothness and variability of neck movement,6 reduced directional specificity of neck muscle activity,7 poorer performance on tests of motor control,8 altered coordination between the deep and superficial neck flexors9 and delayed muscle responses to perturbations.10 Additionally, some people with chronic neck pain present with altered sensorimotor control, including deficits in proprioception, a decline in oculomotor control and poorer balance.11 These alterations, taken together, can lead to a decline in motor performance and postural stability,12 increasing the risk of falls, particularly at older ages.13 Consequently, interventions to enhance neuromuscular and sensorimotor control features are advocated for the effective clinical management of people with chronic neck pain.14
Several studies have demonstrated that different modes of exercise, including strengthening, endurance, stretching and motor control exercises, can be effective for the management of chronic neck pain, but there is no clear evidence that one particular type of exercise is more effective than another in relieving pain.15 However, few randomized controlled trials (RCTs) have examined the effect of neck exercise on neuromuscular and sensorimotor control7, 16 or they have been limited to the investigation of a single aspect of neuromuscular/sensorimotor control only, limiting the broader understanding on the benefits of a particular type of exercise program. It also remains unknown whether a more global form of exercise can change neuromuscular/sensorimotor control in a similar way to a more localized approach.
In recent years, a form of exercise termed “Global Postural Re-education” (GPR) has been introduced and is being used by clinicians worldwide.17 GPR is a method of physiotherapy, developed by Phillipe Souchard in the 1950s.18 Its therapeutic approach rests on causality, and globality and is based on the hypothesis that the muscular system is organized into muscle chains, which can be shortened as a result of musculoskeletal disorders and constitutional, behavioral and psychological factors.17-20 Based on this rationale, the GPR aims to recover muscle function and reduce postural alterations by improving body awareness and postural control management.17, 20 For this purpose, maintained postures of global stretching of the muscle chains are used with the active participation of the patient.17, 18, 20 A series of postures and gentle active movements are performed aimed at stretching shortened muscles, decompressing and aligning joints, with breathing control, contractions of antagonist muscles and sensory integration exercises to work on proprioceptive afferents and re-educate postural control.17-21
A number of studies have demonstrated the effectiveness of the GPR in treating patients with different musculoskeletal disorders.20, 22, 23 The few studies which have examined the effect of GPR on chronic non-specific neck pain have shown positive results in relieving pain, decreasing disability, and increasing flexibility and mobility of the neck.19, 20 Nonetheless, the studies on GPR need to be interpreted with caution due to the heterogeneity of the results and the low quality of the clinical trials.17 Additionally, no study has investigated whether GPR provides comparable effects to other forms of exercise, such as evidenced based specific localized strengthening and motor control training programs. Moreover, there has not been any investigation of the effects of GPR on neuromuscular or sensorimotor features in patients with chronic non-specific neck pain.
This RCT aimed to examine the effectiveness of GPR versus a neck specific exercise (SE) program on neck pain, disability, range of movement, postural stability, and activity of the superficial cervical flexor muscles. It was hypothesized that, when compared to an established SE program, GPR would induce similar changes in neck pain intensity and disability as well as similar changes in mobility, postural sway and muscle given the more global nature of the exercise program.
Materials and methods
Participants
Women with chronic non-specific neck pain were recruited from the community of Guarda County, Portugal. The participants were recruited through an online questionnaire published in social networks, advertisements in physiotherapy clinics, and by emails sent to the Polytechnic Institute of Guarda staff. The inclusion criteria were women aged between 30 and 65 years with chronic non-specific neck pain lasting for at least 12 weeks, with pain intensity greater or equal to 2 in the numerical Pain Rating Scale. Participants were excluded if they received physiotherapy treatment for their neck pain in the last 3 months or are taking any pharmacological treatment, had been diagnosed with a specific cause of neck pain, had a history of spinal surgery, or had central or peripheral neurological signs or cognitive impairment. Initially, 63 women responded to the recruitment questionnaire, of which only 52 women met the selection criteria and were recruited. All participants gave their informed written consent before inclusion in the study. The study was approved by the Ethics Committee of the University of Salamanca (458-2019) and Ethics Committee of Polytechnic Institute of Guarda (n.º2/2019) and was conducted in accordance with the Declaration of Helsinki. The clinical trial was registered in prospectively on ClínicalTrials.gov (NCT04402463).
Study design
This study was a parallel-group, single blinded controlled clinical trial. The study protocol conformed to the SPIRIT 2013 Statement,24 and the reporting of this clinical trial conforms to the CONSORT 2010 Statement (Consolidated Standards of Reporting Trials).25 The study protocol for this randomized, parallel, clinical trial was described in detail in Fernandes et al.26
The number of participants required in each group was estimated based on the potential modification of the primary outcomes, neck pain intensity and neck disability from baseline to final assessments. For repeated measurements, the sample size estimated, accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two-sided test, was of 26 participants in each group to recognise a statistically significant difference greater than or equal to 2 units (SD=1.75) (NPRS) or 7 units (SD=6) (NDI). The sample size calculated for each group, it was also considered appropriate to find an effect size of 0.8 in terms of standardized means between groups (Cohen’s d). The sample size was estimated with the software “PASS 15 (NCSS statistical software)” and “The R Project for Statistical Computing”.
Following the initial clinical interview conducted by a specialist physiotherapist, patients were randomly assigned to either the GPR or SE. The randomisation was undertaken by an independent assessor, with no other involvement in the trial, by using a computerized randomization system (randomized.com). Allocation concealment was guaranteed by sequentially numbered, opaque, sealed envelopes. The participating subjects were not blinded to the intervention, having been informed only that they would receive an effective treatment, without knowing exactly what type of intervention. The researchers who performed the study measurements of all outcome variables were blinded to the treatment performed by each participant. And the physiotherapist who provided the intervention was not blinded due to the treatment characteristics themselves, but was unaware of the outcome of the assessments.
All patients participated in three laboratory sessions, on three separate days, and in eight exercise sessions over a 4-week intervention period (2 visits per week), accompanied by an individual daily exercise program at home (Figure 1).
Figure 1.
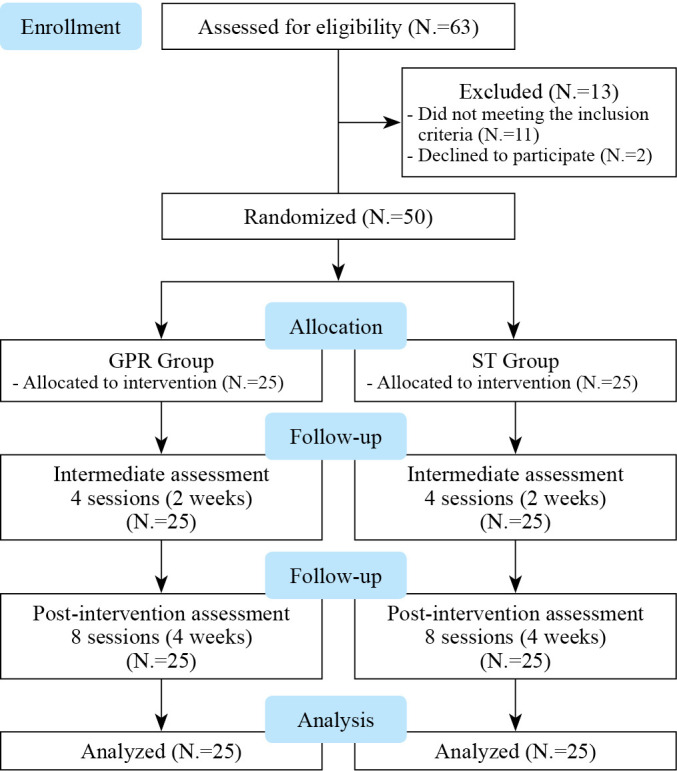
—Flow chart of the study.
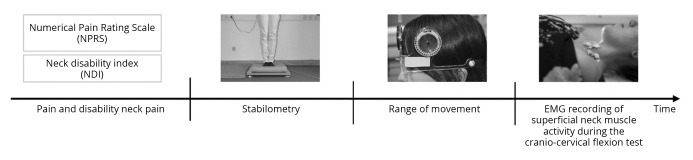
To assess day-to-day variability, two laboratory sessions were completed one week apart before the intervention (PRE1 and PRE 2). After the second assessment, participants started the intervention programs, and the last evaluation (POST) occurred 48 to 72h after the eighth treatment. All patients were assessed under the same conditions and the outcomes were measured in the following order: neck pain and disability, postural sway, cervical range of motion (CROM) and superficial neck flexor activity during performance of the cranio-cervical flexion test (CCFT) (Figure 2).
Figure 2.
—Experimental design followed in the laboratory sessions.
Outcome measures
Primary outcomes
Personal and sociodemographic variables
Individual sociodemographic factors, including age, sex, educational level, marital status, occupation, and employment status, were assessed during the first visit to the laboratory. Measures of anthropometric variables (body weight, height, Body Mass Index), neck pain duration (in months and weeks), physical activity levels and sitting time were also assessed.
Neck pain intensity and neck disability
Neck pain intensity was measured using a Numerical Pain Rating Scale (NPRS) composed of an 11-point scale, ranging from 0 (“no pain”) to 10 (“the “worst pain imaginable”).27, 28 Neck disability was measured using the Portuguese version of the Neck Disability Index (NDI-PT).28 The questionnaire has 10 items relating to daily activities (personal care, lifting, reading, headaches, concentration, work status, driving, sleeping and recreation) and cervical-spine pain. Each item is scored from 0 to 5, and the total score out of 50 points is summated.
Secondary outcomes
CROM
Assessment of neck range of motion with the CROM device was performed according to previous studies.29, 30 Individuals were seated on a chair with no backrest, with their feet on the floor, and the CROM device positioned on their heads. A magnetic collar was placed on the shoulders to take into account any rotation of the trunk, and it was always in the same position with respect to the magnetic pole. A neutral head position (e.g. anatomical position), keeping their gaze straight ahead, was established as the starting and reference positions, and the CROM device was adjusted to zero.29 Range of movement was measured with an accuracy of 1º for flexion, extension, lateral flexion, and rotation in a consistent order for all participants. All participants performed three repetitions of each movement. Subjects were instructed to perform the movement smoothly to the maximum of their capacity (until feel pain, blockage, tissue tension or a compensatory movement appeared), and the final position of each movement was recorded. At the end of each movement, the participant returned the head to the initial position. A rest interval of approximately 15 seconds was given between each measure.
Postural sway
Postural sway was measured while the participants were standing on a force platform (Kistler, model 9260AA6, Switzerland). Participants were asked to stand upright with their arms by their sides and barefoot on the top of the platform in four different positions: 1) narrow stance (feet together), with open eyes; 2) narrow stance, with closed eyes; 3) narrow stance standing on a blue pad foam (46 cm x 6 cm x 40 cm), with open eyes and, 4) narrow stance standing on foam, with closed eyes. Participants were required to maintain each position for 40 seconds, following the aforementioned order. Each position was repeated twice. Data were sampled at 1000 Hz and different parameters were computed, namely: oscillation of center of pressure (COP) (95% confidence elliptical area), mean COP velocity and anteroposterior (AP) and mediolateral (ML) COP velocity.
Electromyography
Bipolar surface electromyography (EMG) signals were detected from the sternal head of the sternocleidomastoid (SCM), and anterior scalene (AS) muscles bilaterally as participants performed the cranio-cervical flexion test. Pairs of Ag-AgCl electrodes (Ambu Neuroline; conductive area 28 mm2) were positioned 10 mm apart over the SCM and AS following skin preparation and guidelines for electrode placement.31 EMG signals were amplified as bipolar derivations (EMG amplifier; LISiN-OT Bioelettronica, Torino, Italy), band-pass filtered (- 3 dB bandwidth, 10-500 Hz), sampled at 2,048 samples/s, and converted to digital data by a 12-bit analog-to-digital (A/D) converter board. A reference electrode was placed around the right wrist.
To perform the test, the participants were comfortably positioned in supine, crook lying with the head and neck in a mid-position. Then CCFT consisted of five incremental movements of increasing cranio-cervical flexion range of motion as described previously.32 The performance was guided by visual feedback from an air-filled pressure sensor (Stabilizer, Chattanooga Group Inc., Austin, TX, USA), which was placed in the suboccipital region, and inflated to a baseline pressure of 20 mmHg. During the test, participants were required to perform gentle nodding motions of cranio-cervical flexion, progressing in ranges to increase the pressure by five incremental levels (22, 24, 26, 28, and-30 mmHg) holding each level for 10s with 30s of rest in between levels. Participants were familiarized with the task before the application of the electrodes. Afterwards, the participants performed a standardized manoeuvre for EMG normalisation that consisted of a head lift (combined cervical and cranio-cervical flexion) to just clear their head from the bed, which was maintained for 10s, during which EMG data were recorded. A one-minute rest period was given before the participants then performed the CCFT. For each level of the CCFT, the EMG recordings were initiated at the point at which the participant steadily reached the target pressure level. The average rectified value (ARV) was computed offline from the EMG signals in intervals of 1s. The ARV values were then averaged and normalized with respect to the ARV computed from the reference voluntary contraction and expressed as a percentage.
Interventions
Both interventions are described in detail in the protocol of this study.26 Briefly, both interventions consisted of eight sessions of ~40 minutes duration, performed twice a week, for four weeks. A time interval of 72h to 96h was permitted between sessions.
Global Postural Re-education
The global postural exercises consisted of three positions as described by Souchard.18 For the first position, the patient lied in supine with their shoulders abducted to 30° and the forearms supinated. The pelvis was kept in a neutral position, while the lumbar spine remained supported. This position is characterized by a progression from flexion to extension of both hips and knees (Figure 3A). For the second position, the patient remained in supine with their hips at 90° of flexion and performed gradual knee extensions (Figure 3B).
Figure 3.
—The three positions of GPR. A) Positioned in supine to stretch anteriorly; B) positioned in supine to stretch posteriorly; C) standing posture.
The participants remained between 15 and 20 minutes in each of these two positions. Under the supervision and verbal and/or manual guidance of the physiotherapist performing the intervention, they performed 5-10s isometric contractions of the antagonist muscles of the muscle chain targeted by each posture, with sufficient intensity to promote and maintain the stretching of that muscle chain. Subjects also made active adjustments to their position during the posture to achieve correct joint alignment and maintained specific control of breathing. At some point, while the patient maintained the corresponding posture, the physiotherapist could favor, with some manual contact, sustained stretching and some joint traction as previously described.18 To complete the session, the participants were requested to maintain an upright posture in standing for 5 minutes (Figure 3C).
Neck specific exercise (SE)
Participants assigned to the SE group performed SEs, as described previously.4 The protocol consisted of exercises for the cervical and axioscapular region and sensoriomotor control exercises with visual feedback with a laser pointer. The program was initiated with specific low-load exercises for both the deep neck flexors, performed in supine lying, using feedback from an air-filled pressure sensor (Stabilizer™, Chattanooga Group Inc., Chattanooga, TN, USA) and deep neck extensors as participants performed isolated neck extension in a prone position. Axioscapular muscles, particularly targeting the lower and middle fibres of the trapezius, were trained using inner range holding exercises of scapular retraction and depression, practiced initially in side lying and then prone. The participants also performed sensoriomotor control exercises with a Visual Feedback Rehab Laser (MotionGuidance®), involving relocation of the head back to a neutral posture or to predetermined points in range, as well as movements of the head to points in different directions (horizontal, vertical lines and circles) of the different designs of Motion Guidance (MotionGuidance®). The exercises followed a progression by introducing changes in direction and range of movement and variants with closed eyes and by increasing speed and tracing more intricate patterns such as a figure of eight, zig-zag or a butterfly form.
For both interventions, the exercises progressed in intensity over the duration of the training, as described in detail in Fernandes et al.26 Additionally, the patients were asked to perform their exercises at home but without the use of any equipment (Supplementary Digital Material 1: Supplementary Table I).
Statistical analysis
Data were analyzed using the IBM-SPSS software package (version 23.0). Descriptive data analysis was reported by groups as means±standard deviation for all quantitative variables. The normality of the distribution of dependent variables was confirmed using Shapiro-Wilk test. Between-group differences in age, height, and weight were assessed using independent t-tests. The Test of Levene was applied to test the homogeneity of variance in the factor of independent measures and Mauchly’s Sphericity Test for the factor of repeated measures. When the sphericity assumption was not met, the Greenhouse-Geisser correction was used. The effects of the two interventions on neck pain, neck disability, neck mobility, and COP parameters were assessed with two-way repeated-measures Analysis of Variance (ANOVA) with factors intervention (GPR vs SE) and time (PRE1, PRE2, and POST). In both groups, there was no side to side difference in the level of SCM and AS EMG amplitude, and therefore an average was taken. The effects of both interventions on CCFT performance were assessed with three-way repeated-measures ANOVA with factors intervention (GPR vs SE), pressure levels (22, 24, 26, 28, and-30 mmHg) and time (Pre1, Pre2, and Post). Partial eta-squared (ŋp2) was used to calculate the effect sizes of the statistical results, which were classified as weak (ŋp2<0.01), medium (ŋp2 0.01<0.06) or high (ŋp2>0.14).33 The significance level was set at P<0.05. Pairwise comparisons were performed with the Bonferroni post-hoc test when ANOVA was significant. The level of significance for the statistical tests was set at P≤0.05 with a confidence interval of 95%. Data are displayed as mean±standard deviation (SD) in the text and tables and as mean±standard error (SE) in the figures.
Results
Participants
Of the 52 patients recruited, 50 completed the full trial. Two patients did not complete due to the incompatibility of schedules for data collection and treatment. Thus, the results are presented for 25 subjects in each group (Table I).
Table I. —Characteristics of the participants, showing mean (standard deviation; SD) for age, height (m), weight (kg), Body Mass Index (BMI) and pain duration and then divided in the postural global re-education group (GPR) (N.=25) and specific neck exercise group (SE) (N.=25).
| Patients | Age Mean (SD) |
Height Mean (SD) |
Weight Mena (SD) |
BMI Mean (SD) |
|---|---|---|---|---|
| All participants (N.=50) | 50.82 (8.77) | 1.60 (0.05) | 62.35 (9.02) | 24.39 (3.54) |
| Postural global re-education group (N.=25) | 47.84* (8.86) | 1.61 (0.03) | 61.82 (6.89) | 24.02 (2.94) |
| Neck SE group (N.=25) | 53.80 (7.74) | 1.5936 (0.06) | 62.88 (10.87) | 24.77 (4.08) |
*Statistically significant difference between groups (independent t-Test) (P<0.05).
All 50 participants attended all of their treatment sessions, and no adverse events were recorded. As a result of the randomisation process, significant differences were observed between groups for age (P=0.02), but not for height, weight or Body Mass Index (P>0.427 for all parameters). Also, no significant differences were observed between groups regarding any of the sociodemographic and physical activity variables analyzed. No differences were observed between groups for neck pain intensity, neck disability, EMG variables, CROM (with the exception for flexion; P<0.02) and COP measurements assessed in the PRE1 and PRE2 sessions (P>0.186 for all parameters).
Neck pain intensity and neck disability
Both exercise interventions induced a significant reduction of neck pain intensity (main effect time: P<0.001, ŋp2=0.770, Table II) and neck disability (main effect time: P<0.001, ŋp2=0.306, Table II) but no differences were observed between groups (main effect group: P=0.534, ŋp2=0.001).
Table II. —Mean±SD of the numeric pain rating scale (NPRS) and the neck disability index (NDI), before (PRE1 and PRE2) and after (POST) “Global Postural Re-education” (GPR) and specific neck exercises (SE) interventions.
| GPR | SE | ||
|---|---|---|---|
| NPRS | PRE1 | 6.16±1.40 | 6.04±1.65 |
| PRE2 | 6.12±1.59 | 6.08±1.55 | |
| POST | 2.56±1.36* | 2.24±1.23 * | |
| NDI | PRE1 | 15.52±5,42 | 16.08±5.34 |
| PRE2 | 13.96±5,01 | 15.36±5.01 | |
| POST | 11.24±5,58* | 11.80±6.09* |
*Statistically significant difference between groups (P<0.05); **P<0.001; PRE1 and PRE2 significantly different from post condition.
The Bonferroni post hoc Test showed that following both interventions neck pain intensity and disability significantly decreased compared to PRE1 and PRE2 moments (P>0.001 for all measurements). On average, patients indicated a reduction in neck pain intensity of 3.6 points and a reduction in disability of 4.2 points following GPR and 3.8 points and 4.3 points, after SE intervention, respectively. All participants reported pain relief, regardless of intervention (ranging between 1 and 7 points).
For those that reported a decrease in disability, 11 from each intervention group reported improvements of 5 points or more on the NDI.
Neck mobility
Analysis of neck ROM showed that neck mobility improved significantly following both interventions (main effect time: P<0.001, 0.385≤ŋp2≤0.623, for all measurements; Table III). The post hoc results are presented in Table III.
Table III. —Mean±SD of the neck flexion, extension, rotation, and inclination mobility, before (PRE1 and PRE2) and after (POST) “Global Postural Re-education” (GPR) and specific neck exercises (SE) interventions.
| GPR | SE | ||
|---|---|---|---|
| Flexion | PRE1 | 58.76±11.87 | 60.12±12.45 |
| PRE2 | 54.36±11.05† | 57.52±12.98† | |
| POST | 64.92±7.83* | 64.92±6.67* | |
| Extension | PRE1 | 46.76±11.99 | 45.48±11.63 |
| PRE2 | 44.76±9.35 | 42.84±11.17 | |
| POST | 54.92±7.93* | 54.44±8.46* | |
| Rotation | PRE1 | 59.62±9.65 | 63.78±8.92 |
| PRE2 | 59.32±9.11 | 63.58±6.40 | |
| POST | 70.90±8.70* | 70.94±5.74* | |
| Lateral Flexion | PRE1 | 31.64±7.38 | 34.70±8.55 |
| PRE2 | 31.32±6.81 | 32.86±5.72 | |
| POST | 39.26±6.47* | 39.10±6.46* |
*P<0.001; PRE1 and PRE2 significantly different from post condition. †P=0.02; PRE1 significantly different from PRE2.
Overall, on average, the GPR group increased their cervical ROM between 7.78º and 11.43° and SE between 3.9º and 7.26° (Table III), but no differences were observed between groups (main effect group: 0.186≤P≤0.635, ŋp2≤0.036, for all CROM measurements). In the GPR group, all participants improved their neck mobility in all measured directions, while in the SE group, 2 of the 25 patients experienced a decrease in extension and lateral flexion (on average – 3.1º).
Neck flexor muscle activity
Figure 4 shows the EMG amplitude of the SCM and AS during the five stages of the CCFT for each group at each time point.
Figure 4.
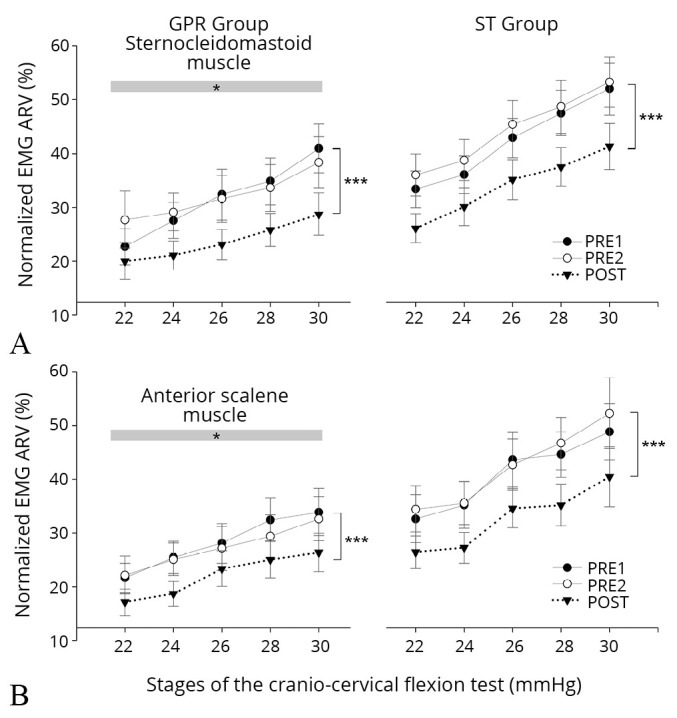
—Mean and SE of the normalised average rectified values (ARV) for the Sternocleidomastoid (A) and anterior scalene (B) muscles for each stage of the cranio-cervical flexion test during the preintervention sessions (PRE1 and PRE2) and postintervention (POST) (“Global Postural Re-education” [GPR] and specific exercise [SE]). *Significant main group effect (P<0.05); ***significant difference between POST and PRE1 and PRE2 sessions (P<0.001).
As expected, a significant main effect of the CCFT stage was observed (P<0.02; ŋp2<0.12, for both muscles). A main effect of time was also observed for the EMG amplitude for the SCM and AS (main effect time: P<0.0001, ŋp2=0.44 and P<0.0001, ŋp2=0.35, respectively; Figure 4); both groups (displayed a similar decrement of the SCM and AS EMG amplitude across all stages of the CCFT after the interventions (P>0.001 when compared Post to PRE1 and PRE2 sessions, for both muscles; Figure 4). Overall, and across all stages of the CCFT, the EMG amplitude of the neck flexors decreased between 3.33% and 17.03% and between 4.38% and 14.97% following GRP and SE programs, respectively. No differences were observed in the EMG amplitude assessed in PRE1 and PRE2 sessions (P>0.823 for both muscles). However, a main group effect was detected (P<0.02; ŋp2<0.12, for both muscles). The SE group presented significantly higher EMG amplitude in both SCM and AS across all stages than the GPR group (Figure 4). Not all participants experienced a reduction in the EMG amplitude of the SCM and AS following treatment (measured as an EMG amplitude average across all 5 test levels). This alteration was observed in 19 participants from the GPR (on average, -13.1%), and 23 from the SE group (on average, - 1.3%). Whereas, six participants of the GPR and two from the SE group experienced an increase in the activity of these muscles during the CCFT (on average +7.4% and+1.3%, respectively) post-treatment.
Postural sway
The results presented in Figure 5 and Table IV indicate that neither of the treatment interventions altered postural sway (main effect time: 0.064<P<0.201, 0.03<ŋp2<0.06; Figure 5, Table IV).
Figure 5.
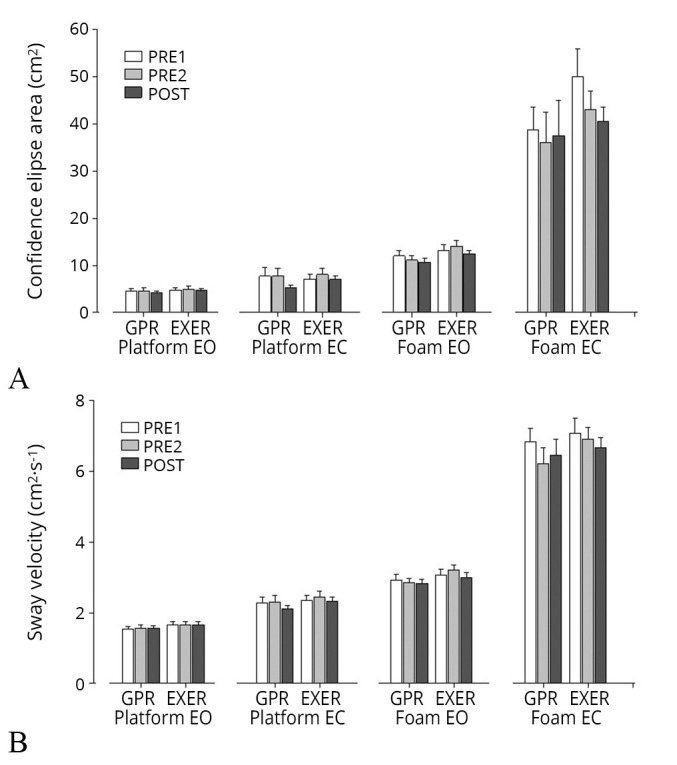
—Mean and SE of the confidence ellipse area (A) and total sway velocity (B) in the conditions with feet side-by-side over the platform and the blue foam with eyes open (EO) and closed (EC) during the pre (PRE1 and PRE2) and post intervention (POST) sessions (“Global Postural Re-education” [GPR] and specific exercise [SE]).
Table IV. —Mean±SD of anteriorposterior velocity (AP velocity) and mediolateral velocity (ML velocity), before (PRE 1 and PRE 2) and after (POST) “Global Postural Re-education” (GPR) and specific - exercises (SE) intervention groups.
| GPR | SE | ||||
|---|---|---|---|---|---|
| AP velocity | ML velocity | AP velocity | ML velocity | ||
| Stable surface, eyes open | PRE1 | 0.88±0.22 | 1.09±0.31 | 0.92±0.27 | 1.17±.029 |
| PRE2 | 0.89±0.30 | 1.09±0.29 | 0.93±0.27 | 1.16±0.31 | |
| POST | 0.90±0.29 | 1.09±0.21 | 0.93±0.26 | 1.18±0.31 | |
| Stable surface, eyes closed | PRE1 | 1.30±0.52 | 1.57±0.61 | 1.35±0.43 | 1.63±0.50 |
| PRE2 | 1.32±0.55 | 1.60±0.64 | 1.40±0.42 | 1.71±0.63 | |
| POST | 1.21±0.28 | 1.48±0.37 | 1.31±0.37 | 1.64±0.45 | |
| Unstable surface, eyes open | PRE1 | 1.76±0.55 | 1.97±0.49 | 1.88±0.60 | 2.02±0.45 |
| PRE2 | 1.72±0.45 | 1.91±0.37 | 1.91±0.53 | 2.15±0.49 | |
| POST | 1.70±0.43 | 1.90±0.36 | 1.82±0.45 | 1.99±0.45 | |
| Unstable surface, eyes closed | PRE1 | 4.40±1.41 | 4.28±1.19 | 4.42±1.35 | 4.60±1.34 |
| PRE2 | 4.14±1.45 | 4.22±1.35 | 4.25±1.02 | 4.55±1.17 | |
| POST | 4.03±4.28 | 6.45±2.29 | 4.28±0.99 | 6.67±1.52 | |
Discussion
This study aimed to investigate the effectiveness of a global versus more localized exercise program in reducing pain and disability and enhancing kinematic, neuromuscular and sensorimotor control features in women with chronic non-specific neck pain. The results showed that both interventions were equally effective in reducing neck pain and disability, improving neck mobility and reducing the activity of the superficial cervical flexor muscles during a test of motor control. On the other hand, neither intervention influenced postural stability. The lack of superiority of one treatment over the other reveals that both options could be considered for the treatment of chronic non-specific neck pain in the short term.
This is the first study to compare the effectiveness of GPR against a SE program that has been previously shown to be effective for the treatment of chronic neck pain.7, 8, 34, 35 In previous studies, the effects of GPR on neck pain were compared to a control group,19 segmental static stretching22, 23 or manual therapy20 interventions. The results of these studies make it challenging to understand the effectiveness of GPR compared to other effective exercise modes. Moreover, this is the first study investigating the effects of GPR on the activity of cervical flexor muscles in patients with chronic neck pain by comparing it to a form of exercise that promotes coordination between the superficial and deep cervical muscles. In the present study, the changes induced by GPR and SE were concurrently investigated in two groups with similar characteristics, which made a direct comparison possible.
Pain, disability and neck mobility
Eight sessions of either GPR or SE over four weeks were sufficient to reduce neck pain (NPRS) and perceived disability (NDI Score) and improve neck mobility. The patients reported, on average, a reduction of 3.6 to 3.8 points on the NPRS after the GPR and SE treatment, respectively, revealing that both interventions were similarly effective in relieving neck pain in patients with mild to moderate chronic non-specific neck pain. In addition, a similar reduction in the NDI was observed after both interventions (~4 points on average). These values are within the same range reported by previous trials studying the effectiveness of SE32, 36, 37 and GPR20, 23 interventions for people with mild to moderate chronic neck pain.
A reduction of 5.5 points in the NDI and 1.5 in the NPRS has previously been determined to be a clinically important difference (MCID) for uncomplicated neck pain.38 Nonetheless, the recommended MCID on the NPRS, and in particular on the NDI, varies substantially. For the NDI, the MCID score ranges between 1.6 points for a patient population with light to moderate recurrent neck pain39 to 7 points for patients with cervical radiculopathy.40 On the other hand, for the NPRS, the MCID scores range between 1.3 points in patients with mixed neck pain5 and 2.5 points for patients non-specific neck pain.41 In the present study, both interventions induced a reduction in the NDI and NPRS scores that fall within these MCID scores. Moreover, the effect size for the NDI and NPRS was high,33 confirming that both SE and GPR are effective in the management of patients with non-specific chronic neck pain.
In our study, the baseline mobility values for all directions (except for flexion) were similar, or even lower in some cases, to those presented by previous studies with subjects with neck pain.29, 37 In flexion, our patients showed similar values to those presented by healthy subjects.29, 37
Following both interventions neck mobility improved in all directions, particularly in flexion, extension and rotation, and the post-intervention values of both groups became closer to the values observed in healthy subjects.29, 37 These results are in line with previous findings on the effectiveness of exercise interventions in improving function in patients with neck pain.8, 34
Different modes of exercise have been shown to be effective, including low-intensity exercise based on precision and control and high-intensity exercise focused on strength and endurance.14 Although the exercise parameters vary between exercise programs, there is no clear evidence that one particular type of exercise is more effective than another in managing patients with chronic neck pain.14, 15 In the present study, the SE program involved localized SEs (based on motor control exercises for the neck muscles), while GPR involved more global exercises (focused on stretching postures and isometric contractions). Despite methodological differences, both exercise programs produced similar improvements in several outcome measures. Our findings are, therefore, in accordance with previous data, confirming a similar impact of different exercise programs in reducing pain and disability in patients with neck pain.34, 42
The mechanisms underlying the effectiveness of different exercise interventions may vary, including a reduction of nociceptor inputs due to modification of tissue loading,14 improvement in the coordination between muscles,36 enhanced physical fitness14, 15 and a reduction of threat due to exposure to the movement.43 The effectiveness of GPR in reducing pain has been associated with mechanisms underlying the prolonged stretching of muscles which is thought to reduce the viscoelasticity of the tissues and increase the range of motion, with a consequent reduction in pain.44 Stretching may also influence the autonomic nervous system and central hemodynamics, leading to decreased parasympathetic activity and alterations in the blood flow in stretched and remote muscles.45 Such alterations may also produce an analgesic effect.
Previous evidence revealed minimal benefit when only stretching exercises were used for the cervical region.15, 46 However, it should be noted that GPR differs from a conventional stretching exercise program since it involves isometric contractions, manual traction and simultaneous stretching of multiple muscles for 15 to 20 minutes, rather than stretching single muscles for short durations. In addition, GPR also incorporates breathing control, which can induce positive effects on the autonomic nervous system.47
Activity of the superficial cervical flexor muscles
GPR and SE induced a similar decline in EMG amplitude of the superficial cervical flexor muscles across all five levels of the cranio-cervical flexion test. Nonetheless, the number of participants experiencing this improvement was slightly greater in the SE group than in the GPR group (23 vs. 19, respectively). Previous studies have confirmed that neck SE is superior to general neck strengthening exercises at reducing the activity of the superficial neck flexor muscles,8, 34, 36 and this change is thought to reflect improved coordination between the deep and superficial neck flexor muscles during this test of motor control.4, 9 The SE program specifically included cranio-cervical flexion exercise, and therefore, it is not surprising that this group improved their performance overall when performing the cranio-cervical flexion test. It should be noted, however, that the GPR group gained a significant improvement in test performance (noted as a reduction in superficial muscle activity) even though the movement of cranio-cervical flexion was not specifically targeted. This finding supports the effect of GPR on neck muscle coordination.
Postural stability
A number of studies have shown that patients with chronic neck pain may present with poor balance compared to asymptomatic people, reflected as a larger displacement of COP during balance tasks either with the eyes open or closed.48 Nevertheless, very few studies have investigated the effects of different interventions on balance performance in people with neck pain. Previous research has suggested that endurance training of the neck muscles49 and manual therapy50 can improve postural stability in patients with whiplash associated disorders. On the other hand, no changes in static balance were observed following a neck-SE program, a behavioral approach or general physical activity.11 No previous study has evaluated the effect of GPR on balance. Since GPR is a more global exercise approach, we anticipated that it would improve postural stability. Yet, the results of the present study indicate that neither intervention affected postural stability. Although the interventions were not specifically designed to improve balance, they both aimed to enhance neuromuscular and sensorimotor control, which could potentially enhance postural stability. Importantly, however, it should be noted that the data from the present study do not allow us to confirm that our participants had impaired balance since a healthy control group was not recruited. Moreover, there is no normative data or cut-off points on COP measures regarding normal or impaired balance, and the measurement parameters vary substantially between the few studies on the topic, limiting the comparison with previous studies.
Limitations of the study
The main limitation of this study was the lack of an asymptomatic control group which would have allowed us to understand if the baseline measures were different to healthy individuals, e.g. balance may not have changed as their balance was normal in the first place. In addition, the participants presented with mild to moderate pain and disability, which limits the results of this study to patients that fall into this category. A further consideration is that the outcome measures were limited to only some aspects of neuromuscular and sensorimotor control, and although the two exercise interventions revealed comparable effects, they may influence other aspects of neuromuscular and sensorimotor control differently. Additionally, the follow-up was limited to immediately after the interventions, and further research is required to determine the impact of these exercise programs in the longer term.
Conclusions
GPR, which focuses on stretching positions and isometric contractions, was equally effective as a specific localized neck exercise program in reducing neck pain and disability and improving neck mobility and neuromuscular coordination in the short term.
Supplementary Digital Material 1
Supplementary Table I
Exercises.
References
- 1.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204–22. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33069326&dopt=Abstract 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skillgate E, Magnusson C, Lundberg M, Hallqvist J. The age- and sex-specific occurrence of bothersome neck pain in the general population—results from the Stockholm public health cohort. BMC Musculoskelet Disord 2012;13:185. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23006655&dopt=Abstract 10.1186/1471-2474-13-185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ 2017;358:j3221. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28807894&dopt=Abstract 10.1136/bmj.j3221 [DOI] [PubMed] [Google Scholar]
- 4.Jull G, Falla D, Treleaven J, O’Leary S, Lewis J. Management of Neck Pain Disorders. Philadelphia, PA: Elsevier; 2018. [Google Scholar]
- 5.Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, et al. American Physical Therapy Association . Neck pain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the american physical therapy association. J Orthop Sports Phys Ther 2008;38:A1–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18758050&dopt=Abstract 10.2519/jospt.2008.0303 [DOI] [PubMed] [Google Scholar]
- 6.Alsultan F, Cescon C, De Nunzio AM, Barbero M, Heneghan NR, Rushton A, et al. Variability of the helical axis during active cervical movements in people with chronic neck pain. Clin Biomech (Bristol, Avon) 2019;62:50–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30690409&dopt=Abstract 10.1016/j.clinbiomech.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 7.Falla D, Lindstrøm R, Rechter L, Boudreau S, Petzke F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: a randomized controlled study. Eur J Pain 2013;17:1517–28. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23649799&dopt=Abstract 10.1002/j.1532-2149.2013.00321.x [DOI] [PubMed] [Google Scholar]
- 8.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther 2007;87:408–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17341512&dopt=Abstract 10.2522/ptj.20060009 [DOI] [PubMed] [Google Scholar]
- 9.Jull G, Falla D. Does increased superficial neck flexor activity in the craniocervical flexion test reflect reduced deep flexor activity in people with neck pain? Man Ther 2016;25:43–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27422596&dopt=Abstract 10.1016/j.math.2016.05.336 [DOI] [PubMed] [Google Scholar]
- 10.Boudreau SA, Falla D. Chronic neck pain alters muscle activation patterns to sudden movements. Exp Brain Res 2014;232:2011–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24632836&dopt=Abstract 10.1007/s00221-014-3891-3 [DOI] [PubMed] [Google Scholar]
- 11.Treleaven J, Peterson G, Ludvigsson ML, Kammerlind AS, Peolsson A. Balance, dizziness and proprioception in patients with chronic whiplash associated disorders complaining of dizziness: A prospective randomized study comparing three exercise programs. Man Ther 2016;22:122–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26678652&dopt=Abstract 10.1016/j.math.2015.10.017 [DOI] [PubMed] [Google Scholar]
- 12.Field S, Treleaven J, Jull G. Standing balance: a comparison between idiopathic and whiplash-induced neck pain. Man Ther 2008;13:183–91. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17306599&dopt=Abstract 10.1016/j.math.2006.12.005 [DOI] [PubMed] [Google Scholar]
- 13.Kendall JC, Boyle E, Hartvigsen J, Hvid LG, Azari MF, Skjødt M, et al. Neck pain, concerns of falling and physical performance in community-dwelling Danish citizens over 75 years of age: A cross-sectional study. Scand J Public Health 2016;44:695–701. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27587563&dopt=Abstract 10.1177/1403494816666414 [DOI] [PubMed] [Google Scholar]
- 14.Falla D, Hodges PW. Individualized exercise interventions for spinal pain. Exerc Sport Sci Rev 2017;45:105–15. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28092298&dopt=Abstract 10.1249/JES.0000000000000103 [DOI] [PubMed] [Google Scholar]
- 15.Gross AR, Paquin JP, Dupont G, Blanchette S, Lalonde P, Cristie T, et al. Cervical Overview Group . Exercises for mechanical neck disorders: A Cochrane review update. Man Ther 2016;24:25–45. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27317503&dopt=Abstract 10.1016/j.math.2016.04.005 [DOI] [PubMed] [Google Scholar]
- 16.Hidalgo-Peréz A, Fernández-García Á, López-de-Uralde-Villanueva I, Gil-Martínez A, Paris-Alemany A, Fernández-Carnero J, et al. Effectiveness of a Motor Control Therapeutic Exercise Program Combined With Motor Imagery on the Sensorimotor Function of the Cervical Spine: a Randomized Controlled Trial. Int J Sports Phys Ther 2015;10:877–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26618067&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 17.Lomas-Vega R, Garrido-Jaut MV, Rus A, Del-Pino-Casado R. Effectiveness of Global Postural Re-education for Treatment of Spinal Disorders: A Meta-analysis. Am J Phys Med Rehabil 2017;96:124–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27386815&dopt=Abstract 10.1097/PHM.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 18.Souchard P. Rééducation posturale globale: RPG - La méthode. Philadelphia, PA: Elsevier-Masson, 2011. [Google Scholar]
- 19.Cavalcanti IF, Antonino GB, Monte-Silva KK, Guerino MR, Ferreira AP, das Graças Rodrigues de Araújo M. Global Postural Re-education in non-specific neck and low back pain treatment: A pilot study. J Back Musculoskeletal Rehabil 2020;33:823–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31929138&dopt=Abstract 10.3233/BMR-181371 [DOI] [PubMed] [Google Scholar]
- 20.Pillastrini P, Banchelli F, Guccione A, Di Ciaccio E, Violante FS, Brugnettini M, et al. Global Postural Reeducation in patients with chronic nonspecific neck pain: cross-over analysis of a randomized controlled trial. Med Lav 2018;109:16–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29405174&dopt=Abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oliveri M, Caltagirone C, Loriga R, Pompa MN, Versace V, Souchard P. Fast increase of motor cortical inhibition following postural changes in healthy subjects. Neurosci Lett 2012;530:7–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23022506&dopt=Abstract 10.1016/j.neulet.2012.09.031 [DOI] [PubMed] [Google Scholar]
- 22.Cunha AC, Burke TN, França FJ, Marques AP. Effect of global posture reeducation and of static stretching on pain, range of motion, and quality of life in women with chronic neck pain: a randomized clinical trial. Clinics (São Paulo) 2008;63:763–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19060998&dopt=Abstract 10.1590/S1807-59322008000600010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amorim CS, Gracitelli ME, Marques AP, Alves VL, Alves VL. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: a preliminary clinical trial. J Manipulative Physiol Ther 2014;37:441–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25092553&dopt=Abstract 10.1016/j.jmpt.2013.08.011 [DOI] [PubMed] [Google Scholar]
- 24.Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23303884&dopt=Abstract 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20332511&dopt=Abstract 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mendes-Fernandes T, Puente-González AS, Márquez-Vera MA, Vila-Chã C, Méndez-Sánchez R. Effects of Global Postural Reeducation versus Specific Therapeutic Neck Exercises on Pain, Disability, Postural Control, and Neuromuscular Efficiency in Women with Chronic Nonspecific Neck Pain: Study Protocol for a Randomized, Parallel, Clinical Trial. Int J Environ Res Public Health 2021;18:10704. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34682453&dopt=Abstract 10.3390/ijerph182010704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S240–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22588748&dopt=Abstract 10.1002/acr.20543 [DOI] [PubMed] [Google Scholar]
- 28.Pereira M. Contribuição para a adaptação cultural do Neck Disability Index e caraterização da prática de fisioterapia em pacientes com Dor Crónica Cervical. Universidade Nova de Lisboa; 2011. [Google Scholar]
- 29.Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther 2008;38:640–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18827326&dopt=Abstract 10.2519/jospt.2008.2680 [DOI] [PubMed] [Google Scholar]
- 30.Wolan-Nieroda A, Guzik A, Mocur P, Drużbicki M, Maciejczak A. Assessment of Interrater and Intrarater Reliability of Cervical Range of Motion (CROM) Goniometer. BioMed Res Int 2020;2020:8908035. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32626769&dopt=Abstract 10.1155/2020/8908035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Falla D, Dall’Alba P, Rainoldi A, Merletti R, Jull G. Repeatability of surface EMG variables in the sternocleidomastoid and anterior scalene muscles. Eur J Appl Physiol 2002;87:542–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12355194&dopt=Abstract 10.1007/s00421-002-0661-x [DOI] [PubMed] [Google Scholar]
- 32.Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine 2004;29:2108–14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15454700&dopt=Abstract 10.1097/01.brs.0000141170.89317.0e [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Mahwah, NJ: Lawrence Erlbaum Assoc; 1988. [Google Scholar]
- 34.Falla D, Jull G, Hodges P, Vicenzino B. An endurance-strength training regime is effective in reducing myoelectric manifestations of cervical flexor muscle fatigue in females with chronic neck pain. Clin Neurophysiol 2006;117:828–37. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16490395&dopt=Abstract 10.1016/j.clinph.2005.12.025 [DOI] [PubMed] [Google Scholar]
- 35.O’Leary S, Falla D, Hodges PW, Jull G, Vicenzino B. Specific therapeutic exercise of the neck induces immediate local hypoalgesia. J Pain 2007;8:832–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17644487&dopt=Abstract 10.1016/j.jpain.2007.05.014 [DOI] [PubMed] [Google Scholar]
- 36.Jull GA, Falla D, Vicenzino B, Hodges PW. The effect of therapeutic exercise on activation of the deep cervical flexor muscles in people with chronic neck pain. Man Ther 2009;14:696–701. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19632880&dopt=Abstract 10.1016/j.math.2009.05.004 [DOI] [PubMed] [Google Scholar]
- 37.Law EY, Chiu TT. Measurement of cervical range of motion (CROM) by electronic CROM goniometer: a test of reliability and validity. J Back Musculoskeletal Rehabil 2013;26:141–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23640315&dopt=Abstract 10.3233/BMR-2012-00358 [DOI] [PubMed] [Google Scholar]
- 38.Young I, Dunning J, Butts R, Mourad F, Cleland J. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother Theory Pract 2018;00:1–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29856244&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 39.Vos CJ, Verhagen AP, Koes BW. Reliability and responsiveness of the Dutch version of the Neck Disability Index in patients with acute neck pain in general practice. Eur Spine J 2006;15:1729–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16670840&dopt=Abstract 10.1007/s00586-006-0119-7 [DOI] [PubMed] [Google Scholar]
- 40.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine 2006;31:598–602. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16508559&dopt=Abstract 10.1097/01.brs.0000201241.90914.22 [DOI] [PubMed] [Google Scholar]
- 41.Pool JJ, Ostelo RW, Hoving JL, Bouter LM, de Vet HC. Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine 2007;32:3047–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18091500&dopt=Abstract 10.1097/BRS.0b013e31815cf75b [DOI] [PubMed] [Google Scholar]
- 42.Häkkinen A, Kautiainen H, Hannonen P, Ylinen J. Strength training and stretching versus stretching only in the treatment of patients with chronic neck pain: a randomized one-year follow-up study. Clin Rehabil 2008;22:592–600. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18586810&dopt=Abstract 10.1177/0269215507087486 [DOI] [PubMed] [Google Scholar]
- 43.Jull G, Kenardy J, Hendrikz J, Cohen M, Sterling M. Management of acute whiplash: a randomized controlled trial of multidisciplinary stratified treatments. Pain 2013;154:1798–806. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23726933&dopt=Abstract 10.1016/j.pain.2013.05.041 [DOI] [PubMed] [Google Scholar]
- 44.Shrier I, Gossal K. Myths and truths of stretching: individualized recommendations for healthy muscles. Phys Sportsmed 2000;28:57–63. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20086656&dopt=Abstract 10.3810/psm.2000.08.1159 [DOI] [PubMed] [Google Scholar]
- 45.Venturelli M, Rampichini S, Coratella G, Limonta E, Bisconti AV, Cè E, et al. Heart and musculoskeletal hemodynamic responses to repetitive bouts of quadriceps static stretching. J Appl Physiol 2019;127:376–84. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31161884&dopt=Abstract 10.1152/japplphysiol.00823.2018 [DOI] [PubMed] [Google Scholar]
- 46.Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best Evidence Rehabilitation for Chronic Pain Part 5: osteoarthritis. J Clin Med 2019;8:1769. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31652929&dopt=Abstract 10.3390/jcm8111769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing—an experimental study. Pain Med 2012;13:215–28. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21939499&dopt=Abstract 10.1111/j.1526-4637.2011.01243.x [DOI] [PubMed] [Google Scholar]
- 48.Ruhe A, Fejer R, Walker B. Altered postural sway in patients suffering from non-specific neck pain and whiplash associated disorder - A systematic review of the literature. Chiropr Man Therap 2011;19:13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21609469&dopt=Abstract 10.1186/2045-709X-19-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stapley PJ, Beretta MV, Dalla Toffola E, Schieppati M. Neck muscle fatigue and postural control in patients with whiplash injury. Clin Neurophysiol 2006;117:610–22. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16427356&dopt=Abstract 10.1016/j.clinph.2005.11.007 [DOI] [PubMed] [Google Scholar]
- 50.Romero del Rey R, Saavedra Hernández M, Rodríguez Blanco C, Palomeque del Cerro L, Alarcón Rodríguez R. Short-term effects of spinal thrust joint manipulation on postural sway in patients with chronic mechanical neck pain: a randomized controlled trial. Disabil Rehabil 2020;0:1–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32730089&dopt=Abstract [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Exercises.