HIGHLIGHTS
-
•
What is known: returning to work after stroke is a key milestone in recovery; however, many patients are unable to achieve this. Research has shown that predictors vary across countries.
-
•
What is new: in addition to identifying predictive factors, this study identified how these factors could be used for screening for referral to return to work services at the time of inpatient rehabilitation discharge.
KEYWORDS: Rehabilitation, Return to work, Stroke
Abstract
Objective
To determine the proportion of patients who return to work after inpatient stroke rehabilitation and to identify demographic, clinical, and functional predictive factors for its success.
Design
A retrospective follow-up study of patients with stroke who were premorbidly working and had completed inpatient rehabilitation in a large metropolitan hospital between January 2016 and December 2017. They underwent a telephone interview at 2 years post discharge.
Setting
Inpatient rehabilitation and follow-up post discharge.
Participants
A total of 314 patients with stroke (73.9% male) with mean age of 58.9 at time of stroke (N=314).
Results
A total of 46% of 314 participants returned to work. In multivariable logistic regression analysis, viewing return to work as important (odds ratio [OR], 11.90; 95% confidence interval [CI], 5.15-27.52), absence of language impairment (OR, 9.39; 95% CI, 3.01-29.34), ambulation FIM≥5 (supervision to independence level) on discharge (OR, 4.93; 95% CI, 2.44-9.98), cognitive FIM on discharge ≥25 (OR, 2.77; 95% CI, 1.19-6.47), employment in premorbid office work (OR, 2.67; 95% CI, 1.26-5.64), and a lower Charlson Comorbidity Index (CCI) score at discharge (OR, 0.83; 95% CI, 0.68-1.00) were associated with successful return to work.
Conclusions
Viewing return to work as important, absence of language impairments on discharge, discharge ambulation FIM≥5, discharge cognitive FIM≥25, employment in premorbid office work, and a lower discharge CCI score were positive predictors of successful return to work.
Stroke has a devastating effect on mortality and morbidity. The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 reported 12.2 million incident strokes and 101 million prevalent strokes.1 Its morbidity spans impairments across a spectrum of functions including consciousness, cognition, and motor and sensory aspects.2 These impairments can hinder meaningful participation in personal, societal, and economic roles including returning to work.
Approximately half of all survivors of stroke have residual physical or cognitive impairments,3 which affect their participation in society and life roles. Returning to work post stroke is a key milestone for many survivors of stroke; however, many cannot achieve this goal. Significant economic costs are incurred because of stroke,4 which do not include further economic costs incurred from the downstream consequences of stroke morbidity, such as caregiver burden and hidden costs from lost earnings.
Research has shown that various predictors are positively or negatively associated with returning to work. These include age, sex, socioeconomic class, stroke types, types of impairments, length of hospitalization stay, nature of employment, and the presence of social support.5, 6, 7, 8 Financial reasons have been quoted as reasons for returning to work in previous studies.9,10
Stroke is the fourth leading cause of death in Singapore11 and one of the top causes of hospitalization. According to previous study, poststroke employment in Singapore is 45.9%,12 which remains a challenge.13 In the Singaporean context, previous studies have suggested that factors such as being the sole income earner, having positive social support, and having no caregiver were positively associated with return to work. However, these studies consisted of relatively small sample sizes with different study methodologies and results ranging from 39%-55% of the study population returning to work after a stroke.13 Furthermore, they were evaluated in the context of preexisting hospital-based early supported discharge programs.14 Early supported discharge programs involved patients who were discharged directly from the acute hospital to a home-based rehabilitation conducted by the physiotherapist and occupational therapist. It was not universally available and the frequency and intensity varies; therefore, it may only represent a small proportion of the population with stroke who needed rehabilitation.
This study aimed to determine the proportion of return to work among survivors of stroke who completed an inpatient rehabilitation program in Singapore. Previous studies have identified various factors associated with returning to work; however, the results vary among different populations.5,10 This study explored whether these factors were relevant in our local context by reviewing the clinical, functional, and demographic predictive factors that determine the return to work.
Methods
Study design
This retrospective follow-up study was conducted between September 2018 and September 2021.
Participants
The participants were patients who completed a stroke rehabilitation program within an acute inpatient rehabilitation unit in Singapore between January 2016 and December 2017. Our acute inpatient rehabilitation unit is situated within a 1000-bedded regional acute care hospital. Our inpatient rehabilitation unit consisted of 60 beds across 3 wards. There are approximately 450 stroke rehabilitation admissions annually. Most patients are transferred directly from the acute stroke unit as early as 2-3 days post stroke. Patients with stroke underwent neurorehabilitation in a 5 days per week program over an average of 16 days. Most patients with stroke who require rehabilitation are transferred to the unit. Patients older than 80 years are transferred to geriatric care from the acute stroke unit unless they are premorbidly independent for activities of daily living. Patients who are medically unstable may be transferred later if they become medically or neurologically stable.
Medical records of patients with a discharge diagnosis of a first-ever stroke were reviewed. Invitation letters were posted to patients who were premorbidly working prior to a telephone interview at 2 years post stroke. Verbal consent was obtained prior to phone interviews. If a survivor of stroke was unable to answer the questions, the response was obtained from the next of kin who consented to participate in the study.
Data collected
Collected data included demographic and clinical information. Demographic data obtained included age (at stroke admission), sex, and ethnicity. Clinical data included stroke type, as well as admission and discharge National Institutes of Health Stroke Scale (NIHSS), FIM, and Charlson Comorbidity Index (CCI) at the time of hospital discharge. Further clinical information was obtained up to 2 years post stroke, including complications such as depression, pain, spasticity, or seizures noted during inpatient or outpatient follow-up clinic visits.
NIHSS score was defined as the sum of 15 individually evaluated elements and ranged from 0-42. Stroke severity may be categorized as follows: no stroke symptoms, 0; minor stroke, 1-4; moderate stroke, 5-15; moderate to severe stroke, 16-20 and severe stroke, 21-42.15 Cognitive FIM refers to the 5 items of the FIM pertaining to cognition, including comprehension, expression, social interaction, problem solving, and memory. Cutoffs of 5 (supervision level) for ambulation and 25 (summation of 5 items for cognition, each at supervision level) were chosen.
Telephone interviews were conducted by the study team members who consists of resident physicians, medical officers and the rehabilitation coordinator trained by the principal investigator using a standardized script to obtain information pertaining to the demographics of the individual at the time of stroke (marital status, living arrangements, presence of family support, educational level, monthly household income), nature of work prior to stroke, time taken to return to work after stroke, nature of work after stroke, and engagement in vocational rehabilitation programs.
Outcome measures
The primary outcome measure was the proportion of return to work, defined as being employed in a paid job, either in a previous or new job, and full-time or part-time work. Part-time work involved working fewer hours than that required in full-time employment, which is typically at least 40 hours of work per week. Predictors favoring successful return to work were identified.
Statistical analysis
Descriptive statistics of demographic, clinical, and functional characteristics were reported as numbers and percentages for categorical data, means ± SDs for normally distributed data, and medians and interquartile ranges for data that were not normally distributed. Candidate variables were selected a priori based on the literature and expert opinions. Simple logistic regression was used to explore the variables hypothesized to be associated with return to work. For variables with multiple categories, the Wald test jointly assesses whether the regression coefficient of each variable is equal to 0.
We then determined the factors that were independently associated with returning to work. To avoid problems associated with stepwise regression, candidate predictors were selected a priori based on the literature5,6,16 and expert opinions. All the selected candidate predictors were included in the multivariable model. Model 1 included age and hypothesized clinical and functional predictors (CCI score, stroke type and area, language impairment, cognitive impairment, walking FIM at discharge, cognitive FIM at discharge). Model 2 included all covariates in model 1 and hypothesized demographic predictors (premorbid employment type, nature of employment, personal attitude toward returning to work). Multivariable logistic regression was used to assess the factors independently associated with return to work.
To assess potential effect modification on the multiplicative scale, we included interaction terms for (1) NIHSS score at admission and walking FIM score at discharge and (2) NIHSS score at admission and cognitive FIM score at discharge in model 2. All potential interactions were selected a priori based on expert opinions. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were reported. Statistical tests were 2-sided with a significance level of 0.05. All statistical analyses were conducted using Stata 15.0.a
This study was reviewed and approved by the central institutional review board for ethics clearance and verbal consent and was conducted in compliance with all applicable institutional policies, regulations, guidelines, and study protocols. This study conforms to all Strengthening the Reporting of Observational Studies in Epidemiology guidelines and reports the required information accordingly (Supplemental Table S1).
Results
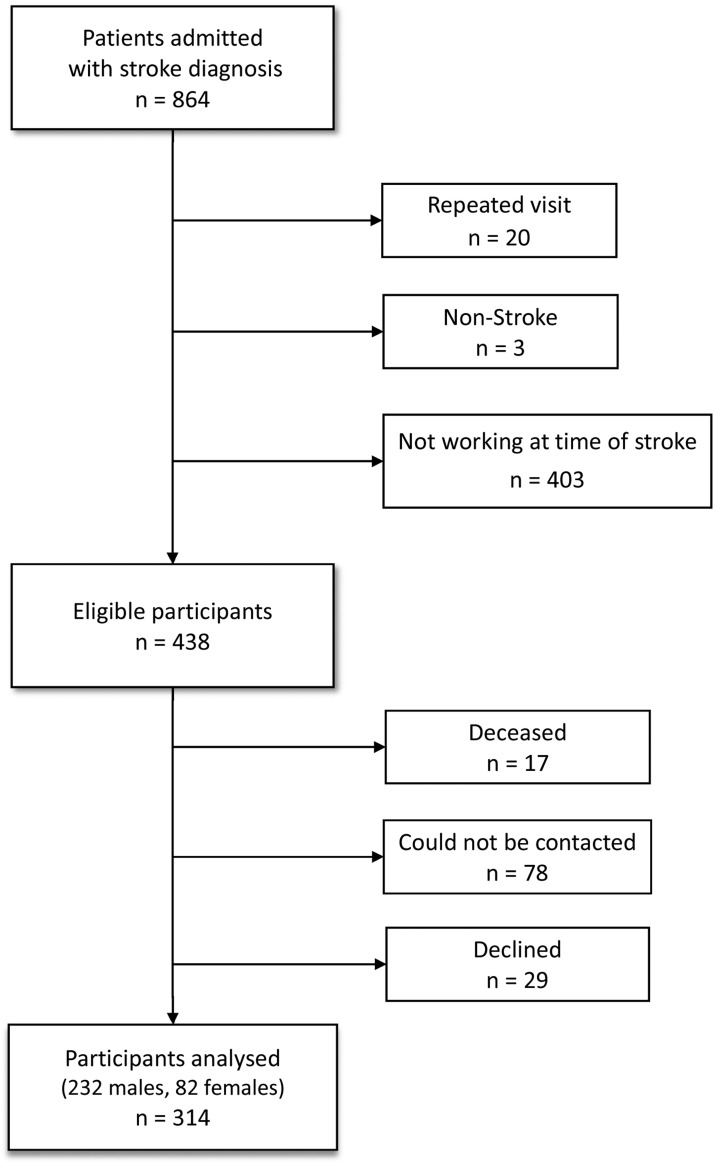
Of the 864 medical records with a discharge diagnosis of stroke, 20 were repeated admissions, 3 were determined to be non–stroke-related, and 403 patients were not working at the time of stroke. Of the remaining 438 eligible patients, 17 died, 78 could not be contacted, and 29 declined to participate (fig 1). Data from 314 participants were analyzed.
Fig. 1.
Flowchart of study population.
Demographic, clinical, and functional characteristics of participants
These characteristics are presented in tables 1 and 2, respectively. Of 314 participants, 145 (46.2%) returned to work. Our patients were in the minor, moderate, and moderately severe stroke groups. The median rehabilitation length of stay in our unit was 16 days.
Table 1.
Demographic, clinical, and functional characteristics of 314 participants
| Characteristic* | Total (N=314) | Did RTW (n=145) | Did Not RTW (n=169) |
|---|---|---|---|
| Age at admission (y), mean ± SD Min-max |
58.9±10.1 29-86 |
56.4±10.6 29-85 |
61.0±9.1 41-86 |
| Age group at admission (y), n (%) >65 51-65 ≤50 |
75 (23.9) 186 (59.2) 53 (16.9) |
24 (16.5) 88 (60.7) 33 (22.8) |
51 (30.2) 98 (58.0) 20 (11.8) |
| Male sex, n (%) | 232 (73.9) | 111 (76.5) | 121 (71.6) |
| Ethnicity, n (%) Indian/others Chinese Malay |
23 (7.3) 223 (71.0) 68 (21.7) |
10 (6.9) 103 (71.0) 32 (22.1) |
13 (7.7) 120 (71.0) 36 (21.3) |
| Education level, n (%) None/primary Secondary Diploma/degree and above |
104 (33.8) 141 (45.8) 63 (20.4) |
42 (29.4) 65 (45.4) 36 (25.2) |
62 (37.6) 76 (46.0) 27 (16.4) |
| Premorbid total monthly household income (SGD$), n (%) <3000 ≥3000 Marital status at admission, n (%) Single/divorced/separated Married |
203 (70.2) 86 (29.8) 75 (23.9) 239 (76.1) |
119 (78.3) 33 (21.7) 112 (77.2) 33 (22.8) |
84 (61.3) 53 (38.7) 127 (75.2) 42 (24.9) |
| Premorbid living arrangement, n (%) Stays alone/in dormitory Stays with family/helper |
57 (18.1) 257 (81.9) |
22 (15.2) 123 (84.8) |
35 (20.7) 134 (79.3) |
| Premorbid employment type, n (%) Nonoffice worker Office worker |
199 (65.0) 107 (35.0) |
83 (57.2) 62 (42.8) |
116 (72.0) 45 (28.0) |
| Premorbid employment nature, n (%) Part time Full time |
34 (11.1) 272 (88.9) |
10 (6.9) 134 (93.1) |
24 (14.8) 138 (85.2) |
| Rehabilitation LOS Median (IQR) Min-max >16 d ≤16 d |
16 (9-24) 1-83 153 (48.9) 160 (51.1) |
12 (7-20) 2-52 48 (33.1) 97 (66.9) |
19 (13-28.5) 1-83 105 (62.5) 63 (37.5) |
| Attitude toward RTW, n (%)† Not important/neutral Quite/very important |
101 (33.2) 204 (66.8) |
17 (11.7) 128 (88.3) |
84 (52.5) 76 (47.5) |
Abbreviations: IQR, interquartile range; LOS, length of stay; RTW, return to work; SGD, Singapore dollar.
n=308, 289, 306, 306, 313, and 305 patients with available education level, total monthly household income, premorbid employment type, premorbid employment nature, rehabilitation length of stay, and personal attitude toward RTW data.
At phone interview (2-y time point).
Table 2.
Clinical and functional characteristics of 314 participants
| Characteristic* | Total (N=314) | Did RTW (n=145) | Did Not RTW (n=169) |
|---|---|---|---|
| Type of stroke, n (%) Ischemic Hemorrhagic |
220 (70.1) 94 (29.9) |
101 (69.7) 44 (30.3) |
119 (70.4) 50 (29.6) |
| Area of ischemic stroke, n (%) PACI/TACI LACI POCI |
61 (29.5) 100 (48.3) 46 (22.2) |
18 (19.0) 55 (57.9) 22 (23.1) |
43 (38.4) 45 (40.2) 24 (21.4) |
| NIHSS score (admission), n (%) 16-29 5-15 1-4 0 |
25 (10.4) 132 (55.0) 78 (32.5) 5 (2.1) |
8 (6.7) 63 (52.5) 45 (37.5) 4 (3.3) |
17 (14.2) 69 (57.5) 33 (27.5) 1 (0.8) |
| CCI score at discharge, median (IQR) ≥5 <5 |
4 (3-6) 137 (43.9) 175 (56.1) |
4 (3-5) 47 (34.3) 98 (67.6) |
5 (3-6) 90 (53.9) 77 (46.1) |
| Poststroke motor impairment, n (%)† Yes No Poststroke language impairment, n (%)† Yes No Poststroke cognitive impairment, n (%)† Yes No Poststroke seizure, n (%)† Yes No Poststroke depression, n (%)† Yes No Poststroke spasticity, n (%)† Yes No FIM: walking (discharge) Mean ± SD Need assistance (14), n (%) Supervision to independence (5-7), n (%) |
212 (67.5) 102 (32.5) 61 (19.5) 251 (80.5) 96 (30.6) 218 (69.4) 15 (4.8) 299 (95.2) 30 (9.5) 284 (90.5) 51 (16.2) 263 (83.8) 4.1 ± 2.0 143 (48.6) 151 (51.4) |
76 (52.4) 69 (47.6) 8 (5.6) 136 (94.4) 27 (18.6) 118 (81.4) 2 (1.4) 143. (98.6) 5 (3.4) 140 (96.6) 6 (4.1) 139 (95.9) 4.9 ± 1.7 39 (29.3) 94 (70.7) |
136 (80.5) 33 (19.5) 53 (31.5) 115 (68.5) 69 (40.8) 100 (59.2) 13 (7.7) 156 (92.3) 25 (14.8) 144 (85.2) 45 (26.6) 124 (73.4) 3.5 ± 2.0 104 (64.6) 57 (35.4) |
| FIM: cognitive total (discharge), n (%) <25 ≥25 |
93 (31.9) 199 (68.2) |
18 (13.6) 114 (86.4) |
75 (46.9) 85 (53.1) |
| Communication difficulties, n (%)† Yes No |
147 (47.7) 161 (52.3) |
36 (25.3) 106 (74.7) |
111 (66.9) 55 (33.1) |
Abbreviations: IQR, interquartile range; LACI, lacunar infarct; PACI, partial anterior circulation infarct; POCI, posterior circulation infarct; RTW, return to work; TACI, total anterior circulation infarct.
n=312, 207, 240, 302, 302, 294, and 308 patients with available CCI, area of ischemic stroke, NIHSS (admission), language impairment, FIM: walking (discharge), FIM: cognitive total (discharge), and communication difficulties 2 years post discharge.
At phone interview (2-y time point).
Factors related to age, type of work, and personal attitude
In unadjusted logistic regression analyses, with yearly increases in age, the odds of returning to work decreased by 5%. Office workers (OR, 1.93; 95% CI 1.20-3.10) and full-time workers (OR, 2.33; 95% CI, 1.07-5.06) were more likely to return to work than nonoffice and part-time workers. Regarding attitudes and perceptions, survivors who viewed returning to work as important were more likely to be successful (OR, 8.32; 95% CI, 4.60-15.1) than those who did not. The time taken for survivors to return to work ranged from 1-24 months, with a median of 3 months (interquartile range 2-9.5). The majority of those who returned to work did so for financial reasons (73.8%), whereas a smaller number quoted personal satisfaction (40.7%), that the company needed them (11.0%), or contribution to society (2.8%) as reasons for returning to work. A total of 26 patients from the entire cohort studied engaged agencies that facilitated return to work, of whom 14 (53.8%) were successful. These agencies include SG-Enable17 and Society for the Physically Disabled,18 which offer services such as vocational rehabilitation and assistive technology to enhance employability and employment options, including job matching and job coaching.
Factors related to clinical and functional status
In the unadjusted analyses, for every increase of 1 unit in the CCI, the odds of success were reduced by 24% (95% CI, 0.68-0.86). Participants with lacunar infarcts were also more likely to return to work than those with cortical strokes (OR, 2.92; 95% CI, 1.48-5.74).
Those who recovered well neurologically with no language impairment (OR, 7.83; 95% CI, 3.58-17.2) were more likely to return to work than patients who had language impairments.
Simple logistic regression showed that ambulation FIM (mobility at supervision to independence level) on discharge (OR, 4.40; 95% CI, 2.68-7.20) and cognitive FIM on discharge ≥25 (OR, 5.59; 95% CI, 3.11-10.04) were associated with successful return to work compared with patients who required assistance in mobility and had a cognitive FIM<25, respectively.
Independent predictors of return to work
Multivariable logistic model 1 showed that the odds of successful return to work decreased by 5% for every yearly increase in age. Having a lacunar stroke (OR, 2.39; 95% CI, 1.03-5.57), absence of language impairment (OR, 6.57; 95% CI, 2.36-18.28), ambulation FIM≥5 on discharge (OR, 4.18; CI, 2.28-7.64), and cognitive FIM≥25 (OR, 2.56; 95% CI, 1.21-5.39) on discharge predicted successful return to work (table 3). In multivariable model 2, CCI score at discharge (OR, 0.83; 95% CI, 0.68-1.00), absence of language impairment (OR, 9.39; 95% CI, 3.01-29.34), ambulation FIM≥5 at discharge (OR, 4.93; 95% CI, 2.44-9.98), cognitive FIM≥25 at discharge (OR, 2.77; 95% CI, 1.19-6.47), holding a premorbid office job (OR, 2.67; 95% CI, 1.26-5.64), and viewing return to work as important (OR, 11.90; 95% CI, 5.15-27.52) were significant predictors (see table 3).
Table 3.
Multivariable logistic regression of factors associated with return to work
| Variable | Univariable Analyses |
Multivariable Model 1 |
Multivariable Model 2 |
|||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | |
| Age at admission (y) | 0.95 (0.93–0.98) | <.001 | 0.95 (0.91–0.98) | .002 | 0.99 (0.95–1.03) | .691 |
| Male sex | 1.30 (0.78–2.16) | .320 | 1.24 (0.64–2.41) | .526 | 1.22 (0.56–2.63) | .618 |
| CCI at discharge Type and area of stroke Ischemic, PACI/TACI Ischemic, LACI Ischemic, POCI Hemorrhagic Post-stroke language impairment* Yes No FIM: walking (discharge) Need assistance (1-4) Supervision to independence (5-7) FIM: cognitive total (discharge) <25 ≥25 |
0.76 (0.68–0.86) 1.00 (ref.) 2.92 (1.48–5.74) 2.19 (0.99–4.87) 2.10 (1.06–3.16) 1.00 (ref.) 7.83 (3.58–17.2) 1.00 (ref.) 4.40 (2.68–7.20) 1.00 (ref.) 5.59 (3.11–10.04) |
<.001 .021 - .002 .054 .033 - <.001 - <.001 - <.001 |
0.88 (0.74–1.05) 1.00 (ref.) 2.39 (1.03–5.57) 1.76 (0.66–4.71) 2.30 (0.96–5.51) 1.00 (ref.) 6.57 (2.36–18.28) 1.00 (ref.) 4.18 (2.28–7.64) 1.00 (ref.) 2.56 (1.21–5.39) |
.150 .151 - .043 .260 .062 - <.001 - <.001 - .014 |
0.83 (0.68–1.00) 1.00 (ref.) 1.99 (0.77–5.19) 1.68 (0.52–5.45) 2.03 (0.74–5.61) 1.00 (ref.) 9.39 (3.01–29.34) 1.00 (ref.) 4.93 (2.44–9.98) 1.00 (ref.) 2.77 (1.19–6.47) |
.050 .484 - .157 .388 .171 - <.001 - <.001 - .019 |
| Premorbid employment type Nonoffice worker Office worker |
1.00 (ref.) 1.93 (1.20–3.10) |
- .007 |
- - |
- - |
1.00 (ref.) 2.67 (1.26–5.64) |
- .010 |
| Premorbid employment nature Part time Full time |
1.00 (ref.) 2.33 (1.07–5.06) |
- .032 |
- - |
- - |
1.00 (ref.) 0.42 (0.11–1.58) |
- .201 |
| Attitude toward RTW* Not important/neutral quite/very important |
1.00 (ref.) 8.32 (4.60–15.1) |
- <.001 |
- - |
- - |
1.00 (ref.) 11.90 (5.15–27.52) |
- <.001 |
NOTE. Model 1 covariates are age and sex+clinical and functional predictors (CCI score, type and area of stroke, language impairment, FIM: walking at discharge, FIM: cognitive total at discharge). Model 2 covariates are age and sex+clinical and functional+demographic predictors (premorbid employment type, premorbid employment nature, personal attitude toward return to work).
Abbreviations: LACI, lacunar infarct; PACI, partial anterior circulation infarct; POCI, posterior circulation infarct; ref., reference; RTW, return to work; SGD, Singapore dollar; TACI, total anterior circulation infarct.
At phone interview (2-y time point).
Effect modification
There was a lack of evidence that the effect of NIHSS score at admission on returning to work was modified by ambulation FIM or cognitive FIM at discharge. In table 4, among patients with ambulation FIM at discharge of 1-4, the adjusted OR of returning to work for patients with an NIHSS score of 0-4 (vs 5-29) was 3.71 (95% CI, 0.76-18.14). On the other hand, the adjusted OR among patients with ambulation FIM at discharge of 5-7 was 1.23 (95% CI, 0.34-4.41).
Table 4.
Effect modification of NIHSS (admission) on return to work by FIM: walking (discharge) and cognitive total (discharge) in 198 participants
| FIM: Walking (Discharge) | NIHSS Score (Admission) 5-29 |
NIHSS Score (Admission) 0-4 |
Adjusted OR (95% CI) Within FIM: Walking (Discharge) Stratum | P Value Within FIM: Walking (Discharge) Stratum | P Value of Effect Modification on Multiplicative Scale |
|---|---|---|---|---|---|
| n (%) RTW |
n (%) RTW |
||||
| Need assistance (1-4) Supervision to independence (5-7) |
18 (27.3) 42 (65.6) |
12 (46.2) 29 (69.1) |
3.71 (0.76-18.14) 1.23 (0.34-4.41) |
.105 .749 |
.176 |
| FIM: Cognitive Total (Discharge) | NIHSS (Admission) 5-29 |
NIHSS (Admission) 0-4 |
Adjusted OR (95% CI) Within FIM: Cognitive Total (Discharge) Stratum | P Value Within FIM: Cognitive Total (Discharge) Stratum | P Value of Effect Modification on Multiplicative Scale |
| n (%) RTW |
n (%) RTW |
||||
| <25 ≥25 |
11 (25.6) 49 (56.3) |
1 (9.0) 40 (69.0) |
0.27 (0.01-13.01) 2.09 (0.77-5.72) |
.505 .149 |
.238 |
NOTE. ORs and P values were adjusted for covariates in model 2 (age and sex+clinical and functional+demographic predictors).
Abbreviation: RTW, return to work.
In table 4, among patients with a cognitive FIM at discharge ≥25, the adjusted OR of returning to work for patients with an NIHSS score of 0-4 (vs 5-29) was 2.09 (95% CI, 0.77-5.72). On the other hand, the adjusted OR among patients with a cognitive FIM at discharge <25 was 0.27 (95% CI, 0.01-13.01).
There was no evidence of nonlinearity in the relationship between age and return to work using the Box-Tidwell test (P=.059). The proportion of return to work by age categories is found in Supplemental Table S1.
Discussion
A Swedish registry-based study and the Korean Stroke Cohort for Functioning and Rehabilitation study found that the majority of patients returned to work within 3 months to 2 years.6,16 The intent of conducting the interview at 2 years post stroke was because some patients took longer than a year to return to work. The ambulation FIM score was chosen because it reflects the ability or potential for community mobility, which is required for returning to work. Cognitive FIM was chosen because cognition is a known factor that influences return to work.19 The intervals between the FIM scores were not equal in terms of difficulty20; therefore, cutoffs of 5 and 25 (supervision level) were used for both ambulation and cognitive subscales, respectively. The proportion of return to work of 46% in our study is congruent with studies performed in Singapore7,21 and internationally.8,22 Survivors of stroke in our group had minor, moderate, and moderate to severe strokes, as indicated by the admission NIHSS scores, and underwent inpatient rehabilitation without an early supported discharge program in contrast to earlier studies of patients with stroke with residual mild to moderate disabilities involving early supported discharge.14 While there were many positive associations, independent predictive factors suggested by multivariable regression were viewing return to work as important, absence of language impairment post discharge, ambulation FIM≥5 (mobility at supervision to independence level) on discharge, cognitive FIM on discharge ≥25, a lower CCI score at discharge, and employment in premorbid office work. A lower CCI score at discharge16 and the absence of language impairment has also been a significant predictive factor in previous studies.5,22, 23, 24, 25
From the literature review, survivors of stroke who were younger, had a shorter length of stay, and did not have severe physical and cognitive impairments had a higher probability of return to work.5,6,16,23,26 In multivariable model 2, age was not statistically significant when other demographic factors were included in the analysis. Singapore has a graying population, and the retirement age is currently 62 and will be raised to 65, and the upper limit of reemployment age of 67 will be increased to 70 locally.27 In Supplemental Table S1, there is a sharper decline in proportion of return to work after age 52 compared with younger persons and further progressive decline after the retirement age of 62 after, which stabilizes past the reemployment age. In accordance with the Retirement and Re-employment Act, employers must offer reemployment to eligible employees when they reach the retirement age to help older workers continue to work if they are willing and able to. In our study, higher income and higher education were not correlated with successful return to work, unlike studies involving bigger numbers of participants (314 vs 7081).28
Our study further extended the functional evaluation during acute inpatient stay by using FIM as a predictive factor for return to work. The FIM may be more sensitive than the more commonly used modified Rankin Scale in identifying cognitive impairments,29 although dependency at discharge (using the modified Rankin Scale) has been known to be a negative predictive factor.7 Because patients with stroke undergoing rehabilitation in the acute phase are usually assessed in detail with the FIM instrument used regularly by multidisciplinary teams, it may be useful to use the FIM to aid in prediction, prognostication, and facilitation of return to work post stroke. The absence of severe physical and cognitive impairment may be difficult to quantify; however, the FIM is an objective and clear-cut assessment tool that is an independent predictive factor. FIM as a predictive factor concurred with an earlier study9 in which a higher FIM score on discharge significantly reflected a better rate of return to work. The intervals between the FIM scores, however, are not equal in terms of difficulty, and it is not known what cutoff score could be used to identify a patient who would be successful in returning to work in that study.
A Swedish study found that participants with expectations of returning to work had higher odds of success within 5 years.6 Our study similarly suggests that this may be applicable in our population, and an attitude toward the importance of returning to work post stroke may be associated with successful RTW. Financial reasons are often cited as the reasons for returning to work. Working closely with medical social workers in the short-term poststroke period is a worthwhile exploration for appropriate patient support. As with other studies,23,24 our study found that office workers had greater odds of returning to work than nonoffice workers.
Patients may be evaluated early using predictive factors such as their premorbid type of work, ambulation and cognitive FIM, absence of language impairments, and viewing return to work as important, and more attention should be paid to linking suitable candidates to outpatient vocational rehabilitation services. Given that these factors are straightforward to assess, a nurse or an allied health member could be the champion to provide screening and direct patients to relevant services. Intentionally pairing patients with such services, particularly those who view returning to work seriously, would better allocate available resources and expedite their return to the workforce.
Although specialized vocational rehabilitation programs are available in the community and despite these programs having success rates of up to 88%30 as reported in a previous study, the number referred to such services in our cohort was only 26, with a success rate of 53.8% overall. In the specialized programs from the previous study, patients tended to be younger, with an average age of 44 years, and spent a median of 9 months in the program. More collaboration with such services should be formalized and extended to a slightly older age group because older age was not a significant independent predictive factor in determining where help may be needed to ensure a successful return to work. Further studies with good predictive factors should be conducted to examine referral patterns to community vocational programs and their success in older patient groups.
Study limitations
Because the study was partially based on telephone interviews, there may be an element of recall bias. Another limitation is the inconsistency in the application of cognitive tools, such as the Montreal Cognitive Assessment and Mini-Mental State Examination, during these time periods; therefore, we relied on cognitive FIM for correlation with return to work. This study was underpowered to detect any effect modifications.
Because this study was performed after discharge from an inpatient rehabilitation unit in Singapore, the implications for overseas centers are unknown. Furthermore, the use of FIM as an outcome measure in inpatient rehabilitation has been discontinued in the US, limiting the use of FIM as a predictive tool for return to work prognostication.
Conclusions
In this study, viewing return to work as important, absence of language impairments at 2 years post stroke, discharge ambulation FIM≥5, discharge cognitive FIM≥25, employment in premorbid office work, and a lower CCI score at discharge independently predicted successful return to work. Most of these predictors may serve as a simple and abbreviated guide in prognostication and facilitation of return to work in the rehabilitation setting.
FIM
| Self-care |
| a) Eating |
| b) Grooming |
| c) Bathing |
| d) Dressing: upper body |
| e) Dressing: lower body |
| f) Toileting |
| Sphincter control |
| g) Bladder management |
| h) Bowel management |
| Transfers |
| i) Bed, chair, wheelchair |
| j) Toilet |
| k) Tub, shower |
| Locomotion |
| l) Walk/wheelchair |
| m) Stairs |
| Motor subtotal score |
| Communication |
| n) Comprehension |
| o) Expression |
| Social cognition |
| p) Social interaction |
| q) Problem solving |
| r) Memory |
| Cognitive subtotal score |
| Total FIM score |
| FIM scoring |
| Independent |
| 7: Complete independence (timely, safely) |
| 6: Modified independence (device) |
| Modified dependence |
| 5: Supervision (subject=100%+) |
| 4: Minimal assist (subject+75%+) |
| 3: Moderate assist (subject+50%+) |
| Complete dependence |
| 2: Maximal assist (subject=25%+) |
| 1: Total assist (subject=less than 25%) |
Supplier
a. Stata 15.0; StataCorp LLC.
Acknowledgments
We thank Christopher Paul and Dr Liew Siew Lee.
Footnotes
List of abbreviations: CCI, Charlson Comorbidity Index; CI, confidence interval; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio.
Declaration of Conflicting Interests: This study was reviewed and approved by Singhealth CIRB (CIRB 2018/2066) for ethics clearance.
Disclosures: none.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2022.100253.
Appendix. Supplementary materials
References
- 1.1.3GBD 2019 Stroke Collaborators Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gittins M, Lugo-Palacios D, Vail A, et al. Stroke impairment categories: a new way to classify the effects of stroke based on stroke-related impairments. Clin Rehabil. 2021;35:446–458. doi: 10.1177/0269215520966473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leys D, Hénon H, Mackowiak-Cordoliani MA, Pasquier F. Poststroke dementia. Lancet Neurol. 2005;4:752–759. doi: 10.1016/S1474-4422(05)70221-0. [DOI] [PubMed] [Google Scholar]
- 4.Evers SM, Struijs JN, Ament AJ, van Genugten ML, Jager JH, van den Bos GA. International comparison of stroke cost studies. Stroke. 2004;35:1209–1215. doi: 10.1161/01.STR.0000125860.48180.48. [DOI] [PubMed] [Google Scholar]
- 5.Wang YC, Kapellusch J, Garg A. Important factors influencing the return to work after stroke. Work. 2014;47:553–559. doi: 10.3233/WOR-131627. [DOI] [PubMed] [Google Scholar]
- 6.Westerlind E, Persson HC, Eriksson M, Norrving B, Sunnerhagen KS. Return to work after stroke: a Swedish nationwide registry-based study. Acta Neurol Scand. 2020;141:56–64. doi: 10.1111/ane.13180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westerlind E, Persson HC, Sunnerhagen KS. Return to work after a stroke in working age persons; a six-year follow up. PLoS One. 2017;12 doi: 10.1371/journal.pone.0169759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westerlind E, Abzhandadze T, Rafsten L, Rafsten L, Persson HC, Sunnerhagen KS. Very early cognitive screening and return to work after stroke. Top Stroke Rehabil. 2019;26:602–607. doi: 10.1080/10749357.2019.1645440. [DOI] [PubMed] [Google Scholar]
- 9.Chan WY, Chew NJ, Nasron LI, Fook-Chong SM, Ng YS. A cross-sectional study of the demographic, cultural, clinical and rehabilitation associated variables predicting return to employment after disability onset in an Asian society. Work. 2012;43:461–468. doi: 10.3233/WOR-2012-1374. [DOI] [PubMed] [Google Scholar]
- 10.Chang WH, Sohn MK, Lee J, et al. Return to work after stroke: the KOSCO study. J Rehabil Med. 2016;48:273–279. doi: 10.2340/16501977-2053. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health, Singapore. Principal causes of death. Available at: https://www.healthhub.sg/a-z/health-statistics/4/principal-causes-of-death. Accessed December 6, 2021.
- 12.Chan ML. Description of a return-to-work occupational therapy programme for stroke rehabilitation in Singapore. Occup Ther Int. 2008;15:87–99. doi: 10.1002/oti.248. [DOI] [PubMed] [Google Scholar]
- 13.Lim MJR, Wong BTY, Koh PPW, Raszewski R, Asano M. A brief review of post-stroke employment in Singapore. Int J Neurorehabilitation Eng. 2019;6:4. [Google Scholar]
- 14.Teo SH, Chen Z. Effectiveness of an activity-based home therapy program for stroke patients in Singapore. Arch Phys Med Rehabil. 2016:97. [Google Scholar]
- 15.Rost NS, Bottle A, Lee JM, et al. Stroke severity is a crucial predictor of outcome: an international prospective validation study. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.115.002433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han J, Lee HI, Shin YI, et al. Factors influencing return to work after stroke: the Korean Stroke Cohort for Functioning and Rehabilitation (KOSCO) study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-028673. https://www.sgenable.sg/about-us/our-story SG Enable. Our story. Available at: Accessed December 8, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.SPD. Who we are. Available at: https://spd.org.sg/about-us. Accessed December 8, 2022.
- 18.Blackburn DJ, Bafadhel L, Randall M, Harkness KA. Cognitive screening in the acute stroke setting. Age Ageing. 2013;42:113–116. doi: 10.1093/ageing/afs116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75:127–132. [PubMed] [Google Scholar]
- 20.Health Promotion Board. Singapore Stroke Registry annual report 2019. Available at:https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/ssr-annual-report-2019.pdf?sfvrsn=594314c4_0. Accessed December 14, 2021.
- 21.Aarnio K, Rodríguez-Pardo J, Siegerink B, et al. Return to work after ischemic stroke in young adults: a registry-based follow-up study. Neurology. 2018;91:e1909–e1917. doi: 10.1212/WNL.0000000000006510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanaka H, Toyonaga T, Hashimoto H. Functional and occupational characteristics predictive of a return to work within 18 months after stroke in Japan: implications for rehabilitation. Int Arch Occup Environ Health. 2014;87:445–453. doi: 10.1007/s00420-013-0883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanaka H, Toyonaga T, Hashimoto H. Functional and occupational characteristics associated with very early return to work after stroke in Japan. Arch Phys Med Rehabil. 2011;92:743–748. doi: 10.1016/j.apmr.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Doucet T, Muller F, Verdun-Esquer C, Debelleix X, Brochard P. Returning to work after a stroke: a retrospective study at the Physical and Rehabilitation Medicine Center La Tour de Gassies. Ann Phys Rehabil Med. 2012;55:112–127. doi: 10.1016/j.rehab.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 25.Wozniak MA, Kittner SJ, Price TR, Hebel JR, Sloan MA, Gardner JF. Stroke location is not associated with return to work after first ischemic stroke. Stroke. 1999;30:2568–2573. doi: 10.1161/01.str.30.12.2568. [DOI] [PubMed] [Google Scholar]
- 26.The Straits Times. Retirement and re-employment ages in Singapore will be raised to 65 and 70. Available at:https://www.straitstimes.com/singapore/politics/retirement-and-re-employment-ages-will-be-raised-to-65-and-70. Accessed June 30, 2022.
- 27.Trygged S, Ahacic K, Kåreholt I. Income and education as predictors of return to working life among younger stroke patients. BMC Public Health. 2011;11:742. doi: 10.1186/1471-2458-11-742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kapoor A, Lanctôt KL, Bayley M, et al. Good outcome” isn't good enough. Cognitive impairment, depressive symptoms, and social restrictions in physically recovered stroke patients. Stroke. 2017;48:1688–1690. doi: 10.1161/STROKEAHA.117.016728. [DOI] [PubMed] [Google Scholar]
- 29.Bin Zainal MN, Pei Wen PK, Sien NY, Kee KM, Chieh KJ, Asano M. Supporting people with stroke to return to work in Singapore: findings from a pilot vocational rehabilitation program. Am J Occup Ther. 2020;74 doi: 10.5014/ajot.2020.041376. 7406205040p1-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.