Abstract
Intervention
In 2014–2015, more than 400 public housing units were constructed in Nunavut and Nunavik, two of the four Inuit regions in Canada. This provided the opportunity to assess the impact of improved housing conditions from a population health perspective in 12 Inuit communities where housing needs were the most severe. The aim of the research is to examine the associations between changes in housing conditions and changes in psychological distress pre-post rehousing.
Methods
A pre-post uncontrolled study was conducted in collaboration with Nunavut- and Nunavik-based organizations. Applicants at the top of public housing waitlists were recruited by local housing officers; participants completed questionnaires 1–6 months before rehousing, and 15–18 months after. Change in psychological distress was measured with the Kessler 6-item scale. Changes in three housing measures were examined: number of adults per household, number of children per household, and sense of home score. For each housing measure, a categorical variable stratified participants into three categories. The reference category included participants reporting significant change in the concerned housing measure; the two other categories included participants reporting little or no change. Associations were tested with linear multilevel regression models for change.
Results
A total of 102 Inuit adults completed the study. A reduction in the number of adults per household (living with 2 adults or less after rehousing) and an increase in sense of home were associated with significant decline in psychological distress pre-post rehousing (p < 0.001).
Conclusion
Increased investments leading to such improvements in housing circumstances are promising ways to promote mental health in Inuit regions.
Supplementary Information
The online version contains supplementary material available at 10.17269/s41997-022-00701-0.
Keywords: Housing, Population health intervention research, Health promotion, Mental health, Psychological distress, Inuit, Indigenous peoples
Résumé
Intervention
En 2014-2015, plus de 400 logements sociaux ont été construits au Nunavut et au Nunavik, deux des quatre régions inuites du Canada, permettant ainsi d’évaluer l’impact de l’amélioration des conditions de logement sur la santé. Cette étude vise à examiner les associations entre les changements dans les conditions de logement et les changements dans la détresse psychologique avant et après le déménagement, dans 12 communautés inuites où les besoins en logement étaient les plus criants.
Méthodes
Une étude pré-post non contrôlée a été menée en collaboration avec des organisations du Nunavut et du Nunavik. Les participants figurant en tête des listes d’attente pour le logement social ont rempli les questionnaires de recherche 1-6 mois avant le déménagement et 15-18 mois après. Les changements de la détresse psychologique ont été mesurés à l’aide de l’échelle Kessler 6-item. Les changements des trois conditions de logement suivantes ont été examinés : le nombre d’adultes par ménage, le nombre d’enfants par ménage et le sentiment d’avoir un chez-soi. Pour chaque condition de logement, une variable catégorielle a été créée pour stratifier les participants ayant rapporté des changements (référence) et les participants n’ayant rapporté que peu ou pas de changement. Les associations ont été testées avec des modèles de régression linéaire multiniveaux.
Résultats
Un total de 102 adultes Inuit ont complété l’étude. Une réduction du nombre d’adultes par ménage (vivre avec 2 adultes ou moins après le déménagement) et une augmentation du sentiment d’avoir un chez-soi étaient associées à une baisse significative de la détresse psychologique (p < 0,001).
Conclusion
Des investissements accrus menant à de telles améliorations des conditions de logement représentent une avenue prometteuse pour promouvoir la santé mentale dans les régions inuites.
Mots-clés: Logement, recherche interventionnelle en santé des populations, promotion de la santé, santé mentale, détresse psychologique, Inuit, Peuples autochtones
Introduction
Housing is a key social determinant of health (NCCIH, 2017). In Inuit regions — collectively known as Inuit Nunangat (Fig. 1, map) — the progressive decline in federal funding transfers under social housing agreements since 1993, coupled with the economic hardship in the Canadian Arctic, have left regional housing authorities with insufficient capital to cover the costs of housing construction, operation, and maintenance (Standing Senate Committee on Aboriginal Peoples, 2017). This situation has created a sizeable housing backlog across all Inuit regions, but most importantly in Nunavut and Nunavik (ITK, 2019; 26). The severe housing shortage has, in turn, led to elevated levels of overcrowding and hidden homelessness (Minich et al., 2011), which have had detrimental consequences on Inuit mental health and well-being. Indeed, analyses from the 2012 Aboriginal Peoples Survey (APS) demonstrate that poor housing quality and household crowding are associated with higher psychological distress among Inuit (Anderson, 2015) and with suicidal behaviours (ideations and attempts) among Indigenous peoples (including the Inuit) (Hajizadeh et al., 2019). To date, research on Inuit health has largely been disease-oriented and there is a need for studies examining health-promoting interventions that address priorities determined by the Inuit (Hayward et al., 2020). The Inuit Nunangat Housing Strategy stresses the importance of assessing the effectiveness of recent investments in housing and to examine whether they lead to better social and health outcomes for the Inuit (ITK, 2019; 14-17). In 2014–2015, more than 400 public housing units were constructed in Inuit communities in which housing needs were the most severe. This study explores the associations between changes in housing conditions and changes in psychological distress among Inuit adults who had moved to a new or preexisting public housing unit.
Fig. 1.
Map of Inuit Nunangat. Source: https://www.itk.ca/inuit-nunangat-map/
The urgency of increased federal investments to reduce housing disparities in Canada has been advocated by Inuit representatives under social and health equity arguments (ITK, 2019; Qaqqaq, 2021). Such disparities are exemplified by recent data on housing suitability, a measure of crowding referring to whether the dwelling has enough bedrooms for the size and composition of the household (Statistics Canada, 2017a). In 2016, 56% and 52% of the population in Nunavut and Nunavik, respectively, lived in housing considered not suitable, as compared to 8.5% for non-Indigenous Canadians (Statistics Canada, 2017a). Across Inuit homelands, household crowding has been associated with depressive symptoms (Riva et al., 2014a) and with elevated chronic stress (Riva et al., 2014b), especially for Inuit women. However, the detrimental role of crowding on health and health behaviours is not as straightforward as these studies imply. In Riva et al. (2014a), higher levels of crowding were associated with lower odds of binge drinking. This counterintuitive association was explained by household composition: the odds of reporting binge drinking were lower in households with children (who contribute significantly to overcrowding given their demographic weight in Inuit regions), compared to adult-only households (Riva et al., 2014a). Because of ongoing debates on the measure of overcrowding in Indigenous populations, for example regarding whether ‘one person per room’ is a culturally appropriate measure (Lauster & Tester, 2010), studies often additionally explore the effect of household size (total number of occupants) and household composition variables (number of adults and children), which have both been linked to self-rated health and mental health (Hansen et al., 2020).
To our knowledge, the link between housing conditions and mental health among Inuit has never been assessed through housing intervention research, and therefore relies almost entirely on cross-sectional associations, with few exceptions (Hansen et al., 2020; Pepin et al., 2018). Cross-sectional associations provide limited evidence on the possible effects of housing improvements on mental health (Pierse et al., 2016).
Another shortcoming raised in housing and mental health literature is the scarcity of studies examining psychosocial processes mediating the associations between housing and health, which can help explain why housing improvements lead, or do not lead, to mental health benefits (Thomson & Thomas, 2015). ‘Sense of home’ conceptually encompasses these psychosocial processes, sometimes referred to as ‘psychosocial benefits from the home’ (Kearns et al., 2011) or ‘psychosocial factors’ (Perreault et al., 2020), defined as social mechanisms inherent to the home environment that positively influence the psychological state of mind of individuals. Increased usable space, improved domestic relationships, or increased opportunities for privacy, studying, and leisure in the home, are examples of psychosocial factors described as having beneficial impact on well-being (Thomson & Thomas, 2015). However, intervention research exploring the impact of improved psychosocial factors, or sense of home, on mental health and well-being has been conducted exclusively in non-Indigenous settings (e.g., Kearns et al., 2011; Padgett, 2007; Rolfe et al., 2020).
Population health intervention research in the Canadian Arctic
The large-scale construction of new public housing units in selected Inuit communities in Nunavut and Nunavik allowed many families to move into these new units, and therefore, presented the opportunity to assess the benefits of changes in housing conditions from a population health intervention perspective. The present study is part of the project Housing, health and well-being in Nunavik and Nunavut, for which pre-post changes in housing conditions and health outcomes were previously examined. After rehousing, a significant reduction in household size was observed, along with improvement in sense of home (Riva et al., 2020b), and decline in psychological distress (Riva et al., 2020a). In addition to the health benefits of moving into new housing, the extent to which improvements in housing conditions explain improvements in psychological distress remains to be established.
Objective
The aim of this article is to assess whether changes in number of adults per household, number of children per household, and sense of home are associated with changes in psychological distress pre-post rehousing.
Methods
A detailed account of methods used in the project was published elsewhere (Perreault et al., 2020; Riva et al., 2020b) and is summarized here.
Inuit regions where the project was conducted: Nunavut and Nunavik
In 2016, nearly 42,000 (65%) of the 65,000 Inuit in Canada lived in Nunavut and Nunavik, the most populous regions of Inuit Nunangat (ITK, 2018), counting 39 remote and isolated communities with populations ranging from 129 to 7740 inhabitants (Levesque & Duhaime, 2019; Nunavut Bureau of Statistics, 2021). None of the communities have road access; they can only be reached by air year-round, or seasonally by water or ice roads. In both regions, the housing market is highly subsidized with more than 80% of the population living in public housing, compared to 13% for Canada as a whole (Statistics Canada, 2017b).
Intervention, recruitment of participants, and sample size
The intervention on which the study is based is the ‘rehousing’ of adult tenants to a newly constructed unit or to a preexisting unit that became available in their community. No differences were observed in terms of major or minor repairs needed between the newly constructed and preexisting units after rehousing (Riva et al., 2020b; supplemental material). The study took place in 12 selected Inuit communities in Nunavut and Nunavik. Construction included a mix of one-, two-, and four-bedroom housing units in multiplexes accommodating adult(s) and family households. Within communities, units were allocated to applicants most in need, where need is assessed on a point-based system, according to criteria such as low income, number of dependent children, living in overcrowded dwellings, or social problems at home (KMHB, 2014; NHC, 2015). Applicants ranked at the top of the waitlist for social housing, i.e., those who were most likely to move, were recruited by local housing officers. All adults aged ≥ 18 years living with the applicants, and who would be moving with them, were invited to participate. Of the 289 participants recruited, 186 did move to a new unit, and 169 were eligible at follow-up (still living in the community and in the same public housing unit). Of these, 102 participants (87 households) completed the study. Among the participants lost at follow-up (n = 67), 20 participants were not reachable, 28 refused to participate, and 19 were lost for other reasons (the flow chart and losses at follow-up are detailed in Riva et al., 2020b). No differences in age, sex, income, and psychological distress scores were observed at baseline between participants who were and were not rehoused, or between rehoused participants who did and did not complete the study (Riva et al., 2020a).
Notwithstanding that all participants received the intervention (rehousing), variation occurred in the magnitude of housing changes pre-post rehousing: some participants experienced improvements of their housing circumstances, while others did not. Variation was also observed in psychological distress pre-post rehousing, hence providing the necessary conditions for testing longitudinal associations between changes in housing measures and changes in psychological distress.
Study design and data collection
This study used a pre-post uncontrolled design. Baseline data were collected 1 to 6 months before rehousing (2014–2015), and follow-up data were collected 15 to 18 months after rehousing (2016–2017). Questionnaires were administered face to face before and after rehousing. They were administered in English by a research assistant or in Inuktut by an interpreter. Information on housing conditions, sense of home, and health outcomes were collected, as well as socioeconomic characteristics. Questionnaires were pilot tested with Inuit living in Nunavik, Nunavut, and Quebec City; adaptations were then made according to participants’ or interpreters’ comments.
Ethical implications
This project was developed in collaboration with organizations responsible for housing, public health, and advancing Inuit rights and interests (see Acknowledgements section) in Nunavut and Nunavik. It was reviewed and supported by the Nunavik Nutrition and Health Committee (NNHC), the Nunavut Research Institute, and the mayors of all communities involved. It received ethical approval from the Comité d’éthique de la recherche du CHU de Québec – Université Laval, and from McGill University’s Institutional Review Board. At recruitment, potential participants were contacted by local housing managers and were informed that their participation in the project (or refusal to participate) would not affect their rank on the waitlist, their current housing situation, or whether they would get to move. All participants provided informed written consent. Partner organizations contributed to developing the objectives and the design of the study. A previous version of the manuscript was shared with regional partners for their critical review and approval, and to ensure that findings were made available to Nunavik and Nunavut first. Three virtual meetings were organized to present and discuss the main findings with partner organizations, other organizations in Nunavut and Nunavik, and community members. All comments and suggestions received were integrated in the present manuscript which was again shared with partner organizations, who approved the final version and its submission to the journal.
Psychological distress measure
The main outcome is change in psychological distress pre-post rehousing, measured as a continuous score, based on the Kessler-6 scale (K6) (Kessler et al., 2002). The K6 is an appropriate screening and severity measure for symptoms of anxiety and depression (Cairney et al., 2007), and has been validated among Inuit in the 2012 Aboriginal People Survey in Canada (Statistics Canada, 2015). It consists of six questions that require participants to indicate how often, in the last month, they felt: (1) nervous, (2) hopeless, (3) restless or fidgety, (4) so depressed that nothing could cheer them up, (5) that everything was an effort, and (6) worthless. Participants reported frequency on a 5-point Likert scale (0 = none of the time; 4 = all of the time). The overall score ranges from 0 to 24, with higher scores reflecting higher psychological distress. The mean K6 score for Inuit diagnosed with mood disorders (such as depression) in the 2012 APS was 8.9 points, versus 2.9 points for Inuit who were not (Statistics Canada, 2015).
Housing measures
Three housing measures were examined: number of adults per household, number of children per household, and sense of home. For each housing measure, participants were classified in one of three nominal categories. The reference category included participants who reported significant change in the concerned housing condition, whereas the two other categories included participants who reported little or no change. The hypothesis was that significant changes in housing conditions would be associated with reduced psychological distress.
Number of adults and number of children per household
Before and after rehousing, participants reported the number of occupants in their house, with specific numbers of adults and children. The presence of children in a household relates differently to health outcomes than the presence of adults (Riva et al., 2014a). Therefore, instead of examining the effect of change in the total number of occupants on change in psychological distress, we examined the effect of change in the number of adults, and change in the number of children, in two separate models. In qualitative interviews conducted in Nunavut exploring the rehousing experiences of Inuit adults (Perreault et al., 2022), almost all participants expressed a preference for households composed of one or two adults (and their children, if applicable).
Categories defining pre-post change in the number of adults
Categories were computed using the cut-off of 3 adults, based on the aforementioned household composition preference, yielding the following nominal categories: 0 = participants who lived with ≥ 3 adults before rehousing, and with ≤ 2 adults after rehousing (reference); 1 = participants who lived with ≥ 3 adults pre-post rehousing; 2 = participants who lived with ≤ 2 adults pre-post rehousing.
Categories defining pre-post change in the number of children
We found no evidence of a specific cut-off that would be considered preferable or associated with health benefits. We therefore used the cut-off of 3 children, based on the pooled median (pre-post), and similarly computed three nominal categories: 0 = participants who lived with ≥ 3 children before rehousing, and with ≤ 2 children after rehousing (reference); 1 = participants who lived with ≥ 3 children pre-post rehousing; 2 = participants who lived with ≤ 2 children pre-post rehousing. Only 4 participants reported living with ≤ 2 children before rehousing, and with ≥ 3 children after rehousing, and were excluded from the analysis. This decision was based on the parsimony principle (Singer & Willett, 2003; 105) since their inclusion would have implied the creation of a fourth nominal category, with the effect of reducing statistical power and complicating the model’s interpretation, without further contributing to answering the research question.
Sense of home
The sense of home scale used is described in detail elsewhere (Perreault et al., 2020). Briefly, the scale is composed of eight items representing psychosocial benefits from the home: space, identity, control, privacy, satisfaction, relationships, location, and safety. Participants answered each item using a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree). Answers were summed to obtain the total sense of home score. The scale demonstrated satisfactory internal reliability with a Cronbach’s alpha coefficient of 0.76, which was assessed using data from the baseline sample of 289 participants (Perreault et al., 2020). Sense of home scores range from 8 to 40, with higher values indicating stronger sense of home.
Categories defining pre-post change in sense of home scores
Categories’ cut-offs were determined based on pooled (pre-post) score tertiles: lowest tertile (scores ≤ 27); mid tertile (scores ≥ 28 but ≤ 31); highest tertile (scores ≥ 32). Participants with scores in the mid or highest tertiles were merged into one category, ‘mid/highest’, since they presented no differences in psychological distress. The following pre-post sense of home nominal categories were computed: 0 = participants who reported sense of home scores in the lowest tertile (≤ 27) before rehousing, and in the mid/highest tertiles after rehousing (≥ 28) (reference); 1 = participants with scores in the mid/highest tertiles pre-post rehousing; 2 = participants with scores in the lowest tertile pre-post rehousing. Only 6 participants reported scores ≥ 28 before rehousing, and ≤ 27 after rehousing, and were excluded from the analyses. As for the previous variable, this decision was based on the parsimony principle (Singer & Willett, 2003;105).
Covariates
Age, sex, and region of residence were included in models as confounding variables. Age was centered around its mean for use in multilevel models for change.
Statistical analyses
All analyses were conducted using Stata v14.2. Differences between the means pre and post rehousing were assessed with paired t-tests, within each category of number of adults, number of children, and sense of home (Table 1). To assess the associations between changes in each of the three housing conditions and change in the continuous scores of psychological distress pre-post rehousing, we applied linear multilevel regression models for change that account for the nested nature of the data in the estimation of fixed effects (Singer & Willett, 2003; 47). The dataset included observations at two time points (level 1), within individuals (level 2), within households (level 3), and within communities (level 4). We opted for a parsimonious 2-level model after having performed variance component estimations and likelihood-ratio tests comparing it with a 3- and a 4-level model. These verifications confirmed that a 2-level model was appropriate for the estimation of fixed effects and led to slightly superior goodness-of-fit statistics (Singer & Willett, 2003; 94–96, 122). Separate models were built for each categorical variable (number of adults, number of children, and sense of home) (Table 2, models a, b, c). Statistical significance was set at p ≤ 0.05. The equation for the fully adjusted models reads as:
Table 1.
Socio-demographic and housing indicators of study participants before rehousing (n = 102 study participants; 87 households)
| n (%) | |
|---|---|
| Socio-demographic characteristicsa | |
| Age categories | |
| 18–25 years | 36 (35) |
| 26–35 years | 40 (39) |
| 36–45 years | 11 (11) |
| ≥ 46 years | 15 (15) |
| Sex (women) | 58 (57) |
| Region of residence (Nunavut) | 49 (48) |
| Work for pay (yes) | 63 (62) |
| Personal income | |
| < $20,000 | 59 (58) |
| $20,000–$40,000 | 22 (22) |
| >$40,000 | 16 (16) |
| Missing | 5 (5) |
| Housing indicatorsb | |
| Time on the waitlist | |
| < 1 year | 11 (13) |
| 1 to < 2 years | 15 (17) |
| 2 to < 4 years | 25 (29) |
| ≥ 4 years | 33 (38) |
| Missing | 3 (3) |
| Average number of occupants per housing unit (adults and children), mean (SE) | 6.9 (0.4) |
| Overcrowding (PPR >1)c | 57 (66) |
| Perceived overcrowdingd | 53 (62) |
| Households with people who had no place to live (hidden homelessness)e | 27 (31) |
| Missing | 3 (3) |
aDescriptive data, 102 study participants
bDescriptive data, 87 households
cPPR: ‘Persons per room’ is an indicator of the level of household crowding calculated by dividing the number of persons in the household by the number of rooms in the dwelling. PPR > 1 = overcrowding. At the time of data collection, it was the indicator used by Statistics Canada
dHousehold respondent who answered ‘yes’ to the question: Do you think there are too many people living in your house?
eHousehold respondent who answered ‘yes’ to the question: During the past year, were there people living in your house because they had nowhere else to live (i.e., they did not have a house to live in)?
Table 2.
Comparison of housing conditions at pre and post rehousing for participants who completed the study, by housing categorical variables
| Mean (SD) PRE |
Mean (SD) POST† |
Difference pre-postb |
|
|---|---|---|---|
| Number of adults per household | |||
| a. Pre-post number of adults per household (na) | |||
| 0. ≥ 3 adults pre, ≤ 2 adults post (n = 73) | 5.1 (1.4) | 1.8 (0.4) *** | 3.3 |
| 1. ≥ 3 adults pre-post (n = 9) | 5.1 (1.5) | 3.3 (0.5) * | 1.8 |
| 2. ≤ 2 adults pre-post (n = 20) | 1.8 (0.4) | 1.7 (0.5) | 0.1 |
| Number of children per household | |||
| b. Pre-post number of children per household (na) | |||
| 0. ≥ 3 children pre, ≤ 2 children post (n = 33) | 4.0 (1.6) | 1.3 (0.7) *** | 2.7 |
| 1. ≥ 3 children pre-post (n = 21) | 4.6 (1.9) | 3.9 (1.4) | 0.7 |
| 2. ≤ 2 children pre-post (n = 44) | 1.0 (0.8) | 0.6 (0.8) ** | 0.4 |
| Sense of home score (/40) | |||
| c. Pre-post sense of home scores — tertiles (na) | |||
| 0. Lowest pre, mid/highest post (n = 39) | 22.6 (3.5) | 31.9 (2.7) *** | 9.3 |
| 1. Lowest pre-post (n = 7) | 22.1 (4.0) | 24.6 (3.5) | 2.5 |
| 2. Mid/highest pre-post (n = 40) | 32.0 (2.9) | 32.3 (2.5) | 0.3 |
aThe number of participants for each categorical variable does not add up to 102 participants (100%) due to exclusions (see Methods section)
bThe difference was obtained by subtracting post from pre rehousing values for the number of adults per household and the number of children per household (pre minus post), and inversely for the sense of home score (post minus pre)
†The means pre and post are statistically different; paired t-test where ***p < 0.001; **p ≤ 0.01; *p ≤ 0.05
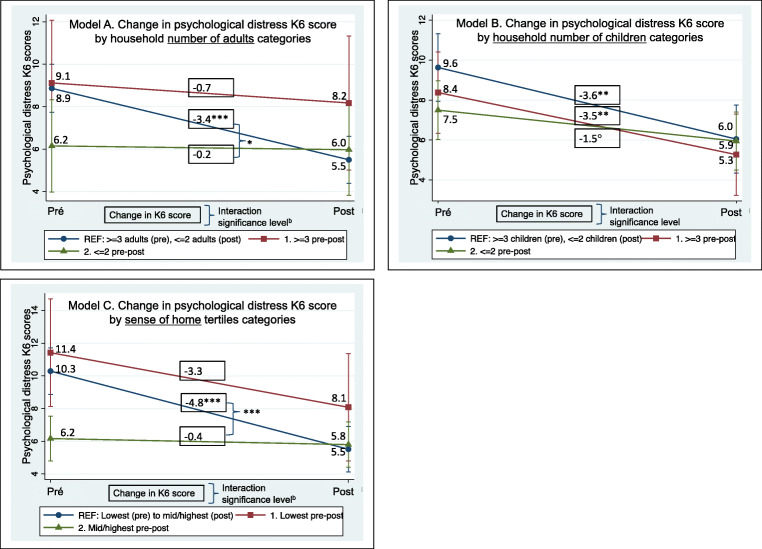
It estimates the value of K6 score for individual i on occasion j. Within each model, the fixed effect of ‘TIME’ (γ10) (0 = before rehousing; 1 = after rehousing) was used to estimate change in psychological distress K6 score for participants in the housing category of reference (coded ‘0’). The fixed effect of the cross-level interactions (γ11) was used to determine whether change in K6 scores for participants in the reference category differed from change in K6 scores for the two other categories (difference in the magnitude of change between categories) (Singer & Willett, 2003; 77–83). When γ10 and one of the γ11 were non-zero, we considered that change in the housing condition (described by the category of reference) was associated with change in K6 scores. Pre and post rehousing K6 scores within each housing category (0, 1, and 2) were estimated through the margins command in Stata, which uses the equation of a previously fitted model and plots the predicted results, illustrated in Fig. 2A, B, and C. Household financial situation or the type of housing unit moved into (newly constructed vs. already existing) were not significantly associated with distress and did not affect the fixed effects of housing predictors. Therefore, these variables are not included in the final models. No interactions were observed between time and sex across models.
Fig. 2.
Graphs of linear multilevel regression models for change in psychological distress K6 score pre-post rehousing, by housing categorical variable: number of adults per household (Model A); number of children per household (Model B); sense of home score (Model C). Figures were generated using the margins command in Stata, see Methods section. ‘b’ indicates whether predicted change in psychological distress for participants in the reference category significantly differs from the predicted change for participants in category 2; corresponds to γ 11(TIMEij × HOUSINGcat.i) in Table 3. ***p < 0.001; **p ≤ 0.01; *p ≤ 0.05; °p < 0.10
Results
Before rehousing, the largest proportion of the 102 participants who completed the study were aged between 26 and 35 years old (39%) (total sample mean age: 31), were women (57%), worked for pay (62%), and earned less than CAN $20,000 annually (58%) (Table 1). Almost two fifths of households (38%) had been on the waitlist for social housing for 4 years or more and close to one third (32%) had temporarily hosted people who had nowhere else to live (hidden homeless people). Most of household respondents perceived they were living in overcrowded dwellings (62%).
Changes in housing measures pre-post rehousing
Means and standard deviations for the number of adults per household, number of children per household, and sense of home scores are presented before and after rehousing, by housing categorical variable (Table 2).
Regarding the number of adults per household, most participants (n = 73) were classified in the reference category (i.e., living with ≥ 3 adults before rehousing, and with ≤ 2 adults after) (Table 2a). This group saw a significant reduction in the number of adults per household, from an average of 5.1 adults per household before rehousing to 1.8 adults post rehousing (p < 0.001), or 3.3 fewer adults after rehousing. Participants in households with ≥ 3 adults pre-post (category 1) experienced a significant reduction in the number of adults in their households, with 1.8 fewer adults per household after rehousing (p = 0.012). This reduction was significantly smaller than that observed for the reference category (p < 0.001, data not shown). There was no significant change for participants classified in category 2 (≤ 2 adults pre-post).
For categories defining change in the number of children, participants were more evenly distributed across the three categories (Table 2b). Participants in the reference category (living with ≥ 3 children before rehousing, and with ≤ 2 children after) and in category 2 (≤ 2 children pre-post) saw significant reductions in the number of children in their households, with 2.7 (p < 0.001) and 0.4 (p = 0.004) fewer children respectively after rehousing. Again, the magnitude of change for participants in category 2 was significantly smaller than that observed in the reference category (p < 0.001, data not shown). There was no significant change for participants classified in category 1 (≥ 3 children pre-post).
Last, for categories defining change in sense of home, participants were mostly distributed across the reference category (n = 39) (from the lowest tertile (≤ 27 points) before rehousing, to the mid/highest tertiles after rehousing (≥ 28 points)) and category 2 (n = 40) (mid/highest tertile pre-post rehousing), with fewer participants in category 1 (lowest sense of home score pre-post) (Table 2c). Participants in the reference category experienced a significant increase of, on average, 9.3 points pre-post rehousing in their sense of home score (from a score of 22.6 before rehousing to 31.9 after rehousing; p < 0.001), whereas participants in the other categories saw no significant change.
Linear multilevel regression models for change
Results of the associations between change in psychological distress after rehousing and change in the number of adults (Model A), change in the number of children (Model B), and change in sense of home (Model C) are presented in Table 3 and Fig. 2.
Table 3.
Linear multilevel regression models: effects of change in household number of adults (Model A), household number of children (Model B), and sense of home score (Model C) on change in psychological distress K6 score pre-post rehousinga
| Coeff. γ10b (SEc) Predicted change in K6 score pre-post rehousingd |
Coeff. γ11b (SEc) Predicted difference in change compared to the reference category (interaction)d | |
|---|---|---|
| Model A. Categories defining pre-post change in number of adults per household | ||
| Ref. ≥ 3 adults pre, ≤ 2 adults post | −3.4 (0.7)*** | |
| 1. ≥ 3 adults pre-post | 2.4 (2.0) | |
| 2. ≤ 2 adults pre-post | 3.2 (1.5)* | |
| Model B. Categories defining pre-post change in number of children per household | ||
| Ref. ≥ 3 children pre, ≤ 2 children post | −3.6 (1.1)** | |
| 1. ≥ 3 children pre-post | 0.5 (1.7) | |
| 2. ≤ 2 children pre-post | 2.0 (1.4) | |
| Model C. Categories defining pre-post change in sense of home score — tertiles | ||
| Ref. Lowest pre, mid/highest post | −4.8 (0.9)*** | |
| 1. Lowest pre-post | 1.4 (2.3) | |
| 2. Mid/highest pre-post | 4.4 (1.3)*** |
aAdjusted for sex, age, and region. Separate models were built for (A) the number of adults in the household, (B) the number of children in the household, and (C) the sense of home score
bCoefficients of the fixed effects of γ10TIMEij and γ11(TIMEij × HOUSINGcat.i), see equation in the Methods section
cSE, standard error
dγ10 represents the predicted change in psychological distress K6 score for participants in the reference category; γ11 (interaction) represents the predicted difference between change in K6 scores for a given category, compared to change in K6 scores for the reference category (difference in the magnitude of change between categories)
***p < 0.001; **p ≤ 0.01; *p ≤ 0.05
The reduction in the number of adults per household for the reference category (Table 3 Model A, and Fig. 2A) was associated with a significant decline in psychological distress of 3.4 points between pre and post rehousing (γ10 Table 3, p < 0.001). This change in psychological distress was significantly greater than the estimated change for participants in category 2, by 3.2 points (γ11 Table 3, p = 0.034). Estimated changes in psychological distress for participants in category 1 (−0.7 points, p = 0.890) and category 2 (−0.2 points, p = 0.733) were not statistically significant (see Fig. 2A; not shown in Table 3).
Concerning the number of children in the household (Table 3 Model B, and Fig. 2B), the change in psychological distress estimated for participants in the reference category (γ10 = −3.6 points, p < 0.001) did not significantly differ from the change in other categories (γ11, p > 0.05). As illustrated in Fig. 2B, there were significant or marginally significant declines in psychological distress after rehousing for all categories of the number of children per household.
The increase in the sense of home score for participants in the reference category (Table 3 Model C, and Fig. 2C) was associated with a significant decline in psychological distress of 4.8 points (γ10 Table 3, p < 0.001). This decline was significantly larger than the change estimated for participants in category 2, by 4.4 points (γ11 Table 3, p < 0.001). Estimated changes in psychological distress for participants in category 1 (−3.3 points, p = 0.114) and category 2 (−0.4 points, p = 0.676) did not reach statistical significance (see Fig. 2C; not shown in Table 3).
Discussion
The objective of this article was to assess whether change in the number of adults, change in the number of children, and change in sense of home were associated with a reduction in psychological distress in the context of a rehousing intervention in Nunavut and Nunavik. Among the three housing measures, a decrease in the number of adults and an increase in sense of home were significant predictors of psychological distress decline after rehousing.
Number of adults in the household and psychological distress
The reduction in the number of adults per household experienced by participants in the reference category was associated with a decline in psychological distress from 8.9 to 5.5 points, which likely reflects clinically relevant improvement (Cairney et al., 2007), but not a complete alleviation of distress since the score of 5.5 remains substantially above the mean K6 score for Inuit who were not diagnosed with mood disorders in the 2012 APS (2.9 points) (Statistics Canada, 2015). This reduction in the number of adults is, by definition, accompanied by important household composition modifications. Before rehousing, participants living with 3 adults or more were typically cohabitating with parents, adult siblings, and/or extended family members, often in multigenerational households, and sometimes with homeless people sleeping wherever they find hospitality. For many households, these types of family arrangements correspond to ‘forced overcrowding’ since the severe housing shortage leaves residents of Inuit regions with no other acceptable housing alternatives (Lauster & Tester, 2014; Vink et al., 2014). According to Inuit accounts, overcrowding in this context leads to family conflicts, anger, domestic violence, and depression (Tester, 2006). Study participants in the reference category transitioned into households composed of 1 or 2 adults (living alone, two adults together, or 1–2 parents with their children) after rehousing. In line with the demographics of Inuit regions and with prioritization criteria for public housing allocation, most of them had children, and therefore lived in nuclear family arrangements after the move. The reduction in the number of adults and its association with psychological distress benefits must be interpreted considering the household rearrangements and what they imply in terms of family dynamics. Regarding the apparent preference for the nuclear family model, it has to be acknowledged that household composition choices may be constrained by the dwellings themselves. Typical public housing units still to this day are designed to accommodate Euro-Canadian ways of living, including the nuclear family model (Dawson, 2008).
Number of children in the household and psychological distress
As for the number of children per household, none of the categories defining pre-post change were clearly more beneficial. Post hoc analyses revealed that when the number of children was introduced in the model as a continuous (rather than categorical) variable, its association with psychological distress significantly varied over time (interaction between time and number of children, p = 0.041) (Online Resource, Appendix A). More specifically, while a greater number of children per household was not associated with distress before rehousing, it was marginally associated with lower distress after rehousing (p = 0.088). Similarly, another post hoc analysis showed that being pregnant or having had a baby in the last 12 months was associated with marginally higher distress scores before rehousing (p = 0.055), but with significantly lower distress scores after rehousing (p = 0.016) (Online Resource, Appendix B).
Living conditions before as compared with after rehousing appear to be conducive to a different state of mind with regard to welcoming a new child or living with more children. In Inuit regions, accounts of children temporarily living elsewhere than with their parents due to overcrowding, safety issues, or health concerns have been reported before (Qaqqaq, 2021; Saturviit Inuit Women’s Association of Nunavik and Laneuville, 2015). A study examining Youth Protective Services reports in Canada found that the disproportionate presence of ‘unsafe housing conditions’ and ‘two or more moves in the year prior’ in Indigenous families (including Inuit) significantly contributed to higher rates of case substantiation and/or out-of-home child placement, compared to the case in Caucasian families (Trocmé et al., 2004)1. This is alarming given the central place of children in Inuit culture (NCCAH, 2012) and considering that children were identified as ‘catalysts’ for health promotion (Montgomery-Andersen & Borup, 2012). The idea of a healthy person in the Inuit culture is defined by connections to others (Kirmayer et al., 2009). The birth of a child actively contributes to reinforcing support systems, cooperation, and sentiments of belonging to a caring community. In doing so, it enables processes that are central to the Inuit conceptualization of ‘health’. Our findings align with recently published qualitative findings demonstrating that the domestic environment in which families live impedes (before rehousing) or facilitates (after rehousing) some of these health-promoting processes inherent to the presence of children (Perreault et al., 2022).
Sense of home and psychological distress
Our findings indicate that increase in sense of home is associated with significant decline in psychological distress, from 10.3 to 5.5 points, again likely reflecting clinically relevant improvement (Cairney et al., 2007). After rehousing, a larger proportion of participants agreed with most statements on the sense of home scale; they reported that their new place better reflected themselves, allowed them to have more control over their lives, more privacy, and better family relationships, and overall led to an increased satisfaction with their house (Riva et al., 2020b). Similar findings were observed in the Scottish Housing, Health and Regeneration Project, a controlled rehousing study of 546 households, where gains in psychosocial benefits — similar to our sense of home statements — were associated with mental health improvement (Kearns et al., 2011).
Limitations
Our findings must be interpreted considering some limitations. The absence of a control group means that we cannot exclude the possibility of biased estimates due to unmeasured factors covarying with housing predictors and distress. However, having a control group would have required participants to wait on average 4 years on waitlists while presenting severe housing needs. This process could not be justified for ethical and financial reasons. The study was not sufficiently powered to detect differential rates of change in psychological distress for housing categories including only 7 or 9 participants, or to identify the moderating effect of sex, as observed in other housing intervention studies (Evans et al., 2003). Because of the small sample size, we could not conduct mediation analysis and therefore could not determine whether the increase in sense of home acted as a mediator linking the reduction in number of adults and psychological benefits. An analysis of mediating processes in the context of a housing intervention would bring valuable knowledge to the field of population health intervention research. By design, participants recruited were more likely to benefit from rehousing since they presented relatively high distress scores and severe housing needs at baseline. Therefore, findings cannot be generalized to other Inuit or non-Indigenous populations. Attrition at follow-up is a common limitation in prospective studies. The extent of selection bias was assessed and published elsewhere (Riva et al., 2020a, 2020b). In short, data suggest missing at random loss to follow-up and limited selection bias within the study population.
Conclusion
Our results suggest that by reducing overcrowding and providing housing that is conducive to an increased sense of home for the Inuit, the construction of social housing units across Nunavut and Nunavik could lead to improvements in mental health at a population level. However, in line with the Inuit Nunangat Housing Strategy (ITK, 2019), we argue that an integrated approach to improving socioeconomic outcomes for Inuit is necessary in order to maximize the health benefits associated with improved housing. Food insecurity or low income, for example, are experienced disproportionately by Inuit compared to other Canadians (ITK, 2018) and have both been linked to higher distress among Inuit in Canada (Anderson, 2015; Hajizadeh et al., 2019). Study participants are representative of that economic hardship, and this may partly explain the above-average distress scores after rehousing, even for those who experienced housing improvement. The success of a number of governmental initiatives aiming at socioeconomic and educational advancements in Inuit regions strongly relies on increased investments in housing. For example, the Government of Canada’s “Opportunity for All” poverty reduction strategy, Inuit stream of the Indigenous Skills and Employment Training program, and Inuit Early Learning and Child Care Framework are important for community and individual well-being, yet will only succeed if housing conditions are significantly improved (ITK, 2019).
Contributions to knowledge
What does this study add to existing knowledge?
This study is derived from the first population health rehousing intervention research conducted in Inuit regions.
It demonstrates longitudinal associations between improved housing measures and decline in psychological distress.
It also addresses an important knowledge gap in the literature on housing and mental health by documenting the contribution of sense of home — a notion that encompasses psychosocial processes inherent to the meaningful experience of ‘feeling at home’ — to reducing psychological distress after rehousing.
What are the key implications for public health interventions, practice, or policy?
The rates of household overcrowding in Nunavut and Nunavik are six times the national average in Canada. Our findings indicate that reducing overcrowding in Inuit regions could lead to significant improvement in mental health at the population level.
More specifically, this study suggests that northern housing policies should aim at supplying an increased number of housing units that allow Inuit to form households composed of fewer adults. Consideration should be given to designing housing units that are conducive to gains in control, identity, and other psychosocial processes that lead to an increased sense of home.
Supplementary Information
(DOCX 422 kb)
Acknowledgements
This study was conducted in collaboration with the following organizations: Kativik Municipal Housing Bureau, Kativik Regional Government, Nunavik Regional Board of Health and Social Services, Société d’habitation du Québec, Nunavut Housing Corporation, Government of Nunavut Department of Health, Nunavut Tunngavik Incorporated. The project was approved and supported by mayors of the communities involved, the Nunavik Nutrition and Health Committee, and the Nunavut Research Institute. Results reported in this article have been provided to representatives of the abovementioned partners before their publication. We acknowledge the collaboration of Inuit research assistants, local housing committees and managers, and mayors without whom this study would not have been possible. We thank participants who generously gave their time to participate in the project. We acknowledge the contribution of other co-researchers on this project, and the contribution of research assistants who collected data.
Author contributions
All authors read and approved the final manuscript. KP: substantial contributions to the conception of the article and methodology, data analysis and interpretation, writing — original draft preparation. PD: data collection, creation and maintenance of the database, interpretation of data and statistical support, critical revision for important intellectual content. LP: interpretation of data and critical revision for important intellectual content. MR: substantial contributions to the conception of the article and methodology, interpretation of data, writing — editing and critical revision for important intellectual content, funding acquisition, supervision of the work leading to the article.
Funding
The project Housing, health and well-being in Nunavik and Nunavut was funded by the Institute of Indigenous Peoples Health of the Canadian Institutes of Health Research (Grant #GIR134230) and by ArcticNet, a Network of Centres of Excellence of Canada. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program (CIHR 950-231678) and from the SSHRC-CMHC Partnership Grant At Home in the North (1004-2019-0007). Potvin holds a Canada Research Chair in Community Approaches and Health Inequalities (CIHR 950-232541). Perreault is supported by a Doctoral Research Award from the Canadian Institutes of Health Research.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
The project was approved and supported by mayors of all communities involved, the Nunavik Nutrition and Health Committee, and the Nunavut Research Institute. It received ethical approval from the Comité d’éthique de la recherche du CHU de Québec and from McGill University Internal Review Board.
Consent to participate
All participants provided informed written consent.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
In Trocmé et al. (2004), there was insufficient information to provide stratified estimates by Indigenous identity (Métis, Inuit, and First Nations). Based on 2016 Census data, Caldwell and Sinha (2020) highlighted the important gaps that remain in out-of-home placement rates among Indigenous children, although Inuit-specific data tended to parallel Indigenous national patterns (Caldwell & Sinha, 2020, pp.483 and 485); Caldwell and Sinha (2020) did not examine associations with housing predictors.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anderson, T. (2015). The social determinants of higher mental distress among Inuit. Statistics Canada. Available at: http://www.statcan.gc.ca/pub/89-653-x/89-653-x2015007-eng.htm. Accessed 4 Sept 2022.
- Cairney J, Veldhuizen S, Wade TJ, Kurdyak P, Streiner DL. Evaluation of 2 measures of psychological distress as screeners for depression in the general population. Canadian Journal of Psychiatry-Revue Canadienne De Psychiatrie. 2007;52(2):111–120. doi: 10.1177/070674370705200209. [DOI] [PubMed] [Google Scholar]
- Caldwell J, Sinha V. (Re) Conceptualizing neglect: Considering the overrepresentation of Indigenous children in child welfare systems in Canada. Child Indicators Research. 2020;13(2):481–512. doi: 10.1007/s12187-019-09676-w. [DOI] [Google Scholar]
- Dawson PC. Unfriendly architecture: Using observations of Inuit spatial behavior to design culturally sustaining houses in arctic Canada. Housing Studies. 2008;23(1):111–128. doi: 10.1080/02673030701731258. [DOI] [Google Scholar]
- Evans, G. W., Wells, N. M., & Moch, A. (2003). Housing and mental health: A review of the evidence and a methodological and conceptual critique. Journal of Social Issues, 59(3), 475-500. 10.1111/1540-4560.00074.
- Hajizadeh M, Bombay A, Asada Y. Socioeconomic inequalities in psychological distress and suicidal behaviours among Indigenous peoples living off-reserve in Canada. CMAJ. 2019;191(12):E325–E336. doi: 10.1503/cmaj.181374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen, C. B., Larsen, C. V. L., Bjerregaard, P., & Riva, M. (2020). The effect of household crowding and composition on health in an Inuit cohort in Greenland. Scandinavian Journal of Public Health, 1403494820929496, 10.1177/1403494820929496. [DOI] [PubMed]
- Hayward A, Cidro J, Dutton R, Passey K. A review of health and wellness studies involving Inuit of Manitoba and Nunavut. International Journal of Circumpolar Health. 2020;79(1):1779524. doi: 10.1080/22423982.2020.1779524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ITK. (2018). Inuit Statistical Profile 2018. (pp. 24): Inuit Tapiriit Kanatami. Available at: https://www.itk.ca/2018-inuit-statistical-profile-3/. Accessed 4 Sept 2022.
- ITK. (2019). Inuit Nunangat Housing Strategy. (pp. 32): Inuit Tapiriit Kanatami. Available at: https://www.itk.ca/inuit-nunangat-housing-strategy/. Accessed 4 Sept 2022.
- Kearns A, Whitley E, Mason P, Petticrew M, Hoy C. Material and meaningful homes: Mental health impacts and psychosocial benefits of rehousing to new dwellings. International Journal of Public Health. 2011;56(6):597–607. doi: 10.1007/s00038-011-0275-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kirmayer, L. J., Fletcher, C., & Watt, R. (2009). Chapter 13. Locating the ecocentric self: Inuit concepts of mental health and illness. In L. J. Kirmayer, & G. G. Valaskakis (Eds.), Healing traditions: The mental health of Aboriginal peoples in Canada (pp. 289-314). Vancouver: UBC Press. Available at: https://www.researchgate.net/profile/Laurence_Kirmayer/publication/285757131_Locating_the_ecocentric_self_Inuit_concepts_of_mental_health_and_illness/links/56645d5f08ae418a786d4dc0.pdf. Accessed 4 Sept 2022.
- KMHB. (2014). Directive concerning the allocation of dwelling units in low rental housing in Nunavik. (pp. 10). Nunavik, Québec, Canada: Kativik Municipal Housing Bureau. Available at: https://www.omhkativikmhb.qc.ca/en/housing/eligibility. Accessed 4 Sept 2022.
- Lauster N, Tester F. Culture as a problem in linking material inequality to health: On residential crowding in the Arctic. Health & Place. 2010;16(3):523–530. doi: 10.1016/j.healthplace.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Lauster, N., & Tester, F. (2014). Chapter 4. Homelessness and health in the crowded Canadian Arctic: Inuit experiences. In M. Guirguis-Younger, R. McNeil, & S. W. Hwang (Eds.), Homelessness & health in Canada (pp. 87-109): Les Presses de l’Université d’Ottawa | University of Ottawa Press. Available at: https://www.jstor.org/stable/j.ctt184qqc6.9. Accessed 4 Sept 2022.
- Lévesque, S., & Duhaime, G. (2019). Demographic changes in Nunavik 2006-2016. Nunivaat Analytics (pp. 3). Québec, Canada: Research Chair on Comparative Aboriginal Conditions. Université Laval. Available at: https://www.nunivaat.org/doc/document/2019-11-18-01.pdf. Accessed 4 Sept 2022.
- Minich K, Saudny H, Lennie C, Wood M, Williamson-Bathory L, Cao ZR, et al. Inuit housing and homelessness: Results from the International Polar Year Inuit Health Survey 2007-2008. International Journal of Circumpolar Health. 2011;70(5):520–531. doi: 10.3402/ijch.v70i5.17858. [DOI] [PubMed] [Google Scholar]
- Montgomery-Andersen, R. A., & Borup, I. (2012). Family support and the child as health promoting agent in the Arctic - “The Inuit way”. Rural and Remote Health, 12(2). 10.22605/RRH1977. [PubMed]
- NCCAH. (2012). INUNNGUINIQ: Caring for children the inuit way. Child and youth health (pp. 8): National Collaboration Centre for Aboriginal Health. Available at: https://www.nccih.ca/en/publicationsview.aspx?sortcode=2.8.10.16&id=4. Accessed 4 Sept 2022.
- NCCIH. (2017). Housing as a social determinant of First Nations, Inuit and Métis health. (pp. 16). Prince George, BC, Canada: National Collaboration Centre for Indigenous Health. Available at: https://www.nccih.ca/495/Housing_as_a_social_determinant_for_First_Nations,_Inuit,_and_M%C3%A9tis_health.nccah?id=20. Accessed 4 Sept 2022.
- NHC. (2015). Public Housing and public housing point-rating allocations. (pp. 4): Sent by email on 2 September 2020 by a Nunavut Housing Corporation personnel. NHC website: http://www.nunavuthousing.ca/publichousing. Accessed 4 Sept 2022.
- Nunavut Bureau of Statistics. (2021). Population estimates July 1, 2020. StatsUpdate (pp. 4): Statistics Canada. Available at: https://www.gov.nu.ca/gavamalirijikkut/information/population-data. Accessed 4 Sept 2022.
- Padgett DK. There’s no place like(a) home: Ontological security among persons with serious mental illness in the United States. Social Science and Medicine. 2007;64:1925–1936. doi: 10.1016/j.socscimed.2007.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepin C, Muckle G, Moisan C, Forget-Dubois N, Riva M. Household overcrowding and psychological distress among Nunavik Inuit adolescents: A longitudinal study. International Journal of Circumpolar Health. 2018;77(1):1541395. doi: 10.1080/22423982.2018.1541395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreault K, Riva M, Dufresne P, Fletcher C. Overcrowding and sense of home in the Canadian Arctic. Housing Studies. 2020;35(2):353–375. doi: 10.1080/02673037.2019.1602720. [DOI] [Google Scholar]
- Perreault, K., Lapalme, J., Potvin, L., & Riva, M. (2022). “We’re Home Now”: How a rehousing intervention shapes the mental well-being of Inuit adults in Nunavut, Canada. International Journal of Environmental Research and Public Health, 19(11). 10.3390/ijerph19116432 [DOI] [PMC free article] [PubMed]
- Pierse N, Carter K, Bierre S, Law D, Howden-Chapman P. Examining the role of tenure, household crowding and housing affordability on psychological distress, using longitudinal data. Journal of Epidemiology and Community Health. 2016;70(10):961–966. doi: 10.1136/jech-2015-206716. [DOI] [PubMed] [Google Scholar]
- Qaqqaq, M. (2021). « Sick of waiting » A report on Nunavut’s housing crisis by Mumilaaq Qaqqaq, MP for Nunavut. (pp. 22). Available at: https://fr.scribd.com/document/500305083/Qaqqaq-housingReport-2021#download. Accessed 4 Sept 2022: Nunatsiaq News.
- Riva M, Larsen CV, Bjerregaard P. Household crowding and psychosocial health among Inuit in Greenland. International Journal of Public Health. 2014;59(5):739–748. doi: 10.1007/s00038-014-0599-x. [DOI] [PubMed] [Google Scholar]
- Riva M, Plusquellec P, Juster RP, Laouan-Sidi EA, Abdous B, Lucas M, et al. Household crowding is associated with higher allostatic load among the Inuit. Journal of Epidemiology and Community Health. 2014;68(4):363–369. doi: 10.1136/jech-2013-203270. [DOI] [PubMed] [Google Scholar]
- Riva, M., Fletcher, C., Dufresne, P., Perreault, K., Muckle, G., Potvin, L., et al. (2020a). Relocating to a new or pre-existing social housing unit: Significant health improvements for Inuit adults in Nunavik and Nunavut. Canadian Journal of Public Health, 111(1), 21-30, 10.17269/s41997-019-00249-6. [DOI] [PMC free article] [PubMed]
- Riva M, Perreault K, Dufresne P, Fletcher C, Muckle G, Potvin L, et al. Social housing construction and improvements in housing outcomes for Inuit in Northern Canada. Housing Studies. 2020;36(7):973–993. doi: 10.1080/02673037.2020.1739233. [DOI] [Google Scholar]
- Rolfe S, Garnham L, Godwin J, Anderson I, Seaman P, Donaldson C. Housing as a social determinant of health and wellbeing: Developing an empirically-informed realist theoretical framework. BMC Public Health. 2020;20(1):1138. doi: 10.1186/s12889-020-09224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saturviit Inuit Women’s Association of Nunavik, & Laneuville, P. (2015). Bring hope and restore peace: A study report on the life and concerns of Inuit women of Nunavik. (pp. 171): In partnership with the Community-University Research Alliance Leadership and Governance in Nunavut and Nunavik. Available at: https://www.saturviit.ca/inner-report.php. Accessed 4 Sept 2022.
- Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence (1st ed., pp. 644). Oxford Scholarship Online: Oxford University Press. Available at: https://oxford.universitypressscholarship.com/view/10.1093/acprof:oso/9780195152968.001.0001/acprof-9780195152968. Accessed 1 July 2022.
- Standing Senate Committee on Aboriginal Peoples. (2017). We can do better: Housing in Inuit Nunangat. Report of the Standing Senate Committee on Aboriginal Peoples. Retrieved from: https://publications.gc.ca/site/eng/9.833402/publication.html. Accessed 4 Sept 2022.
- Statistics Canada. (2015). Psychometric properties of the K6 in the 2012 Aboriginal Peoples Survey. Health Analysis Division. Sent by email on 30 March 2021 by a Statistics Canada personnel.
- Statistics Canada. (2017a). The housing conditions of Aboriginal people in Canada. Census in Brief: Available at: http://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016021/98-200-x2016021-eng.pdf. Accessed 6 Oct 2020.
- Statistics Canada. (2017b). Nunavik and Nunavut Census Profile, 2016 Census. For Nunavik: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=HR&Code1=2417&Geo2=PR&Code2=01&SearchText=Nunavik&SearchType=Contains&SearchPR=01&B1=Housing&TABID=1&type=1 [Change geography to obtain Nunavut’s data]. Accessed 18 April 2021.
- Tester, F. (2006). IGLUTAQ (in my room) : The implications of homelessness for Inuit. (pp. 166). Vancouver, Canada: The Harvest Society, Kinngait, Nunavut Territory. Available at: http://www.tunngavik.com/documents/publications/2006-04-00-Iglutaq-The-Implications-of-Homelessness-for-Inuit.pdf. Accessed 4 Sept 2022.
- Thomson H, Thomas S. Developing empirically supported theories of change for housing investment and health. Social Science and Medicine. 2015;124:205–214. doi: 10.1016/j.socscimed.2014.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trocmé N, Knoke D, Blackstock C. Pathways to the overrepresentation of Aboriginal children in Canada’s child welfare system. Social Service Review. 2004;78(4):577–600. doi: 10.1086/424545. [DOI] [Google Scholar]
- Vink, C., Levy, S., Poole, N., Bopp, J. (2014). Profile of homelessness in Nunavut. (pp. 88): Poverty reduction division, Department of Family Services, Government of Nunavut. Available at: https://homelesshub.ca/sites/default/files/Homelessness%20in%20Nunavut%20-%20Engl_0.pdf. Accessed 14 June 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 422 kb)
Data Availability Statement
Not applicable.
Not applicable.