Abstract
Background
The Worldwide Hospice Palliative Care Alliance has recommended integration of palliative care into primary health care. Diminished capacity to provide palliative care is a barrier for integration. The purpose of this study was to screen for palliative care needs in the community.
Methods
A cross-sectional study was conducted in two rural communities of Udupi district. Supportive and Palliative Care Indicators Tool – 4ALL (SPICT-4ALL) was used to identify the palliative care needs. Purposive sampling was used to collect the individual information from the households for identifying the palliative care need. Conditions requiring palliative care and the sociodemographic factors associated with it were explored.
Results
Out of 2041 participants, 51.49% were female, and 19.65% were elderly. Less than a quarter of them (23.08%) had at least one chronic illness. Hypertension, diabetes, and ischemic heart disease were commonly found. 4.31% had satisfied the requisite SPICT criteria, which indicated a need for palliative care. Diseases of cardiovascular system followed by dementia and frailty were the most common conditions requiring palliative care. Univariate analysis showed that age, marital status, years of education, occupation, and the presence of morbidities were significantly associated with the need for palliative care. Being unemployed and having one or more morbidities were factors independently associated with requirement of palliative care.
Conclusions
The estimated palliative care need in the community survey exceeds the perceived need. Although palliative care is traditionally identified with cancer, the proportion of people with noncancer palliative care needs were significantly higher than cancer palliative care.
Keywords: Palliative care needs, Screening, Community, Chronic illness
Introduction
Worldwide, more than 56.8 million people are estimated to require palliative care every year including 31.1 million prior to and 25.7 million near the end of life. A majority (67.1%) of people requiring palliative care are adults over 50 years, and most of them (76%) live in low- and middle-income countries (LMICs) such as India. Although cancer is the most common condition requiring palliative care among adults, 70% of the requirement is mainly for other noncommunicable diseases (NCDs), communicable diseases such as HIV and also for injuries, poisoning, and maternal and child health conditions.1 Rise in NCDs have led to increase in the number of people with prolonged illness and reduced quality of life. Furthermore, improvements in health care have led to an increase in the proportion of elderly with the projections suggesting that 12.17% of the Indian population will constitute of them by 2026.2 The need for palliative care in India is likely to increase with the rise of NCDs and changing population dynamics in the form of increasing elderly population.
As per the quality of death index, India ranked 67th among the 80 countries surveyed, which shows that much can be done to improve the quality of death in the country via palliative care services.3 Despite of palliative care being part of India's plan for “universal health coverage” as per target 3.8 of the Sustainable Development Goals, less than 1% have access to it.4 The district of Udupi with a population of 12 lakhs has a wide network of healthcare facilities. However, palliative care is available only in one tertiary care hospital. There is no baseline information on requirement of palliative care and the conditions requiring the same in this region. Hence, this study was proposed to estimate the palliative care need and its determinants in the district of Udupi.
Material and methods
An approval from the Institutional Ethics Committee was obtained. This community-based cross-sectional study was conducted in the field practice area of two rural health centres of southern India. Both the areas have a combined population of more than 16,000 people among whom nearly half of them are known to have at least one NCD. A sample size of 2041 study participants was arrived at using the sample size calculation formula for cross-sectional studies, that is, n = 4 pq/d2, where the prevalence was taken as 3.04%.5 Purposive sampling was used for collecting data regarding palliative care need among individuals of the community. A house was selected randomly from a point within the locality, and houses were covered in a particular direction consecutively. The same method was followed in all the localities of both the villages till the requisite sample size was attained. A predesigned, semistructured questionnaire was used to collect the sociodemographic data of the participants. The Supportive and Palliative Care Indicators Tool – 4 ALL (SPICT-4ALL) tool was administered by an interviewer to assess the requirement of palliative care among the community.6 Modified BG Prasad Scale was used for socioeconomic status assessment.7 A house-to-house visit was made by a trained eight-member survey team which consisted of faculty, postgraduates, and medical interns. Any household member aged ≥18 years who was willing to provide the necessary information regarding all the family members residing in the household was chosen as a respondent. Health and demographic details of all the family members were collected from the respondent. The respondents were explained about the objectives and purpose of the study and were interviewed after obtaining a written informed consent. Data were collected using Epi Info (version 7) in mobile phones. After collecting the sociodemographic details of all the family members, the general indicators (Part A) as per the SPICT-4ALL tool was assessed, which involved enquiring about any unplanned (emergency) admissions to the hospital, worsening of general health condition, noticeable loss of weight, requirement of a caretaker for help and support, etc. Whereas (Part B) of the tool, which had 22 clinical indicators were asked only if a family member had any of the eight chronic illnesses mentioned in the SPICT tool like cancer, dementia/frailty, nervous system diseases, heart diseases, lung diseases, kidney diseases, liver diseases, and others. An illness lasting for over 3 months was considered as a chronic illness.8 A person was considered to require palliative care if two or more general indicators were satisfied or if they had at least one clinical indicator with or without the presence of general indicators. Data were analysed using Statistical Package for Social Sciences version 15.0 and were summarized as frequencies and percentages. Continuous variables are presented as mean (±standard deviation; SD) or median (interquartile range; IQR) whichever is applicable. Univariate and multivariate regressions were done to assess the association between sociodemographic and other factors affecting the need for palliative care and unadjusted, and adjusted odds ratios (OR) have been expressed with 95% confidence intervals (CI). Factors that were significant on univariate analysis were included in multivariate analysis.
Results
Background characteristics
The study included a total of 2041 individuals from 522 households with a median (IQR) age of 38 years (Q1-22, Q3-55). The proportion of families belonging to nuclear families was higher (42.4%) compared with three generations (31.1%) and joint families (26.5%). As per the modified B.G. Prasad Scale, 78.5% households belonged to middle class. About 68.4% of all respondents had either a government or a private insurance. Of the 401 people above the age of 60 years, 120 (29.9%) of them were pensioners.
Among all the study participants, nearly a quarter of them (23.1%) had one or more chronic illnesses. As shown in Table 1, hypertension, diabetes mellitus, cardiovascular diseases, and neurological disorders accounted for majority (80.8%) of chronic illnesses. Of the 437 respondents who had been availing of treatment for their chronic illness, a majority (95.19%) of them had availed of services from an allopathic practitioner, whereas the remaining sought care from alternative forms of medicine like Ayurveda, Homeopathy, Yoga, and other traditional forms of healing.
Table 1.
Morbidities among the study participants (n = 2041).
| Morbidities | Frequency (%) |
|---|---|
| Hypertension | 273 (13.4) |
| Type 2 diabetes mellitus | 181 (8.9) |
| Cardiovascular diseases | 85 (4.2) |
| Neurological disorders | 62 (3.0) |
| Musculoskeletal diseases | 38 (1.9) |
| Respiratory diseases | 34 (1.7) |
| Thyroid disorders | 20 (0.9) |
| Surgical conditions | 14 (0.7) |
| Renal diseases | 11 (0.5) |
| Cancers | 8 (0.4) |
| Others | 17 (0.8) |
Palliative care need
As per the SPICT criteria, 88 participants (4.31%) of the surveyed population required palliative care. Mean age of participants requiring palliative care was 61.03 years (±20.94). The age of the individuals requiring palliative care ranged from 9 to 94 years. About four individuals below 18 years of age required palliative care as per SPICT criteria. The study found that 64.8% of the people who required palliative care were ≥60 years of age, 51.2% were female, 53.4% were married, 57.9% had received 5–12 years of schooling, 43.2% were unemployed, 50% belonged to nuclear family, and 71.6% were from middle socioeconomic status.
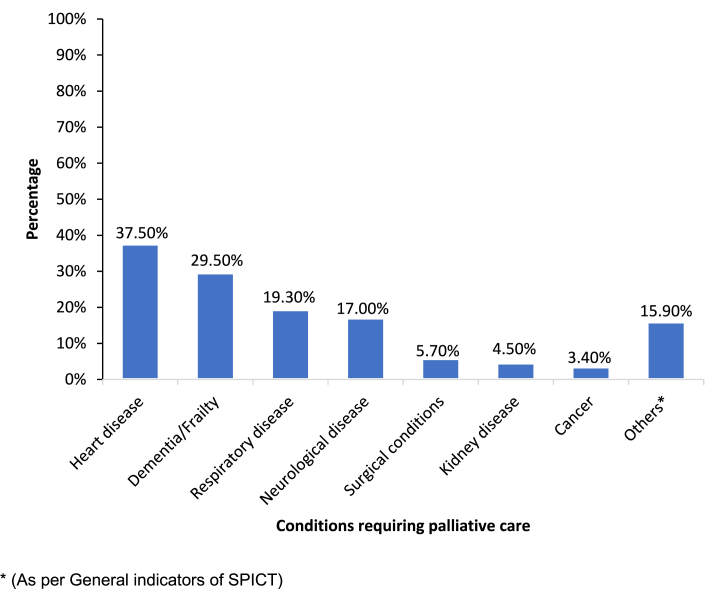
It was found that heart disease (37.5%), dementia/frailty (29.5%), and respiratory diseases (19.3%) were the three most common conditions requiring palliative care as shown in Fig. 1. Only 3.4% of those requiring palliative care had cancer. It was observed that 22.7% of the participants requiring palliative care were below 45 years of age. In these individuals, the conditions requiring palliative care were neurological diseases, respiratory diseases, cardiac diseases, kidney diseases, liver disease, and cancer in that order.
Fig. 1.
Conditions that required palliative care as per the SPICT criteria (n = 88).
As shown in Table 2, on univariate analysis, age, marital status, literacy, occupation, and number of morbidities were found to be significantly associated with the requirement of palliative care. However, on multivariate analysis, being unemployed [AOR = 5.93; 95% CI:2.61–13.49, p < 0.001] and having one morbidity [AOR = 33.84; 95% CI:11.38–100.60, p < 0.001] or more than one morbidity [AOR = 170.88; 95% CI:56.13–520.20, p < 0.001] were significantly associated with palliative care requirement.
Table 2.
Association of sociodemographic characteristics and morbidities with the requirement of palliative care.
| Characteristics | Categories | Requires Palliative Care n (%) n = 88 |
Does not require palliative care n (%) n = 1953 |
Total n=2041 | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|---|---|---|---|
| Unadjusted OR (95%CI) | p-value | Adjusted OR (95%CI) | p-value | |||||
| Age in years | ≤45 | 20 (22.7) | 1275 (65.3) | 453 | 1 | 1 | ||
| 46–59 | 11 (12.5) | 334 (17.1) | 1187 | 2.10 (0.10–4.43) | 0.05 | 0.52 (0.20–1.32) | 0.17 | |
| ≥60 | 57 (64.8) | 344(17.6) | 401 | 10.56 (6.26–17.82) | <0.001 | 0.62 (0.27–1.42) | 0.26 | |
| Gender | Male | 37 (42) | 953 (48.8) | 990 | 1 | |||
| Female | 51 (58) | 1000 (51.2) | 1051 | 1.31 (0.85–2.02) | 0.22 | |||
| Marital status | Married | 47 (53.4) | 1059 (54.2) | 1106 | 2.72 (1.43–5.17) | <0.01 | 0.76 (0.23–2.57) | 0.66 |
| Unmarried | 12 (13.6) | 736 (37.7) | 748 | 1 | 1 | |||
| Widowed/divorced/separated | 29 (33) | 158 (8.1) | 187 | 11.26 (5.62–22.54) | <0.001 | 0.41 (0.14–1.19) | 0.10 | |
| Years of education | <5 years | 24 (27.3) | 278 (14.2) | 302 | 2.55 (1.28–5.10) | 0.01 | 0.88 (0.35–2.17) | 0.78 |
| 5–12 years | 51 (57.9) | 1291(66.1) | 1342 | 1.17 (0.63–2.17) | 0.63 | 0.55 (0.25–1.18) | 0.12 | |
| >12 years | 13 (14.8) | 384 (19.7) | 397 | 1 | 1 | |||
| Occupation | Homemaker | 33 (37.5) | 542 (27.8) | 575 | 4.08 (2.05–7.85) | <0.001 | 2.04 (0.91–4.55) | 0.06 |
| Employed | 12 (13.6) | 792 (40.6) | 804 | 1 | 1 | |||
| Unemployed | 38 (43.2) | 129 (6.6) | 167 | 19.44 (9.89–38.19) | <0.001 | 5.93 (2.61–13.49) | <0.001 | |
| Children/students | 5 (5.7) | 495 (25.1) | 495 | 0.67 (0.23–1.92) | 0.46 | 1.26 (0.31–5.19) | 0.75 | |
| Type of family | Joint | 25(28.4) | 515(26.4) | 540 | 1 | |||
| Nuclear | 44(50) | 822(42.1) | 866 | 1.10 (0.67–1.82) | 0.70 | |||
| Three generation | 19(21.6) | 616(31.5) | 635 | 0.64 (0.35–1.17) | 0.14 | |||
| Socioeconomic status | Upper class | 14 (15.9) | 250 (12.8) | 264 | 1 | |||
| Middle class | 63 (71.6) | 1540 (78.9) | 1603 | 0.73 (0.40–1.32) | 0.30 | |||
| Lower class | 11 (12.5) | 163 (8.3) | 174 | 1.21 (0.53–2.72) | 0.65 | |||
| Number of morbidities | 0 | 5 (5.7) | 1565 (80.1) | 1570 | 1 | 1 | ||
| 1 | 24 (27.3) | 256 (13.1) | 280 | 29.34 (11.09–77.60) | <0.001 | 33.84 (11.38–100.60) | <0.001 | |
| ≥1 | 59 (67) | 132 (6.8) | 191 | 139.90 (55.19–354.59) | <0.001 |
170.88 (56.13–520.20) <0.001 |
||
Bold = Statistically significant.
Discussion
Our study found that 4.31% of the study population required palliative care, whereas studies from urban Puducherry by Daya et al, and rural Tamilnadu by Elayaperumal et al, in India reported the need for palliative care to be only 0.61% and 0.45%, respectively.9,10 The present study has used SPICT, a detailed evaluation tool including seven general indicators and eight disease-specific indicators, which could identify a higher proportion of people requiring palliative care, whereas the above mentioned studies used fewer criteria such as people being bed ridden, ability to go to work and requirement of assistance for daily activities. However, a hospital-based study from Puducherry found that 10.1% of inpatients and outpatients required palliative care as per the need assessment tool for progressive disease. These patients were being treated in the departments of neurology, cardiology, and nephrology.11 The greater need for palliative care in this study could be due to hospital-based nature of the study. A study from rural Nepal found that 3.04% required palliative care according to SPICT criteria, which is similar to our study findings.5 Another cross-national study included 12 European and non-European countries in which death registration data were used to show that the need for palliative care among those who died ranged from 38% to 74%.12 A study done in Ireland by Kane et al, found that, between 2007 and 2011, nearly 80% of the people died of conditions, which needed palliative care.13 Similarly, in England, it was observed that palliative care was needed by almost two-thirds (63%) of the individuals who had died during the years 2006–2008.14 The palliative care need differs from country to country depending on sociodemographic framework like increasing elderly population and income levels. It is also influenced by higher burden of health conditions like cancer and other NCDs.13 As the questionnaires and methods used in various studies are different, comparison of palliative care need across countries is difficult (Table 3). Studies have shown that many of these needs can be met by increasing government support via dedicated funding for palliative care and by implementing specific programs through the existing health infrastructure.1
Table 3.
Requirement of palliative care as assessed by different studies.
| Author | Year | Study setting | Study design | Study tool | Study population | Sample size | Percentage of study participants requiring palliative care |
|---|---|---|---|---|---|---|---|
| Morin L et al. | 2011 | 12-country, multicentric study | Retrospective death record based | Death registration data | People who have expired | 4,908,114 | 38%–74% |
| Daya AP et al. | 2013 | Puducherry, India, Community based | Observational | Questionnaire | General population | 3554 | 0.61% |
| Prasad P et al. | 2015 | Puducherry, India, hospital based | Observational | Questionnaire(Need Assessment Tool for Progressive Disease) | Hospital patients | 458 | 10.1% |
| Kane PM et al. | 2015 | Ireland | Retrospective death record based | Death registration data | People who have expired | 141,807 | 80% |
| Elayaperumal S et al. | 2016 | Tamil Nadu, India, community based | Observational | Questionnaire | General population | 7493 | 0.45% |
| Acharya PK et al. | 2017 | Makwanpur, Nepal, community based | Observational | SPICT | General population | 2168 | 3.04% |
The present study found that heart diseases and dementia/frailty were the most common conditions requiring palliative care, and this is in agreement with that of a study from urban Puducherry in which age-related weakness (41%) and heart diseases (18.5%) were the predominant conditions requiring palliative care.9 Similarly, chronic respiratory disease (51.5%), dementia and frailty (30.3%), heart diseases (22.2%) and diseases of the nervous system (22.2%) were the common conditions requiring palliative care as reported in a study from Nepal. The study also found that only three study participants with cancer required palliative care which is in parallel to our study findings.5 Although the study from rural Tamil Nadu by Elayaperumal et al, reported the most common condition requiring palliative care to be old age–related weakness (41.2%), which is akin to our study, the second most common condition in their study was found to be stroke (20.6%).10 In Ireland and Australia, the conditions potentially requiring palliative care were cancer, heart disease, renal disease, respiratory disease, liver disease, neurological disease, dementia and HIV/AIDS with cancer, heart disease, and respiratory disease accounting for majority of the deaths.13,15 It was also seen in the present study that more the burden of morbidities are, higher were the odds of requiring palliative care. Multiple morbidities leads to increased physical, mental, social, spiritual, and emotional suffering. This is a cause of serious health related suffering and hence warrants palliative care.16
In the present study, age was not found to be independently associated with the requirement of palliative care. This may be attributed to the near-equal distribution of morbidities among those who were below and above 60 years of age. However, the studies by Acharya et al, from Nepal and Daya et al, and Elayaperumal et al, from India found that majority of those who required palliative care are more than 60 years of age.5,9,10 A predominance of female gender was observed in the need for palliative care among various studies (Nepal, urban Puducherry), which corroborates with our study findings.5,9 In the present study, palliative care requirement was higher among those from nuclear families (50%), which is in line with the prior research done in Tamil Nadu by Elayaperumal et al, where majority (79.4%) of the people requiring palliative care belonged to nuclear families.10 However, in the Puducherry study, it was seen that more number of people requiring palliative care were in joint families.9 It was seen in our study that participants who were, unemployed [AOR = 5.93; 95% CI: 2.61–13.49, p < 0.001] were at higher odds of requiring palliative care, which supports the previous findings from Puducherry.9 In our study, the participants with less education, lower socioeconomic status, and reduced support from the extended family had higher palliative care needs. However, these associations were not statistically significant.
This is a first of its kind study in this region assessing the palliative care need using a standardized tool in a community setting. As the study was done in an area with high literacy rate and good health system indicators compared with other parts of the state and country, the results of the study could be extrapolated only to similar settings in the country.
Conclusion
The need for palliative care among the surveyed population was higher compared with other studies from India. Although palliative care is traditionally identified with cancer, the proportion of people with noncancer palliative care needs were significantly higher than cancer palliative care. The results of the study can be used for planning and implementation of community-based palliative care services in this region. Considering the large need for palliative care services in this community, efforts should be made to integrate palliative care services within primary health care settings.
Disclosure of competing interest
The authors have none to declare.
Acknowledgments
We sincerely thank our field workers affiliated to the peripheral health centres of Kasturba Medical College, Manipal, who ensured that the process of data collection went smoothly in the community. We thank all the participants for agreeing to spend their valuable time for the purpose of this study.
References
- 1.Global Atlas of Palliative Care. 2nd ed. 2020. http://www.thewhpca.org/resources/global-atlas-on-end-of-life-care [Internet]. [cited 2021 Jan 30]. Available from: [Google Scholar]
- 2.Office CS . 2011. Implementation M of S& P, India G of. Situation Analysis of the Elderly in India.https://www.researchgate.net/publication/274093346_Association_of_Systemic_Diseases_with_Cutaneous_Dermatosis_in_Elderly_Population_Preliminary_Observation_at_a_Rural_Tertiary_Care_Centre/fulltext/55dbd61b08ae9d6594936bc6/Association-of-Systemic-Diseases- [Internet] [cited 2021 Jan 30]. Available from: [Google Scholar]
- 3.The 2015 Quality of Death Index Ranking Palliative Care across the World. 2015. [Google Scholar]
- 4.The current status of palliative care in India | Cancer Control [Internet]. [cited 2021 Mar 1]. Available from: http://www.cancercontrol.info/cc2015/the-current-status-of-palliative-care-in-india/.
- 5.Acharya P.K., Baral K., Munday D., Gongal R.N. Population based need assessment of palliative care in rural Nepal. J Patan Acad Heal Sci. 2017 Nov 15;4(2):21–26. https://www.nepjol.info/index.php/JPAHS/article/view/24580 [Internet].[cited 2021 Jan 30]. Available from: [Google Scholar]
- 6.The University of Edinburgh. SPICT-4ALLTM – SPICT [Internet]. [cited 2019 Jan 28]. Available from: https://www.spict.org.uk/the-spict/spict-4all/.
- 7.Mathiyalagen P., Davis P., Sarasveni M. Updated BG Prasad socio-economic classification: the 2020 update. Indian J Pediatr. 2020:1–2. doi: 10.1007/s12098-020-03362-4. [Internet]. Springer; [cited 2020 Dec 1]. Available from: [DOI] [PubMed] [Google Scholar]
- 8.Bernell S., Howard S.W. Use your words carefully: what is a chronic disease? Front Public Heal. 2016;4(August):2–4. doi: 10.3389/fpubh.2016.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daya Ap, Sarkar S., Kar S. Estimation of palliative care need in the urban community of Puducherry. Indian J Palliat Care. 2017;23(1):81–87. doi: 10.4103/0973-1075.197959. http://www.jpalliativecare.com/text.asp?2017/23/1/81/197959 [Internet]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elayaperumal S., Venugopal V., Dongre A. Identifying people in need of palliative care services in rural Tamil Nadu: a survey. Indian J Palliat Care. 2018 Oct 1;24(4):393. doi: 10.4103/IJPC.IJPC_92_18. http://www.jpalliativecare.com/text.asp?2018/24/4/393/243299 [Internet] [cited 2021 Jan 30]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prasad P., Sarkar S., Dubashi B., Adinarayanan S. Estimation of need for palliative care among noncancer patients attending a tertiary care hospital. Indian J Palliat Care. 2017 Oct 1;23(4):403–408. doi: 10.4103/IJPC.IJPC_90_17. https://www.jpalliativecare.com/article.asp?issn=0973-1075;year=2017;volume=23;issue=4;spage=403;epage=408;aulast=Prasad [Internet] [cited 2021 May 26]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morin L., Aubry R., Frova L., et al. Estimating the need for palliative care at the population level: a cross-national study in 12 countries. Palliat Med. 2017 Jun 1;31(6):526–536. doi: 10.1177/0269216316671280. http://journals.sagepub.com/doi/10.1177/0269216316671280 [Internet] [cited 2021 Jan 30]. Available from: [DOI] [PubMed] [Google Scholar]
- 13.Kane P.M., Daveson B.A., Ryan K., McQuillan R., Higginson I.J., Murtagh F.E.M. The need for palliative care in Ireland: a population-based estimate of palliative care using routine mortality data, inclusive of nonmalignant conditions. J Pain Symptom Manag. 2015 Apr 1;49(4):726–733.e1. doi: 10.1016/j.jpainsymman.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Murtagh F.E.M., Bausewein C., Verne J., Iris Groeneveld E., Kaloki Y.E., Higginson I.J. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med. 2014 Jan 21;28(1):49–58. doi: 10.1177/0269216313489367. http://journals.sagepub.com/doi/10.1177/0269216313489367 [Internet] [cited 2021 Jan 30]. Available from: [DOI] [PubMed] [Google Scholar]
- 15.Rosenwax L.K., McNamara B., Blackmore A.M., Holman C.D.J. Estimating the size of a potential palliative care population. Palliat Med. 2005 Oct 1;19(7):556–562. doi: 10.1191/0269216305pm1067oa. http://journals.sagepub.com/doi/10.1191/0269216305pm1067oa [Internet] [cited 2021 Jan 30]. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Radbruch L., De Lima L., Knaul F., et al. Redefining palliative care—a new consensus-based definition. J Pain Symptom Manag. 2020 Oct 1;60(4):754–764. doi: 10.1016/j.jpainsymman.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]