Abstract
While there is an evolving literature on the benefits of texting and patient-centered technologies, texting initiatives have not focused on family members. We sought to identify patients’ family members’ perspectives on facilitators and barriers to using 1 digital texting innovation to promote family-centered care during patients’ hospitalizations. This qualitative study was conducted at a tertiary care center in Houston, consisting of 7 hospitals (1 academic hospital and 6 community hospitals), involving analyzation of 3137 comments from family members who used the digital texting technology. Thematic analysis methods were used. The data analysis for loved ones’ feedback resulted in 4 themes as facilitators: (1) inpatient text messaging keeps loved ones updated and connected (n = 611); (2) inpatient text messaging allows for stronger continuity of communication (n = 69); (3) messaging promotes a sense of staff compassion and service (n = 245); and (4) messaging reduces phone calls (n = 65). The data analysis resulted in 4 themes as barriers to text messaging helpfulness: (1) messages could feel generic (n = 31); (2) inpatient texting was not needed if all loved ones were regularly at bedside (n = 6); (3) messages could have a perceived delay (n = 37); and (4) security features could impact convenience (n = 29). Our findings indicate that family members and loved ones value inpatient text messages, not only for the information the messages provide, but also because the act of writing text messages and preparing loved ones shows inclusiveness, compassion, and family-centered care.
Keywords: patient experience, family-centered care, mHealth technology, digital innovations, patient engagement, quality improvement
Introduction
Families’ perceptions of care influence patients’ experiences (1–4). Empirically, families play an integral role in caregiving, having been associated with impacts on patients’ mortality, morbidity, and readmissions (5,6). Despite this recognition that families are important contributors to patients’ care, family-centered care is given little attention in the literature.
Specifically, family-centered care is clumped with “patient-centered care,” presupposing that family-centered care can be equated to patient-centered care, without entertaining the possibility that family-centered care may be a different construct. Consider this: The Agency for Healthcare Research and Quality (AHRQ) hosts patient and family engagement modules. Each e-module contains the words “patient and family.” Yet none of the e-modules consider patients and families separately—what the patients’ information and communication needs are and how those needs might be different from their families (7). It is as though families should be given equal decision-making authority to that of patients and equal access to information and communication with clinicians.
The purpose of this article is to describe families’ experiences with 1 digital texting innovation we created to enhance family-centered care during patients’ inpatient stays. The gap we sought to address is this: When patients have the capacity, clinicians justifiably focus their attention on communicating with hospitalized patients, with the hopes that patients will communicate directly with their family members and loved ones to keep them updated. Yet, patients and their families may want or expect clinicians will update patients’ loved ones. Patients may not feel well and may not be in an optimal position to keep their loved ones updated while hospitalized, or the patient may relay information inaccurately from what was communicated by the provider. The question then becomes: Can providers keep family members accurately updated through texting while giving decisional authority to the patient?
There is a robust body of literature that has evolved over the past few years highlighting the importance of text-based research in the context of patient-centered technologies. Most of this work has demonstrated that texting is promising and efficacious in improving patient adherence and knowledge for smoking cessation, diabetes-related knowledge, postpartum care, cardiovascular and chronic respiratory disease management, mental health management, cancer-related knowledge, and more recently, COVID-19 follow-up monitoring and support (8–11). But, to our knowledge, most of the text-based researches has been focused on patients and only in the post-discharge setting. Where texting has been considered in the context of caregivers or family members, the research has focused exclusively on caregivers of pediatric or adolescent patients or patients with cancer and chronic illness living at home and requiring caregiver support (12–14). Texting initiatives have not focused on updating family members during adult patients’ hospitalizations.
In developing our texting innovation, we hypothesized that a unidirectional texting platform would meet families’ information needs. To our knowledge, this is the first qualitative study on families’ and loved ones’ experiences with a digital technology designed to keep them updated during admission; one of only a few empirical studies on family-centered care, and the first to study barriers and facilitators to inpatient texting.
Methods
Setting and participants: This study was conducted at the Houston Methodist Hospital System—a 2264-bed academic medical center located in Houston, Texas, along with 6 affiliated community hospitals (178-650 beds) in the suburbs. The Hospital Institutional Review Board waived this study.
The study was conducted between February 2022 and June 2022 and involved 2 information technology contractors: (1) Epic (the electronic medical record system) and (2) CareSense, a vendor we use to send text messages to patients and families in a secure, encrypted, password-protected format. CareSense is integrated with Epic.
Design Phase
First, to help inform the development of the digital texting innovation, we conducted a content analysis of comments provided in our HCAHPS survey.15 A total of 314 patient comments over a 2-year period were reviewed. Results from this analysis suggested 2 prominent areas of opportunity to enhance family-centered care: (1) more frequent updates to loved ones and (2) more unified messaging from the clinical team to patients and families.
Second, based on the content analysis, we drafted a smart form template within the Epic electronic health record (EHR) where clinicians could write a text update to the family. Third, we brought the mock up templates to 3 different hospitalist meetings and nurse leadership meetings to assess usability, formatting, and accessibility. In soliciting feedback, we used a focus group methodology, because the interaction among different users would allow for rich exploration of themes. (9) During these meetings, we used a semi-structured moderator guide to explore whether the mock up would fit with clinicians’ workflow and styles.
Finally, we revised and then sent the template to 10 clinicians to confirm the revisions were consistent with their feedback. After revising again, survey builders required 1 month to build and test.
Implementation Phase
Setting and participants: All English-speaking and Spanish-speaking patients with decision-making capacity accessing any of our emergency departments or perioperative registration offices were asked whether they have family members or loved ones they would like to receive healthcare updates if they should become admitted. If so, the registration staff entered loved ones’ names and cell numbers in the EHR. Participants were mainly medical patients with decisional capacity, having chronic cardiovascular or respiratory illnesses on medical nursing floors. There were some elective orthopedic surgery patients and some patients within the medical and cardiovascular intensive care units. Our companion article on clinician perspectives describes the breakdown between units.
The enrolled loved ones received text messages in their preferred language (English or Spanish), and they could accept or decline them with no bearing on the patients’ care. The messages were embedded behind a secure, encrypted, HIPAA-complaint link.
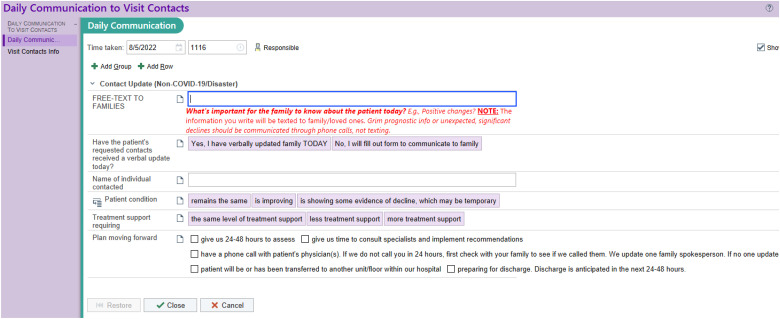
Smart form template: The smart form template allowing clinicians to enter a text message was the same for both physicians and nurses. The form was put within the Epic navigator tab for physicians and Epic flowsheets for nurses. Its features can be found in Figure 1. If 1 field was completed (whether close-ended select buttons or a free-text field) within the Epic smart form, we sent the text message.
Figure 1.
Smart form template.
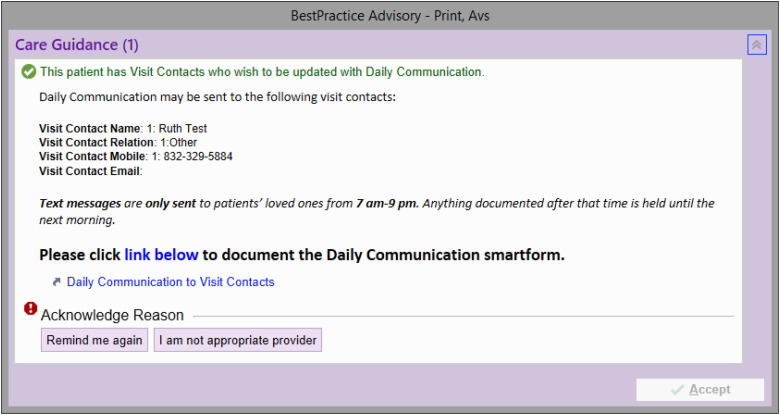
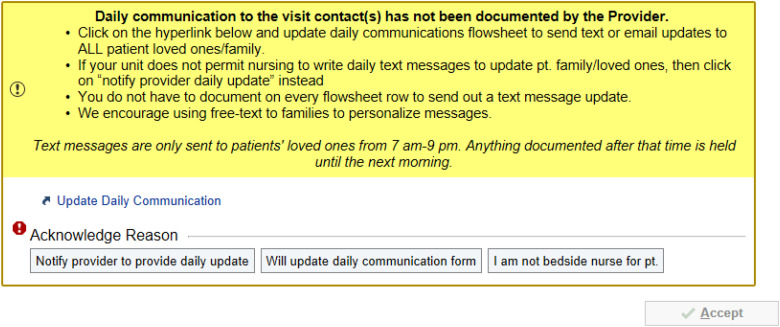
Best practice alerts (BPAs) inside of Epic: We programmed an automatic BPA or clinical decision support alert to prompt providers when the total time a patient is in Observation and/or Inpatient exceeds 24 h and no documentation occurred that day or the previous evening (Figure 2). The primary goal was to have the providers text, and have nursing serve as a back up to providers. Nursing had a similar alert but a different decision logic (Figure 3).
Figure 2.
Best practice alerts (BPAs) inside of Epic for providers.
Figure 3.
Best practice alerts (BPAs) inside of Epic for nurses.
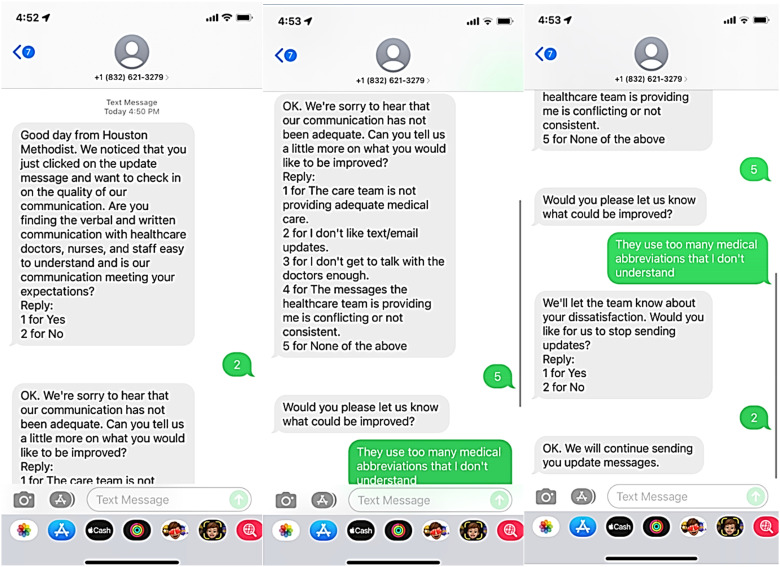
Service recovery escalation: Text messages were primarily unidirectional in that clinicians sent text messages on the patient's health status to loved ones without the ability for loved ones to write clinicians back.
We had 1 bidirectional component: Every 3 days of the patient's admission, we asked loved ones whether they were satisfied with communication and care. If dissatisfied, they would then be asked to select the nature of their dissatisfaction, with 4 options as shown in Figure 4. Where loved ones were dissatisfied, an alert was automatically generated and emailed to unit leadership. The staff would then proactively engage in service recovery. The results of this service recovery escalation process are discussed in the companion piece on clinicians’ perspectives.
Figure 4.
Bidirectional text soliciting family feedback on dissatisfaction.
Post-Implementation Phase
At the end of the patient's hospitalization, loved ones were asked to reflect on whether they liked the digital texting innovation, using a 5-point Likert Scale on its “helpfulness.” After providing a response, they were prompted to provide their scoring rationale in a free-text field, what they liked or what they wanted to be improved. These free-texts responses were used to conduct a thematic analysis during the post-implementation phase. These responses are reported below in the “Results” section.
Additionally, post-implementation, we met with hospitalists and nurse leaders to solicit feedback, using focus group methodology to identify how we could make enhancements (16–20). Those enhancements are discussed in the companion article.
We also performed enhanced education to clinicians in late April 2022 on the automatic messages and value of personalized text messages. Finally, post-implementation, we built real-time reports to aid us in scale-up and sustainment effort.
Data Analysis
We performed an analysis of the family comments using thematic analysis. Thematic analysis involves identifying key themes that emerge as the theory is formed—information needs and decision-making preferences—based on recurring statements (10). Coding involves giving conceptual labels to data, each generating new emergent codes, and later comparing until there is consensus (16).
We used a codebook to assist us in identifying themes and reached a consensus by achieving theoretical saturation—the point in data collection when no additional insights emerge. Emergent patterns and themes were stored electronically (17) to provide analytical depth.
The analysis followed an inductive approach, allowing themes from open-ended questions to emerge with minimal a priori assumptions on content. Questions centered on facilitators and barriers, and analysts were instructed to code in keeping with the SEIPS model (person, task, environment, organization, and/or technology and tools). This framework facilitates actionable findings in healthcare (18).
Results
Eighty-five percent of families approached agreed to participate. Our sample of family members approximated internal demographic trends. Specifically, our patient population is 9.6% (0-18 years old), 26.9% (18-40 years old), 34.2% (40-65), and 28.8% (65 and older). Most patients are female (54.5% are female; 44.8% are male). While we did not ask family members to reflect on their ethnicity, it likely approximates the patient population, consisting of 14.4% Hispanic or Latino; 52.5% Caucasian; 14.2% Black; and 4.6% Asian.
There were 3137 loved ones’ responses to the question on whether text messages were helpful, which served as the primary source of our analysis for loved ones’ perspectives. The comments were from different patients’ families. In the February 2022 to April 2022 period, there were 2030 responses. The remaining 1097 responses were completed between May and June 2022. All but 23 patients completed both the Likert question and a free-text comment explaining their scoring.
In the February to April period, the Likert score results indicated that 66% of loved ones responded with “strongly agree” on whether they found texting helpful. Another 22% and 6% indicated “agree” or “undecided,” respectively, to helpfulness. Finally, 3% indicated “disagree” and 3% indicated “strongly disagree.”
After April revisions, the Likert scores increased. In the April to June period, the Likert score results indicated that 71% of loved ones responded with “strongly agree” to texting helpfulness. Another 22% and 5% indicated “agree” or “undecided,” respectively, to helpfulness. Finally, 1% indicated “disagree” and 1% indicated “strongly disagree.”
In what follows, we arrange the themes by loved ones’ perspectives. We outline facilitators and barriers to texting.
Text Messaging Facilitators
The data analysis for the loved ones’ feedback resulted in 4 positive emerging themes as facilitators (Table 1), the first 3 of which focused on how texting promoted emotional connectedness and value-added conveniences from a family perspective—how it made them feel as a family and how it made communicating more convenient. A less prominent theme focused on how it positively impacted their own workflow and practices as a family in reducing the number of calls they made to the units. The families also positively reflected on the usability and accessibility of texting.
Theme 1: Inpatient text messaging keeps loved ones updated and connected.
Table 1.
Summary Table of Themes and Prevalence.
| Facilitators | Subthemes | Impact or result | Prevalence of theme |
| Inpatient text messaging keeps loved ones updated and connected |
|
n = 611 (19%) | |
| Inpatient text messaging allows for stronger continuity of communication |
|
n = 69 (2%) | |
| Messaging promotes a sense of staff compassion and service |
|
n = 245 (7.8%) | |
| Messaging reduces phone calls |
|
n = 65 (2%) | |
| Barriers | Messages could feel generic or redundant |
|
n = 31 (1%) |
| Inpatient texting was not needed if all loved ones were regularly at bedside |
|
n = 6 (<1%) | |
| Messages could have a perceived delay |
|
n = 31 (1%) | |
| Security features could impact convenience and accessibility |
|
n = 29 (<1%) |
The most prominent theme is that loved ones feel that text messaging allows them to stay informed and that, in turn, reduces their anxiety. This theme surfaced in at least 611 (19%) responses. Other loved ones mentioned that they were comfortable leaving the bedside: “This is the first time in 12 years I felt comfortable going home and sleeping while she was in the hospital.” Families could still feel connected, “I liked that the texts make us feel like there's a connection with our loved ones, even when we can’t be there at the hospital.” The word “connection” appeared 115 times.
Loved ones liked being able to leave the bedside to do errands, as mentioned by this patient: “Text messages allowed me to get home for lunch and let the dog out;” and this family member: “Texts kept me up to date so I could know what was going on while still juggling daily life (kids, work). If not for the updates, I would have to find a sitter and miss work.”
Theme 2: Inpatient text messaging allows for stronger continuity of communication.
Since our texts went to all loved ones listed in the EHR, loved ones could be updated at the same time. Several loved ones mentioned that this feature allowed the extended family to feel up to date at the same time: “Some family members are 4+ hours from Houston, so we could all stay in contact,” and, as another loved one wrote, “All of us want to know. We’re a big family.”
Additionally, some loved ones mentioned how much this feature lifted the burden and responsibility from the patient or from the key family spokesperson or surrogate decision maker in having to keep the family informed. As loved ones wrote, “[The patient] was so tired. He was relieved he didn’t need to keep calling all of us [to keep us updated];” and “I liked how I could just focus [on the patient] and not have to be on the phone constantly with other family to keep them updated.”
Theme 3: Inpatient text messaging promotes a sense of staff compassion and service.
The words “care,” “compassion,” or “service” were mentioned 245 times (7.8%). The act of communicating through text showed caring and a desire for connection, as exemplified by this family, “I really appreciated the updates on what to expect. We also very much appreciated the feeling of importance when you do this.” Even where the families did not benefit from the messages, they referenced the feeling of caring and connection: “You treated me and my husband…like he was not just another person.”
Theme 4: Inpatient text messaging reduces phone calls.
Thirty loved ones reported calling the unit less because they were kept informed: “I didn’t feel the need to bug the nurse and doctors.” They also reported liking that they did not need to call and “be put on hold forever or transferred to Never-Never Land.”
Spanish-preferred loved ones wrote that they liked having the message in writing because they felt less comfortable talking to someone over the phone. This theme was explicitly mentioned (in Spanish writing) by 4 Spanish-preferred loved ones.
Text Messaging Barriers
The data analysis for the loved ones’ feedback resulted in 4 emerging themes as negative barriers (Table 1). Three of the themes related to barriers focused on how clinicians used the technology and how, if clinicians used texting improperly or without intention and purpose, the text messages could do more emotional harm than good for families. The final theme on security related to usability and accessibility of texting and how security undermined conveniences.
Theme 1: Messages could feel generic or redundant.
The most prominent theme for barriers to texting was that clinicians had the option of clicking a button to provide an update without the use of personalized free-text messages, which felt generic and repetitive to loved ones: “What would have been helpful would have been a summary of doctor's notes from their rounds. Instead, it seemed very robotic and repetitive.” The “generic,” “impersonal,” “repetition” or “hurriedness” of canned, scripted messages surfaced in 31 responses.
Sometimes, clinicians would use free texts to write the nurse's name, contact information, and visiting hours without giving additional clinical information, which loved ones found dissatisfying: “The name of my loved ones’ nurse isn't a very informative piece of information.”
Theme 2: Inpatient texting was not needed if all loved ones were regularly at bedside.
A few family members mentioned that, if they were at the bedside regularly and during rounding, they did not benefit from the texted information, as described by this loved one: “I was beside all the time, so [I] knew most of the information provided already. For someone unable to be bedside, would be very helpful.” In every case where this was mentioned, the loved one scored the messaging very high on the Likert scale regardless.
Theme 3: Messages could have a perceived delay.
At least 37 loved ones indicated they thought there was a delay in the messages, even though there was no technical delay in any. If clinicians waited until the end of their shift to write the text message (after talking to family), this information felt outdated, “Waiting until 6 pm to write about a procedure…is compliance for numbers sake.” If clinicians did not document every day, loved ones would report a delay or gap in the messages: “only got one update from doc in a 9-day period.” Finally, for clinicians who documented after 9 pm, loved ones would report feeling as though the information was outdated: “This message said ‘today,’ but I can tell it was from yesterday.”
Theme 4: Security features could impact convenience and accessibility.
In the February to April period, 14 family members commented on the “convenience” and “easy access.” In the May to June period, 11 family members commented on the “convenience”. Once we added the requirement to enter the patient's birth year to see the update, a few loved ones commented that the “added security” was “not needed” or “felt unnecessary,” particularly since the patient had “already provided permission” for texting.
Discussion
We found that family engagement and communication are essential to family-driven care and can be achieved through texting. The findings indicate that family members and loved ones value inpatient text messages, not only for the information the messages provide, but also for the inclusivity and compassion the texts offer.
Based on these findings, it might be ill-advised to conflate patient- and family-centered care, as though achieving patient-centered care necessarily means that care is also family-centered. We would caution against presupposing that communication styles and preferences are the same for both patients and families. A more nuanced interpretation would suggest that there is a range of diverse situations in which families become motivated to create authentic family-clinician relationships. (21,22) Specifically, our data suggests that it is the content—clinicians’ willingness to write personalized free-text messages based on families’ informational needs and avoiding scripted, canned messages—that allows families to feel engaged. Families can tell whether messages sent are genuine attempts to keep them meaningfully and intentionally updated on the day's plan of care or health progress versus ones that are “robotic” sounding and sent for “compliance” purposes.
Another significant contribution of this study is that no loved ones mentioned disliking that they could not write back. Perhaps the back-and-forth, read text and reply, motion provided a sense of bidirectionality without drawing on clinicians’ time in having to respond to family messages. In our previous work, we elicited an important finding: Greater levels of interactivity (bidirectional engagement) enhance the appeal of text messaging. However, modest levels of interactivity with close-ended, option responses, allow patients to feel meaningfully connected. (21,22) We believe this study supports our earlier finding that families also respond favorably to most levels of interactivity. (21,22) This finding suggests that family-clinician connectedness can be achieved without becoming administratively burdensome. (23)
The findings on security features are also insightful. Loved ones only needed to enter the patient's birth year to access the texted information—a minimal inconvenience. Healthcare professionals should maximize and protect patients’ information even where, as here, by avoiding transmitting protected healthcare information (PHI), using data-encrypted URLs that are HIPAA-complaint, and requiring patients’ permission before sending texts. (22) Yet, these findings suggest that loved ones might value convenience more than security. Processes that make individuals more secure are also, by nature, less convenient. (24,25)
The tradeoff between convenience and security should be explored further in future research. These conversations should be contextualized based on the nature of the device, the type of information being shared, when and how the information is shared in the patient's care journey, and security levels. Based on our findings, stakeholders may value trade-offs between privacy and security that are context-dependent and vary over time. Therefore, a one-size-fits-all regulatory approach may be untenable. If additional studies confirm this, then current legislation on healthcare privacy should be amended. (26)
The study limitations are a product of the types of records reviewed. First, coders’ interpretations were necessary when reviewing free-text fields. To offset limitations, as noted, we used a codebook for assigning variables. Second, our study does not fully reflect the diversity of our Houston culture in that it is limited to English-speaking and Spanish-speaking families. This study was conducted in Houston, Texas, which is considered one of the most diverse cities in the world. Our hospital has a substantive Arab and Vietnamese population, among many other cultures. Yet, we could not message in Arabic or Vietnamese due to character limitations, despite having a robust patient population who fit this profile. The lack of diversity in our study impedes our ability to generalize study results. (26–28) Third, we provided percentages alongside the themes to give a measure of theme prevalence. We do not intend for the percentages to be interpreted as a full sample representation. (26,27)
Conclusions
To our knowledge, this is the first qualitative study exploring family and loved ones’ perspectives in using inpatient texting. This study advances our understanding of family-centered care by providing an empirical foundation that buttresses previous conceptual work. (5) Specifically, we found that technologies can empower caretakers to become more involved and informed in their loved one's care. (14) Future research should explore how technologies can be integrated into clinical workflows without being viewed as disruptive.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This study was waived by the Institutional Review Board of Houston Methodist Hospital in Houston, Texas.
ORCID iD: Courtenay R. Bruce https://orcid.org/0000-0002-9503-9834
Statement of Human and Animal Subjects: All procedures in this study were conducted in accordance with the Institutional Review Board protocol that was waived.
Statement of Informed Consent: Informed consent was not obtained because the study was waived. All data were aggregated and anonymized.
References
- 1.Donald MB, Thomas WN, John W. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759-69. [DOI] [PubMed] [Google Scholar]
- 2.Wong P, Redley B, Digby R, Correya A, Bucknall T. Families’ perspectives of participation in patient care in an adult intensive care unit: a qualitative study. Aust Crit Care. 2020;33(4):317-25. [DOI] [PubMed] [Google Scholar]
- 3.Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-61. [DOI] [PubMed] [Google Scholar]
- 4.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruce CR, Minard CG, Wilhelms LA, Abrahma M, Amione-Guerra J, Pham L. Caregivers of patients with left ventricular assist devices. Circ Cardiovasc Qual Outcomes. 2017;10(1). doi: 10.1161/CIRCOUTCOMES.116.002879. [DOI] [PubMed] [Google Scholar]
- 6.Grant CJ, Doig LF, Everson J, Foster N, Doig CJ. Impact of patient and family involvement in long-term outcomes. Critical Care N. 2020;32(2):227-42. [DOI] [PubMed] [Google Scholar]
- 7.Goeschel C, Panoff G. Patient and family-centered care. Agency for healthcare research and quality. 2023. https://www.ahrq.gov/hai/cauti-tools/archived-webinars/patient-family-centered-care-slides.html (accessed July 30, 2022).
- 8.Choi M, Raeside R, Hyun K, Partridge SR, Thiagalingam A, Redfern J. Understanding preferences for lifestyle-focused visual text messages in patients with cardiovascular and chronic respiratory disease: discrete choice experiment. J Med Internet Res. 2021;23(9):e26224. PMID: 34542413; PMCID: PMC8491117. doi: 10.2196/26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mougalian SS, Gross CP, Hall EK. Text messaging in oncology: a review of the landscape. JCO Clin Cancer Inform. 2018;2:1-9. PMID: 30652579. doi: 10.1200/CCI.17.00162. [DOI] [PubMed] [Google Scholar]
- 10.Dawson J, Tong A, Matus Gonzalez A, Campbell KL, Craig JC, Lee VW. Patients’ experiences and perspectives of a mobile phone text messaging intervention to improve dietary behaviours in haemodialysis. Nutr Diet . 2021;78(5):516-23. Epub 2021 Apr 18. PMID: 33870612. doi: 10.1111/1747-0080.12667. [DOI] [PubMed] [Google Scholar]
- 11.Tam HL, Wong EML, Cheung K, Chung SF. Effectiveness of text messaging interventions on blood pressure control among patients with hypertension: systematic review of randomized controlled trials. JMIR mHealth uHealth. 2021;9(9):e24527. PMID: 34550078; PMCID: PMC8495578. doi: 10.2196/24527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuhas M, Porter KJ, Brock DP, Loyd A, McCormick BA, Zoellner JM. Development and pilot testing of text messages to help reduce sugar-sweetened beverage intake among rural caregivers and adolescents: mixed methods study. JMIR mHealth uHealth. 2019;7(7):e14785. PMID: 31364600; PMCID: PMC6691674. doi: 10.2196/14785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ladley A, Hieger AW, Arthur J, Broom M. Educational text messages decreased emergency department utilization among infant caregivers: a randomized trial. Acad Pediatr. 2018;18(6):636-41. Epub 2018 Feb 9. PMID: 29432907. doi: 10.1016/j.acap.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Martindale-Adams JL, Clark CD, Martin JR, Henderson CR, Nichols LO. Text messages to support caregivers in a health care system: development and pilot and national rollout evaluation. J Particip Med. 2022;14(1):e35318. PMID: 36251368; PMCID: PMC9623465. doi: 10.2196/35318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HCAHPS: patients’ perspectives of care survey. www.cms.gov. 2021. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalhcahps (accessed August 12, 2022).
- 16.Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. 3rd ed. Sage Publications; 2007. [Google Scholar]
- 17.ATLAS.ti 7 (Atlas.ti Scientific Software Development Company, GmbH, Berlin, Germany) was used to facilitate the coding process.
- 18.Holden RJ, Carayon P, Gurses APet al. et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics . 2013:56(11):1669-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardyman W, Daunt KL, Kitchener M. Value co-creation through patient engagement in health care: a micro-level approach and research agenda. Public Manage Rev. 2015;17(1):90-107. [Google Scholar]
- 20.Chandler JD, Vargo SL. Contextualization and value-in-context: how context frames exchange. Sage. 2011;11(1):35-49. [Google Scholar]
- 21.Bruce CR, Harrison P, Vinh TM, Manoharan AG, Giammattei C. Design and integration of mobile health technology in the treatment of orthopaedic surgery: a qualitative study. ACI Open Access. 2022;6(1):e11-e20. doi: 10.1055/s-0042-1754011. [DOI] [Google Scholar]
- 22.Bruce CR, Harrison P, Nisar T, Giammattei C, Tan NM. Assessing the impact of patient-facing mobile health technology on patient outcomes: retrospective observational Cohort study. JMIR mHealth uHealth. 2020;8(6):e19333. doi: 10.2196/19333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erickson SM, Rockwern B, Koltov M, McLean RM. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern. 2017;166(9):659-61. [DOI] [PubMed] [Google Scholar]
- 24.Wani TA, Mendoza A, Gray K. Hospital bring-your-own-device security challenges and solutions: systematic review of gray literature. JMIR mHealth uHealth. 2020;8(6):e18175. doi: 10.2196/18175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cherecwich P. Security vs. convenience: the ultimate trade-off? Face value - medium. Published 2019. 2019. https://medium.com/face-value/security-vs-convenience-the-ultimate-trade-off-843e476bf538 (accessed July 30, 2022).
- 26.Privacy Act of 1974. The United States Department of Justice. Published 2021. 2021. https://www.justice.gov/opcl/privacy-act-1974 (accessed July 30, 2022).
- 27.Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Family Med. 2008;6(4):331-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip. 2016;9(1):211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]