Abstract
Background
Bipolar disorder is associated with functional impairment and diminished health-related quality of life (HRQoL). The purpose of this study was to estimate the annual per patient direct healthcare costs, indirect costs, and HRQoL of patients with bipolar disorder by depressive symptom severity and overall compared to the general population in the US.
Methods
This cross-sectional study used self-reported data from the 2020 US National Health and Wellness Survey. Adult respondents who reported bipolar disorder symptoms in the past 12 months and/or a diagnosis of bipolar disorder were identified (bipolar disorder cohort) and were further classified by depressive symptom severity based on Patient Health Questionnaire (PHQ-9) scores (none/mild = 0–9, moderate = 10–14, severe = 15–27). Annualized direct healthcare costs and indirect costs were calculated from 6-month healthcare resource utilization and work productivity, respectively. A general population cohort was constructed using 2:1 propensity score matching. Multivariate regression models of all-cause hospitalizations in the past 6 months, annualized direct healthcare costs, annualized indirect costs, and HRQoL (eg, EuroQol 5-Dimension Health Questionnaire (EQ-5D)) controlled for confounders (demographic and clinical characteristics).
Results
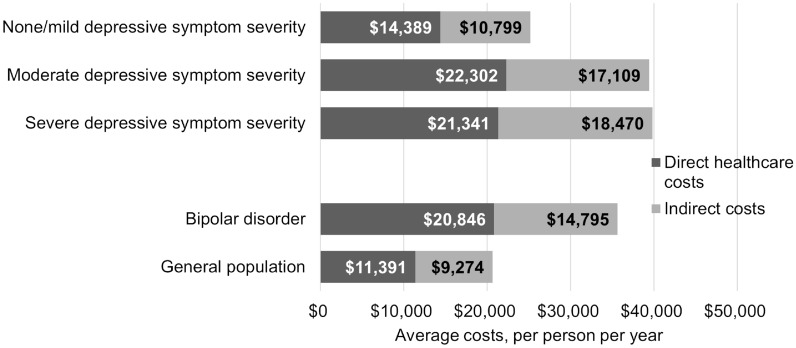
Of 3583 adults meeting pre-specified criteria for bipolar disorder, 1401 (39.1%) reported none/mild, 889 (24.8%) moderate, and 1293 (36.1%) severe depressive symptom severity. Additionally, 3285 (91.7%) were matched to 6570 adults in the general population. Compared to the general population, adjusted mean hospitalizations (0.53 vs. 0.30), annualized per patient direct healthcare costs ($20,846 vs. $11,391), and indirect costs ($14,795 vs. $9274) were significantly greater for the bipolar disorder cohort (all p < 0.001); adjusted HRQoL (EQ-5D: 0.69 vs. 0.79) was significantly worse (p < 0.001). By depressive symptom severity, adjusted mean hospitalizations (none/mild = 0.30, moderate = 0.50, severe = 0.46), direct healthcare costs ($14,389, $22,302, $21,341), and indirect costs ($10,799, $17,109, $18,470) were significantly greater for moderate and severe compared to none/mild depressive symptom severity (all p < 0.01); adjusted HRQoL (EQ-5D: 0.77, 0.67, 0.59) was significantly worse (p < 0.001).
Conclusions
Among respondents with bipolar disorder, those with moderate to severe depression had greater direct healthcare costs and indirect costs as well as worse HRQoL than those with mild or no depressive symptoms. Treatment targeting reduction in depressive symptoms may reduce the economic and humanistic burden of bipolar disorder.
Keywords: Bipolar depression, Direct healthcare costs, Indirect costs, Health-related quality of life, Burden of illness
Introduction
Bipolar disorder is an affective disorder characterized by recurrent manic (bipolar I disorder) or hypomanic (bipolar II disorder) episodes alternating with depressive episodes [1]. The annual prevalence of bipolar disorder is estimated to be 2.8% in the US [2], which may be an underestimation due to under or delayed diagnosis [3]. Symptomatic episodes occur approximately 43–50% of the time [3, 4], and most symptomatic time (70%) is spent in a depressed state (bipolar depression) [4].
The impact of bipolar disorder on patients’ lives is substantial and wide-ranging. Compared to the general population, patients with bipolar disorder have increased risk of cardiovascular disease, obesity, diabetes, hyperglycemia, dyslipidemia, metabolic syndrome, respiratory disease, and migraine headaches [5–7]. In older adults with bipolar disorder, women may be more likely to experience physical comorbidities than men [6]. Co-occurring psychiatric conditions such as substance abuse, anxiety, and borderline personality disorders are also more prevalent in individuals with bipolar disorder compared to the general population [3]. Life expectancy with bipolar disorder is reduced by 9–20 years [8]. Additionally, bipolar disorder has been associated with impaired psychosocial functioning, unemployment, and loss of productivity [5, 9].
Patients with bipolar disorder report worse health-related quality of life (HRQoL) compared to the general population [10, 11]. Bipolar disorder symptoms as well as impaired functioning and productivity in patients with bipolar disorder have been associated with reduced HRQoL [12–14]. Depressive symptoms are more likely associated with worse HRQoL than manic symptoms [13, 15, 16].
The annual economic burden of bipolar disorder in the United States is estimated to be $202 billion [17]. Indirect costs associated with unemployment, productivity loss, and caregiver burden are the main cost driver comprising 72% of total costs [17]. Direct healthcare costs, including inpatient hospitalizations, emergency room visits, and outpatient visits comprise approximately 25% of total costs or $46 billion annually [17]. Direct healthcare costs for individuals with bipolar disorder are estimated to be $25 billion higher than direct healthcare costs for the general population [17].
The economic and humanistic burden of bipolar disorder in the US has not been estimated by severity of depressive symptoms. The aim of this study was to estimate the annual per patient direct healthcare costs and indirect costs as well as the HRQoL of patients with bipolar disorder by depressive symptom severity. Our hypothesis was that economic and humanistic burden would be greater for patients with greater depressive symptom severity. We also report the annual per patient direct healthcare costs, indirect costs, and HRQoL of the general population in the US for comparison.
Methods
Data source and study population
Data used in this retrospective, population-based, observational, cross-sectional study are from the 2020 US National Health and Wellness Survey (NHWS), which is a nationally representative database of patient-reported outcomes covering attitudes, behaviors, characteristics, and demographics. Adult respondents were recruited from an existing, general-purpose, web-based consumer panel, with stratified random sampling within the survey panel to ensure representativeness in terms of age and gender. The NHWS is internet-based and self-administered, and data were collected from respondents between April and July 2020. Following the survey logic, not all questions may be presented to all respondents. Respondents were classified as having bipolar disorder or not (general population) based on respondents’ self-reported experience of bipolar disorder in the past 12 months or subject endorsement of a physician diagnosis of bipolar disorder. Respondents with bipolar disorder were further classified by depressive symptom severity using the Patient Health Questionnaire (PHQ-9) (none/mild = 0–9; moderate = 10–14; severe = 15+) [18], a 9-item questionnaire which assesses severity of depressive symptoms over the past 2 weeks.
Ethical considerations
This study was conducted in accordance with ethical principles consistent with the Declaration of Helsinki and International Conference on Harmonisation (ICH), Good Clinical Practice, Good Pharmacoepidemiology Practice. All respondents explicitly agreed to participate in the NHWS and were provided fair-market value incentives for participation. The 2020 US NHWS was reviewed and approved by the Pearl Institutional Review Board (IRB; Indianapolis, IN, USA). Data were anonymized for use in this study and, as such, did not require further IRB approval.
Outcomes and other variables
The NHWS collects a wide range of demographic and clinical variables. Demographic characteristics included age, sex, employment status, race/ethnicity, marital status, education level, household income, and health insurance status. Clinical characteristics included body mass index (BMI), smoking status, alcohol use, exercise behavior, Charlson Comorbidity Index (CCI) [19], cardiometabolic comorbidities, PHQ-9, and the 7-item General Anxiety Disorder (GAD-7) scale [20].
For respondents with bipolar disorder, additional data were collected including type of bipolar disorder, age at diagnosis, the type of healthcare practitioner who diagnosed bipolar disorder, whether or not a diagnosis of major depressive disorder (MDD) was made prior to bipolar disorder diagnosis, number of depressive episodes (lasting > 2 weeks) in the past year, number of manic episodes (lasting > 1 week) in the past year, and number of hospitalizations related to mood, emotions, or behavior in the past year.
The primary outcome of interest was the economic and humanistic burden of bipolar disorder measured by HCRU, HRQoL, direct healthcare costs, and indirect costs. Self-reported HCRU included hospitalizations, physician visits, and emergency room (ER) visits in the past 6 months for any medical condition (all-cause). Mental health-related hospitalizations were also reported. Work productivity was assessed using the Work Productivity and Activity Impairment (WPAI) Questionnaire, which is a six-item instrument that asks about impairment due to health in the past week [21]. All respondents completed the WPAI item for activity impairment (percentage of impairment in daily activities). Respondents who self-reported being part of the labor force (full-time, part-time, or self-employed) also completed the items for absenteeism (percentage of work time missed) and presenteeism (percentage of impairment experienced while at work).
Two HRQoL instruments were administered. The five-level EuroQol 5-Dimension Health Questionnaire (EQ-5D) is a self-reported measure of health comprised of 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression [22]. The EQ-5D Index Score is a summary across the 5 domains with a range from 0–1 with a lower score indicating greater disability. The EQ-5D visual analog scale (VAS) asks respondents to indicate their self-rated health from 0–100 with 0 = ‘worst imaginable health state’ and 100 = ‘best imaginable health state’. The revised Medical Outcomes Study 36-Item Short Form Survey Instrument (SF-36) is a multipurpose, generic HRQoL instrument composed of 36 questions, which uses norm-based scoring to allow for comparisons with the general population [23]. The normed physical component summary (PCS) and mental component summary (MCS) scores were reported separately. Health utility scores were estimated from six domains of the SF-36 (SF-6D).
Direct healthcare costs were calculated using self-reported HCRU (hospitalizations, ER visits, and physician visits) multiplied by the age-stratified average cost per visit from the 2018 Medical Expenditure Panel Survey (MEPS), which was the most recently available at the time of the analysis. MEPS-based average costs were not specific to practitioner type or reason for the visit. Direct healthcare costs were annualized by multiplying the 6-month HCRU by two before applying the average cost per visit. Indirect costs were calculated based on the human capital approach. Indirect costs were calculated using hours missed from work in the last 7 days due to health and hours worked in the last 7 days while impaired by health and were multiplied by the average 2019 wage per day by sex and age from the Bureau of Labor Statistics [24]. Indirect costs were annualized based on 50 paid working weeks per year. Costs were reported in 2019 USD.
Statistical analysis
Demographic, health, and bipolar disorder-specific characteristics were reported using means and standard deviations for continuous variables and counts and proportions for categorical variables. Multivariate regression models were used to compare hospitalizations, direct healthcare costs, indirect costs, and HRQoL. Generalized linear models (GLMs) were estimated using a negative binomial distribution for hospitalizations, a gamma distribution for direct healthcare costs and indirect costs, and a normal distribution for HRQoL. Covariates were included to control for confounders and were selected based on review of the literature or bivariate significance (p-value < 0.05). Multicollinearity was evaluated in all models. Models of HRQoL and direct healthcare costs by depressive symptom severity controlled for age, sex, race, employment, health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. The model of indirect costs by depressive symptom severity used the same control variables except for employment. Frequency of manic episodes was not included in the models. Propensity score matching was used to construct a general population cohort. A 2:1 match was used to identify two members of the general population without bipolar disorder for each respondent with bipolar disorder. The matching model controlled for age, sex, race, employment, marital status, health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. Respondents with bipolar disorder who were unable to be matched to the general population were dropped. Models comparing respondents with bipolar disorder vs. the general population controlled for CCI. Adjusted means and 95% confidence intervals (CIs) were calculated using the fitted GLMs. Descriptive statistics and bivariate analyses were conducted using SPSS v28 (IBM Corp, New York, USA), and regression models were built in SAS v9.4 (SAS Corporation, North Carolina, USA). Statistical significance was defined as p-value < 0.05.
Results
Respondent characteristics
There were 3583 respondents meeting pre-specified criteria for bipolar disorder in the 2020 US NHWS (Fig. 1). Of those respondents, 1401 (39.1%) reported none/mild, 889 (24.8%) moderate, and 1293 (36.1%) severe depressive symptom severity. Among respondents with bipolar disorder, 3285 (91.7%) were matched to the general population (n = 6570). The demographic and clinical characteristics of the bipolar disorder and general population cohorts were similar except for greater comorbidities among respondents with bipolar disorder (CCI = 0.7 vs. 0.6, p = 0.001) (Table 1).
Fig. 1.
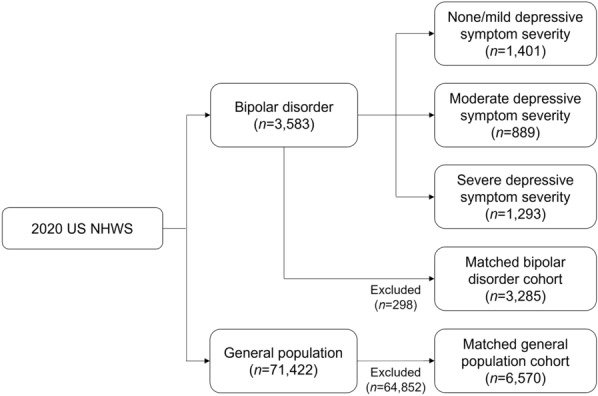
Flow diagram. n, number of respondents
Table 1.
Demographic and clinical characteristics
| Characteristic | Respondents with bipolar disorder by depressive symptom severity | Respondents with bipolar disorder (n = 3285) | General population (n = 6570) | ||
|---|---|---|---|---|---|
| None/mild (n = 1401) | Moderate (n = 889) | Severe (n = 1293) | |||
| Age, mean (SD) | 38.8 (14.5) | 33.0 (12.2)a | 34.4 (11.5)a | 36.3 (13.3) | 35.9 (14.7) |
| Female, n (%) | 833 (59.5%) | 513 (57.7%)a | 848 (65.6%)a | 2031 (61.8%) | 4046 (61.6%) |
| Race/ethnicity, n (%) | |||||
| White | 796 (56.8%) | 439 (49.4%)a | 738 (57.1%)a | 1828 (55.6%) | 3585 (54.6%) |
| Black | 203 (14.5%) | 132 (14.8%)a | 134 (10.4%)a | 433 (13.2%) | 878 (13.4%) |
| Hispanic | 273 (19.5%) | 208 (23.4%)a | 310 (24.0%)a | 700 (21.3%) | 1443 (22.0%) |
| Other | 129 (9.2%) | 110 (12.4%)a | 111 (8.6%)a | 324 (9.9%) | 664 (10.1%) |
| Region, n (%) | |||||
| Northeast | 241 (17.2%) | 164 (18.4%) | 203 (15.7%) | 556 (16.9%) | 1171 (17.8%) |
| Midwest | 283 (20.2%) | 169 (19.0%) | 234 (18.1%) | 629 (19.1%) | 1341 (20.4%) |
| South | 577 (41.2%) | 393 (44.2%) | 564 (43.6%) | 1390 (42.3%) | 2629 (40.0%) |
| West | 300 (21.4%) | 163 (18.3%) | 292 (22.6%) | 710 (21.6%) | 1429 (21.8%) |
| Marital status, n (%) | |||||
| Single | 808 (57.7%) | 521 (58.6%) | 730 (56.5%) | 1872 (57.0%) | 3809 (58.0%) |
| Married/living with Partner | 593 (42.3%) | 368 (41.4%) | 563 (43.5%) | 1413 (43.0%) | 2761 (42.0%) |
| Education, n (%) | |||||
| Less than college/university | 1012 (72.2%) | 643 (72.3%)a | 988 (76.4%)a | 2405 (73.2%) | 4832 (73.5%) |
| College/university degree or higher | 389 (27.8%) | 246 (27.7%)a | 305 (23.6%)a | 880 (26.8%) | 1738 (26.5%) |
| Any employment (full-time/part-time/self-employed), n (%) | 721 (51.5%) | 517 (58.2%)a | 647 (50.0%)a | 1743 (53.1%) | 3506 (53.4%) |
| Any health insurance, n (%) | 1164 (83.1%) | 719 (80.9%)a | 1008 (78.0%)a | 2672 (81.3%) | 5308 (80.8%) |
| Annual household income, n (%) | |||||
| Less than $50,000 | 880 (62.8%) | 521 (58.6%)a | 854 (66.0%)a | 2055 (62.6%) | 4227 (64.3%) |
| $50,000 or greater | 521 (37.2%) | 368 (41.4%)a | 439 (34.0%)a | 1230 (37.4%) | 2343 (35.7%) |
| Smoking status, n (%) | |||||
| Never smoked | 559 (39.9%) | 383 (43.1%)a | 411 (31.8%)a | 1274 (38.8%) | 2507 (38.2%) |
| Former smoker | 332 (23.7%) | 178 (20.0%)a | 262 (20.3%)a | 736 (22.4%) | 1518 (23.1%) |
| Current smoker | 510 (36.4%) | 328 (36.9%)a | 620 (48.0%)a | 1275 (38.8%) | 2545 (38.7%) |
| Any alcohol use, n (%) | 884 (63.1%) | 649 (73.0%)a | 887 (68.6%)a | 2197 (66.9%) | 4388 (66.8%) |
| Any exercise in the past month, n (%) | 909 (64.9%) | 607 (68.3%)a | 764 (59.1%)a | 2103 (64.0%) | 4240 (64.5%) |
| BMI, kg/m2, mean (SD) | 29.4 (8.0) | 28.7 (8.4) | 28.9 (8.5) | 28.9 (8.3) | 28.9 (8.2) |
| CCI, mean (SD) | 0.7 (2.0) | 0.8 (1.6) a | 1.1 (2.3) a | 0.7 (1.4) | 0.6 (1.4)b |
| Cardiometabolic comorbidities, n (%) | |||||
| Obesity | 566 (39.7%) | 303 (34.1%)a | 486 (37.6%)a | 1273 (38.8%) | 2400 (36.5%)b |
| Hypertension | 309 (22.1%) | 160 (18.0%)a | 308 (23.8%)a | 721 (21.9%) | 1141 (17.4%)b |
| Migraine | 270 (19.3%) | 207 (23.3%)a | 417 (32.3%)a | 827 (25.2%) | 940 (14.3%)b |
| Diabetes | 176 (12.6%) | 104 (11.7%) | 147 (11.4%) | 374 (11.4%) | 623 (9.5%) |
| Cardiovascular disease | 123 (8.8%) | 81 (9.1%) | 145 (11.2%) | 288 (8.8%) | 431 (6.6%)b |
| Cerebrovascular disease | 47 (3.4%) | 32 (3.6%) | 63 (4.9%) | 111 (3.4%) | 149 (2.3%)b |
| PHQ-9, mean (SD) | 4.9 (3.3) | 12.1 (1.4)a | 19.9 (3.9)a | 12.0 (7.2) | 7.6 (7.0)b |
| GAD-7, mean (SD) | 5.7 (4.8) | 10.1 (4.1)a | 14.5 (4.9)a | 9.9 (6.1) | 6.1 (5.8)b |
BMI, body mass index; CCI, Charlson Comorbidity Index; GAD-7, 7-item General Anxiety Disorder scale; n, number of respondents; PHQ-9, Patient Health Questionnaire; SD, standard deviation
aSignificant at p < 0.05 across depressive symptom severity cohorts [reference = none/mild]
bSignificant at p < 0.05 for bipolar disorder vs. general population [reference]
Across the current depressive symptom severity cohorts, demographic and clinical characteristics were significantly different (Table 1). Respondents with none/mild depressive symptom severity were the oldest on average (none/mild = 38.8 years, moderate = 33.0 years, severe = 34.4 years; p < 0.001) and had the lowest CCI score (0.7, 0.8, 1.1; p < 0.001). Respondents with moderate depressive symptom severity were most likely to be male (none/mild = 40.5%, moderate = 42.3%, severe = 34.4%; p < 0.001) and employed (51.5%, 58.2%, 50.0%; p = 0.001) and to have an annual household income of $50,000 or greater (37.2%, 41.4%, 34.0%; p = 0.002). Respondents with moderate depressive symptom severity also had the greatest rates of never smoked (39.9%, 43.1%, 31.8%; p < 0.001), alcohol use (63.1%, 73.0%, 68.6%; p < 0.001), and exercise in the past month (64.9%, 68.3%, 59.1%; p < 0.001). Respondents with severe depressive symptom severity were most likely to have less than a college or university degree (72.2%, 72.3%, 76.4%; p = 0.026) and had the greatest rates of being a current smoker (36.4%, 36.9%, 48.0%; p < 0.001).
Approximately 40% of respondents in the bipolar disorder cohort reported a current diagnosis or presence of symptoms consistent with bipolar I disorder, 40% with bipolar II disorder, and 20% with unspecified bipolar disorder (p = 0.134) (Table 2). The average numbers of depressive (none/mild = 3.1, moderate = 4.5, severe = 7.4; p < 0.001) and manic (2.6, 3.7, 5.3; p < 0.001) episodes were twice as high for respondents with current severe compared to none/mild depressive symptom severity.
Table 2.
Additional characteristics of respondents with bipolar disorder
| Characteristic | Respondents with bipolar disorder by depressive symptom severity | ||
|---|---|---|---|
| None/mild (n = 1401) | Moderate (n = 889) | Severe (n = 1293) | |
| Number of depressive episodes in the past year, mean (SD) | 3.1 (5.0) | 4.5 (5.3)b | 7.4 (7.3)b |
| Number of manic episodes in the past year, mean (SD) | 2.6 (4.6) | 3.7 (5.1)b | 5.3 (6.2)b |
| Number of hospitalizations related to mood, emotions, or behavior in the past year, mean (SD) | 0.7 (3.9) | 1.5 (5.2)b | 1.5 (6.0)b |
| Type of bipolar disorder, n (%)a | |||
| Type I | 394 (40.7%) | 184 (37.0%) | 334 (40.5%) |
| Type II | 365 (37.7%) | 222 (44.7%) | 322 (39.1%) |
| Unspecified | 208 (21.5%) | 91 (18.3%) | 168 (20.4%) |
| Age at diagnosis of bipolar disorder, mean (SD)a | 27.3 (12.6) | 24.8 (12.2)b | 24.9 (11.5)b |
| Healthcare practitioner who diagnosed bipolar disorder, n (%)a | |||
| Psychiatrist | 634 (65.6%) | 283 (56.9%) | 473 (57.4%) |
| Primary Care Physician/General Practitioner/Internist | 143 (14.8%) | 86 (17.3%) | 137 (16.6%) |
| Psychologist | 116 (12.0%) | 81 (16.3%) | 137 (16.6%) |
| Nurse Practitioner/Physician Assistant in a psychiatry practice | 29 (3.0%) | 18 (3.6%) | 27 (3.3%) |
| Nurse Practitioner/Physician Assistant in a primary care physician/general practitioner/internist practice | 16 (1.7%) | 11 (2.2%) | 17 (2.1%) |
| Other | 29 (3.0%) | 18 (3.6%) | 33 (4.0%) |
| Diagnosis of MDD prior to bipolar disorder diagnosis, n (%)a | 582 (60.2%) | 361 (72.6%)b | 636 (77.2%)b |
MDD, major depressive disorder; n, number of respondents; SD, standard deviation
aNumber of respondents was lower for type of bipolar disorder, age at diagnosis of bipolar disorder, healthcare practitioner who diagnosed bipolar disorder, and diagnosis of MDD prior to bipolar disorder diagnosis (none/mild: n = 967, moderate: n = 497, severe: n = 824)
bSignificant at p < 0.05 across depressive symptom severity cohorts [reference = none/mild]
Economic burden in respondents with bipolar disorder vs. general population
After adjusting for demographic and clinical characteristics, respondents in the bipolar disorder cohort reported an average of 0.53 (95% CI 0.43, 0.66) all-cause hospitalizations in the past 6 months compared to 0.30 (0.26, 0.35) for the matched general population (Table 3). Average annualized direct healthcare costs were $20,846 ($17,654, $24,615) in the bipolar cohort compared to $11,391 ($10,129, $12,811) in the matched general population. Average annualized indirect costs were $14,795 ($13,867, $15,786) in the bipolar cohort compared to $9274 ($8861, $9705) in the matched general population.
Table 3.
Adjusted hospitalizations, direct healthcare costs, and indirect costs
| Outcome | Respondents with bipolar disorder by depressive symptom severity | Respondents with bipolar disorder (n = 3285) | General population (n = 6570) | ||
|---|---|---|---|---|---|
| None/mild (n = 1401) | Moderate (n = 889) | Severe (n = 1293) | |||
| All-cause hospitalizations in the past 6 months, mean (95% CI) | 0.30 (0.24, 0.37) | 0.50 (0.39, 0.64) | 0.46 (0.38, 0.57) | 0.53 (0.43, 0.66) | 0.30 (0.26, 0.35) |
| Annualized total direct healthcare costs, per patient, mean (95% CI) | $14,389 ($12,390, $16,711) | $22,302 ($18,420, $27,001) | $21,341 ($18,231, $24,981) | $20,846 ($17,654, $24,615) | $11,391 ($10,129, $12,811) |
| Annualized indirect costs, per patient, mean (95% CI) | $10,799 ($9938, $11,734) | $17,109 ($15,487, $18,901) | $18,470 ($16,889, $20,200) | $14,795 ($13,867, $15,786) | $9274 ($8861, $9705) |
BMI, body mass index; CCI, Charlson Comorbidity Index; CI, confidence interval; n, number of respondents
Models by depressive symptom severity adjusted for age, sex, race, employment (models of hospitalizations and directs costs only), health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. Models comparing respondents with bipolar disorder vs. matched general population adjusted for CCI
Economic burden by depressive symptom severity
After adjusting for demographic and clinical characteristics, all-cause hospitalizations in the past 6 months (moderate: mean (95% CI) 0.50 (0.39, 0.64); severe: 0.46 (0.38, 0.57)), annualized direct healthcare costs [$22,302 ($18,420, $27,001); $21,341 ($18,231, $24,981)), and annualized indirect costs ($17,109 ($15,487, $18,901); $18,470 ($16,889, $20,200)] were not significantly different when comparing respondents with moderate or severe depressive symptom severity. However, both moderate and severe depressive symptom cohorts had significantly greater economic burden compared to the none/mild cohort [hospitalizations: 0.30 (0.24, 0.37), direct healthcare costs: $14,389 ($12,390, $16,711), indirect costs: $10,799 ($9938, $11,734)]. Combined average direct healthcare costs and indirect costs were similar for respondents with current moderate and severe depressive symptom severity (Fig. 2). Combined average direct healthcare costs and indirect costs were greater among respondents with bipolar disorder compared to the general population cohort.
Fig. 2.
Adjusted direct healthcare costs and indirect costs. BMI, body mass index; CCI, Charlson Comorbidity Index. Models by depressive symptom severity adjusted for age, sex, race, employment (model of direct healthcare costs only), health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. Models comparing respondents with bipolar disorder vs. matched general population adjusted for CCI
Humanistic burden in respondents with bipolar disorder vs. general population
After adjusting for demographic and clinical characteristics, the average EQ-5D score in respondents in the bipolar disorder cohort was 0.69 (95% CI 0.68, 0.69) compared to 0.79 (0.79, 0.80) for the matched general population (Table 4). Both SF-36 components were worse for respondents in the bipolar disorder cohort (MCS: mean (95% CI) 35.4 (35.0, 35.8); PCS: 46.5 (46.2, 46.9) compared to the matched general population (MCS: 42.0 (41.7, 42.3); PCS: 49.6 (49.3, 49.8)).
Table 4.
Adjusted HRQoL
| Outcome | Respondents with bipolar disorder by depressive symptom severity | Respondents with bipolar disorder (n = 3285) | General population (n = 6570) | ||
|---|---|---|---|---|---|
| None/mild (n = 1401) | Moderate (n = 889) | Severe (n = 1293) | |||
| EQ-5D, mean (95% CI) | 0.77 (0.76, 0.78) | 0.67 (0.66, 0.68) | 0.59 (0.58, 0.60) | 0.69 (0.68, 0.69) | 0.79 (0.79, 0.80) |
| EQ-5D VAS, mean (95% CI) | 70.9 (69.6, 72.3) | 62.1 (60.3, 63.8) | 56.1 (54.6, 57.5) | 63.8 (63.0, 64.7) | 71.7 (71.1, 72.3) |
| SF-36 MCS, mean (95% CI) | 42.0 (41.5, 42.5) | 35.1 (34.5, 35.8) | 28.1 (27.6, 28.6) | 35.4 (35.0, 35.8) | 42.0 (41.7, 42.3) |
| SF-36 PCS, mean (95% CI) | 48.7 (48.2, 49.2) | 44.9 (44.3, 45.6) | 44.4 (43.9, 45.0) | 46.5 (46.2, 46.9) | 49.6 (49.3, 49.8) |
| SF-6D, mean (95% CI) | 0.65 (0.65, 0.66) | 0.57 (0.57, 0.58) | 0.53 (0.52, 0.54) | 0.59 (0.59, 0.60) | 0.67 (0.66, 0.67) |
BMI, body mass index; CCI, Charlson Comorbidity Index; CI, confidence interval; EQ-5D, EuroQol 5-Dimension Health Questionnaire; MCS, mental component summary; n, number of respondents; PCS, physical component summary; SF-36, Medical Outcomes Study 36-Item Short Form Survey Instrument; VAS, visual analog scale
Models by depressive symptom severity adjusted for age, sex, race, employment, health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. Models comparing respondents with bipolar disorder vs. matched general population adjusted for CCI
Humanistic burden by depressive symptom severity
After adjusting for demographic and clinical characteristics, the average EQ-5D score was 0.59 (95% CI 0.58, 0.60) for respondents with current severe depressive symptom severity compared to 0.67 (0.66, 0.68) and 0.77 (0.76, 0.78) for moderate and none/mild, respectively. The SF-36 MCS was 28.1 (27.6, 28.6) for respondents with severe depressive symptom severity compared to 35.1 (34.5, 35.8) and 42.0 (41.5, 42.5) for moderate and none/mild, respectively. The SF-36 PCS was 44.9 (44.3, 45.6) and 44.4 (43.9, 45.0) for moderate and severe depressive symptom severity, respectively, which was significantly lower than 48.7 (48.2, 49.2) in the none/mild cohort. EQ-5D scores for respondents with none/mild depressive symptom severity were slightly lower than for the general population (Fig. 3).
Fig. 3.
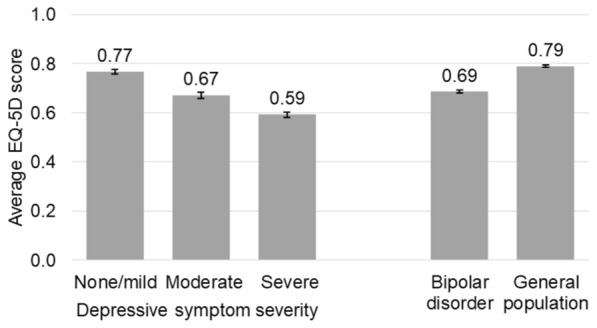
Adjusted HRQoL. BMI, body mass index; CCI, Charlson Comorbidity Index; CI, confidence interval; EQ-5D, EuroQol 5-Dimension Health Questionnaire. Model by depressive symptom severity adjusted for age, sex, race, employment, health insurance, smoking status, alcohol use, exercise behavior, BMI, education level, income level, and CCI. Model comparing respondents with bipolar disorder vs. matched general population adjusted for CCI. Error bars represent 95% CI
Discussion
Among respondents with bipolar disorder, current moderate or severe depressive symptom severity was associated with greater hospitalizations, direct healthcare costs, and indirect costs compared to none/mild depressive symptom severity. HRQoL was significantly worse with greater levels of depressive symptom severity. To our knowledge, this is the first study comparing differences in economic and humanistic burden of bipolar disorder by depressive symptom severity in a US nationally representative sample. Additionally, respondents with bipolar disorder reported significantly greater hospitalizations, direct healthcare costs, and indirect costs as well as worse HRQoL compared to a matched sample of the general population without bipolar disorder.
Previous estimates of per patient annual all-cause healthcare costs for patients with bipolar disorder ranged from $11,051 to $46,971 (2018 USD) with mental health-related costs accounting for approximately half of direct medical costs (range from literature = $6374–$21,523, 2018 USD) [25]. The current study is aligned with those findings with per patient annual direct healthcare costs of $20,846. Additionally, results from this study suggest that direct healthcare costs are likely driven by patients with moderate or severe depressive symptoms. Annualized all-cause direct healthcare costs were 48–55% greater for respondents with moderate or severe compared to none/mild depressive symptom severity. Slightly greater adjusted direct healthcare costs for moderate compared to severe depressive symptom severity were likely due to greater non-mental health-related hospitalizations as mental health-related hospitalizations were similar in the two cohorts (Table 2).
Multiple studies have demonstrated that depressive symptoms in patients with bipolar disorder are associated with worse work productivity, employment outcomes, and occupational functioning [14, 26, 27]. A recent post-hoc analysis of clinical trial data in patients with bipolar depression estimated annualized indirect costs due to productivity loss of $58,075–$61,235 [28]. In the current study, respondents with severe depressive symptoms (i.e., most comparable to a bipolar depression clinical trial cohort) had average indirect costs of $18,470. The difference in estimates could be due to the study population, the instrument used to measure productivity, or the methods used to estimate indirect costs. However, the current study also suggests that greater levels of depressive symptom severity may be associated with worse work outcomes; annualized indirect costs were 58–71% greater for respondents with moderate or severe compared to none/mild depressive symptom severity.
Many instruments have been used to measure HRQoL in patients with bipolar disorder [10]. EQ-5D utility scores are useful for incorporating humanistic burden in health economic assessments, and SF-36 MCS and PCS scores demonstrate the association of a condition with different aspects (mental and physical) of HRQoL. This study demonstrated that worse HRQoL in patients with bipolar disorder may be driven by moderate or severe depressive symptoms. The association was greater for mental vs. physical health-related HRQoL as measured by the SF-36 MCS and PCS scores, respectively.
In the real world, patients in the euthymic phase of illness may continue to experience worse functioning [29], sleep disturbances [30], and worse HRQoL [31] compared to the general population. Continued impacts on functioning have been associated with residual depressive symptoms [32, 33]. Although statistical significance was not tested directly for depressive symptom severity groups compared to the general population, respondents with current none/mild depressive symptom severity in this study reported greater direct healthcare costs and indirect costs and worse HRQoL compared to the general population.
The association of depressive symptom severity with worse HRQoL and higher costs underscores the importance of identifying, treating, and monitoring depressive symptoms of bipolar disorder in the clinical setting. PHQ-9 has been recommended to assess depressive symptom severity and monitor response to treatment [7]. FDA-approved treatments for acute depressive episodes associated with bipolar disorder include several second-generation antipsychotics: cariprazine, lurasidone, olanzapine-fluoxetine, lumateperone, and quetiapine [5]. While these therapies are largely successful in managing depressive symptoms, they are associated to varying degrees with side effects including weight gain, metabolic syndrome, movement disorders, and sedation [5]. Further innovation in the treatment of bipolar depression is needed to provide more clinical options for specialists and primary care practitioners caring for patients with bipolar disorder.
There were several limitations to this study. First, the diagnosis of bipolar disorder was self-reported by survey respondents and not confirmed with a physician diagnosis. The higher prevalence of bipolar disorder in this study, almost 5% vs 2.8% in other US estimates [2], suggests our sample may over-represent the bipolar disorder population in the US. Second, the outcomes of interest in this study were based on self-reported data and may be subject to recall bias. Respondents were asked to recall the past 6 months of HCRU and the past week of work productivity and HRQoL. Third, the annualization of HCRU and work productivity measures assumes that the incidence and duration of manic and depressive episodes are uniformly consistent across 12 months. Fourth, the analysis by depressive symptom severity did not control for the frequency of manic episodes in the past year, which may also be associated with hospitalizations. A detailed evaluation of manic symptom severity was not collected in the survey. Finally, this analysis was not a comprehensive study of the burden of bipolar disorder. Indirect costs related to unemployment and productivity loss for patients with bipolar disorder have been estimated to be approximately 57% of total indirect costs attributed to bipolar disorder [25]. Additional contributors to indirect costs include premature mortality, productivity loss of caregivers, and healthcare costs of caregivers [25]. However, premature mortality and caregiver information were not collected in the survey.
Conclusions
Current moderate to severe depressive symptoms were associated with greater direct healthcare costs and indirect costs as well as worse HRQoL for respondents with bipolar disorder. New therapies for the treatment of depressive symptoms may decrease the economic and humanistic burden of bipolar disorder.
Acknowledgements
We thank Barbara Blaylock, Ph.D. from Blaylock Health Economics LLC for providing medical writing support.
X. Niu was an employee of Sunovion Pharmaceuticals Inc. at the time of this research.
Previous presentations
An earlier version of this work was presented as a poster at the 2022 American Psychiatric Association Annual Meeting (New Orleans; May 21–25; 2022).
Abbreviations
- BMI
Body mass index
- CCI
Charlson Comorbidity Index
- CI
Confidence intervals
- EQ-5D
EuroQol 5-Dimension Health Questionnaire
- ER
Emergency room
- GAD-7
General Anxiety Disorder 7-item scale
- GLM
Generalized linear model
- HCRU
Healthcare resource utilization
- HRQoL
Health-related quality of life
- ICH
International Conference on Harmonisation
- IRB
Institutional Review Board
- MCS
Mental component summary
- MDD
Major depressive disorder
- MEPS
Medical Expenditure Panel Survey
- NHWS
National Health and Wellness Survey
- PCS
Physical component summary
- PHQ-9
Patient Health Questionnaire 9-item scale
- SF-36
36-Item Short Form Survey Instrument
- SF-6D
Six domains of the SF-36
- US
United States
- USD
United States Dollars
- VAS
Visual analog scale
- WPAI
Work Productivity and Activity Impairment Questionnaire
Author contributions
All authors were involved in the study design, data analysis, interpretation of results, drafting of the manuscript, and providing final review. All authors read and approved the final manuscript.
Funding
This study was funded by Sunovion Pharmaceuticals Inc.
Availability of data and materials
This study used data from the 2020 US NHWS, which are not publicly available.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with ethical principles consistent with the Declaration of Helsinki and International Conference on Harmonisation (ICH), Good Clinical Practice, Good Pharmacoepidemiology Practice. All respondents explicitly agreed to participate in the NHWS and were provided fair-market value incentives for participation. The 2020 US NHWS was reviewed and approved by the Pearl Institutional Review Board (IRB; Indianapolis, IN, USA). Data were anonymized for use in this study and, as such, did not require further IRB approval.
Consent for publication
Not applicable.
Competing interests
CD and TG are employees of Sunovion. XN was an employee of Sunovion at the time of this research. dM and KM are employees of Cerner Enviza, an Oracle company, which received funding from Sunovion to conduct this analysis. YZ is a postdoctoral research fellow at the Center for the Evaluation of Value and Risk in Health and at Sunovion.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carvalho AF, Firth J, Vieta E. Bipolar disorder. N Engl J Med. 2020;383(1):58–66. doi: 10.1056/NEJMra1906193. [DOI] [PubMed] [Google Scholar]
- 2.Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68(3):241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fagiolini A, Forgione R, Maccari M, Cuomo A, Morana B, Dell'Osso MC, et al. Prevalence, chronicity, burden and borders of bipolar disorder. J Affect Disord. 2013;148(2–3):161–169. doi: 10.1016/j.jad.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Forte A, Baldessarini RJ, Tondo L, Vázquez GH, Pompili M, Girardi P. Long-term morbidity in bipolar-I, bipolar-II, and unipolar major depressive disorders. J Affect Disord. 2015;178:71–78. doi: 10.1016/j.jad.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Baldessarini RJ, Vázquez GH, Tondo L. Bipolar depression: a major unsolved challenge. Int J Bipolar Disord. 2020;8(1):1. doi: 10.1186/s40345-019-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almeida OP, Dols A, Blanken M, Rej S, Blumberg HP, Villa L, et al. Physical health burden among older men and women with bipolar disorder: results from the Gage-Bd Collaboration. Am J Geriatr Psychiatry. 2022;30(6):727–732. doi: 10.1016/j.jagp.2021.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Huang H, Nissen N, Lim CT, Gören JL, Spottswood M, Huang H. Treating bipolar disorder in primary care: diagnosis, pharmacology, and management. Int J Gen Med. 2022;15:8299–8314. doi: 10.2147/IJGM.S386875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gitlin MJ, Miklowitz DJ. The difficult lives of individuals with bipolar disorder: a review of functional outcomes and their implications for treatment. J Affect Disord. 2017;209:147–154. doi: 10.1016/j.jad.2016.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012;14(1):6–18. doi: 10.1111/j.1399-5618.2011.00969.x. [DOI] [PubMed] [Google Scholar]
- 11.Michalak EE, Yatham LN, Lam RW. Quality of life in bipolar disorder: a review of the literature. Health Qual Life Outcomes. 2005;3:72. doi: 10.1186/1477-7525-3-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nevarez-Flores AG, Sanderson K, Breslin M, Carr VJ, Morgan VA, Neil AL. Systematic review of global functioning and quality of life in people with psychotic disorders. Epidemiol Psychiatr Sci. 2019;28(1):31–44. doi: 10.1017/S2045796018000549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cotrena C, Branco LD, Shansis FM, Fonseca RP. Predictors of quality of life in bipolar disorder: a path analytical study. Psychiatry Res. 2020;285:112846. doi: 10.1016/j.psychres.2020.112846. [DOI] [PubMed] [Google Scholar]
- 14.Kato T, Baba K, Guo W, Chen Y, Nosaka T. Impact of bipolar disorder on health-related quality of life and work productivity: estimates from the national health and wellness survey in Japan. J Affect Disord. 2021;295:203–214. doi: 10.1016/j.jad.2021.07.104. [DOI] [PubMed] [Google Scholar]
- 15.Miller CJ, Abraham KM, Bajor LA, Lai Z, Kim HM, Nord KM, et al. Quality of life among patients with bipolar disorder in primary care versus community mental health settings. J Affect Disord. 2013;146(1):100–105. doi: 10.1016/j.jad.2012.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khafif TC, Belizario GO, Silva M, Gomes BC, Lafer B. Quality of life and clinical outcomes in bipolar disorder: an 8-year longitudinal study. J Affect Disord. 2021;278:239–243. doi: 10.1016/j.jad.2020.09.061. [DOI] [PubMed] [Google Scholar]
- 17.Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;226:45–51. doi: 10.1016/j.jad.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 22.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maruish M, Kosinski M, Bjorner J, Gandek B, Turner-Bowker D, Ware J. User's manual for the SF-36v2 health survey. 3. London: Quality Metric Incorporated; 2011. [Google Scholar]
- 24.Bureau of Labor Statistics . Employment and wages, annual averages 2019. Washington: US Department of Labor; 2019. [Google Scholar]
- 25.Bessonova L, Ogden K, Doane MJ, O'Sullivan AK, Tohen M. The economic burden of bipolar disorder in the United States: a systematic literature review. Clinicoecon Outcomes Res. 2020;12:481–497. doi: 10.2147/CEOR.S259338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan KA, Eisenberg D, Kim HM, Lai Z, McInnis M, Kilbourne AM. Longitudinal impact of a collaborative care model on employment outcomes in bipolar disorder. J Affect Disord. 2015;188:239–242. doi: 10.1016/j.jad.2015.08.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Donnell LA, Deldin PJ, Grogan-Kaylor A, McInnis MG, Weintraub J, Ryan KA, et al. Depression and executive functioning deficits predict poor occupational functioning in a large longitudinal sample with bipolar disorder. J Affect Disord. 2017;215:135–142. doi: 10.1016/j.jad.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Niu X, Dembek C, Fan Q, Mao Y, Divino V, Burch S, et al. The impact of lurasidone on functioning and indirect costs in adults with bipolar depression: a post-hoc analysis. J Med Econ. 2022;25(1):152–159. doi: 10.1080/13696998.2022.2030147. [DOI] [PubMed] [Google Scholar]
- 29.Léda-Rêgo G, Bezerra-Filho S, Miranda-Scippa Â. Functioning in euthymic patients with bipolar disorder: a systematic review and meta-analysis using the Functioning Assessment Short Test. Bipolar Disord. 2020;22(6):569–581. doi: 10.1111/bdi.12904. [DOI] [PubMed] [Google Scholar]
- 30.Jermann F, Perroud N, Favre S, Aubry JM, Richard-Lepouriel H. Quality of life and subjective sleep-related measures in bipolar disorder and major depressive disorder. Qual Life Res. 2021;31:117–124. doi: 10.1007/s11136-021-02929-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pascual-Sánchez A, Jenaro C, Montes-Rodríguez JM. Quality of life in euthymic bipolar patients: a systematic review and meta-analysis. J Affect Disord. 2019;255:105–115. doi: 10.1016/j.jad.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 32.Miller S, Dell'Osso B, Ketter TA. The prevalence and burden of bipolar depression. J Affect Disord. 2014;169(Suppl 1):S3–11. doi: 10.1016/S0165-0327(14)70003-5. [DOI] [PubMed] [Google Scholar]
- 33.Bonnín CM, Jiménez E, Solé B, Torrent C, Radua J, Reinares M, et al. Lifetime psychotic symptoms, subthreshold depression and cognitive impairment as barriers to functional recovery in patients with bipolar disorder. J Clin Med. 2019;8(7):1046. doi: 10.3390/jcm8071046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study used data from the 2020 US NHWS, which are not publicly available.