Abstract
Background
Previous studies have shown that perioperative dexmedetomidine could reduce the incidence of postoperative AKI in cardiovascular surgery, however, its effectiveness in the non-cardiovascular surgery patient population has not been reported. The aim of this study was to investigate the effect of intraoperative dexmedetomidine on the incidence of postoperative AKI and postoperative ICU admissions in patients undergoing non-cardiovascular surgery.
Design and setting
A single-center retrospective cohort study obtained from the database of the Center for Anesthesia and Surgery, the Third Xiangya Hospital.
Patients
Inpatients between 18 and 75 years of age who were admitted to our hospital for non-cardiovascular surgery from 2012 to 2019.
Results
Overall 2391 patients who used dexmedetomidine intraoperatively were analyzed in comparison to 4552 patients who did not use dexmedetomidine after one-to-two matching. The two cohorts had similar baseline values and demographic characteristics. The incidence of AKI was lower in patients with intraoperative dexmedetomidine use than in the nonuse group (OR 0.60, p < .001). The rate of severe renal failure needing dialysis was also lower than in the nonuse group (β = –0.02, p < .05). After adjusting for confounding factors, the rate of AKI was still lower in the dexmedetomidine group. The rate of postoperative ICU admissions and in-hospital deaths were similar in the two groups (p > .05).
Conclusion
For non-cardiovascular surgery patient population, intraoperative use of dexmedetomidine was associated with a lower incidence and less severity of postoperative AKI. However, there was no significant correlation with postoperative ICU occupancy or in-hospital mortality. Further prospective RCTs are needed in the future.
Keywords: Dexmedetomidine, acute kidney injury, non-cardiovascular surgery, retrospective study
Introduction
Acute kidney injury (AKI) is a common clinical syndrome with a prevalence of up to 15% in hospitalized patients and a high mortality rate [1]. Major surgery, sepsis, and medications are all common clinical causes of AKI [2]. The incidence of AKI is significantly higher in surgical patients than in non-surgical patients, and its occurrence carries a higher mortality and medical burden. Due to the sensitivity of the kidney to hemodynamic changes, major surgical stresses such as intraoperative bleeding, vascular injury, and vasoconstriction as well as venous congestion can easily lead to reduced renal blood flow resulting in ischemia and reperfusion injury to the kidney, leading to postoperative AKI [3–5]. Dexmedetomidine, a selective α2-adrenoceptor agonist, is a commonly used sedative and analgesic drug [6]. Studies have shown that the sympathetic inhibition of dexmedetomidine may lead to improved renal hemodynamics through vasodilatation, and may also improve sodium and water regulation by inhibiting renin secretory agents, thereby improving the outcome of AKI [7,8]. Data from clinical studies have shown that dexmedetomidine reduces the incidence of postoperative AKI in patients undergoing aortic dissection or cardiac surgery [9,10]. However, the effect of intraoperative dexmedetomidine use on postoperative AKI in patients undergoing non-cardiovascular surgery (cardiac surgery and arterial coarctation surgery) has not been reported. The aim of this study was to investigate the effect of dexmedetomidine on postoperative AKI incidence and severity in patients undergoing non-cardiovascular surgery and the effect on postoperative ICU admissions and in-hospital mortality.
Method
Data source and population
This is a single-center retrospective cohort study with data obtained from the electric medical record system of the Center for Anesthesia and Surgery, Third Xiangya Hospital, Central South University. Inpatients between 18 and 75 years old admitted to our hospital for non-cardiovascular surgery from 2012 to 2019 were included in this study. Exclusion criteria: cardiac surgery, arterial entrapment surgery, nephrectomy and renal or liver transplantation, perioperative use nephrotoxic drugs or therapies that may impair kidney (e.g., nephrotoxic antibiotics, antitumor platinum drugs, specific herbal medicine and contrast media), lack of renal function testing or preoperative impaired renal function whether it were considered as acute kidney injury or chronic kidney disease.
Data collection included (1) gender age, body mass index (BMI); (2) personal history including preoperative comorbidities and medication history; (3) laboratory test data including serum creatinine and eGFR (calculated using the CKD-EPI formula), hemoglobin, and albumin levels; (4) surgical data including whether the surgery was emergency, surgical classification, type of anesthesia, length of surgery, intraoperative fluid volume, bleeding volume, blood transfusion volume, intraoperative blood pressure and whether vasoactive drugs were used.
All clinical data of the 27,166 patients who had undergone non-cardiac surgery were obtained by a retrospective analysis from the computerized patient record system of our hospital. Definitions: Postoperative AKI was defined according to the Kidney Disease: Improving Global Outcomes 2012 creatinine criteria, as one of the following: an increase in serum creatinine by ≥0.3 mg/dL within 48 h or ≥1.5 times increase in serum creatinine from baseline within seven postoperative days [3]. The baseline serum creatinine level was recorded using the lowest value during preoperative days [11]. The primary outcome was the impact of Dexmedetomidine on AKI, defined as AKI occurring within seven days after the operation as our previous report [11]. Diabetes and hypertension were defined in accordance with the WHO diagnostic criteria for diabetes and hypertension [12,13]. History of smoking was defined as those who smoked more than 1 cigarette per day for more than 6 months, and history of alcohol consumption was defined as those who consumed alcohol more than 1 time per month for more than 6 months.
Method of dexmedetomidine administration
The intraoperative use of dexmedetomidine were conducted during the last 30–40 min of the surgery via bolus or microdosis venous pump at a dosage 0.6–1.2 mcg/kg/h according to the drug instruction and anesthetist’s preference. The treatment usually lasted for 30 min and will not continue after the surgery.
Statistical analysis
All statistical analyses were performed using CRAN R (V.4.1.6). Multiple imputation was used for missing covariate data (including BMI and eGFR). For continuous variables, the mean value is expressed in a standard deviation (SD) form, while for categorical variables, the numbers are expressed as percentages. When comparing continuous variables between groups, Kruskal-Wallis rank sum tests were used, while categories were compared with Fisher’s exact probability tests.
Based on age, sex, and BMI, we performed propensity score matching. The development of AKI was significantly associated with epidemiological, preoperative laboratory, and intraoperative factors analyzed using univariable logistic regression analysis. Multivariable regression models were adjusted for potential confounders. Sensitivity test was performed in the following four different subgroups: eGFR ≥ 90mL/min·1.73/m2, non-diabetes, blood loss <1000 mL and non-NSAIDs drug.
In general, results are expressed as ‘beta’ or OR with 95%CI. A statistically significant difference was indicated by a p < .05.
Results
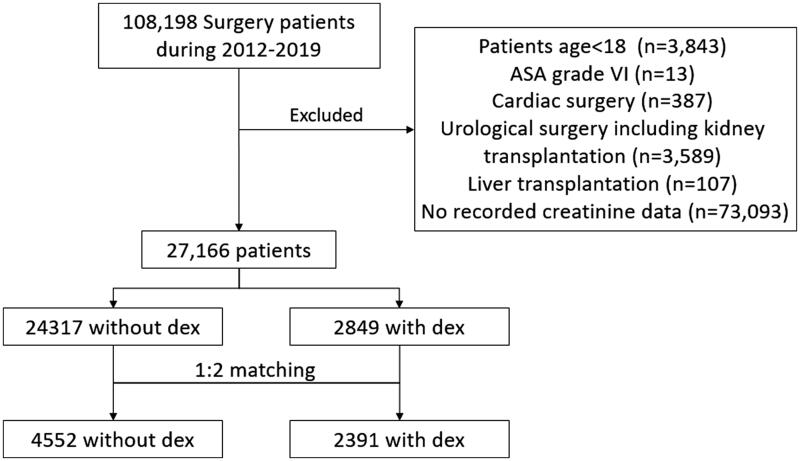
A total of 27,166 surgical patients (including gastrointestinal operations, Hepatobiliary and pancreatic surgery, Gynecologic operation, and tumor surgery et al.) were included in this study, of which 2,849 patients received intraoperative dexmedetomidine treatment and 24,317 did not receive dexmedetomidine treatment. After 1:2 propensity score matching (PSM), we identified 2391 non-cardiovascular surgical patients who received intraoperative dexmedetomidine treatment between January 2012 and December 2018 and 4552 surgical patients who did not receive dexmedetomidine (Figure 1). Of note the proportion of laparoscopic surgery (laparoscopy: 21.25% vs. 19.97%, p = .062) as well as the robot surgery (robot surgery: 4.21% vs. 3.98%, p = .069) were comparable among the two groups. Data on baseline demographic characteristics, comorbidities, preoperative biochemical tests, and intraoperative conditions for both groups of patients before and after PSM matching are presented in Table 1. Although a PSM matching were conducted, the baseline data still showed that a group of demographic characteristics are significantly different between control and dexmedetomidine group after matching, like alcohol intake, smoking, diuretics, type of anesthesia, use of NSAIDs, these factors are clinical relevant and favored dexmedetomidine group. While another factor like operative time which favored the control group was also significantly different. Other factors including preoperative eGFR, ASA grade (except the number of ASA 4 category), amount of fluid out and lowest MAP are significantly different but clinically irrelevant between groups. For all those differences in baseline characteristics, we subsequently did univariable analysis in Table 2 to identify potential influence factors. And we further conducted a multivariable regression analysis in Table 3 to remove potential influence factors and confounding factors based on the results of univariable analysis.
Figure 1.
Inclusion of study patients. Dex: Dexmedetomidine, 1:2 matching: propensity score matching.
Table 1.
Baseline characteristics.
| Before matching |
After matching |
|||||
|---|---|---|---|---|---|---|
| Variable | Control (n = 24317) |
Dexmedetomidine (n = 2849) | p value | Control (n = 4552) |
Dexmedetomidine (n = 2391) |
p value |
| Demographics | ||||||
| Age, year | 53.37 ± 14.43 | 53.72 ± 14.67 | .217 | 53.23 ± 13.78 | 53.24 ± 14.17 | .846 |
| Male, % | 47.1 | 52.5 | <.001 | 47.2 | 46.8 | .707 |
| BMI (kg/m2) | 22.92 ± 3.58 | 23.31 ± 3.59 | <.001 | 22.78 ± 2.98 | 22.98 ± 3.07 | .078 |
| Alcohol, % | 5.2 | 2.5 | <.001 | 5.8 | 2.7 | <.001 |
| Smoking, % | 8.0 | 3.3 | <.001 | 7.2 | 4.6 | .006 |
| Hypertension, % | 21.3 | 20.5 | .286 | 18.7 | 17.5 | .231 |
| Diabetes, % | 12.4 | 11.3 | .11 | 7.6 | 6.5 | .13 |
| Diuretics, % | 2.1 | 0.7 | <.001 | 1.8 | 0.8 | <.001 |
| ACEI/ARB, % | 1.1 | 0.5 | .002 | 0.6 | 0.5 | .411 |
| CCB, % | 0.13 | 0.04 | .283 | 0.1 | 0.5 | .691 |
| Pre-operative conditions | ||||||
| Hemoglobin, g/L | 122.64 ± 22.69 | 125.23 ± 22.31 | <.001 | 124.12 ± 22.33 | 125.01 ± 20.01 | .021 |
| Serum albumin, g/L | 39.73 ± 5.53 | 39.90 ± 5.08 | .121 | 39.88 ± 5.20 | 40.04 ± 5.00 | .797 |
| Pre-operation eGFR (mL/min) | 97.62 ± 23.59 | 99.74 ± 20.85 | <.001 | 97.55 ± 22.79 | 100.44 ± 20.79 | <.001 |
| Surgical data | ||||||
| ASA grade, % | <.001 | <.001 | ||||
| 1 | 5.7 | 5 | 6.02 | 5.47 | ||
| 2 | 55.3 | 54.9 | 57.14 | 57.34 | ||
| 3 | 33.8 | 37 | 32.27 | 34.63 | ||
| 4 | 5.2 | 3.2 | 4.57 | 2.55 | ||
| Anesthesia method, % | ||||||
| General anesthesia, % | 89.4 | 78.4 | <.001 | 90.05 | 78.21 | <.001 |
| Non-general anesthesia, % | 10.6 | 21.6 | <.001 | 9.95 | 21.29 | <.001 |
| Amount of fluid infusion, (mL/24 hours) | 2100 (1500–3100) | 2100 (1500–3100) | .685 | 2100 (1500–3100) | 2100 (1500–3100) | .352 |
| Amount of fluid out (mL/24 hours) | 500 (300–900) | 600 (300–1000) | <.001 | 550 (300–909) | 600 (300–1000) | <.001 |
| Amount of blood loss, mL | 150 (50–400) | 200 (50–400) | .013 | 200 (50–400) | 200 (50–400) | .984 |
| Operative time, min | 151 (103–220) | 175 (120–253) | <.001 | 158 (105–224) | 175 (120–250) | <.001 |
| Lowest MAP, mmHg | 61.29 ± 14.64 | 58.87 ± 17.03 | <.001 | 61.42 ± 14.77 | 58.86 ± 16.82 | <.001 |
| Duration of hypotension, min | 15 (10, 22) | 17 (12, 25) | .442 | 15 (10, 21) | 15 (11, 22) | .591 |
| Vasoactive drugs, % | 8.5 | 8.4 | .729 | 7.7 | 7.9 | .725 |
| NSAIDS, % | 24.1 | 18.8 | <.001 | 25.13 | 19.41 | <.001 |
Baseline characteristics of the patients who received Dexmedetomidine versus who did not before and after propensity score matching. ACEI: ACE inhibitors; AKI: acute kidney injury; ARB: angiotensin receptor blockers; ASA: American Society of Anesthesiologist; BMI: body mass index; CCB: calcium-channel blockers; eGFR: estimated glomerular filtration rate: MAP: mean arterial pressure. Vasoactive drugs include ephedrine and metaraminol: NSAIDs: Non-steroidal anti-inflammatory drugs; Parecoxib (40–80mg) or Flurbiprofen (50–100mg).
Table 2.
Univariable analysis.
| Variable | Statistics | Univariable OR (95% CI) |
p value |
|---|---|---|---|
| Dexmedetomidine, % | 2391 (34.44%) | 0.60 (0.59, 0.81) | <0.001 |
| Male, % | 3268 (47.07%) | 0.71 (0.55, 0.92) | 0.010 |
| Age, year | 53.22 ± 13.91 | 1.02 (1.01, 1.03) | <0.001 |
| BMI (kg/m2) | 22.99 ± 2.85 | 0.97 (0.92, 1.01) | 0.1167 |
| Alcohol, % | 326 (4.70%) | 0.89 (0.53, 1.48) | 0.640 |
| Smoking, % | 487 (7.01%) | 1.22 (0.77, 1.92) | 0.394 |
| Hypertension, % | 1267 (18.25%) | 1.74 (1.31, 2.31) | <0.001 |
| Diabetes, % | 501 (7.22) | 2.11 (1.60, 2.77) | <0.001 |
| Vasoactive drugs, % | 538 (7.75%) | 3.55 (2.73, 4.61) | <0.001 |
| Diuretics, % | 97 (1.40%) | 5.56 (3.20, 9.65) | <0.001 |
| ACEI, % | 39 (0.56%) | 1.44 (0.35, 6.03) | 0.614 |
| CCB, % | 4 (0.06%) | 0.00 (0.00, inf.) | 0.969 |
| Hb (g/L) | 124.60 ± 22.27 | 0.98 (0.97, 0.98) | <0.001 |
| Alb (g/L) | 40.04 ± 5.13 | 0.89 (0.88, 0.92) | <0.001 |
| Preoperation eGFR (mL/min) | 98.55 ± 21.92 | 0.98 (0.97, 0.98) | <0.001 |
| ASA, % | |||
| 1 | 405 (5.83%) | 1 | |
| 2 | 3972 (57.21%) | 1.62 (0.65, 4.03) | 0.297 |
| 3 | 2297 (33.08%) | 4.49 (1.82, 11.04) | <0.001 |
| 4 | 269 (3.87%) | 16.07 (6.29, 41.07) | <0.001 |
| General anesthesia, % | 5981 (86.14%) | 1.03 (0.71, 1.48) | 0.885 |
| Amount of fluid infusion (mL/24 h) | 2100 (1500–3100) | 1.00 (1.00, 1.00) | 0.019 |
| Amount of fluid out, mL | 600 (300–900) | 1.00 (1.00, 1.00) | 0.180 |
| Amount of blood loss (mL/24 h) | 200 (50–400) | 1.00 (1.00, 1.00) | <0.001 |
| Operative time, min | 165 (110–234) | 1.00 (1.00, 1.00) | 0.059 |
| Lowest MAP, mmHg | 60.54 ± 15.55 | 0.99 (0.98, 1.00) | 0.067 |
| Duration of hypotension, min | 15 (10, 22) | 0.99 (0.98, 1.00) | 0.073 |
| NSAIDs, % | 1608 (23.16%) | 0.64 (0.45, 0.90) | <0.001 |
Univariable analysis of AKI incidence. ACEI: ACE inhibitors; AKI: acute kidney injury; ARB: angiotensin receptor blockers; BMI: body mass index; CCB: calcium-channel blockers; ASA: American Society of Anesthesiologists; eGFR: estimate glomerular filtration rate.
Table 3.
Multivariable regression analysis.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| |
OR/β (95% CI) p value |
|||
| AKI (OR) | 0.60 (0.59, 0.81) <0.001 | 0.66 (0.49, 0.89) <0.001 | 0.68 (0.51, 0.92) 0.012 | 0.71 (0.52, 0.97) 0.034 |
| AKI stages (β) | –0.02 (–0.03, −0.01) <0.001 | –0.02 (–0.03, −0.00) <0.001 | –0.02 (–0.03, −0.00) 0.009 | –0.01 (–0.02, −0.00) 0.044 |
Multivariable regression analysis of AKI incidence. AKI stages (outcome of postoperative AKI was divided into four groups: stage 0, no AKI; stage 1, AKI grade 1; stage 2, AKI grade 2 and stage 3, AKI grade 3).
Model 1: non-adjusted.
Model 2: adjusted for age, sex, eGFR.
Model 3: model 2 plus hypertension, diabetes, diuretics.
Model 4: model 3 plus blood lossed, vasoactive drugs, Hb, Alb, amount of fluid infusion and out, operative time, ASA, lowest MAP and NSAIDs.
Postoperative AKI and in-hospital death
The incidence of postoperative AKI and the rate of ICU admission (non-planed) and death during hospitalization are presented in Table 4 for both groups before and after matching. The percentage of patients with different grades of AKI is also presented. The results show that the overall incidence of AKI was lower in the dexmedetomidine group than in the non-dexmedetomidine group whether before or after matching (before:4.4% vs. 3.3%, after: 4.2% vs. 2.6%), and the proportion of patients requiring dialysis for severe AKI was significantly lower in the dexmedetomidine group than in the control group (0.21% vs 0.04%). In addition, the results showed that the proportion of patients with unplanned ICU admission after surgery were 4.45% and 4.63 respectively, and the postoperative in-hospital mortality rate was 0.60% and 0.63% respectively, which were not statistically different between the two groups.
Table 4.
Post-operation outcomes.
| Before matching |
After matching |
|||||
|---|---|---|---|---|---|---|
| Out come | Control (n = 24,317) |
Dexmedetomid ine (n = 2849) |
p value | Control (n = 4552) |
Dexmedetomidine (n = 2391) |
p value |
| Post-operation eGFR (mL/min) | 92.41 ± 21.30 | 97.24 ± 23.63 | <.001 | 94.84 ± 21.41 | 97.84 ± 23.14 | <.001 |
| AKI,% | 4.4 | 3.3 | .008 | 4.2 | 2.6 | <.001 |
| AKI stages,% | .026 | .003 | ||||
| 0 | 95.61 | 96.67 | 95.83 | 97.45 | ||
| 1 | 3.98 | 2.98 | 3.76 | 2.30 | ||
| 2 | 0.22 | 0.28 | 0.20 | 0.21 | ||
| 3 | 0.19 | 0.07 | 0.21 | 0.04 | ||
| ICU admission,% | 4.68 | 4.73 | .845 | 4.45 | 4.63 | .872 |
| Death (in hospital), % | 0.63 | 0.62 | .865 | 0.60 | 0.63 | .625 |
Perioperative outcomes of the patients who received Dexmedetomidine versus who did not after propensity score matching. ICU, intensive care unit.
Univariable analysis and multivariable regression analysis
Univariate analysis (Table 2) showed that the use of dexmedetomidine, female, preoperative albumin, and preoperative NSAIDs were associated with a lower risk of AKI, whereas age >60, hypertension, diabetes mellitus, preoperative vasoactive drugs, and diuretics used 1 week before surgery were associated with a higher risk of postoperative AKI. A corrected multifactorial analysis still showed that dexmedetomidine use was independently associated with a lower incidence of AKI (OR = 0.60, 0.66, 0.68, 0.71, p < .05 for all four models) and reduced the severity of AKI (β = –0.02, −0.02, −0.02, −0.01, p < .05 for all four models) after removing the effects of gender, albumin, NSAIDs, underlying disease hypertension (Table 3).
Subgroup analysis
We also analyzed the effect of dexmedetomidine on AKI in particular subgroups (Table 5) including those with eGFR greater than 90 mL/min, those who had less than 1000 mL of intraoperative bleeding, and those who did not use NASAIDs, respectively. The results showed that dexmedetomidine reduced the incidence (OR = 0.5, 0.62, 0.57, 0.71, p < .05) of AKI in all three different subgroups without adjustment, respectively, and that the differences remained statistically significant after correction with different factors (four models) (Table 5).
Table 5.
Subgroup analysis of the association between postoperative AKI and Dexmedetomidine.
| Model 1 | Model 2 | Model 3 | Model 4 | ||
|---|---|---|---|---|---|
| AKI |
|
OR (95% CI) p value |
|||
| Non-Dex | Dex | ||||
| eGFR > 90 (mL/min), n = 4908 |
1 | 0.50 (0.33, 0.75) <0.001 | 0.49 (0.32, 0.74) <0.001 | 0.49 (0.33, 0.75) <0.001 | 0.51 (0.37, 0.79) 0.003 |
| Blood loss < 1000 mL, n = 6384 |
1 | 0.62 (0.45, 0.86) 0.004 | 0.69 (0.50, 0.96) 0.029 | 0.70 (0.50, 0.98) 0.038 | 0.70 (0.50, 0.98) 0.039 |
| NSAIDs = 0, n = 5335 |
1 | 0.57 (0.41, 0.78) <0.001 | 0.65 (0.47, 0.90) <0.001 | 0.67 (0.49, 0.93) 0.018 | 0.67 (0.48, 0.95) 0.027 |
The association between postoperative AKI and Dexmedetomidine in different subgroups. Dex, Dexmedetomidine.
AKI stages (outcome of postoperative AKI was divided into four groups: stage 0, no AKI; stage 1, AKI grade 1; stage 2, AKI grade 2 and stage 3, AKI grade 3).
Model 1: non-adjusted.
Model 2: adjusted for age, sex, eGFR.
Model 3: model 2 plus hypertension, diabetes, diuretics.
Model 4: model 3 plus blood lossed, vasoactive drugs, Hb, Alb, amount of fluid infusion and out, operative time, ASA, lowest MAP and NSAIDs.
Discussion
In the present single-center retrospective study, we reported that intraoperative use of dexmedetomidine was associated with a reduction in the incidence and severity of postoperative AKI in patients undergoing non-cardiovascular surgery. While, there was no significant association between dexmedetomidine use and postoperative ICU admission or in hospital mortality. Postoperative AKI, even of low grade, can significantly increase the risk of patients’ mortality, prolong hospitalization, and increase the economic burden [14]. The data reported in our center suggest that the incidence of AKI after non-cardiovascular surgery is 4.8% which is generally close to the report Murat Biteker’s study [15]. In contrast, the incidence of AKI after cardiovascular surgery is much higher [16]. Although studies have reported the benefit of sympathetic blocking drugs for postoperative AKI in cardiac surgery and arterial entrapment surgical fidelity, however, there are no comprehensive data reported for population of non-cardiovascular surgery patient.
Dexmedetomidine is a α2-adrenoceptor agonist that reduces sympathetic nervousness and catecholamine levels [6]. It also induces sedation and analgesia, stabilizes hemodynamics, and has anti-inflammatory and diuretic effects. In basic experiments, it has been reported that dexmedetomidine could inhibit the release of epinephrine and norepinephrine, thereby reducing sympathetic adrenal hyperactivity due to surgical stress and thus improving renal hemodynamics, especially in the context of ischemic renal injury [17]. Studies have shown that ischemic renal injury is often associated with increased adrenaline and sympathetic excitation. It has also been shown that dexmedetomidine can reduce inflammatory response, which is also an important pathological factor in the pathogenesis of AKI, especially ischemia-related AKI [14,17]. A prospective RCT reported that dexmedetomidine administered for 24 h from induction of anesthesia significantly reduced the incidence and severity of postoperative AKI as well as the length of postoperative ICU stay and mortality in patients undergoing cardiovascular surgery [18]. These findings strongly support the protective effect of dexmedetomidine on postoperative AKI in patients undergoing major cardiovascular surgery. In this study, in order to further investigate the effect of dexmedetomidine on AKI in patients undergoing routine surgery, patients undergoing major cardiac surgery, aortic dissection and renal transplantation and nephrectomy were excluded to reduce confounding factors. The results still showed a negative correlation between dexmedetomidine and the risk of AKI in this population. A protective effect of dexmedetomidine against complications of AKI has also been reported in patients undergoing abdominal cytoreductive surgery, renal transplantation, and sepsis [19–21]. Animal studies have also shown a protective effect of dexmedetomidine in the kidney of mice with cisplatin-induced AKI [22]. These clinical or basic studies suggest a more comprehensive renoprotective effect of dexmedetomidine. Our results combined with literature reports strongly suggest that dexmedetomidine has a positive effect against AKI in different clinical settings.
Interestingly, in our single-center retrospective observation, we found that women, preoperative albumin (35–45 g/L), and preoperative use of nonsteroidal drugs were associated with a lower risk of AKI; whereas age >60, hypertension, diabetes, preoperative use of vasoactive drugs, preoperative diuretics within 1 week were associated with a higher risk of postoperative AKI. It is widely recognized that old age and hypertensive, diabetic complications can increase the risk of AKI [14], and the correlation between high risk of AKI and preoperative use of diuretics in our study is consistent with previous reports [11]. While the data of NSAIDs usage were also associated with a relatively lower risk of AKI incident which is consistent with our recent study of Parecoxib [11].
As to the AKI stages, our analysis showed that numbers of stage 2 patients were close between the two groups. While AKI stage 1 and 3 are less in the dexmedetomidine group, particularly stage 3 patients who need dialysis treatment. These indicate that dexmedetomidine usage is associated with less severity of AKI after surgery. After correction for all these factors by multivariable regression analysis, we still observed a negative effect of dexmedetomidine on postoperative AKI. Although there was no difference between the two groups in terms of postoperative ICU admission and in-hospital mortality, our study provides strong evidence for the protective effect of intraoperative dexmedetomidine use on postoperative AKI in non-diabetic patients undergoing conventional surgery.
Limitation
This study is a single-center retrospective study with some inevitable statistical bias, in addition to the short duration of observation, limited data on postoperative follow-up, untested prognosis for longer periods of time, and failure to obtain potential clinical biochemical inflammatory indicators. A number of variables from the baseline characteristics showed differences between the dexmedetomidine and control groups respectively in Table 1. Some of these variables did have impact on the effect of dexmedetomidine and those data were presented in Table 2 by univariable analysis. As a limitation of a retrospective study we cannot fully avoid those confounding factor, even though we did the propensity score matching and try to reduce the variables factors. Moreover, patients’ preoperative renal function was assessed only by creatinine methods, and the frequency of monitoring varied from person to person, and data on urinary output were incomplete, so there could also be patients with abnormal preoperative renal function who were not monitored.
Conclusion
This study is the first to examine the effect of intraoperative use of dexmedetomidine on postoperative AKI in patients undergoing non-cardiovascular surgery. Patients with intraoperative dexmedetomidine treatment had a lower risk of AKI or severe AKI requiring dialysis treatment. However, there was no significant association regarding to postoperative ICU admissions and in-hospital deaths. Future prospective randomized controlled multicenter trials with large sample are needed to further confirm the protective effect of dexmedetomidine on postoperative AKI and other prognostic effects in this population.
Funding Statement
This work was supported by grants from the National Natural Sciences Foundation of China [No.81900633], the Natural Sciences Foundation of Hunan Province [No. 2021JJ40954, No. 2020JJ5854].
Ethics statement
This study was approved by the ethics committee of the third Xiangya hospital of Central South University (2020S264). Because of the observational nature of the study, informed consent was waived.
Author contributions
Y-ZT helped in designing the study, analyzing and interpreting the data, Q W helped in data collection and checking and drafting and revising the manuscript. Z L and X L helped in collecting, analyzing and interpreting the data, and revising the manuscript. Y L and Q L helped in analyzing and interpreting the data. B L helped in supervising, funding acquisition and drafting and revising the manuscript. W Z helped in designing the study, analyzing and interpreting the data and drafting and revising the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The raw data of experiments used to support the findings of this study are available from the corresponding author upon request.
References
- 1.Bellomo C, Kellum R, Ronco JA.. Acute kidney injury. Lancet. 2019;394(10212):1949–1964. [DOI] [PubMed] [Google Scholar]
- 2.Scholz H, Boivin FJ, Schmidt-Ott KM, et al. Kidney physiology and susceptibility to acute kidney injury: implications for renoprotection. Nat Rev Nephrol. 2021;17(5):335–349. [DOI] [PubMed] [Google Scholar]
- 3.Hoste EAJ, Kellum JA, Selby NM, et al. Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14(10):607–625. [DOI] [PubMed] [Google Scholar]
- 4.Medve C, Gondos L, Kopitko T.. The value of combined hemodynamic, respiratory and intra-abdominal pressure monitoring in predicting acute kidney injury after major intraabdominal surgeries. Ren Fail. 2019;41(1):150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopitkó C, Gondos T, Fülöp T, et al. Reinterpreting renal hemodynamics: the importance of venous congestion and effective organ perfusion in acute kidney injury. Am J Med Sci. 2020;359(4):193–205. [DOI] [PubMed] [Google Scholar]
- 6.Coursin DB, Maccioli DB, Coursin GA.. Dexmedetomidine. Curr Opin Crit Care. 2001;7(4):221–226. [DOI] [PubMed] [Google Scholar]
- 7.Myles PS, Hunt JO, Holdgaard HO, et al. Clonidine and cardiac surgery: haemodynamic and metabolic effects, myocardial ischaemia and recovery. Anaesth Intensive Care. 1999;27(2):137–147. [DOI] [PubMed] [Google Scholar]
- 8.Ming S, Xie Y, Du X, et al. Effect of dexmedetomidine on perioperative hemodynamics and organ protection in children with congenital heart disease: a randomized controlled trial. Medicine. 2021;100(1):e23998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shan X-S, Dai H-R, Zhao D, et al. Dexmedetomidine reduces acute kidney injury after endovascular aortic repair of stanford type B aortic dissection: a randomized, double-blind, placebo-controlled pilot study. J Clin Anesth. 2021;75:110498. [DOI] [PubMed] [Google Scholar]
- 10.Kwiatkowski DM, Axelrod DM, Axelrod SM, et al. Dexmedetomidine is associated with lower incidence of acute kidney injury after congenital heart surgery. Pediatr Crit Care Med. 2016;17(2):128–134. [DOI] [PubMed] [Google Scholar]
- 11.Tang Y-Z, Zeng P, Liao Y, et al. Correlation between perioperative parecoxib use and postoperative acute kidney injury in patients undergoing non-cardiac surgery: a retrospective cohort analysis. BMJ Open. 2021;11(8):e047840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersmann A, Müller-Wieland D, Müller UA, et al. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2019;127(S01):S1–S7. [DOI] [PubMed] [Google Scholar]
- 13.Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137(2):109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zarbock A, Koyner JL, Hoste EAJ, et al. Update on perioperative acute kidney injury. Anesth Analg. 2018;127(5):1236–1245. [DOI] [PubMed] [Google Scholar]
- 15.Biteker M, Dayan A, Tekkeşin Aİ, et al. Incidence, risk factors, and outcomes of perioperative acute kidney injury in noncardiac and nonvascular surgery. Am J Surg. 2014;207(1):53–59. [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Bellomo R.. Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol. 2017;13(11):697–711. [DOI] [PubMed] [Google Scholar]
- 17.Tang C, Hu Y, Gao J, et al. Dexmedetomidine pretreatment attenuates myocardial ischemia reperfusion induced acute kidney injury and endoplasmic reticulum stress in human and rat. Life Sci. 2020;257:118004. [DOI] [PubMed] [Google Scholar]
- 18.Cho JS, Shim J-K, Soh S, et al. Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int. 2016;89(3):693–700. [DOI] [PubMed] [Google Scholar]
- 19.Liu Z, Jin Y, Feng C, et al. Renoprotective effect of intraoperative dexmedetomidine in renal transplantation. Comput Math Methods Med. 2022;2022:9275406. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Moriyama N, Kanmura T, Kiyonaga Y.. Effects of dexmedetomidine on lipopolysaccharide-induced acute kidney injury in rats and mitochondrial function in cell culture. Biomed Pharmacother. 2020;125:109912. [DOI] [PubMed] [Google Scholar]
- 21.Song Y, Kim D-H, Kwon TD, et al. Effect of intraoperative dexmedetomidine on renal function after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: a randomized, placebo-controlled trial. Int J Hyperthermia. 2019;36(1):1–8. [DOI] [PubMed] [Google Scholar]
- 22.Chai Y, Zhu K, Li C, et al. Dexmedetomidine alleviates cisplatininduced acute kidney injury by attenuating endoplasmic reticulum stressinduced apoptosis via the alpha2AR/PI3K/AKT pathway. Mol Med Rep. 2020;21(3):1597–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data of experiments used to support the findings of this study are available from the corresponding author upon request.