Abstract
Introduction:
Patients with hypertension should perform diverse self-care activities that incorporate medication adherence and lifestyle modification, such as no smoking or alcohol, weight reduction, a low-salt diet, increased physical activity, increased self-monitoring, and stress reduction, for effective management at home.
Aim:
This systematic review assessed and synthesized the factors that are associated with self-care and home-based management of hypertension.
Methods:
The search of the articles incorporated the population, intervention, comparison, and outcome (PICO) framework. The literature was searched in four databases (PubMed, the Cumulative Index to Nursing and Allied Health Literature [CINAHL], Embase, and Web of Science) until 2022. The articles retrieved and searched from the reference list (531) were transported to EndNote version 20, and duplicates (19) were identified and removed to produce 512 titles. Following the eventual title, abstracts, and full-text screening, 13 articles were appropriate for this study. The narrative and thematic data analysis were used to analyze and integrate the data.
Results:
The analysis showed five themes were associated with home-based self-care and blood pressure (BP) control among patients diagnosed with hypertension. These themes that emerged were (1) the prevalence of control of BP, (2) sociodemographic factors, (3) treatment-related factors, (4) knowledge of management, and (5) knowledge of the prevention of risk factors of hypertension. The demographic factors influencing home-based self-care for hypertension were gender, age, and socioeconomic status. In contrast, the treatment factors were duration of hypertension treatment, medication burden, and medication adherence. Other factors that influenced self-care were inadequate knowledge of BP management, follow-up care, and risk factors of hypertension.
Conclusion:
Hypertension self-care interventions must incorporate individual, societal, and cultural perspectives in increasing knowledge and improving home-based hypertension management. Therefore, well-designed clinical and community-dwelling interventions should integrate personal, social, and cultural perspectives to improve behavior in the home management of hypertension by increasing knowledge and self-efficacy.
Keywords: home-based management, self-care, hypertension, treatment, adherence, care
Introduction
Hypertension disease presents a challenge to patients, as they are expected to institute measures at home to ensure effective self-care and management practices. Patients with hypertension perform diverse activities that can be described as self-care activities for effective disease management [1]. The focus of hypertension self-care management must incorporate medication adherence and lifestyle modification (no smoking or alcohol, weight reduction, low-salt diet, and increased physical activity), increased self-monitoring of blood pressure (BP), and stress reduction [2]. However, self-care management in hypertensive patients must be lifelong, even though it is usually challenging and overwhelming because the patient lacks experience in self-management and the necessary knowledge, tools, and support [3]. Self-care is described as individual actions directed toward self or the environment to regulate individual functioning to improve health, reduce risk, and avoid related complications, as well as ensure general well-being [4,5]. It is important to note that self-care behavior among hypertension patients relates to BP control and prevents related complications [5]. Patient self-care and home-based management of hypertension positively affect clinical outcomes and reduce the occurrence of stroke and related cardiovascular disease [2,5]. Home-based measures are important in the patient’s likelihood of avoiding complications and effective improvement [2,4,6]. Self-care adherence is low among adults with hypertension [7] because patients are often unwilling to make recommended behavioral changes [8,9], especially in settings where lay health knowledge is averagely low.
Globally, the prevalence of hypertension has increased and shifted from developed to developing countries over the past 40 years [10]. Nearly three-quarters of hypertensive patients live in developing countries [11]. Awareness of high BP management is deficient in developing countries [12,13]. Many hypertensive patients are ignorant of their disease and treatment due to lack of health care access, distrust of Western medicine, and inadequate health literacy [12,14]. Although adherence to self-care and management is an important part of patient management to achieve hypertension treatment goals, self-care in the African population remains poor [15,16]. Therefore, it is very important to identify factors that influence hypertension self-care and management at home.
The self-care and home management of hypertension, like other chronic diseases, involve various behavioral changes that require optimal and effective medication adherence, self-efficacy, and prevention of complications [6,8,17]. Recent systematic reviews on self-care management of hypertension focused on the use of electronic-based technologies [18,19,20], the influence of self-care efficacy [6], and health promotion interventions for the prevention of hypertension [16,17,21]. However, to the best of our knowledge, no systematic review in recent times has specifically focused on the factors that influence home-based and self-care management of hypertension. This systematic review assessed and thematically synthesized the factors that are associated with self-care and home-based management of hypertension.
Methods
Study framework
The search of the articles incorporated the population, intervention, comparison, and outcome (PICO) framework. The population was patients diagnosed with hypertension and referred to home care or self-care management. There were no specific comparisons. The outcome was improved hypertension status or a reduction in BP. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework was incorporated in reporting the studies. Using the PRISMA guidelines and checklist allowed for reproducibility, transparency, and clarity in reporting the findings [22,23]. The phases of the entire study included identifying the research question, identifying relevant studies, quality appraisal, and selecting studies for inclusion.
Identification of the research question
Home and self-care management of hypertension is an essential factor that can promote the health of people diagnosed with the disease, especially in the poorest parts of the world, like sub-Saharan Africa. Therefore, interventions must be tailored toward addressing the specific determinants of hypertension self-care management. The specific research question was, what are the determinants of self-care and home management of hypertension in low-resource settings in Africa?
Identification of relevant studies
The literature search was done in four databases (PubMed, the Cumulative Index to Allied Health and Nursing Research [CINAHL], Embase, and Web of Science) up until 2022. In developing the search terms, the medical subject heading (MeSH) terms were used as the bases as well as free terms and wildcards incorporated with the appropriate Boolean operators. The search keywords were modified with the appropriate keywords to reflect the specific requirement of each database. The key terms used were first generated in PubMed and subsequently modified to sweet for each database. These primary keywords from PubMed using the PICO framework include population as “Hypertension”[MeSH] OR “High Blood Pressure” OR “Heart Disease”; Interventions as (“Self-Care”[MeSH] OR “Home Care Services”[MeSH] OR “Disease Management”[MeSH] OR “Therapeutics”[MeSH]); Comparison (Determinant* OR Predictor* OR Related OR Associated); and Outcome as “Medication Adherence” OR “Dietary Restriction” OR “Improved Physical Activity” OR “Increased Knowledge” OR “Improved Awareness.” These keywords were combined with the appropriate Boolean operators and MeSH terms where it was applicable.
Selection of studies
After conducting the initial search, each title, abstract, and full text was screened based on predetermined inclusion criteria and the identified key terms. Also, the references of selected articles were also searched to identify any additional articles that would be relevant to this study. The articles retrieved from the database search and reference list (531) were transported to EndNote version 20, and duplicates (19) were identified and removed to produce 512 titles. Following the eventual title, abstracts, and full-text screening, the total number of appropriate articles for this study was 13.
Selection criteria
Only studies that identified the factors associated with home management hypertension, regardless of the study setting, were included. The studies excluded were protocols, systematic studies (hospital service factors) that hinder diagnosis and self-monitoring of hypertension, and the factors related to the service provider (e.g., nurse, doctor), like shortage of items.
Quality appraisal
The two authors independently used the Mixed Methods Appraisal Tool (MMAT) version 2018 to assess each study for quality [24,25]. The assessment results using this tool were compared between the two researchers for similarities. Where differences were found between the results from the authors, it was discussed until a consensus was achieved. The MMAT is a quality assessment tool that appraises the methodological quality of qualitative, quantitative, and mixed methods studies. The quantitative section appropriate for appraising the articles selected for this review assessed the aim of the study, study design, methodology, recruitment of study participants, and data collection methods, including analysis, presentation of results, and discussion, as well as the conclusions. Based on the assessment, the studies can be individually rated as high, moderate, or low quality. However, the subsequent views of Hong et al. 2018 emphasized that the researcher does not need to assess the overall quality of studies using this categorization [25]. In their paper, the authors strongly recommended that a detailed presentation of the appraised findings should be done. The components of the screening questions from the MMAT include whether there were (a) the presence of clear research questions and (b) collected data addressing the research question. Based on the consensus gained during the appraisal, all the articles received an affirmative response to the two screening questions above.
The appraisal sections that were relevant for this study were the descriptive quantitative section that assessed the following criteria: (1) relevance of sampling strategy, (2) representativeness of sample to the target population, (3) appropriateness of measurements, (4) risk of nonresponse bias, and (5) appropriateness of statistical analysis. All the studies (n = 11) met the criteria of the appropriateness of the sampling strategy to answer the research question except two studies [26,27]. One study [28] assessed methodological quality using the qualitative section. The results showed an affirmation of all the qualitative appraisal questions. Another study [29] was assessed under the mixed methods section and was also affirmative to all the questions.
Data extraction and analysis
First, the two authors developed, discussed, and accepted a matrix to ensure comprehensiveness in the extracted data. The key parameters extracted from each study were the year, population and sample, study settings, outcome variable, main determinants of home care and self-care, and key findings. Second, the information of each study was transformed into narrative statements to enable the use of the thematic synthesis approach for data analysis [30,31]. Third, in this approach, codes were generated from the narratives formed; the codes were then linked to form subthemes, while similar themes were coalesced to form the main themes. The main themes incorporated in informing the report of this study were (1) the prevalence of control of BP, (2) sociodemographic factors, (3) treatment-related factors, (4) knowledge of management, and (5) knowledge of prevention of risk factors of hypertension.
Results
Through the advanced search of electronic databases using predetermined keywords (529) and a reference list of identified studies [2], about 531 studies were identified, and 19 were identified as duplicates in the endnotes. The duplicates were removed, and all 512 titles were screened through title and abstract. Based on a predetermined inclusion criterion, 41 studies were full articles, and 13 were identified as appropriate for this study. The process of article selection is shown in Figure 1.
Figure 1.
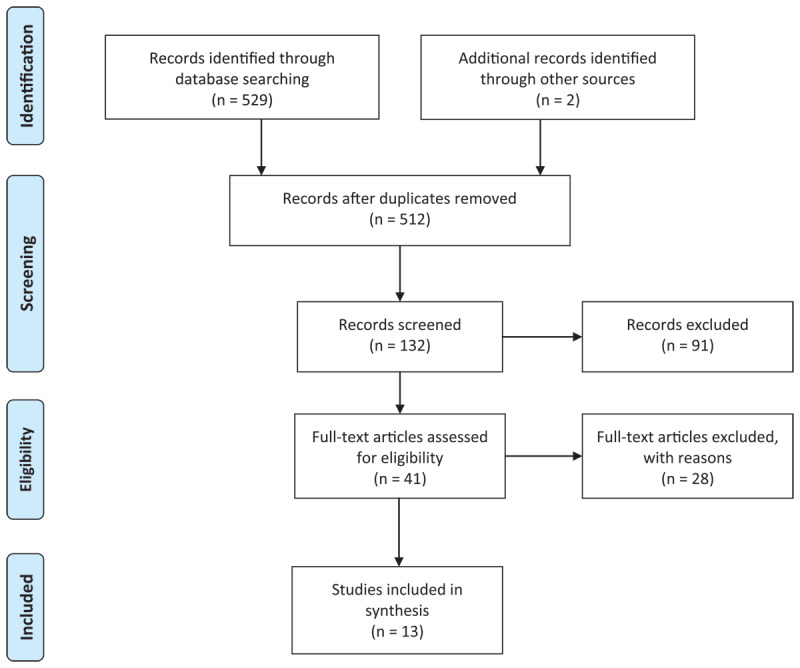
PRISMA flow diagram for selection of studies.
Study characteristics
The studies were conducted in various countries, including Tanzania [27], Ethiopia [32,33,34,35,36], Ghana [37], Sierra Leone [29], Cameroon [38], Eritrea [28], South Africa [26,39], and Kenya [40]. The various studies used diverse study designs. The characteristics of the studies used are shown in Table 1. The designs that were adopted in identifying the factors associated with home-based self-care management of hypertension in sub-Saharan Africa were cross-sectional [26,27,34,37,38], hospital-based cross-sectional [33,35,36], nationally representative cross-sectional data [39,40], retrospective cohort study [32], retrospective chart review [29], and qualitative study designs [28].
Table 1.
Distribution of study characteristics.
|
| |||||
|---|---|---|---|---|---|
| AUTHOR | MAIN GOAL | SETTING | DESIGN | SAMPLE | DATA ANALYSIS |
|
| |||||
| Maginga et al., 2015 | Determine factors associated with BP control among adults attending a hypertension clinic | Bugando Medical Centre, Tanzania | Cross-sectional study | 300 hypertension patients, selected consecutively | Fisher’s exact, Wilcoxon rank-sum test, univariable and multivariable logistic regression |
|
| |||||
| Berhe et al., 2017 | Examined determinants of achieving BP control and treatment intensification in patients with uncontrolled BP | Six public hospitals, Ethiopia | A retrospective cohort study | 897 adult ambulatory hypertension patients | Descriptive statistics and multivariable logistic regression |
|
| |||||
| Labata et al., 2019 | Assessed predictors of self-care practices among hypertensive patients | Jimma University Specialized Hospital, Ethiopia | Hospital-based cross-sectional study | 341 adult hypertensive patients | Descriptive statistics and multivariate logistics regression |
|
| |||||
| Niriayo et al., 2019 | Assessed the rate of adherence to self-care behaviors and associated factors among hypertensive patients | Ayder Comprehensive Specialized Hospital, Ethiopia | Cross-sectional study | 276 ambulatory hypertensive patients | Univariable and binary logistic regression |
|
| |||||
| Berhe et al., 2020 | Assessed the prevalence and factors associated with uncontrolled hypertension among adults | Mekelle public hospitals, Tigray, Ethiopia | Hospital-based cross-sectional study | 396 hypertensive patients, systematic random sampling | Bivariable and multivariable logistic regression |
|
| |||||
| Gebremichael et al., 2019 | Assessed self-care practices and associated factors among hypertensive patients | Ayder Comprehensive Specialized Hospital, Ethiopia | Hospital-based cross-sectional study | 320 hypertension patients, simple random sampling | Descriptive statistics, logistics, and multivariate regression |
|
| |||||
| Okai et al., 2020 | Assessed the patient-level factors that influence hypertension control | Two hospitals in Accra, Ghana | Cross-sectional study | 360 hypertensive patients | Chi-square tests and logistic regression |
|
| |||||
| Herskind et al., 2019 | Assessed an initiative conducted by two health clinics to begin treatment of hypertension among patients | Two clinics, Sierra Leone | Retrospective chart review and survey | 487 records of patients and 68 hypertension patients’ convenience sample | Descriptive statistics |
|
| |||||
| Adidja et al., 2018 | Determine the rate and factors associated with nonadherence to antihypertensive pharmacotherapy, the association between nonadherence and BP control | Buea Health District, Cameroon | Community-based cross-sectional study | 183 adults, stratified cluster sampling | Descriptive, chi-square, Fisher’s exact test, t-test, multivariable logistic regression |
|
| |||||
| Gebrezgi et al., 2017 | Identified barriers and facilitated hypertension management from the perspective of the patients | Asmara, Eritrea | Qualitative study | 48 individual in-depth interviews and 2 FGD | Thematic analysis |
|
| |||||
| Ware et al., 2019 | Investigated traditional risk factors alongside other health and sociodemographic indicators to determine predictors of hypertension prevalence and management | South Africa | Cross-sectional of a nationally representative cohort | WHO-SAGE South Africa Wave 1 recruited 4,223 respondents from selected probability sampled | Chi-square, Mann-Whitney U test, t-tests, logistic regression |
|
| |||||
| Mohamed et al., 2018 | Estimated the prevalence of hypertension, awareness, treatment, and control | Kenya | A national cross-sectional household survey study | 4,485 data from the 2015 Kenya STEPs survey, randomly selected | Descriptive statistics, multiple logistic regression, bivariate logistic regression |
|
| |||||
| Adeniyi et al., 2016 | Examined the sociodemographic and clinical determinants of uncontrolled hypertension among individuals living with T2DM in the rural communities | Mthatha, South Africa. | Cross-sectional study | 265 individuals living with T2DM and hypertension | Univariate and multivariate logistic regression |
|
| |||||
Legends: BP = blood pressure; FGD = focus group discussion; T2DM = type 2 diabetes mellitus.
Thematic Data Analysis
The synthesis showed that five key themes were associated with home-based self-care and BP control among patients. These key terms that emerged were (1) the prevalence of control of BP, (2) sociodemographic factors, (3) treatment-related factors, (4) knowledge of management, and (5) knowledge of prevention of risk factors of hypertension. The distribution of key findings is presented in Table 2.
Table 2.
Distribution of key findings.
|
| |||
|---|---|---|---|
| AUTHOR | OUTCOME AND MEASUREMENT | KEY DETERMINANTS OF HYPERTENSION CONTROL | KEY FINDINGS |
|
| |||
| Maginga et al., 2015 |
|
|
|
|
| |||
| Berhe et al., 2017 |
|
|
|
|
| |||
| Labata et al., 2019 |
|
|
|
|
| |||
| Niriayo et al., 2019 |
|
|
|
|
| |||
| Berhe et al., 2020 |
|
|
|
|
| |||
| Gebremichael et al., 2019 |
|
|
|
|
| |||
| Okai et al., 2020 |
|
|
|
|
| |||
| Herskind et al., 2019 |
|
|
|
|
| |||
| Adidja et al., 2018 |
|
|
|
|
| |||
| Gebrezgi et al., 2017 |
|
|
|
|
| |||
| Ware et al., 2019 |
|
|
|
|
| |||
| Mohamed et al., 2018 |
|
|
|
|
| |||
| Adeniyi et al., 2016 |
|
|
|
|
| |||
Legends: AOR = adjusted odds rations; BMI = body mass index; BMQ = belief about medicine questionnaire; CI = confidence interval; HELM = hypertension evaluation of lifestyle and management; MMAS = Morisky Medication Adherence Scale; WHS = World Health Survey.
Prevalence of control of BP
Two studies specifically assessed the prevalence of hypertension control during their respective studies. It was shown that hypertension control prevalence during the study periods was 47.7% [27] and 37.0% [32].
Sociodemographic factors associated with BP control
Several sociodemographic variables were assessed to determine the factors that influence hypertension control. The key subthemes assessed included gender (sex), age, and socioeconomic status.
Gender as a predictor of BP
The gender of hypertension patients was identified as an important factor associated with the ability to control BP [34,36]. Some of the studies showed that females (AOR = 2.25, 95% CI 1.09–4.65, p = 0.028) were found 2.25 times [36], 3.55 times (AOR = 3.55, 95% CI 1.72–7.22) more likely to have good self-care practice than males [37]. Also, men were identified to have reduced awareness of BP status [26,39,40]. Men had significantly reduced odds of being aware of their hypertensive status (AOR = 0.35, 95% CI 0.22–0.56) compared to women [40]. Another important predictor was that females had an increased tendency to be adherent to antihypertensive medication use [26,27,34,39]. Females had a higher tendency of BP control behavior, such as weight management (AOR = 0.46, 95% CI 0.23–0.92) and physical activity (AOR = 0.22, 95% CI 0.12–0.40) than males [34]. Females were also identified to have higher medication adherence and BP control [38]. However, some studies did not identify any significant difference in BP control across genders [26,27,33]. Control of BP was not significantly different between men and women [27]. Female respondents were less likely to adhere to physical activity (AOR = 0.51, 95% CI 0.30–0.88) and nonsmoking (AOR = 3.62, 95% CI 1.21–10.85) behavior [33].
Age as a predictor of BP control
The age of hypertension patients was identified as an important predictor of the ability to control BP [32,34,35,36,38,39]. Uncontrolled hypertension was 2.3 times (AOR = 0.19, 95% CI 0.06–0.61) higher among patients above 50 years compared to those above 60 [34]. Also, patients above 50 years were less adherent to weight management than younger individuals (18–35 years) [34]. Self-care practices of participants also improved with advancing age [36]. Patients under 65 years were 3.26 times (AOR = 3.26, 95% CI 1.03–10.35, p = 0.044) more likely to have good self-care practice than patients above 65 years [36]. Also, other studies showed that increasing age was associated with the tendency to be medication adherent and consequently maintain BP control [34,36].
The socioeconomic situation as a predictor of BP control
The socioeconomic status of hypertension patients was an important factor associated with BP control [27,34]. The major economic challenge associated with controlling BP was the medication cost and treatment [27]. The higher medication cost was associated with decreased odds of BP control at the study visit [27]. Odds of control (OR = 0.80, 95% CI 0.70–0.95, p = 0.010) decreased by 20% for every 10,000 Tanzanian shillings (TZS) spent on medication [27]. The place of residence influences the ability of respondents to adhere to medications [34]. Rural residents were less adherent to their medication (AOR = 0.45, 95% CI 0.21–0.97) than urban dwellers [34].
Other factors that predicted BP control and the self-care ability of respondents were the educational levels, as those who had at least a college level of education were found to be 4.205 times (AOR = 4.20, 95% CI 1.30–13.55, p = 0.016) more likely to have good self-care practice than those who were unable to read and write [36]. Participants with greater social support were 2.81 times (AOR = 2.81, 95% CI 1.20–6.53) more likely to adhere to a low-salt diet than their counterparts [33]. Other important socioeconomic factors that predicted control of hypertension were forgetfulness (AOR = 7.90, 95% CI 3.00–20.80, p < 0.001) and lack of finances (AOR = 2.80, 95% CI 1.10–6.90, p = 0.024) [34].
Treatment-related factors
The treatment-related factors associated with home-based and self-care management of hypertension had three themes: (1) duration of treatment of hypertension, (2) pill-related factors, and (3) medication adherence.
Duration of treatment
Several important key factors influence the ability to continue treatment and ensure BP control [32,36,37]. Some of these factors included the duration of disease and treatment, significantly influencing the ability to initiate and maintain self-care [36,38] and control BP [32,38]. Less than four years of disease duration was 3.12 times (AOR = 3.12, 95% CI 1.20–8.10, p = 0.019) more likely to practice good self-care than those with less than < 2 years of disease duration [36].
Medication-related factors
The number of medications the hypertension patient took also influenced their ability to control and maintain self-care [26,37]. When hypertension patients took three to four antihypertensive pills daily, the odds of having a controlled BP were reduced by 68.0% (AOR = 0.32, 95% CI 0.18–0.57) compared to those who took one to two pills [37]. When patients take multiple antihypertensive agents, it improves their tendency to have controlled BP [26]. Also, multiple daily doses (AOR = 2.50, 95% CI 1.20–5.60, p = 0.020) and drug side effects (AOR = 7.00, 95% CI 1.70–33.6, p = 0.007) were independent predictors of nonadherence after controlling for potential confounders in multivariate analysis [38]. Other pill-related factors that influence the control of BP were follow-up at general hospitals (OR = 1.89, 95% CI 1.26–2.83), inadequately controlled BP at prior visits (OR = 0.30, 95% CI 0.21–0.43), longer treatment duration per year (OR = 1.04, 95% CI 1.01–1.06), and prescribed diuretics (OR = 0.68, 95% CI 0.50–0.94) [32].
Medication adherence to BP control
The level of medication adherence was determined to be high [27,32,34] and was measured using the Morisky Medication Adherence Scale [MMAS] [27,32]. Most patients (56.0%) had high adherence to medication on the MMAS-4 [27]. The antihypertensive medication adherence rate (MMAS ≥ 7) was 40.0% and 57.0% for the lower cutoff (MMAS ≥ 6) [32]. Patients with high medication adherence to the MMAS-4 had increased odds (OR = 18.8, 95% CI 7.80–45.40, p < 0.001) of control relative to those with low adherence at the study visit [27]. Patients with a negative medication belief were less likely to adhere to their medication (AOR = 0.25, 95% CI 0.14–0.46) than those with a positive medication belief [34]. Adult participants were adherent to the prescribed antihypertensive medications (48.2%) and the recommended level of physical activity (44.9%) [34]. Patients who were nonadherent to prescribed antihypertensive drugs were two times (AOR = 1.82, 95% CI 1.08–3.04) more likely to have uncontrolled hypertension than those who were adherent [35]. Participants with poor self-efficacy (AOR = 0.40, 95% CI 0.22–0.73) were less likely to adhere to medication usage than participants with good self-efficacy [33]. Regarding specific practices, rarely or never taking medications as prescribed (OR = 0.10, 95% CI 0.50–0.20, p < 0.001) was associated with decreased hypertension [HTN] control [27].
Knowledge as a predictor of BP control
An important determinant of BP control was the level of knowledge of hypertension and control measures [27,34,36]. This was because moderate (OR = 1.80, 95% CI 1.01–3.20, p = 0.046) and good knowledge (OR = 2.10, 95% CI 1.00–4.50, p = 0.049) of HTN had increased odds of control [27]. Also, good knowledge was found 6.19 times (AOR = 6.19, 95% CI 2.90–13.21, p < 0.001) more positively associated with good self-care practice than poor knowledge [36]. Hypertension patients who knew the negative effects of salt (94.9%), alcohol (81.5%), and smoking (87.7%) and the positive effect of physical exercise (54.7%) had positive actions toward hypertension control [34]. Hypertension patients who were not knowledgeable about SCBs were less adherent to weight management (AOR = 0.13, 95% CI 0.03–0.57) and alcohol abstinence (AOR = 0.07, 95% CI 0.03–0.16) compared to those who were knowledgeable [34]. Overall, 82.2% of the participants were knowledgeable about the impact of the Self-care behavior [SCB] on hypertension control [34]. Those with moderate (OR = 2.80, 95% CI 1.20–6.40, p = 0.020) and good (OR = 3.00, 95% CI 1.30–7.00, p = 0.010) attitudes had increased odds of hypertension control [27]. Hypertension patients having adequate knowledge of hypertension were 2.58 times (AOR = 2.58, 95% CI 1.12–5.94) more likely to adhere to practicing physical activity [33].
Knowledge of prevention of risk factors of hypertension
Several risk factors of hypertension were identified to influence the tendency to have good BP control. Some of these key risk factors include salt intake, practices, weight control, avoiding smoking and alcohol, and the presence of other comorbidities.
The level of salt in the diet was associated with BP control
The level of salt intake was an important predictor of hypertension control among patients, as nonadherents to a low-salt diet were two times (AOR = 1.98, 95% CI 1.18–3.31) more likely to develop uncontrolled hypertension [35]. Also, when individuals’, especially women’s, knowledge of hypertension was identified to be low, their chances of having a high-salt diet increased [39]. Another important factor was adding salt to meals (OR = 0.40, 95% CI, 0.20–0.60, p = 0.001) as an important factor for BP control [27].
Behavioral measures as a predictor of BP control
The conscious behavioral measures instituted by individuals were an important predictor of BP control among hypertension patients [27,32,36]. Controlled BP was found 2.7 times (AOR = 2.72, 95% CI 1.25–5.92, p = 0.011) more associated with good self-care practice than uncontrolled BP [36]. Those who had moderate (OR = 4.80, 95% CI 2.40–9.40, p < 0.001) and good (OR = 11.00, 95% CI 5.00–24.20, p < 0.001) practices to prevent hypertension also had increased odds of controlled BP [27]. More severe hypertension stages, stage II hypertension (OR = 0.17, 95% CI 0.09–0.35) and stage I hypertension (OR = 0.34, 95% CI 0.17–0.67), were associated with more difficulty in achieving the target BP [32].
Weight as a predictor of BP control
Hypertension patients who were more conscious of controlling body weight had a higher chance of BP control [33,35]. The odds (AOR = 2.06, 95% CI 1.31–3.23) of uncontrolled hypertension were twice as high among those with nonadherent weight management [35]. Normal weight patients were 1.82 times (AOR = 1.82, 95% CI 1.07–3.09) more likely to adhere to medication usage practice than overweight respondents [33,35], while normal weight respondents were 2.22 times more likely (AOR = 2.21, 95% CI 1.21–4.04) to practice weight management [33]. Hypertension patients with good self-efficacy were 2.60 times more likely (AOR = 2.58, 95% CI 1.41–4.73) to maintain their weight than poor self-efficacy [33]. Also, rarely or never adhering to normal weight control advice (OR = 0.40, 95% CI 0.20–0.60, p < 0.001) was a predictor of poor hypertension control [27]. Patients who did not adhere to physical exercise were 1.8 times (AOR = 1.79, 95% CI 1.13–2.83) more likely to have uncontrolled hypertension compared to those who adhered to physical exercise [35].
Smoking and alcohol intake are predictors of high BP
Alcohol intake was identified as an important factor that influenced the likelihood of having hypertension control [27,33]. This was because drinking alcohol (OR = 0.30, 95% CI 0.10–0.70, p = 0.006) was a significant factor in BP control [27,33]. Females were more likely to adhere to alcohol abstinence (AOR = 1.97, 95% CI 1.03–3.75) and nonsmoking behavior (AOR = 6.33, 95% CI 1.80–22.31) than males [34].
Comorbidities as a predictor of BP control
The level and presence of comorbidities were identified to be associated with hypertension patients’ ability to have controlled BP [34,37,39]. Patients with comorbidities were also less adherent to their medication (AOR = 0.16, 95% CI 0.08–0.31) than those without comorbidities [34]. Also, a 69.0% (AOR = 0.31, 95% CI 0.11–0.89) reduction in the odds of having controlled hypertension was identified among patients who suffered from dyslipidemia as a comorbidity [37]. Elevated waist-to-height ratio and diabetes diagnosis were the most significant predictors of hypertension and being aware of hypertension status [39].
Discussion
This review identified and integrated the factors associated with home-based self-care management of hypertension. In chronic diseases like hypertension, home-based management is cardinal in improving a patient’s outcome and the ability to avoid complications and limit the progress of the disease [41,42,43]. Hypertension patients must identify and institute home measures that help them improve their BP levels and avoid related complications. The studies on hypertension home-based management are largely cross-sectional and limited to a specific culture or geographical location. Therefore, we were motivated to identify the factors associated with home-based management of hypertension to identify and integrate measures to improve client outcomes. We identified the prevalence of BP control to range from 21.3% [38] to 47.7% [27] among hypertension patients.
This study highlighted the diverse components that must be considered when interventions are implemented for home-based self-care management of hypertension. Hypertension control through self-care at home was reported in similar systematic reviews to be influenced by diverse factors [41]. An important point of this home management involves measuring BP [42,43]. Self-care management of hypertension was instrumental when it was noted that intervention efficacy is most felt when the patient is used as the change agent [44]. Poor self-management and medication adherence were identified to negatively influence hypertension control among patients [9].
In this study, we identified multiple interactive factors that influence home-based self-care and management of BP. These factors include sociodemographic, treatment-related, and knowledge of hypertension management and risk factors. Divergent and multiple nature of the factors that are identified to influence hypertension control in Africa warrants commensurate measures to eliminate the associated repercussions of the disease. The culmination of these interventions must focus on reducing hypertension risk, ensuring medication adherence, and promoting appropriate lifestyle modifications.
The divergent factors of multilevel, multicomponent interventions will ensure and promote comprehensive solutions (Mills et al., 2018), especially in lower- and middle-income countries like those in sub-Saharan Africa. This strategy is imperative to limit the challenges imposed by high BP. The sociodemographic factors that influence hypertension control through the home-based self-care ability of patients were gender (female), age (older), place of residence (urban), educational level (educated), and socioeconomic status (high). These sociodemographic characteristics are predictive of hypertension as explanatory variables [16,17,40,45,46,47,48], yet they were identified to influence the ability of patients to control hypertension. While little can be done about sociodemographic factors as a risk to hypertension (nonmodifiable risk), identifying these factors gives a category of where the emphasis should be placed on preventing and controlling hypertension. Home management education must prioritize categories that have inadequate skills in home management. To promote home-based self-care management of hypertension in lower- and middle-income countries, intervention studies must focus on identifying the influence of each factor on the care of the patient and their ability to institute home-based management of hypertension.
Increasing knowledge on control measures, including limiting risk factors, and improving medication adherence through health education will be central in assisting patients in improving home-based care. In a related systematic review and meta-analysis, this study demonstrated that the number of pills and intake duration strongly influence adherence to medication at home, especially among patients with hypertension [49]. Patients who were noted to take antihypertensive medications over a long period with few medications were said to have higher adherence levels. These factors were important in other systematic reviews [49,50,51]. It is important that when patients are discharged from the hospital to home for self-care management, only relevant (few) medications with limited pill dosage requirements will promote a positive attitude toward care and ensure hypertension control. It was noted that coordinated interventions used in managing hypertension that limit pill number and frequency among patients and increase knowledge and lifestyle changes are useful [52,53].
Other important themes that emerged were the level of knowledge on hypertension and the presence of risk factors (modifiable risk factors) of hypertension. These modifiable risk factors are mainly centered on knowledge levels, smoking, alcohol, BMI, level of salt intake, and the presence of comorbidities. It was shown that even though this factor predicts the presence of hypertension, it also influences the level of treatment patients adopt during home management. The impact of these modifiable risk factors on the ability to control hypertension, especially in lower- and middle-income countries, was also documented in a previous study [54,55,56]. To improve knowledge and, at the same time, eliminate the risk associated with hypertension, interactive technological methods will increase the likelihood of behavior change, which is implicated in the inability to achieve successful home-based self-care management [12,52].
Research and policy making should streamline intervention studies that will improve home-based and self-care management of hypertension, especially in low-resource settings. In this review, we identified that important interventions that will improve self-care and home management of hypertension should focus on improving self-efficacy, increasing knowledge, and targeting specific attitudes of patients to improve adherence. Also, intervention research methods must focus on eliminating the risk factors of hypertension and segregating patients based on demographic categorization (like age, gender, socioeconomic status, and level of education) for implementation.
Conclusion
This systematic review identified and synthesized the factors associated with home-based and self-care management of hypertension. These factors are complex and multi-sectoral to improve the lives of people with hypertension; multi-sectoral approaches are their force required. Hypertension self-care interventions in lower resource settings must incorporate individual, societal, and cultural perspectives in increasing knowledge and improving home-based hypertension management. In this review, it could be seen that the use of technology-based interventions for improving home-based self-care management of hypertension is limited. This warrants the use of technology-based intervention (including social media networks and phone-based text messaging) that could improve teaching, coaching, and monitoring and give feedback to patients, especially when they engage in home-based self-care management of hypertension. Also, well-designed clinical experimental studies use complex interventions to increase knowledge and self-efficacy and improve behaviors toward home management of hypertension.
Data Accessibility Statement
All data from which the conclusions of this study were made are included in this manuscript, and no data is deposited in any public database.
Additional File
The additional file for this article can be found as follows:
Results of quality appraisal using the mixed methods appraisal tool.
Competing Interests
The author has no competing interests to declare.
Author Contributions
All the authors contributed substantially to the conception, design, search, and acquisition of data, extraction, and synthesis. All the researchers also contributed significantly to drafting and revising the manuscript for critically important intellectual content and gave final approval for publication of this manuscript in your esteemed journal.
References
- 1.Salim H, Lee PY, Sazlina SG, Ching SM, Mawardi M, Shamsuddin NH, et al. The self-care profiles and its determinants among adults with hypertension in primary health care clinics in Selangor, Malaysia. PLOS One. 2019; 14(11): e0224649. DOI: 10.1371/journal.pone.0224649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin P-H, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, et al. The PREMIER intervention helps participants follow the Dietary Approaches to Stop Hypertension dietary pattern and the current Dietary Reference Intakes recommendations. Journal of the American Dietetic Association. 2007; 107(9): 1541–1551. DOI: 10.1016/j.jada.2007.06.019 [DOI] [PubMed] [Google Scholar]
- 3.Bayliss EA, Steiner JF, Fernald DH, Crane LA, Main DS. Descriptions of barriers to self-care by persons with comorbid chronic diseases. Annals of Family Medicine. 2003; 1(1): 15–21. DOI: 10.1370/afm.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han H-R, Lee H, Commodore-Mensah Y, Kim M. Development and validation of the hypertension self-care profile: A practical tool to measure hypertension self-care. Journal of Cardiovascular Nursing. 2014; 29(3): E11. DOI: 10.1097/JCN.0b013e3182a3fd46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure–lowering medication in ambulatory care? Systematic review of randomized controlled trials. Archives of Internal Medicine. 2004; 164(7): 722–732. DOI: 10.1001/archinte.164.7.722 [DOI] [PubMed] [Google Scholar]
- 6.Tan FCJH, Oka P, Dambha-Miller H, Tan NC. The association between self-efficacy and self-care in essential hypertension: A systematic review. BMC Family Practice. 2021; 22(1): 1–12. DOI: 10.1186/s12875-021-01391-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zare S, Rezaee R, Aslani A, Shirdeli M, Kojuri J. Moving toward community based telehealth services using mhealth for hypertensive patients. International Journal of Technology Assessment in Health Care. 2019; 35(5): 379–383. DOI: 10.1017/S0266462319000655 [DOI] [PubMed] [Google Scholar]
- 8.Motlagh SFZ, Chaman R, Sadeghi E, Eslami AA. Self-care behaviors and related factors in hypertensive patients. Iranian Red Crescent Medical Journal. 2016; 18(6). DOI: 10.5812/ircmj.35805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu X, Yang H, Xia X, Lu X, Lin J, Liu F, et al. Interactive mobile health intervention and blood pressure management in adults: A meta-analysis of randomized controlled trials. Hypertension. 2019; 74(3): 697–704. DOI: 10.1161/HYPERTENSIONAHA.119.13273 [DOI] [PubMed] [Google Scholar]
- 10.Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 191 million participants. Lancet. 2017; 389(10064): 37–55. DOI: 10.1016/S0140-6736(16)31919-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mallat SG, Samra SA, Younes F, Sawaya M-T. Identifying predictors of blood pressure control in the Lebanese population—A national, multicentric survey—I-PREDICT. BMC Public Health. 2014; 14(1): 1–9. DOI: 10.1186/1471-2458-14-1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van de Vijver S, Akinyi H, Oti S, Olajide A, Agyemang C, Aboderin I, et al. Status report on hypertension in Africa—Consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan African Medical Journal. 2014; 16(1). DOI: 10.11604/pamj.2013.16.38.3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agyemang C, Bruijnzeels MA, Owusu-Dabo E. Factors associated with hypertension awareness, treatment, and control in Ghana, West Africa. Journal of Human Hypertension. 2006; 20(1): 67–71. DOI: 10.1038/sj.jhh.1001923 [DOI] [PubMed] [Google Scholar]
- 14.Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: A systematic review. BMC Cardiovascular Disorders. 2013; 13(1): 1–11. DOI: 10.1186/1471-2261-13-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clinical Hypertension. 2017; 23(1): 1–9. DOI: 10.1186/s40885-017-0081-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konlan KD, Afam-Adjei CJ, Afam-Adjei C, Oware J, Appiah TA, Konlan KD, et al. Practice and sociodemographic factors influencing self-monitoring of blood pressure in Ghanaians with hypertension. International Journal of Chronic Diseases. 2020; 2020: 6016581. DOI: 10.1155/2020/6016581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konlan KD, Lee H, Lee M, Kim Y, Lee H, Abdulai JA. Risk factors associated with the incidence and prevalence of hypertension in Ghana: An integrated review (2016–2021). International Journal of Environmental Health Research. 2022; 1–16. DOI: 10.1080/09603123.2022.2076814 [DOI] [PubMed] [Google Scholar]
- 18.Jamshidnezhad A, Kabootarizadeh L, Hoseini SM. The effects of smartphone applications on patients self-care with hypertension: A systematic review study. Acta Informatica Medica. 2019; 27(4): 263. DOI: 10.5455/aim.2019.27.263-267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma Y, Cheng HY, Cheng L, Sit JW. The effectiveness of electronic health interventions on blood pressure control, self-care behavioural outcomes and psychosocial well-being in patients with hypertension: A systematic review and meta-analysis. International Journal of Nursing Studies. 2019; 92: 27–46. DOI: 10.1016/j.ijnurstu.2018.11.007 [DOI] [PubMed] [Google Scholar]
- 20.Yue N, Claes S. Wearable sensors for smart abnormal heart rate detection during skiing. Internet Technology Letters. 2021; 4(3): e230. DOI: 10.1002/itl2.230 [DOI] [Google Scholar]
- 21.Shin J, Konlan KD, Mensah E. Health promotion interventions for the control of hypertension in Africa, a systematic scoping review from 2011 to 2021. PLOS One. 2021; 16(11): e0260411. DOI: 10.1371/journal.pone.0260411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panic N, Leoncini E, De Belvis G, Ricciardi W, Boccia S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLOS One. 2013; 8(12): e83138. DOI: 10.1371/journal.pone.0083138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition). Journal of Chinese Integrative Medicine. 2009; 7(9): 889–896. DOI: 10.3736/jcim20090918 [DOI] [Google Scholar]
- 24.Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). Journal of Evaluation in Clinical Practice. 2018; 24(3): 459–467. DOI: 10.1111/jep.12884 [DOI] [PubMed] [Google Scholar]
- 25.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018; 34(4): 285–291. DOI: 10.3233/EFI-180221 [DOI] [Google Scholar]
- 26.Adeniyi OV, Yogeswaran P, Longo-Mbenza B, Goon DT. Uncontrolled hypertension and its determinants in patients with concomitant type 2 diabetes mellitus (T2DM) in rural South Africa. PLOS One. 2016; 11(3): e0150033. DOI: 10.1371/journal.pone.0150033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maginga J, Guerrero M, Koh E, Holm Hansen C, Shedafa R, Kalokola F, et al. Hypertension control and its correlates among adults attending a hypertension clinic in Tanzania. Journal of Clinical Hypertension. 2016; 18(3): 207–216. DOI: 10.1111/jch.12646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebrezgi MT, Trepka MJ, Kidane EA. Barriers to and facilitators of hypertension management in Asmara, Eritrea: Patients’ perspectives. Journal of Health, Population and Nutrition. 2017; 36(1): 1–7. DOI: 10.1186/s41043-017-0090-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herskind J, Holmes D, Bacher K, Zelasko J. The outpatient management of hypertension at two Sierra Leonean health centres: A mixed-method investigation of follow-up compliance and patient-reported barriers to care. African Journal of Primary Health Care and Family Medicine. 2020; 12(1): 1–7. DOI: 10.4102/phcfm.v12i1.2222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pluye P, Hong QN. Combining the power of stories and the power of numbers: Mixed methods research and mixed studies reviews. Annual Review of Public Health. 2014; 35: 29–45. DOI: 10.1146/annurev-publhealth-032013-182440 [DOI] [PubMed] [Google Scholar]
- 31.Clarke V, Braun V, Hayfield N. Thematic analysis. In: Smith JA (Ed.) Qualitative psychology: A practical guide to research methods. London: SAGE Publications. 2015; 222–248. [Google Scholar]
- 32.Berhe DF, Taxis K, Haaijer-Ruskamp FM, Mulugeta A, Mengistu YT, Mol PG. Hypertension treatment practices and its determinants among ambulatory patients: Retrospective cohort study in Ethiopia. BMJ Open. 2017; 7(8): e015743. DOI: 10.1136/bmjopen-2016-015743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Labata BG, Ahmed MB, Mekonen GF, Daba FB. Prevalence and predictors of self care practices among hypertensive patients at Jimma University Specialized Hospital, Southwest Ethiopia: Cross-sectional study. BMC Research Notes. 2019; 12(1): 1–8. DOI: 10.1186/s13104-019-4125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niriayo YL, Ibrahim S, Kassa TD, Asgedom SW, Atey TM, Gidey K, et al. Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLOS One. 2019; 14(6): e0218947. DOI: 10.1371/journal.pone.0218947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aberhe W, Mariye T, Bahrey D, Zereabruk K, Hailay A, Mebrahtom G, et al. Prevalence and factors associated with uncontrolled hypertension among adult hypertensive patients on follow-up at Northern Ethiopia, 2019: Cross-sectional study. Pan African Medical Journal. 2020; 36(1). DOI: 10.1155/2020/8896990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gebremichael GB, Berhe KK, Beyene BG, Gebrekidan KB. Self-care practices and associated factors among adult hypertensive patients in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia, 2018. BMC Research Notes. 2019; 12(1): 1–6. DOI: 10.1186/s13104-019-4502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okai DE, Manu A, Amoah EM, Laar A, Akamah J, Torpey K. Patient-level factors influencing hypertension control in adults in Accra, Ghana. BMC Cardiovascular Disorders. 2020; 20(1): 1–7. DOI: 10.1186/s12872-020-01370-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adidja NM, Agbor VN, Aminde JA, Ngwasiri CA, Ngu KB, Aminde LN. Non-adherence to antihypertensive pharmacotherapy in Buea, Cameroon: A cross-sectional community-based study. BMC Cardiovascular Disorders. 2018; 18(1): 1–9. DOI: 10.1186/s12872-018-0888-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ware LJ, Chidumwa G, Charlton K, Schutte AE, Kowal P. Predictors of hypertension awareness, treatment and control in South Africa: Results from the WHO-SAGE population survey (Wave 2). Journal of Human Hypertension. 2019; 33(2): 157–166. DOI: 10.1038/s41371-018-0125-3 [DOI] [PubMed] [Google Scholar]
- 40.Mohamed SF, Mutua MK, Wamai R, Wekesah F, Haregu T, Juma P, et al. Prevalence, awareness, treatment and control of hypertension and their determinants: results from a national survey in Kenya. BMC Public Health. 2018; 18(3): 1–10. DOI: 10.1186/s12889-018-6052-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation. 2016; 134(6): 441–450. DOI: 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OS, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: A systematic review and meta-analysis. Lancet Public Health. 2017; 2(2): e108–e20. DOI: 10.1016/S2468-2667(17)30003-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Türker F, Sahın T, Oral A, Koçak E, Türker BÇ, Niğdelioğlu A, et al. Evaluation of predisposing metabolic risk factors for portopulmonary hypertension in patients with NASH cirrhosis. International Journal of General Medicine. 2022; 15: 859–865. DOI: 10.2147/IJGM.S339474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaboli PJ, Howren MB, Ishani A, Carter B, Christensen AJ, Vander Weg MW. Efficacy of patient activation interventions with or without financial incentives to promote prescribing of thiazides and hypertension control: A randomized clinical trial. JAMA Network Open. 2018; 1(8): e185017. DOI: 10.1001/jamanetworkopen.2018.5017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Craig LS, Gage AJ, Thomas AM. Prevalence and predictors of hypertension in Namibia: A national-level cross-sectional study. PLOS One. 2018; 13(9): e0204344. DOI: 10.1371/journal.pone.0204344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mamdouh H, Alnakhi WK, Hussain HY, Ibrahim GM, Hussein A, Mahmoud I, et al. Prevalence and associated risk factors of hypertension and pre-hypertension among the adult population: Findings from the Dubai Household Survey, 2019. BMC Cardiovascular Disorders. 2022; 22(1): 1–9. DOI: 10.1186/s12872-022-02457-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Okello S, Muhihi A, Mohamed SF, Ameh S, Ochimana C, Oluwasanu AO, et al. Hypertension prevalence, awareness, treatment, and control and predicted 10-year CVD risk: A cross-sectional study of seven communities in East and West Africa (SevenCEWA). BMC Public Health. 2020; 20(1): 1–13. DOI: 10.1186/s12889-020-09829-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manios Y, Karatzi K, Moschonis G, Ioannou G, Androutsos O, Lionis C, et al. Lifestyle, anthropometric, sociodemographic and perinatal correlates of early adolescence hypertension: The Healthy Growth Study. Nutrition, Metabolism and Cardiovascular Diseases. 2019; 29(2): 159–169. DOI: 10.1016/j.numecd.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 49.Parati G, Kjeldsen S, Coca A, Cushman WC, Wang J. Adherence to single-pill versus free-equivalent combination therapy in hypertension: A systematic review and meta-analysis. Hypertension. 2021; 77(2): 692–705. DOI: 10.1161/HYPERTENSIONAHA.120.15781 [DOI] [PubMed] [Google Scholar]
- 50.Reeves L, Robinson K, McClelland T, Adedoyin CA, Broeseker A, Adunlin G. Pharmacist interventions in the management of blood pressure control and adherence to antihypertensive medications: A systematic review of randomized controlled trials. Journal of Pharmacy Practice. 2021; 34(3): 480–492. DOI: 10.1177/0897190020903573 [DOI] [PubMed] [Google Scholar]
- 51.Hermida RC, Mojón A, Hermida-Ayala RG, Smolensky MH, Fernández JR. Extent of asleep blood pressure reduction by hypertension medications is ingestion-time dependent: Systematic review and meta-analysis of published human trials. Sleep Medicine Reviews. 2021; 59: 101454. DOI: 10.1016/j.smrv.2021.101454 [DOI] [PubMed] [Google Scholar]
- 52.Abel WM, Spikes T, Greer DB. A qualitative study: Hypertension stigma among black women. Journal of Cardiovascular Nursing. 2021; 36(2): 96–103. DOI: 10.1097/JCN.0000000000000759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salam A, Atkins ER, Hsu B, Webster R, Patel A, Rodgers A. Efficacy and safety of triple versus dual combination blood pressure-lowering drug therapy: A systematic review and meta-analysis of randomized controlled trials. Journal of Hypertension. 2019; 37(8): 1567–1573. DOI: 10.1097/HJH.0000000000002089 [DOI] [PubMed] [Google Scholar]
- 54.Debon R, Coleone JD, Bellei EA, De Marchi ACB. Mobile health applications for chronic diseases: A systematic review of features for lifestyle improvement. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2019; 13(4): 2507–2512. DOI: 10.1016/j.dsx.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 55.Debon R, Bellei EA, Biduski D, Volpi SS, Alves ALSA, Portella MR, et al. Effects of using a mobile health application on the health conditions of patients with arterial hypertension: A pilot trial in the context of Brazil’s family health strategy. Scientific Reports. 2020; 10(1): 1–10. DOI: 10.1038/s41598-020-63057-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet. 2020; 395(10226): 795–808. DOI: 10.1016/S0140-6736(19)32008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results of quality appraisal using the mixed methods appraisal tool.
Data Availability Statement
All data from which the conclusions of this study were made are included in this manuscript, and no data is deposited in any public database.


