Abstract
For older adults, acute hospitalization is a high-risk event with poor health outcomes, including functional decline. In absence of practical guidelines and high quality randomized controlled trials, this Delphi study was conducted. The aim of this study was to obtain consensus on an exercise intervention program, a core outcome set (COS) and handover information to prevent functional decline or restore physical function in acutely hospitalized older patients transitioning from hospital to home. An internal panel of experts in the field of exercise interventions for acutely hospitalized older adults were invited to join the study. In the Delphi study, relevant topics were recognized, statements were formulated and ranked on a 9-point Likert scale in two additional rounds. To reaching consensus, a score of 7–9 was classified as essential. Results were expressed as median and semi-interquartile range (SIQR), and consensus threshold was set at SIQR≤0.5. Fifteen international experts from eight countries participated in the panel. The response rate was 93%, 93% and 80% for the three rounds respectively. After three rounds, consensus was reached on 167 of the 185 (90.3%) statements, of which ninety-five (51.4%) were ranked as essential (median Likert-score ≥7.0, SIQR ≤0.5). This Delphi study provides starting points for developing an exercise intervention, a COS and handover information. The results of this Delphi study can assist physical therapists to provide a tailored exercise intervention for older patients with complex care needs after hospital discharge, to prevent functional decline and/or restore physical function.
Introduction
For older adults, an acute hospitalization for multiple days due to an acute illness is a high-risk event with poor health outcomes, including functional decline, readmission, and mortality [1]. More than 30% of older adults experience physical deconditioning and functional decline after acute hospitalization [2, 3]. Several factors are associated with functional decline, including severity of the acute disease, immobility [4, 5], reduced physical activity [6, 7], low muscle mass/strength [8, 9], nutritional deficiency [10] and geriatric syndromes [11, 12]. These factors are highly prevalent in older patients after acute hospitalization and might hinder recovery, reduce physical functioning and promote functional decline [3, 11].
Functional decline is the loss of activities of daily living with worsening self-care skills [13] and can be reduced during hospitalization with an exercise program [14]. In this study [14], in-hospital exercise programmes to prevent functional decline were performed twice per day. These programmes included multiple components that focused on the patients’ individual needs [14]. Providing older patients with an exercise programme when they transition from the hospital to home has been associated with better recovery and less functional decline. However, this association has not been confirmed [15–17]. Exercise interventions started in the hospital are often not continued at home, despite the importance of these interventions to the patients [2].
A seamless transition of exercise interventions from the hospital to home might stimulate recovery and prevent functional decline [1, 11, 13]. International exercise recommendations in older adults are reported [18, 19], These recommendations indicate that exercise improve physical function and quality of life and exercise is essential to older adults. However, practical guidelines on the frequency, intensity, time, and type (FITT) of home-based exercise interventions specifically for older patients after hospitalization are lacking. Also important to a seamless transition in rehabilitation care from hospital to home are recommendations for handover information and measurement tools as part of a core outcome set (COS) for clinical practice. It has been suggested that a COS would increase uniformity [19–22] in research and clinical practice and might help create exercise intervention programmes that are tailored to the individual needs and goals of the patient.
In the absence of practical guidelines and high-quality randomized controlled trials focusing on acute hospitalized older adults, the Delphi methodology is often applied to obtain expert consensus on interventions for different populations [23, 24]. If experts could agree on practical guidelines for an exercise intervention, a COS and handover information for older patients after acute hospitalization in the home situation, this would guide physical therapists in their clinical decision-making. The aim of this Delphi study was to develop a consensus statement on 1) the characteristics of a home-based exercise intervention, 2) a COS of measurements on daily functioning and 3) handover information for older, acutely hospitalized patients transitioning from hospital to home that can prevent functional decline or restore physical function.
Methods
To determine topics relevant to the objective of this Delphi study, a scoping literature review was conducted on measurement tools and exercise interventions for older adults. After this, a three round Delphi method was applied. A steering committee consisting of experts in complex care and rehabilitation after acute hospitalization from the Amsterdam University Medical Centers (Amsterdam UMC) supervised the Delphi project. The project was registered with the Core Outcome Measures in Effectiveness Trials (COMET) initiative (study reference: http://www.comet-initiative.org/Studies/Details/1294).
We conducted a scoping literature review searching PubMed, Medline, PEDro, CINAHL, Science Direct and ProQuest Social Sciences to summarize the current state of the art [24, 25]. This scoping review included studies on characteristics of exercise interventions and measurement tools within the domains of the International Classification of Functioning (ICF) [26] for older patients after acute hospitalization. Articles were considered for review if they were systematic reviews or clinical trials and published in the last 10 years and if exercise for older adults was the studied intervention. Based on the scoping review, the following three topics were recognized: 1) characteristics of the exercise intervention, 2) COS of measurement tools and 3) handover information from hospital on to healthcare professionals in primary care. Statements on the three topics were formulated and then discussed by the panel.
Expert panel
Delphi panel members were recruited based on their clinical and scientific expertise in exercise interventions, their professional background, their research output, and their geographical location. Eligible panellists were invited to participate via email, and informed consent for publication of the results was obtained when they agreed to participate.
Delphi rounds
The Delphi rounds were conducted between January and April 2019. It was decided, a priori, to conduct a minimum of three rounds because this is considered appropriate when limited scientific evidence is available [24]. A digital survey was sent to generate ideas and to rank statements on a 9-point Likert scale, as per Delphi methodology recommendations [20]. A score of 1–3 was given to items of limited importance; a score of 4–6 to items ranked as important but not essential; and a score of 7–9 to items deemed essential (Fig 1). Panellists could also give a score of 0 (unable to score) if they felt a topic or statement fell outside of their scope of expertise. For each statement scored in the second and third Delphi rounds, a median Likert-score and semi-interquartile range (SIQR) were computed based on the first and third quarters of the SIQR. Results from the second Delphi round were imputed into the final round results if no third-round score was given. Consensus was defined a priori as an SIQR ≤0.5. Statements with consensus and a median Likert score ≥7.0 were used for further analysis. Consensus was reached on ≥80% of the statements after round three, so no extra Delphi round was deemed necessary [23–25].
Fig 1. 9-point Likert scale used in the Delphi rounds.
Delphi round 1: Collecting expert opinions
The aim of the first round was to collect expert opinions on the three topics identified in the scoping review (exercise intervention, COS, and handover information). A case description of an acutely hospitalized older adult transitioning home from hospital provided the context and was the starting point for each panel member (supplementary material). The questions were related to the different aspects of the ICF and used a standard description of health and health-related status [26]. In this first round, 22 closed questions on the three topics were asked with multiple possible answers. Additional information was also collected from 17 open questions on topics such as the intensity of training or involvement of other healthcare professionals (supplementary material). All items checked as relevant by the panel members were included in the following rounds. Answers to the open questions were examined to check whether they raised new questions or identified different topics. All input was categorized, and statements were drafted for each of the topics and approved by the steering committee.
Delphi round 2: Ranking statements
After the first Delphi round, 185 statements were formulated: 74 on exercise interventions, 86 on measurement tools and COS, and 25 on handover information.
Delphi round 3: Consensus round
In the third Delphi round, each panellist received their results from the second Delphi round together with the panel’s median Likert scores and SIQR for each of the statements. If an individual panel member’s scores differed from the panel’s median scores, they were asked to consider re-ranking the statement towards the median to reach consensus. Participants were motivated further if they chose not to re-rank their statements.
Results
All invited experts agreed to participate in the Delphi panel (n = 16). One panellist did not respond within the allocated time for the first Delphi round so 15 panellists were included in the analysis. The response rates were 93% for round one, 93% for round two and 80% for round three. Table 1 presents the panellists’ nationalities, profession, field of expertise, years of clinical experience and response. The panel consisted of nine physical therapists, two exercise physiologists, two sports scientists, one physician and one occupational therapist. After round three, consensus was reached on 185 statements, warranting the end of the Delphi consensus process. Ninety-five of the 185 statements (51.4%) were consensually ranked between 7 and 9 on the Likert scale and therefore considered essential for implication in clinical practice by the Delphi panel.
Table 1. International Delphi panel characteristics.
| Country | Gender | Title | Field of Expertise | Years of Clinical experience | Number of Publications in PubMed | Round 1 | Round 2 | Round 3 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Australia | Male | Professor | Exercise physiologist | >20 | >100 | ✓ | ✓ | ✓ |
| 2 | Belgium | Male | MSc | Physical therapist | >20 | >5 | ✓ | ✓ | ✓ |
| 3 | Belgium | Male | Professor | Exercise Physiologist | 10–15 | >100 | ✓ | ✓ | ✓ |
| 4 | Canada | Female | PhD | Physical therapist | 5–10 | >50 | ✓ | ✓ | ✓ |
| 5 | Denmark | Female | PhD | Physical therapist | 15–20 | 10 | ✓ | – | – |
| 6 | Netherlands | Female | MSc | Physical therapist | 15–20 | 0 | ✓ | ✓ | ✓ |
| 7 | Netherlands | Female | MSc | Physical therapist | 15–20 | 0 | ✓ | ✓ | ✓ |
| 8 | Netherlands | Female | PhD | Physical therapist | 10–15 | >50 | ✓ | ✓ | ✓ |
| 9 | Netherlands | Male | PhD | Exercise physiologist | 10–15 | >50 | ✓ | ✓ | ✓ |
| 10 | Netherlands | Female | MSc | Physical therapist | >20 | 0 | ✓ | ✓ | ✓ |
| 11 | Spain | Female | Associate professor | Physical therapist Sport scientist | 10–15 | >50 | ✓ | ✓ | ✓ |
| 12 | Spain | Male | Professor | Sport scientist | 15–20 | >100 | ✓ | ✓ | – |
| 13 | Spain | Male | Associate professor | Medical doctor | >20 | >100 | ✓ | ✓ | – |
| 14 | USA | Female | Associate professor | Occupational therapist | 10–15 | >20 | ✓ | ✓ | ✓ |
| 15 | USA | Male | Associate professor | Physical therapist | 5–10 | >10 | – | ✓ | ✓ |
– = no response; ✓ = response obtained
Theme 1: Exercise intervention
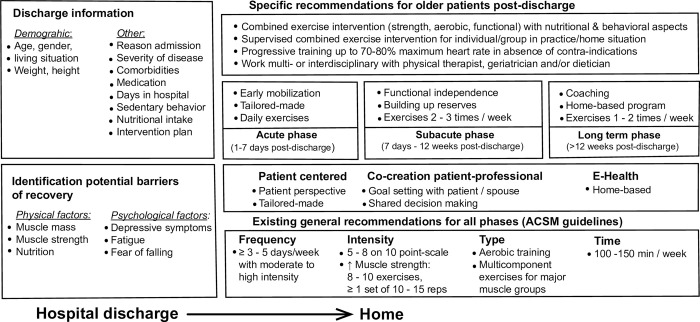
Seventy-four of the 185 (40.0%) statements were about exercise interventions to prevent functional decline after hospital discharge. Of these, 55 statements (74.3%) were consensually ranked as essential (supplementary material). Statements covered topics such as FITT of training, the need for supervised exercise programmes, importance of exercise programmes, and whether exercise interventions should be combined with nutritional and behavioural interventions. Regarding training frequency, daily exercise interventions in the acute phase (up to 7 days post-discharge), 2–3 times weekly interventions in the sub-acute phase (up to 12 weeks post-discharge) and 1–12 times weekly in the long-term phase (>12 weeks post-discharge) were consensually ranked as essential for preventing functional decline. The panel agreed that exercise intensity levels up to 70–80% of the maximum heart rate are essential for preventing functional decline and that contra-indications should be absent. With regards to the type of training in the acute phase, the panel ranked early mobilization, supervised tailor-made exercise interventions adjusted to the specific needs and goals of the patient, and combined exercise interventions (including strength, aerobic and functional training, either individual or in a group) as essential. Furthermore, co-creation of a training program by the patient and healthcare professional, functional training, building up physiological reserves, coaching, and reassessment and treatment by a geriatrician post-discharge were all ranked as essential during the recovery phases. Fig 2 summarizes these exercise intervention characteristics and existing recommendations.
Fig 2. Recommended exercise intervention characteristics and handover information derived from this Delphi consensus process in addition to general recommendations for older patients after discharge from hospital.
Theme 2: Core outcome set
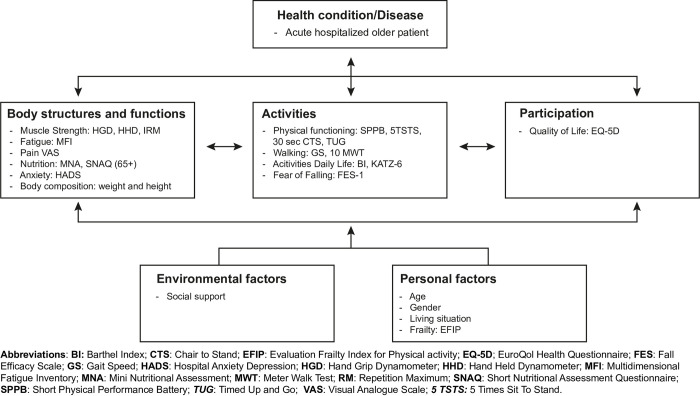
Eighty-six of the 185 (46.5%) statements were related to measurement tools for the COS. Of these statements, 25.6% (22 statements) were consensually ranked as essential. For activities of daily living, functional exercise capacity, performance, and muscle strength, more than one measurement outcome was ranked as essential. Fig 3 presents an overview of the measurement tools across all ICF domains. A COS of measurement tools was consensually ranked as essential for identifying risk factors of functional decline.
Fig 3. Core outcome set (COS) of measurement tools per ICF domain post-discharge.
Theme 3: Handover information
Of the 185 statements, 25 (13.5%) were related to the handover information provided when the patient is discharged from hospital. The panel consensually ranked five demographic aspects as essential for inclusion in handover information: age, gender, weight, height and living situation. Panellists also ranked the following 13 items as essential for inclusion in the handover information: hospital length of stay, number of days of bedrest and sedentary behaviour, comorbidities, reason for hospital admission and/or severity of illness, medication usage, physical therapy interventions, level of (physical) functioning at hospital discharge, premorbid level of functioning, nutritional intake, and treatment goals. Detailed ranking results including median Likert scores and SIQRs can be found in the supplementary material.
Discussion
This Delphi study provides practice guidelines for an exercise intervention, a COS and handover information to facilitate the seamless transition of exercise interventions when older patients are discharged from hospital. Experts agreed that supervised intensive exercise programmes should continue after hospital discharge and that these interventions should be tailored to the specific needs of the patient. COS measurement tools in all domains of the ICF and handover information from the hospital can help to tailor the exercise intervention to promote recovery, prevent functional decline, and restore physical function.
After discharge from hospital, exercises and physical activity are often not continued because stimulus by staff or community [22] and/or self-discipline [17] are lacking. The expert panel agreed that an exercise intervention with FITT criteria should be continued after discharge to prevent functional decline or restore physical function. This is consistent with the guidelines on exercise from the American College of Sports Medicine [27, 28] and other exercise recommendations [18, 19]. Exercise interventions are associated with higher activities of daily living [29], better mental health [30] and improved quality of life in older adults. Our panellists also agreed that high-intensity exercise interventions are suitable in this population if no contra-indications are present such as decompensated congestive heart failure or severe aortic stenosis [31]. Therefore, high intensity exercises can certainly be considered to restore physical function in line with the international exercise recommendation [18] Exercise interventions to regain physical functioning should be supervised by a physical therapist in older patients who are discharged from hospital with multiple chronic diseases. This is in line with the recommendation from Echeverria et al. [17]. that home-based programmes require self-discipline, and that group exercise may have an important social element. A novel finding of our study is the expert consensus that tailored exercise interventions should be tuned to the specific needs and goals (such as independent self-care, cooking or gardening) of the patient. Previous research has also suggested setting collaborative goals for complex care interventions in older patients with chronic diseases or multimorbidities [32, 33].
A COS in all domains of the ICF can give a complete overview of an older patient’s physical functioning when they return home. Geriatric syndromes such as apathy, fear of falling, fatigue, depressive symptoms [11] or undernutrition [10] are highly prevalent in older patients and prevent recovery of functioning after acute hospitalization [11]. Indicating that these syndromes are present in the handover information when a patient is discharged home from hospital might increase the success of an exercise intervention. Our expert panel agreed that if multiple risk factors are identified, other healthcare professionals should be involved in the interventions. However, it can be difficult to collect information on all ICF domains of patient functioning because this is time-consuming and burdensome for older patients. Future studies could investigate how to collect this information using wearables [34, 35].
To optimize transitional care, a seamless transition with handover information is important. However, this does not automatically prevent functional decline in older patients [36, 37]. It has been shown that exercise interventions during hospitalization can prevent functional decline or restore physical function [14, 15, 38], but the effects of exercise interventions at home after discharge have not been properly defined [16]. In older patients, the cardiopulmonary and musculoskeletal systems are often not appropriately challenged or loaded by exercise interventions. Finding the optimal FITT training parameters is crucial for recovery [39]. Future research should investigate the effectiveness and appropriateness of exercise interventions and determine how to tailor these interventions to the patient’s goals. Our expert panel agreed that eHealth should be investigated in future studies to see whether it can improve the post-discharge care of older patients with complex care needs. Evidence-based knowledge of how psychometric sound assessment tools with normative sex-related values and proper clinical reasoning can be used to tailor exercise interventions to individual older patients who have been acutely hospitalized might reduce the pathophysiological disease process and restore physical functioning.
Study strengths and limitations
The strengths of this study were the international panel with expertise in exercise interventions, the high response rate, the structured methodology and the relevance of the topic. The study also had limitations. First, although the Delphi panel was chosen with care, all panel members were from Western countries, so recommendations from this study cannot be easily extrapolated to the healthcare systems of non-Western countries. Second, most panel members have a primary background in physical therapy, so the physical therapy profession may be overrepresented in the practice recommendations. This might have influenced the choice of the selected measurement tools or exercise intervention. However, the panel had a broad view on this topic and underscored the involvement of other healthcare professionals for optimal intervention.
Conclusion
This Delphi study has provided starting points for developing an exercise intervention, COS and handover information that can prevent functional decline or restore physical functioning in older patients after discharge from hospital. The results of this Delphi study might help physical therapists to develop an exercise intervention for older patients with complex care needs after hospital discharge.
Supporting information
(DOCX)
(PDF)
Acknowledgments
This study would not have been accomplished without the help of the panel of the ‘Delphi consensus study on an exercise intervention for acutely hospitalized older patients’, whose input in the three Delphi rounds made this study possible. The study panel consisted of the following members: A.W. Heinen, MSc, D. van Wijk, MSc, G. Pijnenburg, MSc, Prof. Dr. E.L. Cadore, Dr. C.J. Liu, Dr. C. McArthur, Prof. Dr. R. Daly, Dr. A.C. Bodilsen, Dr. N. Martinez-Velilla, Dr. E.V. Papa, Dr. J. Demarteau, Dr. M. Giné-Garriga, Dr. N. de Vries, Dr. M. Tieland, Prof. Dr. P. Calders.
Data Availability
All relevant data are within the paper and its Supporting Information Files.
Funding Statement
YES: This research is supported by a doctoral grant for J.J. Aarden from NWO, the Netherlands organization for scientific research (No 023.011.059).
References
- 1.Buurman BM, Hoogerduijn JG, de Haan RJ, et al. Geriatric conditions in acutely hospitalized older patients: Prevalence and One-Year survival and functional decline. PLoS One. 2011;6(11):e26951 doi: 10.1371/journal.pone.0026951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyd CM, Ricks M, Fried LP, Guralnik JM, Xue QL, Bandeen-Roche K. Functional Decline and Recovery of Activities of Daily Living among Hospitalized, Disabled Older Women: The Women’s Health and Aging Study I. J Am Geriatr Soc. 2009;57(10):1757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: She was probably able to ambulate, but I’m not sure. JAMA. 2011;26;306(16):1782–93. [DOI] [PubMed] [Google Scholar]
- 4.Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Geronto A Biol Med Sci. 2008;63(10):1076–81. doi: 10.1093/gerona/63.10.1076 [DOI] [PubMed] [Google Scholar]
- 5.Coker RH, Hays NP, Williams RH, Wolfe RR, Evans WJ. Bed rest promotes reductions in walking speed, functional parameters, and aerobic fitness in older, healthy adults. J Geronto A Biol Med Sci. 2015;70(1):91–6. doi: 10.1093/gerona/glu123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low Mobility During Hospitalization and Functional Decline in Older Adults. J Am Geriatr Soc. 2011. Feb;59(2):266–73. doi: 10.1111/j.1532-5415.2010.03276.x [DOI] [PubMed] [Google Scholar]
- 7.Kolk D, Aarden JJ, MacNeil-Vroomen JL, et al. Factors Associated with Step Numbers in Acutely Hospitalized Older Adults: The Hospital-Activities of Daily Living Study. J Am Med Dir Assoc. 2021;22(2):425–32. doi: 10.1016/j.jamda.2020.06.027 [DOI] [PubMed] [Google Scholar]
- 8.Bodilsen AC, Klausen HH, Petersen J, et al. Prediction of Mobility Limitations after Hospitalization in Older Medical Patients by Simple Measures of Physical Performance Obtained at Admission to the Emergency Department. PLoS One. 2016;11(5):e0154350. doi: 10.1371/journal.pone.0154350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aarden JJ, Reijnierse EM, van der Schaaf M, et al. Longitudinal Changes in Muscle Mass, Muscle Strength, and Physical Performance in Acutely Hospitalized Older Adults. J Am Med Dir Assoc. 2021;22(4):839–45. doi: 10.1016/j.jamda.2020.12.006 [DOI] [PubMed] [Google Scholar]
- 10.van Dronkelaar C, Tieland M, Aarden JJ, et al. Decreased Appetite is Associated with Sarcopenia-Related Outcomes in Acute Hospitalized Older Adults. Nutrients. 2019;11:932. doi: 10.3390/nu11040932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Seben R, Reichardt LA, Aarden JJ, et al. The Course of Geriatric Syndromes in Acutely Hospitalized Older Adults: The Hospital-ADL Study. J Am Med Dir Assoc. 2019;20(2):152–58.e2. doi: 10.1016/j.jamda.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 12.Reichardt LA, van Seben R, Aarden JJ, et al. Trajectories of cognitive-affective depressive symptoms in acutely hospitalized older adults: The hospital-ADL study. J Psychosom Res. 2019;120:66–73. doi: 10.1016/j.jpsychores.2019.03.011 [DOI] [PubMed] [Google Scholar]
- 13.Hoogerduijn JG, Schuurmans MJ, Korevaar JC, Buurman BM, de Rooij SE. Identification of older hospitalised patients at risk for functional decline, a study to compare the predictive values of three screening instruments. J Clin Nurs. 2010;19(9–10):1219–25. doi: 10.1111/j.1365-2702.2009.03035.x [DOI] [PubMed] [Google Scholar]
- 14.Martinez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Inter Med 2019:1;179; 1:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanach FA, Pastva AM, Hall KS, Pavon JM, Morey MC. Effects of structured exercise interventions for older adults hospitalized with acute medical illness: a Systematic review. J Aging Phys Act 2018;01;26(2):284–303. doi: 10.1123/japa.2016-0372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verweij L, van de Korput E, Daams JG, et al. Effects of Postacute Multidisciplinary Rehabilitation Including Exercise in Out-of-Hospital Settings in the Aged: Systematic Review and Meta-analysis. Arch Phys Med Rehabil 2019;100(3):530–50. doi: 10.1016/j.apmr.2018.05.010 [DOI] [PubMed] [Google Scholar]
- 17.Echeverria I, Amasene M, Urquiza M, et al. A. Multicomponent Physical Exercise in Older Adults after Hospitalization: A Randomized Controlled Trial Comparing Short- vs. Long-Term Group-Based Interventions. Int J Environ Res Public Health. 2020:20;17(2):666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Izquierdom Merchant RA, Morley JE, et al. International exercise recommendations in older adults (ICFSR): Expert consensus guidelines. J Nutr Health Aging 2021;25(7):824–53. doi: 10.1007/s12603-021-1665-8 [DOI] [PubMed] [Google Scholar]
- 19.Baldwin CE, Philips A, Edney SM, Lewis LK. Recommendations for older adults’ physical activity and sedentary behaviour during hospitalisation for an acute medical illness: an international Delphi study. Int J Behav Nutr Phys Act 2020:25;17(1):69. doi: 10.1186/s12966-020-00970-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williamson PR, Altman DG, Blazeby JM, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012:6; 13:132. doi: 10.1186/1745-6215-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Major ME, Kwakman R, Kho ME, et al. Surviving critical illness: what is next? An expert consensus statement on physical rehabilitation after hospital discharge. Critical Care 2016; 20:354. doi: 10.1186/s13054-016-1508-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Millar AN, Daffu-O’Reily A, Hughes CM, et al. Development of a core outcome set for effectiveness trials aimed at optimising prescribing in older adults in care homes. Trials 2017;12;18(1):175. doi: 10.1186/s13063-017-1915-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–9. doi: 10.1016/j.jclinepi.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One. 2011;6(6): e20476. doi: 10.1371/journal.pone.0020476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.von der Gracht HA. Consensus measurement in Delphi studies: Review and implications for future quality assurance. Technol Forecast Soc Change. 2012;79(8):1525–36. [Google Scholar]
- 26.WHO | International Classification of Functioning, Disability and Health (ICF). WHO 2018 [cited 2019 Jun 11]; Available from: https://www.who.int/classifications/icf/en/
- 27.Thompson PD, Arena R, Riebe D, Pescatello LS, American College of Sports Medicine. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription, Ninth Edition. Curr Sports Med Rep. 2013;12(4):215–7 [DOI] [PubMed] [Google Scholar]
- 28.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 8th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 29.Papa E, Dong X, Hassan M. Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review. Clin Interv Aging. 2017;13; 12:955–61. doi: 10.2147/CIA.S104674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J Psychiatr Res. 2016; 77:42–51. doi: 10.1016/j.jpsychires.2016.02.023 [DOI] [PubMed] [Google Scholar]
- 31.Lee PG, Jackson EA, Richardson CR. Exercise prescriptions in older adults. Am Fam Physician 2017:1;95(7):425–32. [PubMed] [Google Scholar]
- 32.De Vries NM, Staal B, van der Wees PJ, et al. Patient centred physical therapy is (cost)- effective in increasing physical activity and reducing frailty in older adults with mobility problems: a randomized controlled trial with 6 months follow-up. J Cachexia Sarcopenia Muscle 2016;7(4):422–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vermunt NPCA, Harmsen M, Westert GP, Olde Rikkert MGM, Faber MJ. Collaborative goal setting with elderly patients with chronic disease or multimorbidity: a systematic review. BMC Geriatr. 2017:31;17(1):167. doi: 10.1186/s12877-017-0534-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kononova A, Li L, Kamp K, et al. The use of wearable activity trackers among older adults: Focus group study of tracker perceptions, motivators, and barriers in the maintenance stage of behavior change. JMIR Mhealth Uhealth. 2019:5;7(4):e9832. doi: 10.2196/mhealth.9832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilmink G, Dupey K, Alkire S, et al. Artificial Intelligence-powered digital health platform and wearable devices improve outcomes for older adults in assisted living communities: Pilot intervention study. JMIR Aging 2020:10;3(2):e19554. doi: 10.2196/19554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verhaeg KJ, Buurman BM, Veenboer GC, de Rooij SE, Geerlings ES. The implementation of a comprehensive discharge bundle to improve the discharge process: a quasi-experimental study. Neth J Med. 2014. Jul;72(6):318–25. [PubMed] [Google Scholar]
- 37.Buurman BM, Parlevliet JL, Allore HG, et al. Comprehensive Geriatric Assessment and Transitional Care in acutely hospitalized patients. JAMA Intern Med. 2016;176(3):302. [DOI] [PubMed] [Google Scholar]
- 38.Kosse NM, Dutmer AL, Dasenbrock L, Bauer JM, Lamoth CJC. Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: a systematic review. BMC Geriatr 2013:10; 13:107. doi: 10.1186/1471-2318-13-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zaleski AL, Taylor BA, Panza GA, Coming of age: Considerations in the prescription of exercise for older adults. ethodist Debakey Cardiovac J. 2016. Apr-Jun; 12(2): 98–104. doi: 10.14797/mdcj-12-2-98 [DOI] [PMC free article] [PubMed] [Google Scholar]