Abstract
Background
Undernutrition (Body Mass Index < 18.5 kg/m2) is a common problem and a major cause of hospital admission for patients living with HIV. Though sub-Saharan Africa is the most commonly affected region with HIV and malnutrition, a meta-analysis study that estimates the prevalence and correlates of undernutrition among adults living with HIV has not yet been conducted. The objective of this study was to determine the pooled prevalence of undernutrition and associated factors among adults living with HIV/AIDS in sub-Saharan Africa.
Methods
Studies published in English were searched systematically from databases such as PubMed, Google Scholar, and gray literature, as well as manually from references in published articles. Observational studies published from 2009 to November 2021 were included. The data extraction checklist was prepared using Microsoft Excel and includes author names, study area, publication year, sample size, prevalence/odds ratio, and confidence intervals. The results were presented and summarized in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) standard. Heterogeneity was investigated using the Q test, I2, τ2, τ and predictive interval. STATA version 17 was used to analyze the data. A meta-analysis using a random-effects model was used to determine the overall prevalence and adjusted odds ratio. The study has been registered in PROSPERO with a protocol number of CRD42021268603.
Results
In this study, a total of 44 studies and 22,316 participants were included. The pooled prevalence of undernutrition among adult people living with HIV (PLWHIV) was 23.72% (95% CI: 20.69–26.85). The factors associated with undernutrition were participants’ age (AOR = 0.5, 95% CI: 0.29–0.88), gender (AOR = 2.08, 95% CI: 0.22–20.00), World Health Organization (WHO) clinical stage (AOR = 3.25, 95% CI: 2.57–3.93), Cluster of Differentiation 4 (CD4 count) (AOR = 1.94, 95% CI: 1.53–2.28), and duration of ART (AOR = 2.32, 95% CI: 1.6–3.02).
Conclusion
The pooled prevalence of undernutrition among adult PLWHIV in sub-Saharan Africa remained high. WHO clinical stage, CD4 count, duration of ART treatment, age, and sex were found to be the factors associated with undernutrition. Reinforcing nutrition counseling, care, and support for adults living with HIV is recommended. Priority nutritional screening and interventions should be provided for patients with advanced WHO clinical stages, low CD4 counts, the male gender, younger age groups, and ART beginners.
Introduction
According to the United Nations Program on HIV/AIDS (UNAIDS) 2021 fact sheet, there were 38.4 million people living with HIV, of whom 36.7 million were adults (15 years of age or older). Seventy-six percent of adults living with HIV had access to ART treatment [1]. Sub-Saharan Africa accounted for 57% of all new HIV infections in 2019 [2]. Similarly, Eastern and Southern Africa constituted the largest number of AIDS-related deaths (280,000) globally in 2021 [1]. Despite progress in HIV care, the overall life expectancy among adults living with HIV is 5 to 10 years less than that of uninfected adults [3]. Malnutrition takes the lion’s share in increasing the risk of mortality and the occurrence of other opportunistic infections among adults living with HIV [4, 5].
Poor nutrition and HIV have bidirectional relationships and exacerbate one another [6]. In resource-limited countries like sub-Saharan Africa, many people living with HIV (PLWHIV) on long-term ART follow-up lack adequate nutrition [7, 8], and, undernutrition is an indicator of a poor prognosis of HIV care [9]. Similarly, malnutrition is among the major causes of hospital admission in PLWHIV [10]. Meanwhile, HIV affects nutritional status in three distinct ways. It decreases food consumption (through poor appetite and inability to eat and swallow), raises energy needs (up to 20% more energy), and hinders the body’s ability to absorb nutrients. All these factors predispose patients to undernutrition and finally to wasting syndrome [11]. Thus, identifying and treating malnutrition in people living with HIV can fasten recovery from infection, enhance immunity, and possibly slow the progression to AIDS [12].
A meta-analysis study in Ethiopia showed the pooled prevalence of undernutrition among adults receiving ART was 26%. Undernutrition among people living with HIV is associated with socio-demographic and clinical factors such as age, WHO clinical stage, CD4 count, duration of ART treatment, and food security [13, 14]. There is a need to estimate the overall prevalence of undernutrition in Sub-Saharan Africa, as the region remains the world’s epicenter of HIV transmission. Similarly, several studies indicated that the region is affected by food insecurity, which is directly linked to undernutrition for individuals, households, and communities affected by HIV [15–18]. Beside this, several nutritional programs to address undernutrition in adults living with HIV in sub-Saharan Africa have been instituted without consolidated evidence on the overall estimates of the prevalence and correlates of undernutrition [19]. Moreover, the available primary studies in sub-Saharan Africa lack consistency and are not conclusive. Therefore, the purpose of this meta-analysis study was to determine the pooled (overall) prevalence of undernutrition and its associated factors among adults living with HIV in sub-Saharan Africa. This study will help policymakers devise evidence-based nutrition intervention programs for patients living with HIV in sub-Saharan Africa.
Methods
Inclusion and exclusion criteria
Both published and unpublished observational studies (i.e., cross-sectional, case-control, and cohort) conducted among HIV-positive adults in SSA countries were included. Articles published only in the English language were included. On the other hand, studies with no free full texts, and studied only pregnant women were excluded. For clarity, the topic is described using a PICO format as follows:
 Population (P): Adult patients (> 15 year, as defined by UNAIDS and other studies) [20].
Population (P): Adult patients (> 15 year, as defined by UNAIDS and other studies) [20]. Intervention or exposure (I): Living with HIV
Intervention or exposure (I): Living with HIV Comparison or control (C): Living without HIV
Comparison or control (C): Living without HIV Outcome (O): Undernutrition (prevalence)
Outcome (O): Undernutrition (prevalence)
Information source and search strategy
We used the databases mainly PubMed, Google Scholar, and Gray (unpublished) literature, university repositories, and manual searches of references from a list of included articles. Articles published from 2009 to November 10, 2021, were included. We used 2009 as there was a previous study among women living with HIV and published in 2008. However, our study also included male adults. Articles identified through the electronic searches were exported and managed using EndNote Version 8 reference manager. Articles from PubMed were accessed using the following keywords (Table 1).
Table 1. The search strategy used in the PubMed database, 2021.
| Key variables | Searching words in PubMed |
|---|---|
| Prevalence of undernutrition | “Proportion” or “Prevalence” or “Magnitude” or “Burden” AND “Malnutrition” OR “Undernutrition” OR “Under-weight” OR “Wasting” OR “Malnourished” AND “Adult” AND “Living with HIV” OR “HIV-positive” OR “HIV-infected” OR “Anti-Retroviral Therapy” AND (Each country) sub-Saharan Africa”. |
| Associated factors | “Associated factors” OR “Determinants” OR “Predictors” OR “Correlates” AND “Malnutrition” OR “Undernutrition” OR “Under-weight” OR “Wasting” OR “Malnourished” AND “Adult” AND “Living with HIV” OR “HIV-positive” OR “HIV-infected” OR “Anti-Retroviral Therapy AND (Each country) in sub-Saharan Africa”. |
Studies were selected after two reviewers (AS) and (OS) independently screened for inclusion eligibility. A third author (GD) was involved in resolving disagreements between the two authors.
Data collection process and data items
The authors prepared data extraction using Microsoft Excel. All relevant data for this review were extracted by two reviewers (AS and OS). The disparities between reviewers at the time of data abstraction were resolved through discussion with the third author (ZWB).
The data extraction sheet included primary authors, publication year, country, study design, sample size, response rate, study setting, study population, proportion, 95% confidence interval, and the logarithm of proportion S1 Table.
Effect measures
We include studies that measure under-weight (undernutrition) using BMI < 18.5 Kg/m2. Underweight was utilized as an indicator of advanced malnutrition, despite the fact that it does not reliably indicate the nutritional status of adults [21]. The proportion of undernutrition was calculated by dividing the number of individuals under-nourished by the total sample of study subjects included in the final analysis. We used the adjusted odds ratio (AOR) as an effect measure to find associated factors of undernutrition.
Risk of bias assessment
Newcastle Ottawa Scale (NOS) adapted for cross-sectional studies was used to assess the quality of the studies. NOS has three categories and has a maximum score of 10 for cross-sectional studies. The categories are selection (maximum of 5 stars), comparability (maximum of 2 stars), and study outcome (maximum of 3 stars). Each study was independently appraised by two authors. Disagreements between authors were resolved through discussion with a third author. Finally, the quality score of each study was calculated as the sum of scores, thus ranging from zero to ten for cross-sectional studies, and zero to nine for cohort and case-control studies. A score of greater or equal to 6 points was considered “good” and included in the study [22]. Additionally, publication bias was assessed using Egger’s regression test, funnel plot, and sensitivity analysis.
Synthesis methods
Data analysis was performed using STATA (version 17) software. We employed a random effect model to find the pooled prevalence and associated factor estimates of under-nutrition. Heterogeneity of effect sizes was assessed using I2, τ2,τ and prediction interval. Subgroup and trim and fill were performed to deal with the potential source of heterogeneity. Sensitivity analysis was also performed. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist is used for data presentation S2 Table [23].
Results
Study selection and characteristics
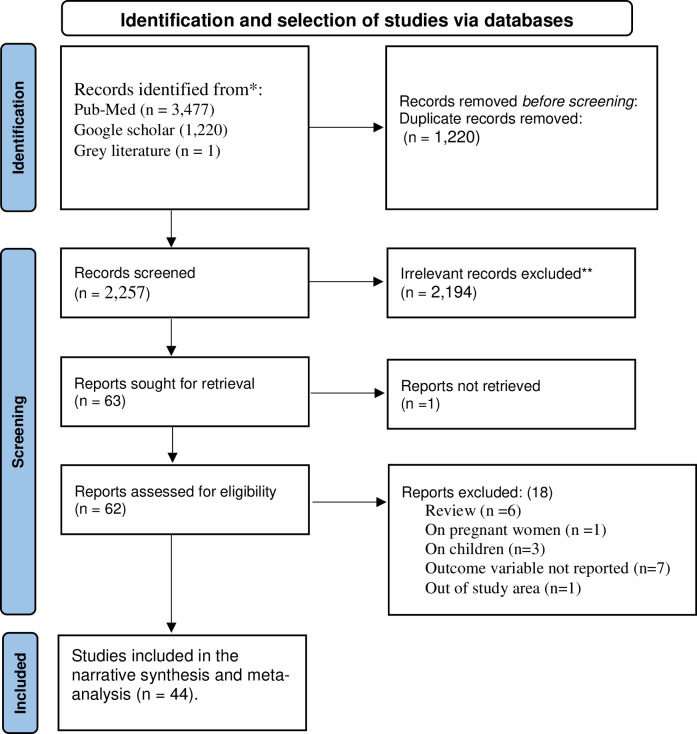
A total of 3,477 articles were identified from PubMed, Google scholar, and gray literature in the initial search. After the removal of 1,220 duplicates, 2,257 articles were screened for title and abstract. In the next step, 2,194 articles were excluded based on titles and abstracts. The full texts of 62 articles were downloaded and assessed against inclusion criteria. Thus, 18 articles were excluded for the following reasons: 7 studies did not report data on the outcome variable [5, 24–29], six studies were review papers [4, 14, 30–33], three studies focused on children [30, 34, 35], one study was conducted out of SSA [36], one study focused on pregnant women [37], and one study lacks full text [38]. Finally, 44 studies were included in final systematic review and meta-analysis (Fig 1) [23]. No studies were excluded after appraising the quality using NOS.
Fig 1. Flow chart showing the sequence of study selection on undernutrition among adult PLWHIV in sub-Saharan Africa, 2009–2021.
In this study, a total of 22,316 adults living with HIV were included. The sample size of the included studies ranged from 145 in Botswana to 3,993 in Tanzania. Of the 44 included studies, only one was a retrospective cohort and the rest were carried out using cross-sectional study designs. The largest number of articles (33 studies) were reported from Ethiopia [8, 39–70] and only one article is reported from Kenya [71], Botswana [72], Ghana [73], Democratic Republic of Congo (DRC) [74], Senegal [75], Uganda [76], and Zimbabwe [77]. Four articles were from each of South Africa [78, 79] and Tanzania [13, 80]. Regarding the publication year, studies were published from 2009 to 2021 and the majority of the studies (11), were reported in 2020, followed by nine in 2017, and five in each of 2018 and 2015 (Tables 2 and 3).
Table 2. Study characteristics included in meta-analysis of undernutrition among adult PLWHIV in sub-Saharan Africa, 2009–2021.
| S. N | Authors | Publication Year | Country | Sample Size | Study design | Mean/ age range (year) | ART Status | No of cases | P | 95% CI | NOS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Adal M, Howe R, Kassa D et al | 2018 | Ethiopia | 594 | Cross-sectional | 34 | Pre-ART | 87 | 15.1 | 12.2–17.9 | 6 | |
| 2 | Akilimali PZ, Musumari PM, Kashala-Abotnes E et al | 2016 | DRC | 583 | Cross-sectional | 41 | On ART | 141 | 24.1 | 20.6–27.6 | 8 | |
| 3 | Amza L, Demissie T, Halala Y. | 2017 | Ethiopia | 519 | Cross-sectional | 18–45+ | On ART | 133 | 26.6 | 22.8–30.4 | 8 | |
| 4 | Asnakew M. | 2015 | Ethiopia | 340 | Cross-sectional | 35 | On ART | 103 | 31.2 | 26.3–30.1 | 7 | |
| 5 | Benzekri NA, Sambou J, Diaw B, | 2015 | Senegal | 109 | Cross-sectional | 45 | On ART | 25 | 22.9 | 15.0–30.8 | 6 | |
| 6 | Birhane M, Loha E, Alemayehu FR. | 2015 | Ethiopia | 389 | Cross-sectional | 40 | On ART | 60 | 25 | 20.7–29.3 | 8 | |
| 7 | Daka DW, Ergiba MS. | 2020 | Ethiopia | 1062 | Cross-sectional | 16–50+ | On ART | 357 | 34 | 31.1–36.8 | 8 | |
| 8 | Daniel M, Mazengia F, Birhanu D. | 2013 | Ethiopia | 408 | Cross-sectional | 18–45+ | Pre & on ART | 104 | 25.5 | 21.3–29.7 | 8 | |
| 9 | M Dedha, M Damena, G Egata et al | 2017 | Ethiopia | 459 | Cross-sectional | 35 | On ART | 131 | 30 | 25.8–34.2 | 7 | |
| 10 | Fentie M, Wassie MM, Tesfahun A, | 2017 | Ethiopia | 317 | Cross-sectional | 39 | On ART | 57 | 18.3 | 14.0–22.6 | 6 | |
| 11 | Fufa H, Umeta M, Taffesse S et al | 2009 | Ethiopia | 153 | Cross-sectional | 27 | Pre-ART | 27 | 18 | 11.9–24.1 | 7 | |
| 12 | Gebru TH, Mekonen HH, Kiros KG. | 2020 | Ethiopia | 394 | Cross-sectional | 41 | On ART | 169 | 42.9 | 38.0–47.8 | 7 | |
| 13 | Gedle D, Gelaw B, Muluye D, | 2015 | Ethiopia | 305 | Cross-sectional | 40 | On ART | 77 | 25.2 | 20.3–30.1 | 8 | |
| 14 | Girma M, Motuma A, Negasa L. | 2017 | Ethiopia | 502 | Cross-sectional | 24 | Pre & on ART | 133 | 26.5 | 22.6–30.4 | 8 | |
| 15 | Gebremichael DY, Hadush KT, Kebede EM, et al | 2018 | Ethiopia | 512 | Cross-sectional | 34 | On ART | 119 | 23.6 | 19.9–27.3 | 8 | |
| 16 | Hadgu TH, Worku W, Tetemke D, et al | 2013 | Ethiopia | 276 | Cross-sectional | 33 | On ART | 159 | 42.3 | 36.5–48.1 | 6 | |
| 17 | Hailemariam S, Bune GT, Ayele HT et al | 2013 | Ethiopia | 520 | Cross-sectional | 34 | On ART | 64 | 12.3 | 9.4–15.1 | 8 | |
| 18 | Kabalimu TK, Sungwa E, Lwabukuna WC. | 2018 | Tanzania | 125 | Cross-sectional | 20–60+ | On ART | 24 | 19.4 | 12.5–26.3 | 6 | |
| 19 | Kenea MA, Garoma S, Gemede HF. | 2015 | Ethiopia | 423 | Cross-sectional | 15–50+ | On ART | 112 | 26.47 | 22.3–30.7 | 7 | |
| 20 | Getaw Kume | 2017 | Ethiopia | 457 | Cross-sectional | 41 | On ART | 53 | 12.3 | 9.3–15.3 | 8 | |
| 21 | Mahlangu K, Modjadji P, Madiba S. | 2020 | South Africa | 480 | Cross-sectional | 35 | On ART | 62 | 13 | 9.9–16.0 | 7 | |
| 22 | Mitiku A, Ayele TA, Assefa M, et al | 2016 | Ethiopia | 452 | Cross-sectional | 35 | On ART | 105 | 23.2 | 19.3–27.1 | 7 | |
| 23 | Motuma A, Abdeta T. | 2021 | Ethiopia | 502 | Cross-sectional | 37 | On ART | 133 | 26.5 | 22.6–30.4 | 8 | |
| 24 | Mulu H, Hamza L, Alemseged F. | 2016 | Ethiopia | 109 | Cross-sectional | 33 | On ART | 51 | 46.8 | 37.4–56.2 | 6 | |
| 25 | Naidoo K, Yende-Zuma N, Augustine S | 2018 | South Africa | 1000 | Retrospective cohort | NR | On ART | 149 | 15.7 | 13.5–17.9 | 7 | |
| 26 | Nanewortor BM, Saah FI, Appiah PK, et al | 2021 | Ghana | 152 | Cross-sectional | 39 | On ART | 21 | 13.8 | 8.3–19.3 | 6 | |
| 27 | Nigusso FT, Mavhandu-Mudzusi AH | 2020 | Ethiopia | 390 | Cross-sectional | 36 | On ART | 232 | 60 | 55.1–64.9 | 7 | |
| 28 | Nnyepi MB | 2009 | Botswana | 145 | Cross-sectional | 33 | Pre & on ART | 41 | 28.5 | 21.2–35.9 | 6 | |
| 29 | Odwee A, Kasozi KI, Acup CA, | 2020 | Uganda | 253 | Cross-sectional | 39 | On ART | 26 | 10.28 | 6.5–14.0 | 7 | |
| 30 | Oumer B, Boti N, Hussen S, et al | 2019 | Ethiopia | 333 | Cross-sectional | 33 | On ART | 79 | 23.72 | 19.2–28.3 | 7 | |
| 31 | Regassa TM, Gudeta TA. | 2020 | Ethiopia | 1007 | Cross-sectional | 18–50+ | On ART | 154 | 16 | 13.7–18.3 | 8 | |
| 32 | Sahile AT, Ayehu SM, Fanta SF. | 2021 | Ethiopia | 319 | Cross-sectional | 31–41+ | On ART | 61 | 19.1 | 14.8–23.4 | 6 | |
| 33 | Saito A, Karama M, Kamiya Y. | 2020 | Kenya | 251 | Cross-sectional | 38 | On ART | 21 | 8.3 | 4.9–11.7 | 6 | |
| 34 | Saliya MS, Azale T, Alamirew A, | 2018 | Ethiopia | 428 | Cross-sectional | 36 | On ART | 97 | 24.1 | 20.1–28.2 | 7 | |
| 35 | Shifera N, Molla A, Mesafint G, et al | 2020 | Ethiopia | 402 | Cross-sectional | 34 | On ART | 115 | 29.2 | 24.8–33.6 | 7 | |
| 36 | Sunguya BF, Ulenga NK, Siril H,et al | 2017 | Tanzania | 3993 | Cross-sectional | 38 | Pre-ART | 1106 | 27.7 | 26.3–29.1 | 9 | |
| 37 | Takarinda KC, Mutasa-Apollo T, Madzima B, et al | 2017 | Zimbabwe | 1,242 | Cross-sectional | 41 | On ART | 122 | 10 | 8.3–11.7 | 8 | |
| 38 | Takele AE, Engida AR. | 2017 | Ethiopia | 295 | Cross-sectional | 34 | On ART | 71 | 24 | 19.1–28.9 | 7 | |
| 39 | Teklu T, Chauhan NM, Lemessa F, et al | 2020 | Ethiopia | 519 | Cross-sectional | 41 | On ART | 95 | 18.3 | 14.9–21.6 | 7 | |
| 40 | Teshome | 2017 | Ethiopia | 302 | Cross-sectional | 36 | On ART | 81 | 27.2 | 22.2–32.2 | 6 | |
| 41 | Wasie B, Kebede Y, Yibre A. | 2010 | Ethiopia | 331 | Cross-sectional | 34 | On ART | 92 | 27.8 | 22.9–32.6 | 6 | |
| 42 | Wasihun Y, Yayehrad M, Dagne S et al | 2020 | Ethiopia | 350 | Cross-sectional | 35 | On ART | 85 | 26.9 | 22.3–31.6 | 6 | |
| 43 | Yitbarek GY, Engidaw MT, Ayele BA, et al | 2020 | Ethiopia | 263 | Cross-sectional | 38 | On ART | 30 | 11.9 | 7.9–15.8 | 6 | |
| 44 | Zemede Z, Tariku B, Kote M, et al | 2019 | Ethiopia | 351 | Cross-sectional | 40 | On ART | 64 | 18.23 | 14.2–22.3 | 7 | |
DRC: Democratic Republic of Kongo
ART: Antiretroviral therapy, NR: Not reported
Table 3. Sub-group analysis of the prevalence of undernutrition among adults living with HIV in sub-Saharan Africa by country, study design, and publication year, 2009–2021.
| Variables | Responses | No of studies | Pooled prevalence (95% CI) | I2 (p-value) |
|---|---|---|---|---|
| Country | Ethiopia | 33 | 25.8% (22.4–29.3) | 95.9% (0.001) |
| Tanzania | 2 | 24.3% (16.3–32.3) | 81.08% (0.022) | |
| South Africa | 2 | 14.5% (14.9–17.2) | 49.33% (0.16) | |
| Kenya | 1 | 8.3% (4.9–11.7) | - | |
| DRC | 1 | 24.1% (20.6–27.6) | - | |
| Senegal | 1 | 22.9% (15.0–30.8) | - | |
| Botswana | 1 | 28.5% (21.2–35.9) | - | |
| Ghana | 1 | 13.8% (8.3–19.3) | - | |
| Uganda | 1 | 10.3% (6.5–14.0) | - | |
| Zimbabwe | 1 | 10% (8.3–11.6) | - | |
| Study design | Cross-sectional | 43 | 23.9% (20.9–26.9) | 96.67% (0.001) |
| Retrospective cohort | 1 | 15.7% (13.4–17.9) | - | |
| Publication year | 2009–2015 | 11 | 25.8% (21.3–30.3) | 89.72% (0.001) |
| 2016–2021 | 33 | 23.1% (19.4–26.8) | 97.52% (0.001) | |
| ART characteristics | Pre-ART | 3 | 20.5% (12.6–28.3) | 95.32% (0.001) |
| Both “on & pre” ART | 3 | 26.4% (23.7–29.1) | 0.00% (0.783) | |
| On ART | 38 | 23.8 (20.4–27.2) | 96.84% (0.001) |
NB: meta-analysis works when two or more effect estimates are reported
Quality appraisal results
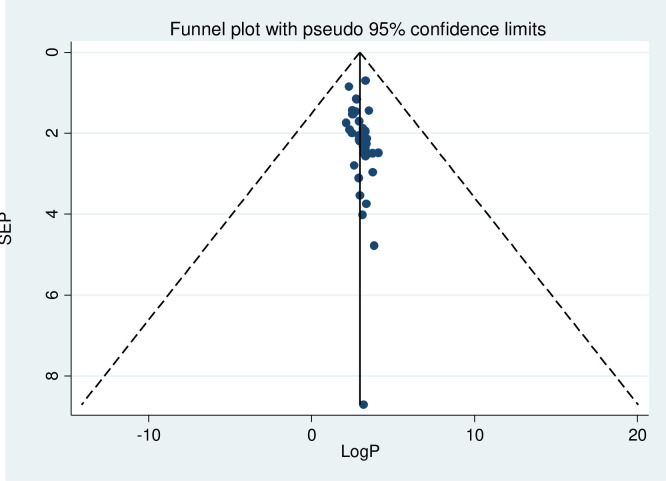
The heterogeneity test of the study revealed I2 = 96.8%, τ2 = 98.83, τ = 9.94, prediction interval (13.8–33.68%), and 95% confidence interval of the average estimate (20.69–26.79%). The source of high I2 is not identified, though it is expected to rise in a meta-analysis of proportions in different countries, and the result should be interpreted conservatively [81]. Furthermore, the study also demonstrated a wide prediction interval, a direct and easily interpretable indicator as compared to the confidence interval, implying evidence of high heterogeneity. Regarding the publication bias, Egger’s regression test (B1 = 5.72, p = 0.002) showed there was publication bias but studies looked relatively symmetrical in the funnel plot (Fig 2). However, these indicators of publication bias were developed in the context of comparative data and may not be reliable indicators of publication bias in a meta-analysis of proportions [82].
Fig 2. Funnel plot of studies on undernutrition among adult PLWHIV in SSA, 2009–2021.
Sub-group analysis and trim and fill analysis were also performed to deal with the publication bias and heterogeneity S3 Table. A sensitivity analysis was performed and all estimates were within the confidence interval limit, and no individual study contributed to the publication bias. Consequently, it is unnecessary to exclude studies from the final meta-analysis.
Meta-analysis results
Prevalence of undernutrition among adult PLWHIV in sub-Saharan Africa
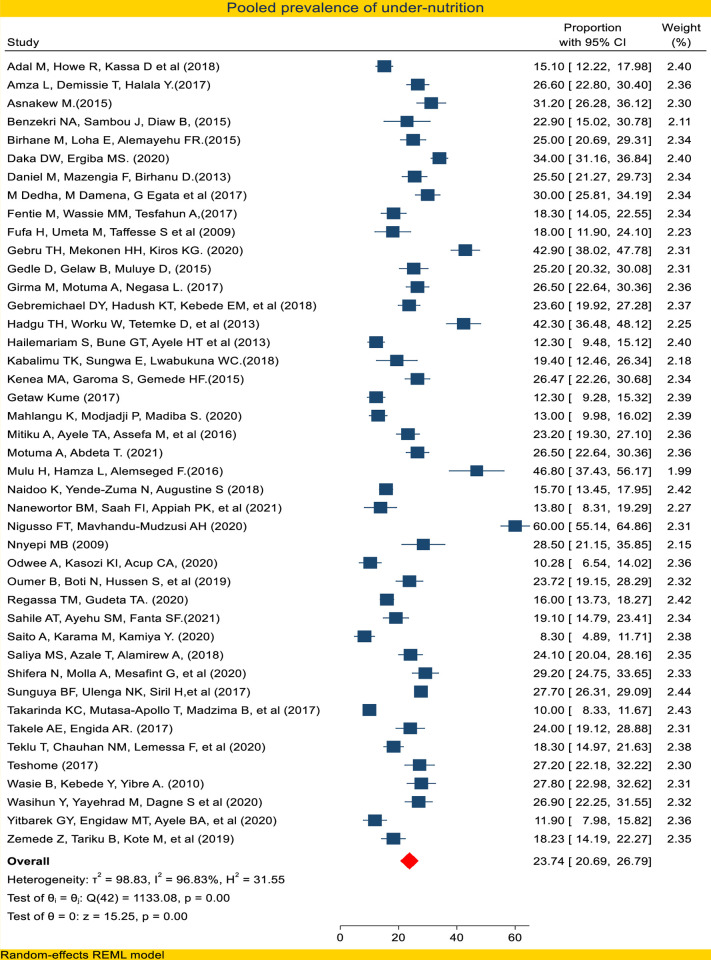
Of the 44 studies that reported a proportion of undernutrition, the highest prevalence (60%) was reported in Ethiopia [58], whereas the lowest (8.3%) was reported in Kenya [71]. Majority of the studies are reported from Ethiopia (33 studies), cross-sectional design (43 studies), carried out during 2016–2021 (33 studies), and on patients taking ART (38 studies).
In this study, the pooled prevalence of undernutrition using a random-effect model meta-analysis was found to be 23.74% (95% CI: 20.77–26.73) (Fig 3). Sub-group analysis by country showed 25.8% (95% CI: 22.4–29.3) in Ethiopia, 14.5% (95% CI: 14.9–17.2) in South Africa, and 24.3% (95% CI: 16.3–32.3) in Tanzania. Additional sub-group analysis by ART status, by study design, and by publication year also carried out (Table 3).
Fig 3. Forest plot of pooled prevalence of undernutrition among adult PLWHIV in sub-Saharan Africa 2021.
Factors associated with undernutrition among adults of PLWHIV in sub-Saharan Africa
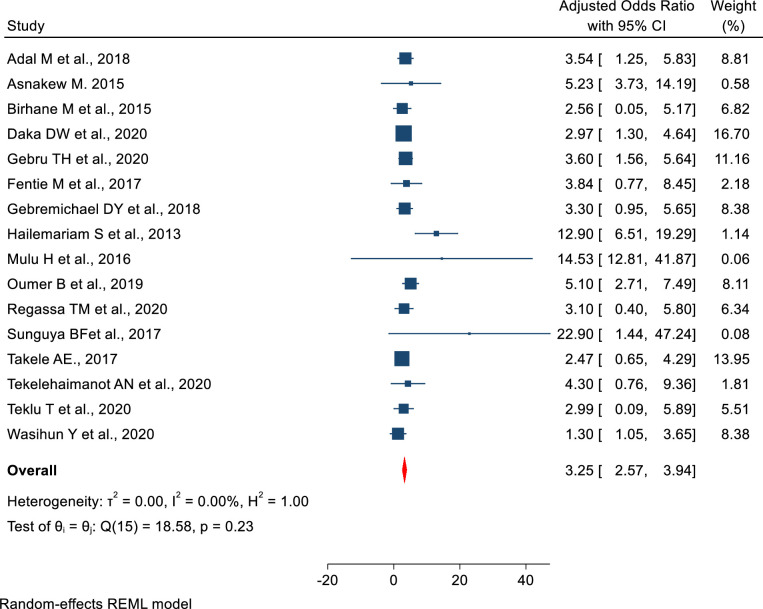
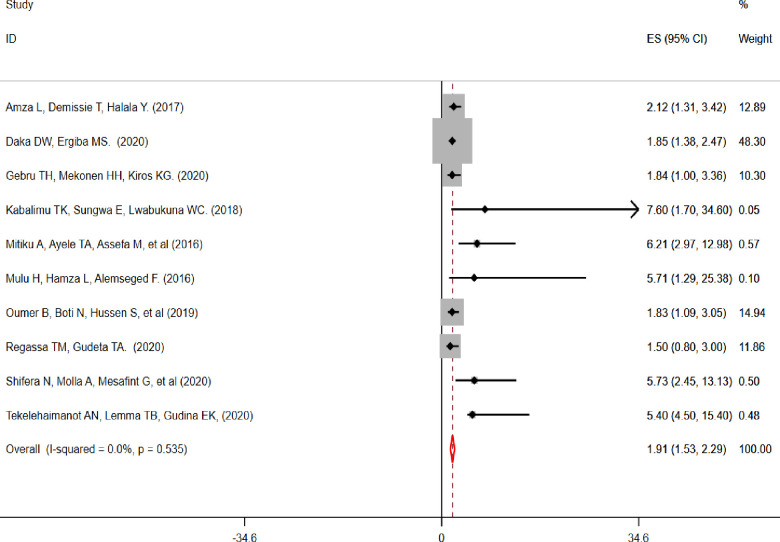
From the searched published articles 16 reported “WHO clinical stage” [13, 39, 41–43, 45, 47, 50, 52, 57, 59, 60, 64–66, 68, 83], four studies reported “CD4 count” [40, 43, 47, 55, 57, 59, 60, 80, 83], four studies reported patient’s “age” [13, 39, 55, 56, 60, 77], four studies reported “sex” [40, 56, 64, 80, 83], and four articles reported “duration of ART treatment” [8, 59, 64, 67, 68] as factors associated with undernutrition among adult PLWHIV in sub-Saharan Africa (Table 4). Patients living with HIV and WHO clinical stage III/IV were 3.25 (AOR, 95% CI: 2.57–3.93) times higher odds of developing undernutrition as compared to WHO clinical stage I/II (Fig 4). Similarly, patients whose CD4 count was less than 200cells/mm3 were 1.94 times (AOR = 1.94, 95% CI: 1.53–2.28) with higher odds of developing undernutrition as compared to their counterparts (CD4 ˃500cells/mm3) (Fig 5).
Table 4. Summary of the factors associated with undernutrition among adults living with HIV in sub-Saharan Africa, 2021.
| Factor | No of included studies | Pooled AOR (95% CI) | I2 (p-value) | Reference category |
|---|---|---|---|---|
| WHO clinical stage | 16 | 3.25 (2.57–3.94) | I2 = 0.0% (0.233) | WHO clinical Stage I |
| CD4 count | 10 | 1.91 (1.53–2.29) | I2 = 0.0% (0.535) | CD4 ˃ 500 cells /mm3 |
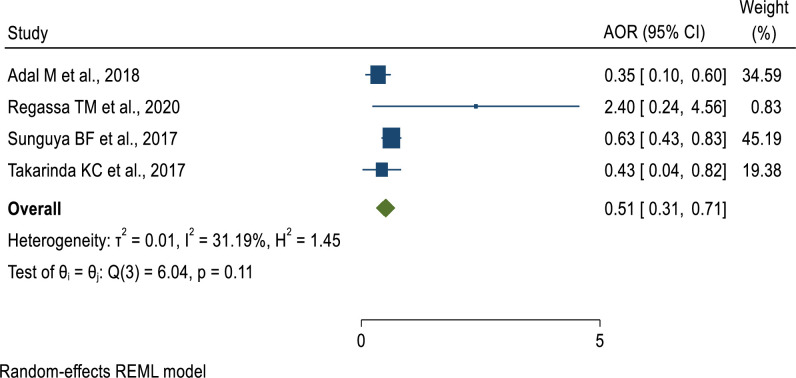
| Age | 4 | 0.51 (0.31–0.71) | I2 = 31.2% (0.11) | 19–30 years |
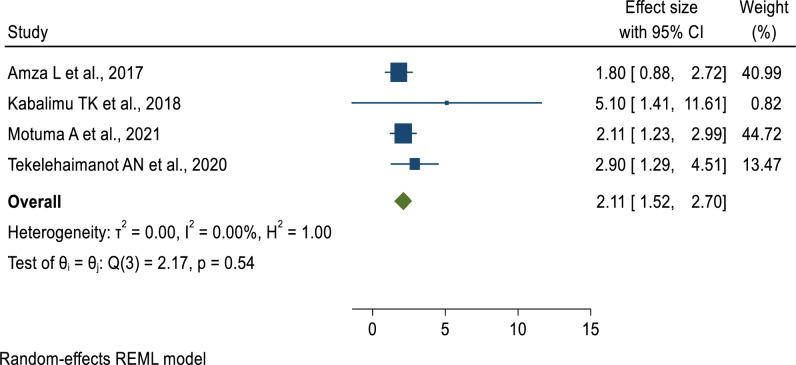
| Sex | 4 | 2.11 (1.52–2.7) | I2 = 0.0% (0.534) | Females |
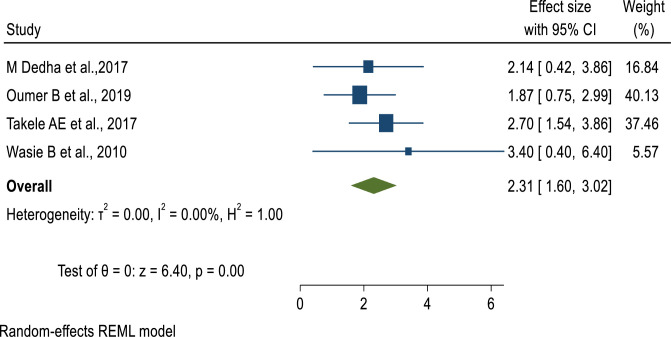
| ART duration | 4 | 2.31 (1.6–3.02) | I2 = 0.0% (0.001) | ≥12 months |
Fig 4. The pooled effect of “WHO clinical stage” on undernutrition among adult PLWHIV in sub-Saharan Africa, 2021.
Fig 5. Pooled effect of “CD4 count” on undernutrition among adult PLWHIV in sub-Saharan Africa, 2021.
Regarding the age of study participants, patients aged 40 years and above had 49% lower odds of developing undernutrition as compared to those aged 19 to 30 years (AOR = 0.51, 95% CI: 0.26–0.76) (Fig 6). Furthermore, the odds of developing undernutrition among males living with HIV were 2 times (AOR = 2.11, 95% CI: 1.52–2.7) higher as compared to female patients (Fig 7). Similar to this, patients receiving ART for less than 12 months had 2.68 times the risk of developing undernutrition compared to individuals taking it for more than 12 months (Fig 8). This implies that the longer the duration of patients’ taking ART, the lower the risk of developing under-nutrition.
Fig 6. Pooled effect of “age” of study participants on undernutrition among adult PLWHIV in sub-Saharan Africa, 2021.
Fig 7. Pooled effect of “sex” on undernutrition among adult PLWHIV in sub-Saharan Africa, 202.
Fig 8. Pooled effect of “ART duration” on undernutrition among adult PLWHIV in sub-Saharan Africa, 2021.
Discussion
Despite the improvement of comprehensive HIV care, sub-Saharan Africa continues to be an epicenter of HIV transmission and has a high prevalence of malnutrition among adults living with HIV. This study aimed to investigate the pooled prevalence and correlates of undernutrition among adults living with HIV/AIDS. The result shows a significant number of adults living with HIV are malnourished, and several socio-demographic and clinical factors have been associated with undernutrition.
In this meta-analysis, the pooled prevalence of undernutrition (adult BMI <18.5kg/m2) among adults living with HIV was high (23.74%) and interpreted as a serious situation according to WHO nutrition landscape information system cut-off values (20–39%) [84]. It is serious because studies have shown that undernutrition increases the risk of opportunistic infections (OIs) and mortality [4, 85]. The pooled prevalence slightly decreased from 25.8% in 2009–2015 to 23% in 2015–2021. This might be attributed to the expansion of nutrition intervention programs and the improvement of comprehensive HIV care in Africa. This finding is in line with a previous meta-analysis study in Ethiopia, in which the pooled prevalence was reported as 26% (95% CI: 22–30%) [14].
In contrast, our finding is higher as compared to a previous meta-analysis study conducted on women living with HIV in sub-Saharan Africa: 10.3% (95% CI: 7.4%–14.1%). The study used secondary data from the DHS and analyzed the reported estimate of only 11 sub-Saharan African countries. The disparity might be explained by the fact that over the last 13 years, there have been changes in socio-demography, the trend of HIV incidence, food insecurity, and other population factors that might have been associated with undernutrition. Moreover, the study was carried out only among women, which may have affected the result. Nevertheless, our study also asserts that men living with HIV are at a higher risk of developing malnutrition as compared to women [37], even though the biological mechanism is not clear.
We also found that patients with an advanced WHO clinical stage, a lower CD4 count, being of male sex, a younger age, and a shorter duration of ART treatment had a higher likelihood of developing undernutrition in adults living with HIV. The factor regarding the WHO clinical stage was also reported in a meta-analysis report in Ethiopia [86]. This may be due to the advanced WHO clinical stage and low CD4 count, which are indicators of severe immune deficiency are directly linked to undernutrition, especially protein and energy malnutrition. Thus, it is important to give due emphasis to nutrition counseling and supplementation with high-energy and protein foods during the follow-up visit.
Furthermore, young adults and ART beginners were identified as being at risk for malnutrition. The reason for the younger ages might be due to the poor emotional readiness to accept the disease condition and the failure to receive comprehensive HIV care at an early age. On the other hand, increasing age may improve acceptance and the perceived benefits of adherence to recommendations by health care providers. However, the result for younger ages requires further exploration. In spite of this, although it is acknowledged that receiving ART improves nutritional status, the impact of HIV on nutrition begins even before diagnosis and needs a longer course of therapy in order to be reversed, and noticed by anthropometric measurements.
Limitation of the study
The possible limitation for this review was the inability of accessing some databases like EMBASE, CINHAL, and Scopus. This was compensated by searching for published articles in broad databases like Google scholar. The other limitation is the absence of similar meta-analysis studies for comparison of our result. There is an uneven distribution of included studies among countries, a large number of which were reported from Ethiopia. Additionally, there is high heterogeneity, and studies published only in English were included.
Conclusion
The pooled prevalence of undernutrition among adult PLWHIV in sub-Saharan Africa remained high. WHO clinical stage, CD4 count, duration of ART treatment, age, and sex were found to be the factors associated with undernutrition. Reinforcing nutrition counseling, care, and support for adults living with HIV is recommended. Priority nutritional screening and interventions should be provided for patients with advanced WHO clinical stages, low CD4 counts, the male gender, younger age groups, and ART beginners.
Supporting information
(XLSX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.UNAIDS. Fact Sheet. 2022. [Google Scholar]
- 2.UNAIDS. 2020 Global AIDS Update: Seizing the moment. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS. 2020. [Google Scholar]
- 3.Cawley C, Wringe A, Todd J, Gourlay A, Clark B, Masesa C, et al. Risk factors for service use and trends in coverage of different HIV testing and counselling models in northwest T anzania between 2003 and 2010. Tropical Medicine & International Health. 2015;20(11):1473–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alebel A, Demant D, Petrucka P, Sibbritt D. Effects of undernutrition on mortality and morbidity among adults living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. BMC infectious diseases. 2021;21(1):1–20. doi: 10.1186/s12879-020-05706-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masiira B, Baisley K, Mayanja BN, Kazooba P, Maher D, Kaleebu P. Mortality and its predictors among antiretroviral therapy naïve HIV-infected individuals with CD4 cell count≥ 350 cells/mm3 compared to the general population: data from a population-based prospective HIV cohort in Uganda. Global health action. 2014;7(1):21843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piwoz E, Preble E. Policy Brief: HIV, Food Security and Nutrition. Retrieved August. 2000;21:2009. [Google Scholar]
- 7.Osei Akumiah P, Akuamoah Sarfo L, Agyekum O, Asare K, Azumah Nayembil D, Ofosu Agyapong G, et al. Nutritional Knowledge, Attitude and Intake among HIV Patients: A Study at Agogo Presbyterian Hospital, Ghana. 2015. [Google Scholar]
- 8.Dedha M, Damena M, Egata G, Negesa L. Undernutrition and associated factors among adults human immunodeficiency virus positive on antiretroviral therapy in hospitals, East Hararge Zone, Oromia, Ethiopia: A cross-sectional study. International journal of health sciences. 2017;11(5):35. [PMC free article] [PubMed] [Google Scholar]
- 9.Fadeiye E, Adegbenro C, Olumakaiye M. Assessment of nutritional knowledge of HIV positive adult patients of obafemi awolowo university teaching hospitals complex ile-ife, nigeria. J Nutr Health Sci. 2016;3:102. [Google Scholar]
- 10.Ford N, Shubber Z, Meintjes G, Grinsztejn B, Eholie S, Mills EJ, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. The lancet HIV. 2015;2(10):e438–e44. doi: 10.1016/S2352-3018(15)00137-X [DOI] [PubMed] [Google Scholar]
- 11.Project F, Project L. Nutrition and HIV/AIDS: A training manual for nurses and midwives. ECSA-HC (East, Central, and Southern African Health Community) Arusha; 2008. [Google Scholar]
- 12.Health FMo. Ethiopian Guide to Clinical Nutrition Care for Children and Adults with HIV. 2008. [Google Scholar]
- 13.Sunguya BF, Ulenga NK, Siril H, Puryear S, Aris E, Mtisi E, et al. High magnitude of under nutrition among HIV infected adults who have not started ART in Tanzania—a call to include nutrition care and treatment in the test and treat model. BMC nutrition. 2017;3(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alebel A, Kibret GD, Petrucka P, Tesema C, Moges NA, Wagnew F, et al. Undernutrition among Ethiopian adults living with HIV: a meta-analysis. BMC nutrition. 2020;6(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aibibula W, Cox J, Hamelin A-M, Mamiya H, Klein MB, Brassard P. Food insecurity and low CD4 count among HIV-infected people: a systematic review and meta-analysis. AIDS care. 2016;28(12):1577–85. doi: 10.1080/09540121.2016.1191613 [DOI] [PubMed] [Google Scholar]
- 16.Drammeh W, Hamid NA, Rohana A. Determinants of household food insecurity and its association with child malnutrition in Sub-Saharan Africa: A review of the literature. Current Research in Nutrition and Food Science Journal. 2019;7(3):610–23. [Google Scholar]
- 17.Giller KE. The food security conundrum of sub-Saharan Africa. Global Food Security. 2020;26:100431. [Google Scholar]
- 18.Saha S, Behnke A, Oldewage-Theron W, Mubtasim N, Miller M. Prevalence and Factors Associated with Food Insecurity among Older Adults in Sub-Saharan Africa: A Systematic Review. Journal of Nutrition in Gerontology and Geriatrics. 2021;40(4):171–96. doi: 10.1080/21551197.2021.1988027 [DOI] [PubMed] [Google Scholar]
- 19.Tesfay FH, Javanparast S, Gesesew H, Mwanri L, Ziersch A. Characteristics and impacts of nutritional programmes to address undernutrition of adults living with HIV in sub-Saharan Africa: a systematic review of evidence. BMJ Open. 2022;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dwyer-Lindgren L, Cork MA, Sligar A, Steuben KM, Wilson KF, Provost NR, et al. Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature. 2019;570(7760):189–93. doi: 10.1038/s41586-019-1200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koethe JR, Heimburger DC. Nutritional aspects of HIV-associated wasting in sub-Saharan Africa. The American journal of clinical nutrition. 2010;91(4):1138S–42S. doi: 10.3945/ajcn.2010.28608D [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. 2011:1–12. [Google Scholar]
- 23.Page MJ MJ, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372(71). doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tadele M, Tesfa M, Tsegaye G, Temesgen H, Alamirew NM. Determinants of chronic energy deficiency among adults living with HIV in Shebel Berenta District, East Gojjam, Amhara region, North West Ethiopia, 2017: case control study. BMC research notes. 2019;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oluma A, Abadiga M, Mosisa G, Etafa W, Fekadu G. Food Insecurity among people living with HIV/AIDS on ART follower at public hospitals of Western Ethiopia. International Journal of Food Science. 2020;2020. doi: 10.1155/2020/8825453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kassie AM, Abate BB, Kassaw MW. Prevalence of overweight/obesity among the adult population in Ethiopia: a systematic review and meta-analysis. BMJ open. 2020;10(8):e039200. doi: 10.1136/bmjopen-2020-039200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalil FS, Kabeta T, Jarso H, Hasen M, Ahmed J, Kabeta S. Determinants of Undernutrition Among Adult People on Antiretroviral Therapy in Goba Hospital, Southeast Ethiopia: A Case–Control Study. Nutrition and Dietary Supplements. 2020;12:223–36. [Google Scholar]
- 28.Getahun MB, Teshome GS, Fenta FA, Bizuneh AD, Mulu GB, Kebede MA. Determinants of Severe Acute Malnutrition Among HIV-positive Children Receiving HAART in Public Health Institutions of North Wollo Zone, Northeastern Ethiopia: Unmatched Case–Control Study. Pediatric Health, Medicine and Therapeutics. 2020;11:313. doi: 10.2147/PHMT.S267892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gedle D, Mekuria G, Kumera G, Eshete T, Feyera F, Ewunetu T. Food insecurity and its associated factors among people living with HIV/AIDS receiving anti-retroviral therapy at Butajira Hospital, Southern Ethiopia. Journal of Nutrition & Food Sciences. 2015;5(2):2–6. [Google Scholar]
- 30.Nigussie J, Girma B, Molla A, Mareg M. Under-nutrition and associated factors among human immunodeficiency virus-infected children in sub-Saharan Africa: A systematic review and meta-analysis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mengie T, Dejen D, Muche T, Getacher L, Kindie B, Tamiru C, et al. Under Nutrition and Its Determinants Among Adults Receiving Antiretroviral Therapy in Ethiopia: A Systematic Review and Meta-analysis. [Google Scholar]
- 32.Hidru HD, Gebremedhine H, Gebretsadik A, Teame H, Negash H, Mengesha MB. Prevalence of Food Insecurity and Its Associated Factors among Adult People with Human Immunodeficiency Virus in Ethiopia: A Systematic Review and Meta-Analysis. International Journal of Food Science. 2021;2021. doi: 10.1155/2021/7816872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abate BB, Aragie TG, Tesfaw G. Magnitude of underweight, wasting and stunting among HIV positive children in East Africa: A systematic review and meta-analysis. PloS one. 2020;15(9):e0238403. doi: 10.1371/journal.pone.0238403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tiruneh CM, Walle BG, Emiru TD, Tibebu NS, Abate MW, Nigat AB, et al. Under-nutrition and associated factors among children on ART in Southern Ethiopia: a facility-based cross-sectional study. Italian Journal of Pediatrics. 2021;47(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gondar E. PREVALENCE OF MALNUTRITION AND ASSOCIATED FACTORS AMONG HIVINFECTED CHILDREN AGED 6–59 MONTHS AT GONDAR UNIVERSITY HOSPITAL. NORTHWEST ETHIOPIA: DEPARTMENT OF PEDIATRICS AND CHILDHEALTH, COLLEGE OF MEDICINE AND HEATLH. 2014. [Google Scholar]
- 36.Thapa R, Amatya A, Pahari DP, Bam K, Newman MS. Nutritional status and its association with quality of life among people living with HIV attending public anti-retroviral therapy sites of Kathmandu Valley, Nepal. AIDS research and therapy. 2015;12(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uthman OA. Prevalence and pattern of HIV-related malnutrition among women in sub-Saharan Africa: a meta-analysis of demographic health surveys. BMC public health. 2008;8(1):1–8. doi: 10.1186/1471-2458-8-226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Debebe L. Under nutrition and Associated Factors among Adults Living with Hiv/Aids Attending in Selected Public Hospitals in Addis Ababa, Ethiopia: A Cross-Sectional Study 2019. [Google Scholar]
- 39.Adal M, Howe R, Kassa D, Aseffa A, Petros B. Malnutrition and lipid abnormalities in antiretroviral naive HIV-infected adults in Addis Ababa: a cross-sectional study. PloS one. 2018;13(4):e0195942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amza L, Demissie T, Halala Y. Under nutrition and associated factors among adult on highly active antiretroviral therapy in Wolaita Sodo teaching and referral hospital, southern nations nationalities peoples region, Ethiopia. International Journal of Nutrition and Metabolism. 2017;9(2):10–9. [Google Scholar]
- 41.Asnakew M. Malnutrition and associated factors among adult individuals receiving highly active antiretroviral therapy in health facilities of Hosanna Town, Southern Ethiopia. Open Access Library Journal. 2015;2(01):1. [Google Scholar]
- 42.Birhane M, Loha E, Alemayehu FR. Nutritional status and associated factors among adult HIV/AIDS patients receiving ART in Dilla University Referral Hospital, Dilla, Southern Ethiopia. Research Gate. 2017. [Google Scholar]
- 43.Daka DW, Ergiba MS. Prevalence of malnutrition and associated factors among adult patients on antiretroviral therapy follow-up care in Jimma Medical Center, Southwest Ethiopia. PloS one. 2020;15(3):e0229883. doi: 10.1371/journal.pone.0229883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daniel M, Mazengia F, Birhanu D. Nutritional status and associated factors among adult HIV/AIDS clients in Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia. Science Journal of Public Health. 2013;1(1):24–31. [Google Scholar]
- 45.Fentie M, Wassie MM, Tesfahun A, Alemu K, Mequanent M, Ayele TA. Chronic energy deficiency and associated factors among adults living with HIV in Gondar University Referral Hospital northwest Ethiopia. BMC Nutrition. 2017;3(1):1–9. [Google Scholar]
- 46.Fufa H, Umeta M, Taffesse S, Mokhtar N, Aguenaou H. Nutritional and immunological status and their associations among HIV-infected adults in Addis Ababa, Ethiopia. Food and nutrition bulletin. 2009;30(3):227–32. doi: 10.1177/156482650903000303 [DOI] [PubMed] [Google Scholar]
- 47.Gebru TH, Mekonen HH, Kiros KG. Undernutrition and associated factors among adult HIV/AIDS patients receiving antiretroviral therapy in eastern zone of Tigray, Northern Ethiopia: a cross-sectional study. Archives of Public Health. 2020;78(1):1–8. doi: 10.1186/s13690-020-00486-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gedle D, Gelaw B, Muluye D, Mesele M. Prevalence of malnutrition and its associated factors among adult people living with HIV/AIDS receiving anti-retroviral therapy at Butajira Hospital, southern Ethiopia. BMC nutrition. 2015;1(1):1–11. [Google Scholar]
- 49.Girma M, Motuma A, Negasa L. 13. Assessment of Nutritional Status and Associated Factors among Adult People Living With HIV/AIDS in Hiowt Fana Specialized University Hospital, Eastern Ethiopia. Edited and Compiled by. 2017:199. [Google Scholar]
- 50.Gebremichael DY, Hadush KT, Kebede EM, Zegeye RT. Food insecurity, nutritional status, and factors associated with malnutrition among people living with HIV/AIDS attending antiretroviral therapy at public health facilities in West Shewa Zone, Central Ethiopia. BioMed research international. 2018;2018. doi: 10.1155/2018/1913534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hadgu TH, Worku W, Tetemke D, Berhe H. Undernutrition among HIV positive women in Humera hospital, Tigray, Ethiopia, 2013: antiretroviral therapy alone is not enough, cross sectional study. BMC public health. 2013;13(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hailemariam S, Bune GT, Ayele HT. Malnutrition: Prevalence and its associated factors in People living with HIV/AIDS, in Dilla University Referral Hospital. Archives of Public Health. 2013;71(1):13. doi: 10.1186/0778-7367-71-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kenea MA, Garoma S, Gemede HF. Assessment of adult nutritional status and associated factors among ART users in Nekemte referral hospital and health center, east Wollega zone, Ethiopia. Journal of Food and Nutrition Sciences. 2015;3(2):56. [Google Scholar]
- 54.Kumie G. PREVALENCE OF MALNUTRITION AND ASSOCIATED FACTR AMONG ADULT PEOPLE LIVING WITH HIV/AIDS RECEIVING ANTI-RETROVIRAL THERAPY AT ARADA SUB CITY, ADDIS ABABA, ETHIOPIA 2020. [Google Scholar]
- 55.Mitiku A, Ayele TA, Assefa M, Tariku A. Undernutrition and associated factors among adults living with Human Immune Deficiency Virus in Dembia District, northwest Ethiopia: an institution based cross-sectional study. Archives of Public Health. 2016;74(1):1–8. doi: 10.1186/s13690-016-0143-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Motuma A, Abdeta T. Undernutrition and Associated Factors Among Seropositive Adults in ART Clinic Treatment Centre, Hiwot Fana Specialized University Hospital, Eastern Ethiopia. Pathology and Laboratory Medicine. 2021;5(1):10. [Google Scholar]
- 57.Mulu H, Hamza L, Alemseged F. Prevalence of Malnutrition and Associated Factors among Hospitalized Patients with Acquired Immunodeficiency Syndrome in Jimma University Specialized Hospital, Ethiopia. Ethiop J Health Sci. 2016;26(3):217–26. doi: 10.4314/ejhs.v26i3.4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nigusso FT, Mavhandu-Mudzusi AH. High magnitude of food insecurity and malnutrition among people living with HIV/AIDS in Ethiopia: A call for integration of food and nutrition security with HIV treatment and care Programme. Nutrition and Health. 2021;27(2):141–50. doi: 10.1177/0260106020971855 [DOI] [PubMed] [Google Scholar]
- 59.Oumer B, Boti N, Hussen S, Gultie T. Prevalence Of Under nutrition And Associated Factors Among Adults Receiving First-Line Antiretroviral Treatment In Public Health Facilities Of Arba Minch Town, Southern Ethiopia. HIV/AIDS (Auckland, NZ). 2019;11:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Regassa TM, Gudeta TA. Under nutrition and Associated Factors Among Adult People Attending Highly Active Anti-Retroviral Therapy in Health Facilities of Bench Maji Zone, South West Ethiopia, 2018. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sahile AT, Ayehu SM, Fanta SF. Underweight and Its Predictors Among Patients on Anti Retroviral Therapy at Selected Health Facilities of Addis Ababa, Ethiopia, 2020. HIV/AIDS (Auckland, NZ). 2021;13:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Saliya MS, Azale T, Alamirew A, Tesfaye DJ. Assessment of nutritional status and its associated factors among people affected by human immune deficiency virus on antiretroviral therapy: A cross sectional study in Siltie zone, South Ethiopia. Healthcare in Low-resource Settings. 2021;9(1). [Google Scholar]
- 63.Shifera N, Molla A, Mesafint G, Gichew S, Matiyas R, Yosef T. Malnutrition status, and its Associated Factors among Adult HIV Positive Attending ART at Public Hospitals of Bench Sheko Zone, South West, Ethiopia, 2020. 2021. [Google Scholar]
- 64.Takele A, Engida ARA. Under nutrition and Associated Factors among Adult Individuals Receiving Highly Active Antiretroviral Therapy in Health Facilities of Nekemte Town. Eastern Ethiopia. [Google Scholar]
- 65.Teklu T, Chauhan NM, Lemessa F, Teshome G. Assessment of Prevalence of Malnutrition and Its Associated Factors among AIDS Patients from Asella, Oromia, Ethiopia. BioMed Research International. 2020;2020:7360190. doi: 10.1155/2020/7360190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Teshome MS, Gissa SB, Tefera BZ, Lema TB. Undernutrition and its predictors among people living with HIV/AIDS attending antiretroviral therapy clinic in Jimma University Specialized Hospital. International Journal of Nutrition and Metabolism. 2017;9(8):67–74. [Google Scholar]
- 67.Wasie B, Kebede Y, Yibre A. Nutritional status of adults living with HIV/AIDS at the University of Gondar Referral Hospital, Northwest Ethiopia. Ethiopian Journal of Health and Biomedical Sciences. 2010;3(I):3–14. [Google Scholar]
- 68.Wasihun Y, Yayehrad M, Dagne S, Menber Y, Awoke T, Nega G. Prevalence of Undernutrition and Associated Factors among Adult People Living with HIV/AIDS and on ART in Achefer District, North West Ethiopia: Cross-Sectional study. 2020. [Google Scholar]
- 69.Yitbarek GY, Engidaw MT, Ayele BA, Tiruneh SA, Alamir MT. Magnitude of obesity/overweight and its associated factors among HIV/AIDS patients on antiretroviral therapy in Jimma Zone Hospitals, South West Ethiopia: hospital-based cross-sectional study. Diabetes, metabolic syndrome and obesity: targets and therapy. 2020;13:1251. doi: 10.2147/DMSO.S247221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zemede Z, Tariku B, Kote M, Estifanos W. Undernutrition and associated factors among HIV-positive adult patients enrolled in antiretroviral therapy (ART) clinics in the Arba Minch area, southern Ethiopia. HIV/AIDS (Auckland, NZ). 2019;11:147. doi: 10.2147/HIV.S200120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saito A, Karama M, Kamiya Y. HIV infection, and overweight and hypertension: a cross-sectional study of HIV-infected adults in Western Kenya. Tropical medicine and health. 2020;48(1):1–12. doi: 10.1186/s41182-020-00215-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nnyepi M. The risk of developing malnutrition in people living with HIV/AIDS: Observations from six support groups in Botswana. South African Journal of Clinical Nutrition. 2009;22(2):89–93. doi: 10.1080/16070658.2009.11734224 [DOI] [Google Scholar]
- 73.Nanewortor BM, Saah FI, Appiah PK, Amu H, Kissah-Korsah K. Nutritional status and associated factors among people living with HIV/AIDS in Ghana: cross-sectional study of highly active antiretroviral therapy clients. BMC nutrition. 2021;7(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Akilimali P, Musumari P, Kashala-Abotnes E, Tugirimana P, Mutombo P. Food insecurity and undernutrition in treated HIV patients a (post-) conflict setting: A cross sectional study from Goma, Eastern Democratic Republic of Congo. J Nutrition Health Food Sci. 2016;4(2):1–9. [Google Scholar]
- 75.Benzekri NA, Sambou J, Diaw B, Sall EHI, Sall F, Niang A, et al. High prevalence of severe food insecurity and malnutrition among HIV-infected adults in Senegal, West Africa. PloS one. 2015;10(11):e0141819. doi: 10.1371/journal.pone.0141819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Odwee A, Kasozi KI, Acup CA, Kyamanywa P, Ssebuufu R, Obura R, et al. Malnutrition amongst HIV adult patients in selected hospitals of Bushenyi district in southwestern Uganda. African Health Sciences. 2020;20(1):122–31. doi: 10.4314/ahs.v20i1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Takarinda KC, Mutasa-Apollo T, Madzima B, Nkomo B, Chigumira A, Banda M, et al. Malnutrition status and associated factors among HIV-positive patients enrolled in ART clinics in Zimbabwe. BMC Nutrition. 2017;3(1):15. doi: 10.1186/s40795-017-0132-8 [DOI] [Google Scholar]
- 78.Mahlangu K M P, Madiba S The nutritional status of adult antiretroviral therapy recipients with a recent HIV diagnosis; a cross-sectional study in primary health facilities in Gauteng, South Africa. InHealthcare. 2020. 8(3):290. doi: 10.3390/healthcare8030290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Naidoo K, Yende-Zuma N, Augustine S. A retrospective cohort study of body mass index and survival in HIV infected patients with and without TB co-infection. Infectious diseases of poverty. 2018;7(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kabalimu TK, Sungwa E, Lwabukuna WC. Malnutrition and associated factors among adults starting on antiretroviral therapy at PASADA Hospital in Temeke District, Tanzania. Tanzania Journal of Health Research. 2018;20(2). [Google Scholar]
- 81.Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Medical Research Methodology. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10(10.1002):14651858. doi: 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tekelehaimanot AN, Lemma TB, Gudina EK, Getnet M, Amdisa D, Dadi LS. Predictors of Under Nutrition and Its Implication toward HIV Continuum Care among Adult People Living with HIV in Jimma Zone Public Hospitals, Southwest Ethiopia: A Mixed Method Study. Journal of the International Association of Providers of AIDS Care (JIAPAC). 2020;19:2325958220976254. doi: 10.1177/2325958220976254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Organization WH. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. 2019. [Google Scholar]
- 85.Alebel A, Demant D, Petrucka P, Sibbritt D. Effects of undernutrition on opportunistic infections among adults living with HIV on ART in Northwest Ethiopia: Using inverse-probability weighting. PLOS ONE. 2022;17(3):e0264843. doi: 10.1371/journal.pone.0264843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tesfa Mengie D D, Temesgen Muche, Lemma Getacher Under Nutrition and Its Determinants Among Adults Receiving Antiretroviral Therapy in Ethiopia: A Systematic Review and Meta-analysis. International Journal of Homeopathy & Natural Medicines. 2021;7(1):1–6. doi: 10.11648/j.ijhnm.20210701.11 [DOI] [Google Scholar]