Abstract
Background:
Total knee arthroplasty (TKA) is a common orthopedic procedure, following which many patients benefit from physical therapy (PT). However, such services may not be uniformly accessible and utilized. To that end, disparities in access to care such as PT following interventions may be a factor for those of varying race/ethnicities.
Methods:
TKAs were abstracted from the 2014 to 2016 Standard Analytic Files (SAF) PearlDiver dataset – a large national health administrative dataset containing information on over 60 million Medicare patients. Occurrences of home or outpatient PT within 90 days following TKA were identified. Patient demographic factors were extracted, including age, sex, Elixhauser Comorbidity Index (ECI), estimated average household income of patient based on zip code (low average household income [<75k/year], high average household income [>75k/year]), and patient race/ethnicity (White, Hispanic, Asian, Native American, Black, Other). Predictive factors for PT utilization were determined and compared with univariate and multivariate analyses.
Results:
Of 23,953 TKA patients identified, PT within 90 days following TKA was utilized by 18,837 (78.8%). Patients self-identified as White (21,824 [91.1%]), Black (1,250 [5.2%]), Hispanic (268 [1.1%]), Asian (241 [1.0%]), Native American (90 [0.4%]), or “other” (280 [1.2%]) and were of low household income (19,957 [83.3%]) or high household income (3,994 [16.7%]). When controlling for age, sex, and ECI, PT was less likely to be received by those of low household income (relative to high household income OR 0.79) or by those of defined race/ethnicity (relative to White, Black OR 0.81, Native American OR 0.58, Asian OR 0.50, or Hispanic OR 0.44) (p<0.05 for each).
Conclusions:
In a large Medicare dataset, disparities in utilization of PT following TKA were identified based on patient estimated household income and race/ethnicity. Identification of such factors may help facilitate the expansion of care to meet the needs of all groups adequately.
Keywords: Knee, Total knee replacement, Race, Ethnicity, Disparities, Physical Therapy
Introduction
Total Knee Arthroplasty (TKA) is a commonly performed orthopedic procedure. Postoperatively, mobilization, strengthening, and range-of-motion are areas of focus to facilitate full recovery – all of which can be bolstered by rehabilitative care/ physical therapy (PT)1. In fact, patients who participate in a structured exercise program coupled with manual therapy have been shown to benefit in terms of function, satisfaction, and pain relief following TKA2. Despite the benefits associated with PT following TKA, such services may not be uniformly accessible and utilized. 1
Racial disparities have been studied in regard to several aspects of care related to total joint arthroplasty. In terms of those who undergo such surgeries, several studies have reported that members of differing race/ethnicity groups – particularly Hispanics and Black patients – are less likely to receive total joint arthroplasty of the lower extremities when compared with Whites3–7. In terms of perioperative adverse events, similar disparities exist, with several studies reporting worse functional outcomes and higher rates of postoperative complications in Hispanic and Black total joint arthroplasty patients when compared with White patients3–7.
Limited studies have analyzed disparities in PT utilization following surgery. Postoperative PT could influence patient outcomes and thereby warrants exploration of potential disparities in utilization. Self-reported survey results have revealed barriers in accessibility to and rigor of rehabilitative care following TKA among African American patients compared to White patients8, 9. In contrast, other studies evaluating racial disparities in rehabilitation following TKA reported no significant difference in utilization among the groups analyzed10. That study, however, was limited to a population of post-menopausal women who self-identified as White or non-Hispanic Black and underwent TKA between 2006-201310. As such, there continues to be gaps in the present understanding of disparities in PT use in this population – particularly regarding race/ethnicity groups other than Whites and Blacks and patient socioeconomic status10.
In light of the above-noted gaps in the literature, the current study aims to elucidate racial/ethnic and patient-income related disparities in PT utilization following TKA using a large national health administrative database including data on patients who self-identify as White, Black, Native American, Hispanic, Asian, or “Other” race. Prior work including such databases are growing and provide reliable information on large, detailed patient populations11–14.
Methods:
Database and cohort:
Data for the current retrospective cohort study was obtained from the 2014 to 2016 PearlDiver Standard Analytic Files (SAF) dataset – a large national Medicare claims dataset containing information on over 60 million unique patients. PearlDiver data is de-identified and aggregate and therefore Health Insurance Portability and Accountability Act (HIPAA) compliant. Given this, our Institutional Review Board (IRB) determined studies employing this dataset exemption from review.
Using Current Procedural Terminology (CPT) and International Classification of Disease (ICD) codes, patients with a diagnosis of knee osteoarthritis who underwent total knee arthroplasty (TKA) were identified. Exclusion criteria included surgical indication of trauma/neoplasm/infection (based on ICD codes), patients without race/ethnicity data in the dataset, and any patients under age 65.
CPT codes were then used to identify which of these patients received outpatient physical therapy (PT) within 90 days of TKA. The cohort was subsequently divided into those who did and did not undergo PT within 90 days of surgery. Several patient characteristics were extracted from the dataset and tabulated: age, sex, and Elixhauser Comorbidity Index (ECI – an estimate of patient comorbidity burden based on ICD diagnosis codes).
Additionally, race/ethnicity was identified as a variable, including White, Black, Native American, Asian, Hispanic, and “Other” subgroups. Finally, average patient household income was estimated based on zip code of residence (low average household income [<75k/year], high average household income [>75k/year]).
Data Analysis:
The proportion of patients within each characteristic variable was defined, as well as those that did and did not receive PT in the 90 days following TKA. Univariate analyses were then used to compare characteristics of those who did and did not receive PT following TKA. Differences in patient sex, race/ethnicity, and income (high income vs. low income) were compared using Pearson’s chi-squared test. Average patient age and ECI were compared between the two groups using Welch’s T-test.
Controlling for patient age, sex, and ECI, multivariate logistic regression analysis was then used to determine whether race/ethnicity and/or patient household income (based on zip code) were independently associated with odds of PT utilization following TKA. Odds ratios (OR+/− 95% Confidence Intervals) were calculated for race/ethnicity and income subcategories compared to referent subcategories (White race/ethnicity and high income [>75k/year], respectively).
All statistical analysis was conducted within the PearlDiver system, using p<0.05 as the threshold for statistical significance. Prim9 (GraphPad Softwares, San Diego, CA) and Microsoft Excel (Microsoft Corporation, Redmond, WA) were used to generate figures.
RESULTS
Study cohort demographics
A total of 34,633 TKA patients meeting criteria for the present study were identified. Of this population, 10,680 (30.8%) patients were excluded due to lack of race/ethnicity information regarding these individuals in the SAF database. Supplementary table 1 depicts the demographics of patients excluded due to lack of race/ethnicity data compared to those included. As such, the final study cohort contained 23,953 TKA patients, of which 18,837 (78.8%) received PT within 90-days of surgery.
The race/ethnicity breakdown of the study cohort population is depicted in Figure 1. Of the 23,953 TKA patients identified, patients were identified as White for 21,824 (91.1%) or non-White for the remaining 2,129 (8.9%). Among patients who identified as non-White, patients were identified as Black for 1,250 (5.2% of the total study cohort), Hispanic for 268 (1.1%), Native American for 90 (0.4%), Asian for 241 (1.0%), and “Other” for 280 (1.2%).
Figure 1.
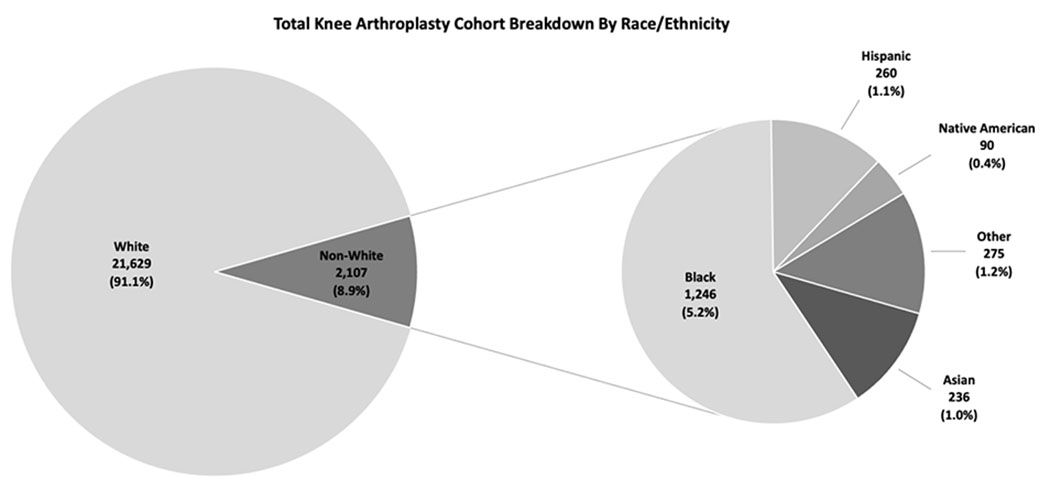
Race/ethnicity breakdown of TKA cohort. All percentages are relative to total study population.
The percent of patients within each race/ethnicity group who underwent physical therapy in the 90-days following TKA is shown in Figure 2. Percents receiving PT following surgery were as follows: White 79.3%, Black 74.6%, Native American 72.2%, Asian 66.4%, Hispanic 63.1%, and “Other” 75.7%. Apart from those who identified as “Other,” a significantly lower proportion of Black, Native American, Asian, and Hispanic patients received PT following TKA when compared to White patients (p<0.0001).
Figure 2.
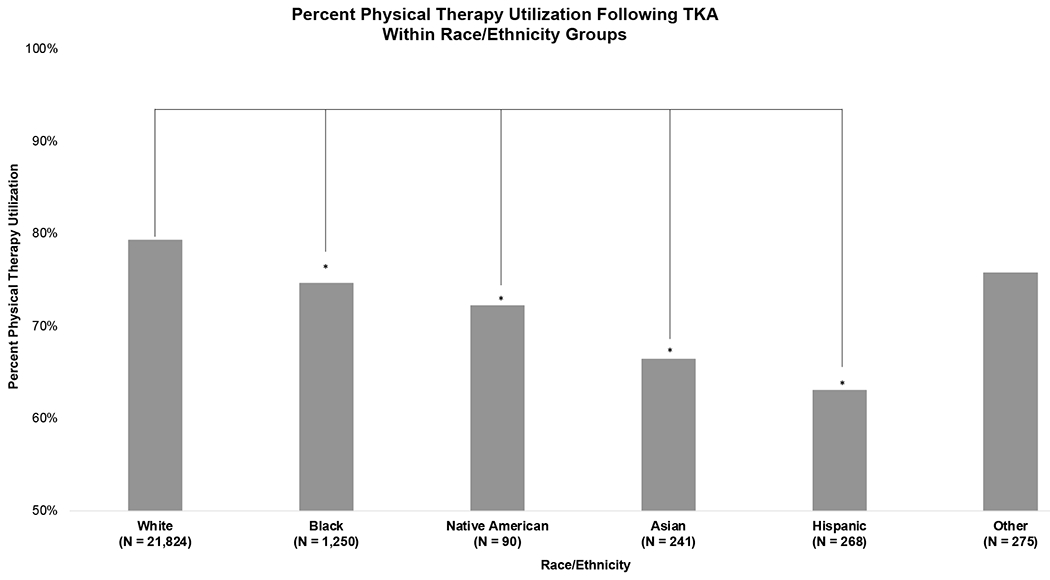
Percent of patients in each respective race/ethnicity group who received physical therapy in the 90 days following TKA. Astrixes represent statistical significance (p<0.05), with each race/ethnicity group being compared to White race/ethnicity. N values represent total number of patients in each race/ethnicity group
Factors associated with PT utilization following TKA
Demographics of the entire study TKA population are shown in Table 1. The largest proportion of patients were aged 65-69 (35.9%), with steadily fewer patients in each subsequent older age group. The cohort was female predominant (63.9%) and highly comorbid with an average ± standard deviation ECI of 6.78 ± 4.17. Race/ethnicity data is as defined in the above section. Most patients fell within the low average annual household income category (83.3%).
Table 1.
Univariate Analysis of characteristics of patients with Total Knee Arthroplasty
| Total | PT | No PT | p-value | |
|---|---|---|---|---|
|
| ||||
| N | 23,953 (100%) | 18,837 (78.8%) | 5,114 (21.2%) | |
|
| ||||
| Age | ||||
| 65-69 | 8,602 (35.9%) | 6,387 (33.9%) | 1,425 (27.9%) | <0.0001 |
| 70-74 | 6,989 (29.2%) | 5,758 (30.6%) | 1,304 (25.5%) | |
| 75-79 | 4,854 (20.3%) | 3,957 (21%) | 1,192 (23.3%) | |
| 80-84 | 2,537 (10.6%) | 2,018 (10.7%) | 747 (14.6%) | |
| 85+ | 971 (4.1%) | 717 (3.8%) | 446 (8.7%) | |
|
| ||||
| Sex | ||||
| Female | 15,296 (63.9%) | 11,918 (63.3%) | 3,377 (66%) | 0.0003 |
| Male | 8,657 (36.1%) | 6,919 (36.7%) | 1,737 (34%) | |
|
| ||||
| ECI (mean ± st dev) | 6.78 ± 4.17 | 6.81 ± 4.04 | 7.81 ± 4.60 | |
| 0-3 | 5,818 (24.3%) | 4,295 (22.8%) | 963 (18.8%) | <0.0001 |
| 4-7 | 9,015 (37.6%) | 7,394 (39.3%) | 1,681 (32.9%) | |
| 8-11 | 5,755 (24%) | 4,624 (24.5%) | 1,360 (26.6%) | |
| 12+ | 3,365 (14%) | 2,524 (13.4%) | 1,110 (21.7%) | |
|
| ||||
| Race/Ethnicity | ||||
| White | 21,824 (91.1%) | 17,298 (91.8%) | 4,524 (88.5%) | <0.0001 |
| Other | 280 (1.2%) | 212 (1.1%) | 57 (1.1%) | |
| Black | 1,250 (5.2%) | 933 (5%) | 319 (6.2%) | |
| Native American | 90 (0.4%) | 65 (0.3%) | 65 (1.3%) | |
| Asian | 241 (1%) | 160 (0.8%) | 82 (1.6%) | |
| Hispanic | 268 (1.1%) | 169 (0.9%) | 104 (2%) | |
|
| ||||
| Income (based on zip code) | ||||
| High Income (>75k/year) | 3,994 (16.7%) | 3,243 (17.2%) | 751 (14.7%) | <0.0001 |
| Low Income (<75k/year) | 19,957 (83.3%) | 15,594 (82.8%) | 4,363 (85.3%) | |
Those who did and did not receive PT in the 90 days following TKA are also shown in Table 1. On univariate analysis, all demographic factors examined were significantly correlated with patients undergoing PT in the 90 days following TKA (p = 0.0003 for sex; p<0.0001 for age, ECI, race/ethnicity, and average household income).
Race/ethnicity and income (based on zip code) variables independently predictive of receiving PT in the 90 days following TKA, controlling for the other patient factors, were then assessed, and results are presented in Table 2 and Figure 3. In terms of race/ethnicity, relative to White patients, differences in receiving PT within 90-days of TKA were identified for those who identified as Black (Odds Ratio [95% CI] 0.81 [0.71, 0.93]), Native American (0.58 [0.37, 0.94]), Asian (0.50 [0.38, 0.67]), or Hispanic (0.44 [0.34, 0.57]). Additionally, compared to patients with high average annual household income (>75k/year), patients in the low average annual household income group (<75k/year) had significantly lower odds of receiving PT in the 90 days following TKA (0.79 [0.73, 0.86]).
Table 2.
Multivariate analysis of predictive factors for PT
| N = 23,953 | OR (95% CI) | p-value |
|---|---|---|
|
| ||
| Race/Ethnicity | ||
| White (referent) | ||
| Other | 0.92 (0.69, 1.24) | 0.5717 |
| Black | 0.81 (0.71, 0.93) | 0.0026 |
| Native American | 0.58 (0.37, 0.94) | 0.0215 |
| Asian | 0.50 (0.38, 0.67) | <0.0001 |
| Hispanic | 0.44 (0.34, 0.57) | <0.0001 |
|
| ||
| Income (based on zip code) | ||
| Income >75k/year (referent) | ||
| Income <75k/year | 0.79 (0.73, 0.86) | <0.0001 |
Multivariate analysis controlling for patient age, sex, and Elixhauser Comorbidity Index (ECI)
Figure 3.
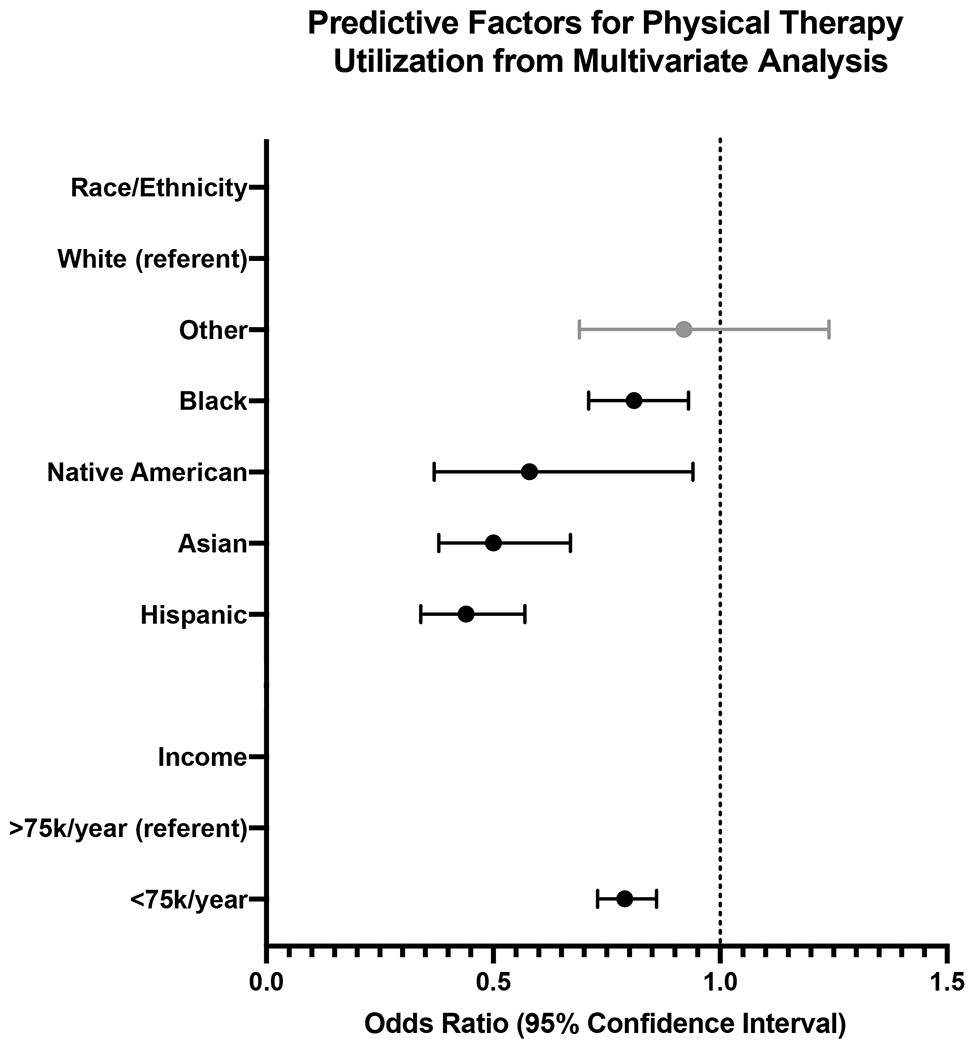
Forest plot depicting results of multivariate analysis for independent predictors of physical therapy utilization following TKA among race/ethnicity and average household income groups. Black bars represent statistically significant (P<0.05) difference in odds of receiving PT following TKA compared to referent category.
DISCUSSION:
While PT is frequently utilized following THA, such services may not be uniformly accessible and utilized. Data from the present study suggest that specific race/ethnicities and household income groups have differing likelihoods of PT utilization in this setting and disparities in care.
Despite the importance of PT in effective rehabilitation, of the 23,953 TKA patients in the current study, postoperative PT was utilized by 18,837 (78.8%). Past literature has reported relatively similar levels of PT utilization following TKA. One small study composed of 29 Black and 75 White patients reported that approximately 85% of patients utilized outpatient PT following TKA15. A review study including five works on outpatient PT use following TKA reported a broad range of utilization – ranging from 16.7-84.5%16. The authors note that this range could be – in part – due to large variations in follow-up periods following hospital discharge and differing definitions in PT reporting16. Such broad discrepancies in PT utilization following TKA could be due to a lack of national guidance on the subject. Regardless, the overall rate of PT utilization in the present study is within the realm of past studies.
The race/ethnicity breakdown of the study cohort was then assessed. In the present study, 91.1% of TKA patients self-identifying as White, 5.2% Black, 1.1% Hispanic, 1.0% Asian, 0.4% Native American, and 1.2% as “Other.” A large national retrospective cohort study examining nearly 550,000 TKAs performed from 2001-2008 reported a racial breakdown of 87.24% White, 5.88% Black, 4.20% Hispanic, 0.46% Asian, 0.51% Native American, and 1.71% Mixed Race17. Given this, the racial distribution of TKA utilization in the present study is relatively in-line with past literature. Based on this evidence, most TKA patients self-identify as White, with TKA utilization among other racial/ethnic groups generally smaller than their overall proportion of the US population18. As such, racial disparities in TKA utilization likely persist – a position reiterated by several studies19, 20. With the rapid growth of some minority populations in the US – addressing such disparities is essential to maintain high-quality and equitable care.
When evaluating PT utilization concerning race/ethnicity demographic breakdowns – controlling for age, sex, and ECI – minority patients were significantly less likely than White patients to receive PT after TKA. Asian and Hispanic populations had the most significant discrepancies, being approximately half as likely as their White counterparts to receive PT after TKA. Similarly, previous studies21 have shown that minorities, particularly Hispanic patients, are significantly less likely to seek PT utilization or receive PT/OT referrals in various circumstances such as following hospitalization for COVID1922, musculoskeletal conditions23, and following osteoarthritis diagnosis24.
Several potential barriers may contribute to inequities in access to or utilization of PT post-TKA. These include, but are not limited to, language barrier22, socioeconomic factors, and cultural differences19, 20, 6. For instance, attending outpatient PT settings may be time-consuming and therefore more difficult for patients who cannot take time off work due to financial constraints. Additionally, cultural differences in at-home support networks may influence the utilization of outpatient PT services following TKA. Importantly, implicit referral bias must be considered as a potential reason underlying disparities in accessibility and availability of receiving PT following TKA.
The present study also showed that higher-income patients are more likely to receive PT post-TKA. Controlling for age, sex, and ECI, patients with an estimated average household income of greater than $75,000 were significantly more likely to receive PT after TKA compared to those with an average household income of less than $75,000. This data aligns with several other studies indicating utilization of PT to correspond with increasing income/socioeconomic status and again highlights the disparities in care available to certain marginalized groups25–27.
The present study has several strengths. For one, the dataset analyzed allowed for characterization of PT utilization following TKA in nearly 24,000 Medicare patients across all sites of care in the United States. Access to such a large national patient population suggests high generalizability of the present studies’ findings. Furthermore, this study characterized the influence of race on postoperative PT utilization when controlling for patient factors including age, sex, comorbidity burden, and family income. As such, these results highlight the unique impact race may have on PT following TKA. The present study does have several limitations. With any study that makes use of administrative data, it is reliant and thus limited to the accuracy of the administrate data that was coded. Additionally, we did not have race and ethnicity data for all TKA patients identified in the database, creating the potential for non-response bias. Lastly, there may have been other forms of physical rehabilitation (i.e., inpatient PT) that were not included within our study and may account for the seemingly decreased frequency of PT utilization with increasing age.
Overall, significant differences in PT utilization post-TKA were identified based on race/ethnicity groups and income groups, suggesting that disparities might play a role in both access to therapy and the quality of rehabilitation in this population. Future studies should identify specific barriers to PT access among different race/ethnicity groups, such as bias, inadequate access to care, and other factors. Additionally, future works should characterize the impact racial disparities in PT utilization following TKA may have on patient outcomes and satisfaction. With physical rehabilitation often playing an important role in the recovery process in TKA patients, a better understanding of which groups are at greatest risk of not receiving equitable rehabilitation following surgery can inform both surgeons and administrative level initiatives to note and address potential barriers to care.
Supplementary Material
Funding:
Funding for this project was provided by National Heart, Lung, and Blood Institute of the National Institute of Health (NIH) grant 2T35HL007649-36.
Footnotes
Disclosures:
Dr. Jonathan Grauer serves as Editor-in-Chief of the North American Spine Society Journal (NASSJ).
Conflict of Interest: No conflicts of interest to report.
Level of Evidence: Level III
Bibliography
- 1.Mistry JB, Elmallah RD, Bhave A, et al. Rehabilitative Guidelines after Total Knee Arthroplasty: A Review. J Knee Surg 2016;29:201–217. [DOI] [PubMed] [Google Scholar]
- 2.Karaborklu Argut S, Celik D, Kilicoglu OI: The Combination of Exercise and Manual Therapy Versus Exercise Alone in Total Knee Arthroplasty Rehabilitation: A Randomized Controlled Clinical Trial. Pm r 2021;13:1069–1078. [DOI] [PubMed] [Google Scholar]
- 3.Pierce TP, Elmallah RK, Lavernia CJ, et al. Racial Disparities in Lower Extremity Arthroplasty Outcomes and Use. Orthopedics 2015;38:e1139–1146. [DOI] [PubMed] [Google Scholar]
- 4.Reyes AM, Katz JN: Racial/Ethnic and Socioeconomic Disparities in Osteoarthritis Management. Rheum Dis Clin North Am 2021;47:21–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chun DS, Leonard AK, Enchill Z, Suleiman LI: Racial Disparities in Total Joint Arthroplasty. Curr Rev Musculoskelet Med 2021;14:434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amen TB, Varady NH, Rajaee S, Chen AF: Persistent Racial Disparities in Utilization Rates and Perioperative Metrics in Total Joint Arthroplasty in the U.S.: A Comprehensive Analysis of Trends from 2006 to 2015. J Bone Joint Surg Am 2020;102:811–820. [DOI] [PubMed] [Google Scholar]
- 7.Dharmasukrit C, Chan SYS, Applegate RL 2nd, Tancredi DJ, Harvath TA, Joseph JG: Frailty, Race/Ethnicity, Functional Status, and Adverse Outcomes After Total Hip/Knee Arthroplasty: A Moderation Analysis. J Arthroplasty 2021;36:1895–1903. [DOI] [PubMed] [Google Scholar]
- 8.Bove AM, Dong E, Hausmann LRM, et al. Exploring Race Differences in Satisfaction With Rehabilitation Following Total Knee Arthroplasty: A Qualitative Study. J Gerontol A Biol Sci Med Sci 2022;77:e48–e55. [DOI] [PubMed] [Google Scholar]
- 9.Cavanaugh AM, Rauh MJ: Does Patient Race Affect Physical Therapy Treatment Recommendations? J Racial Ethn Health Disparities 2021;8:1377–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavanaugh AM, Rauh MJ, Thompson CA, et al. Rehabilitation After Total Knee Arthroplasty: Do Racial Disparities Exist? J Arthroplasty 2020;35:683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kammien AJ, Zhu JR, Gouzoulis MJ, et al. Emergency Department Visits Within 90 Days of Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med 2022;10:23259671221083586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gouzoulis MJ, Kammien AJ, Zhu JR, Gillinov SM, Moore HG, Grauer JN: Single-level posterior lumbar fusions in patients with Ehlers Danlos Syndrome not found to be associated with increased postoperative adverse events or five-year reoperations. N Am Spine Soc J 2022;11:100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joo PY, Jayaram RH, McLaughlin WM, et al. Four-level anterior versus posterior cervical fusions: Perioperative outcomes and five-year reoperation rates: Outcomes after four-level anterior versus posterior cervical procedures. N Am Spine Soc J 2022;10:100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sabatino MJ, Burroughs PJ, Moore HG, Grauer JN: Spine coding transition from ICD-9 to ICD-10: Not taking advantage of the specificity of a more granular system. N Am Spine Soc J 2020;4:100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bove AM, Hausmann LRM, Piva SR, Brach JS, Lewis A, Fitzgerald GK: Race Differences in Postacute Physical Therapy Utilization and Patient-Reported Function After Total Knee Arthroplasty. Arthritis Care Res (Hoboken) 2022;74:79–88. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs H, Seeber GH, Allers K, Hoffmann F: Utilisation of outpatient physiotherapy in patients following total knee arthroplasty - a systematic review. BMC Musculoskelet Disord 2021;22:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W, Lyman S, Boutin-Foster C, et al. Racial and Ethnic Disparities in Utilization Rate, Hospital Volume, and Perioperative Outcomes After Total Knee Arthroplasty. JBJS 2016;98:1243–1252. [DOI] [PubMed] [Google Scholar]
- 18.Bureau TUSC: QuickFacts United States, in Census (ed), 2022. [Google Scholar]
- 19.Irgit K, Nelson CL: Defining racial and ethnic disparities in THA and TKA. Clin Orthop Relat Res 2011;469:1817–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavanaugh AM, Rauh MJ, Thompson CA, et al. Racial and ethnic disparities in utilization of total knee arthroplasty among older women. Osteoarthritis Cartilage 2019;27:1746–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braaten AD, Hanebuth C, McPherson H, et al. Social determinants of health are associated with physical therapy use: a systematic review. British Journal of Sports Medicine 2021;55:1293. [DOI] [PubMed] [Google Scholar]
- 22.Jolley S, Nordon-Craft A, Wilson MP, et al. Disparities in the allocation of inpatient physical and occupational therapy services for patients with COVID-19. J Hosp Med 2022;17:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter SK, Rizzo JA: Use of Outpatient Physical Therapy Services by People With Musculoskeletal Conditions. Physical Therapy 2007;87:497–512. [DOI] [PubMed] [Google Scholar]
- 24.Cisternas MG, Yelin E, Katz JN, Solomon DH, Wright EA, Losina E: Ambulatory visit utilization in a national, population-based sample of adults with osteoarthritis. Arthritis Rheum 2009;61:1694–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freburger JK, Li D, Johnson AM, Fraher EP: Physical and Occupational Therapy From the Acute to Community Setting After Stroke: Predictors of Use, Continuity of Care, and Timeliness of Care. Arch Phys Med Rehabil 2018;99:1077–1089.e1077. [DOI] [PubMed] [Google Scholar]
- 26.Chan L, Wang H, Terdiman J, et al. Disparities in Outpatient and Home Health Service Utilization Following Stroke: Results of a 9-Year Cohort Study in Northern California. PM&R 2009;1:997–1003. [DOI] [PubMed] [Google Scholar]
- 27.Chevan J, Riddle DL: Factors Associated With Care Seeking From Physicians, Physical Therapists, or Chiropractors by Persons With Spinal Pain: A Population-Based Study. Journal of Orthopaedic & Sports Physical Therapy 2011;41:467–476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


