Abstract
Background:
Little is known about the recovery experiences of older trauma intensive care unit (TICU) survivors and the relationship between geriatric trauma care and long-term functional ability and health-related quality of life (HRQOL).
Methods:
We conducted a prospective cohort study of 218 patients (age ≥ 65 years) admitted to a Level 1 regional trauma center TICU before versus after implementation of a geriatric care bundle with protocolized geriatrics consultations (Geri-T). Survivors or their proxies were interviewed approximately 1-year after hospitalization. Outcomes included the Katz Index of Independence in Activities of Daily Living (ADLs), Lawton Instrumental Activities of Daily Living (IADLs), and EQ-5D-5L HRQOL survey. Two investigator-developed questions regarding recovery experiences were included. Differences in outcomes among survivors admitted before versus after Geri-T were analyzed using multivariable linear regression. Responses to questions about recovery experiences were qualitatively assessed using content analysis.
Results:
We reached 67% (146/218) of hospital survivors or their proxies across both groups; 126 patients were still alive and completed the survey. Mean age was 76 (SD 8), 36% were female, and 90% were independent with ADLs pre-injury. At follow-up, independence with ADLs was 76% and IADLs was 63%. The mean EQ-5D-5L index score was 0.78 (SD 0.18). Most patients (65%) reported having not returned to pre-injury functional status. Neither functional ability or HRQOL differed significantly among patients admitted before versus after Geri-T. Content analysis of open-ended questions revealed themes of activity limitations, persistent pain, and cognitive dysfunction.
Conclusions:
Nearly one-fifth of TICU survivors experienced loss of ADL function one year after injury, and most reported having not returned to pre-injury functional status. Nonetheless, patient-reported HRQOL was comparable to age-adjusted norms. Geri-T was not associated with differences in HRQOL or functional ability. Survivors reported persistent difficulty with activities beyond those of daily living, pain, and cognition.
Level of evidence:
Level III, prognostic/epidemiologic
Keywords: geriatrics, trauma, critical care, survivorship
Media summary:
Most older TICU survivors were independent with ADLs and IADLS at 1-year, but 65% didn’t return to pre-injury baseline, with persistent activity limitations, pain, and cognitive problems.
Hashtags:
#Trauma #OlderAdults #LongTermOutcomes
Background
Traumatic injury is a leading cause of morbidity and mortality among a growing population of older adults in the United States (U.S.) (1). Prior studies have estimated that 85–90% of seriously injured older adults survive to hospital discharge, and improvements in short-term survival have been demonstrated over time (2,3). However, less is known about long-term outcomes among older survivors of serious injury. Data have shown long-term mortality among trauma survivors at 1- and 3-years is significantly higher than age-adjusted population norms (2,4–6), yet only a handful of studies have evaluated long-term outcomes in functional status. Findings from these studies have demonstrated declines in activities of daily living (ADLs) among survivors that persist 1-year after injury (7,8). In conjunction with ADLs, instrumental activities of daily living (IADLs), health-related quality of life (HRQOL) and perceptions of recovery among patients and their families are meaningful targets for trauma quality improvement and require further investigation (9).
With the goal of improving outcomes for injured older adults, some trauma centers have implemented pathways of care tailored to the needs of older patients admitted for serious injury, with protocolized geriatrics consultation as a central component (10–13). These care pathways have been shown to be associated with improvement in short-term outcomes including delirium (10) and 30-day readmission rates (11). One prior study demonstrated an association between routine geriatrics consultation for older trauma patients and a lower likelihood of loss of ADL function one-year after hospitalization (13), however findings from this single-center study have not been replicated, and few prior studies to our knowledge have evaluated for associations between inpatient geriatrics consultation and long-term IADL function and HRQOL among older survivors of severe traumatic injury.
In 2017, a quality improvement initiative called Geri-T was implemented to standardize trauma care for injured older adults admitted to the trauma intensive care unit (TICU) at a Level I regional trauma center. Recognizing that older patients with frailty are at higher risk of disability and poor HRQOL (14–16), frailty screening was implemented as part of Geri-T using the Clinical Frailty Scale (CFS) (17), and was found to be associated with increased geriatric-centered multi-disciplinary trauma care, a lower prevalence of delirium, and greater use of opioid-sparing pain management strategies. In this study, we sought to (1) describe functional ability, HRQOL, and perceptions of post-injury recovery one-year after hospital discharge among older survivors of serious injury or their proxies; and (2) evaluate for associations between increased multidisciplinary trauma care as a result of Geri-T implementation and improved long-term functional ability and HRQOL.
Methods
Design
This was a prospective cohort study of long-term functional ability, HRQOL, and perceptions of recovery among severely injured older adults. Associations between Geri-T implementation and long-term outcomes of interest were evaluated using a quasi-experimental before-and-after study design. This project received Institutional Review Board approval on June 25, 2017 (#130992). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (SDC Table 1).
The Geri-T Care Bundle Quality Improvement Project
In brief, the Geri-T care bundle was designed as a quality improvement project and was initiated in October of 2017 at a county hospital and Level I regional trauma center. The goal of the care bundle was to standardize care practices for injured older patients admitted to the TICU. As part of the bundle, the CFS was administered to patients or their proxies by trained nursing staff at admission. Patients with mild or moderate frailty (CFS score of 4–6) were recommended to receive geriatrics consultation, and those with severe frailty (CFS score of 7–9) were recommended to receive specialty palliative care consultation. Frailty was used to identify patients at risk of poor long-term outcomes, as it has been consistently shown to be predictive of long-term disability among older survivors of critical illness and serious injury.(18–21) While no one specific frailty screening tool has been demonstrated to be superior to others in acute care trauma populations, we chose the CFS as it has demonstrated feasibility and high reliability among older trauma patients, and is simple and brief.(22–24) Prior to Geri-T implementation, about 5% of older TICU patients received a comprehensive geriatrics assessment (CGA) through geriatrics consultation; after implementation about half (52%) of older TICU patients received a CGA through geriatrics consultation. The proportion receiving palliative care consultation did not change significantly.
Sample and Setting
The study took place at a single urban county hospital and Level I regional trauma center. Patients were eligible to receive a follow-up call one year after hospital discharge if they were 65 years or older at time of hospital admission, admitted to the TICU for traumatic injury between July 1 and September 30 in 2017 (unexposed to the Geri-T bundle) or 2018 (exposed to the Geri-T bundle), and survived hospitalization. Patients admitted in identical months of the year in 2017 and 2018 were chosen given known seasonal variation in the incidence of traumatic injury and relative proportions of different injury mechanisms, as well as an assumption that clinical practice changes as a result of Geri-T implementation were likely to have a ramp-up period and take place over a timeframe of months. All patients matching eligibility criteria were included in the study.
Procedures
Patients or their proxies were invited to participate in a follow-up survey via telephone approximately one year after hospital discharge. The survey included validated measurements of functional status and HRQOL as well as two questions regarding the recovery process (described in detail below). Study coordinators called the primary contact telephone number listed in the patient’s medical record. If no one answered the telephone at the time of initial call, two additional attempts were made at different times of day taking into account findings from prior studies regarding optimal call patterns for telephone surveys and unique considerations in reaching older adults (25,26). Telephone surveys were administered by one of two trained study coordinators. Survey responses were recorded in RedCap. Telephone calls were not audio-recorded. Proxy respondents were permitted to complete the survey either at the patient’s request or if the proxy stated that the patient would be unable to participate and reported having current knowledge of the patient’s health and functional status. Response rates were calculated based on the proportion of the living sample who completed the follow-up survey.
Outcomes
Primary outcomes of interest were one-year HRQOL and functional ability with ADLs and IADLs. HRQOL was measured using the EQ-5D-5L survey (27). The survey is comprised of questions regarding five health dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has five response-levels of severity: no problems, slight problems, moderate problems, severe problems, and extreme problems or inability to perform the activity. The descriptive system profile can be linked to a summary health state index score, allowing for comparisons to age-adjusted national population norms (28).
Functional ability was measured at time of follow-up using the Katz Index of Independence in ADLs and the Lawton IADL Scale. The Katz Index sums a rating of independence in six ADLs (bathing, dressing, toileting, transferring, continence, and feeding) with the resulting score ranging from 0 (dependent for all ADLs) to 6 (independent with all ADLs) (29). The Lawton Scale sums a rating of independence in eight IADLs (shopping, food preparation, managing finances, housekeeping, laundry, ability to use telephone, mode of transportation, and managing medications) with the resulting score ranging from 0 (dependent for all IADLs) to 8 (independent with all IADLs) (30).
Additional information collected at time of follow-up included the patient’s residence type (private home, assisted living facility, nursing facility) and whether any hospital readmissions had occurred, self-reported by patients or their proxies. Two investigator-developed questions about post-injury recovery and complications were included: “Have you returned to your pre-injury level of function?” and “Were there any complications in your recovery process?”. If a proxy respondent completed the survey, they were asked to answer the questions based on knowledge of the patient’s recovery process and current condition. Binary “yes/no” responses were recorded to these two questions and patient and proxy comments were transcribed by study coordinators at the time of the call. Death within one-year of hospital discharge was determined by querying state vital records data.
Covariates
Baseline patient demographic and clinical data was collected using the electronic health record (EHR) and Trauma Registry for patients age 65 years and older admitted to the TICU after July 1, 2017, and included age, sex, race and ethnicity, Charlson comorbidity index, trauma mechanism, Injury Severity Score, hospital length of stay, and discharge location type. The Clinical Frailty Scale was only recorded for patients admitted after Geri-T implementation. Race and ethnicity were patient or proxy-reported and entered in the EHR at time of admission. Pre-admission residence type and independence with ADLs was obtained from review of social work and physical or occupational therapy documentation respectively.
Data Analysis
Stata/BE 17.0 was used for the quantitative data analysis. Categorical variables were described in frequencies and percentages. Measures of central tendency and variability were provided for continuous variables. In order to assess potential non-response bias, baseline characteristics among patients with completed surveys were compared to those who were lost to follow-up. Patients were classified as exposed to the Geri-T bundle if they were hospitalized in 2018 after Geri-T implementation, and were compared to an unexposed cohort of patients admitted in the prior year. With our sample size of 126 (pre-bundle, n=61; post-bundle, n=65), we had 80% power to detect a 15% change in EQ5D5L score, a 1-point difference in the Katz Index, and a 1-point difference in the Lawton Scale comparing patients admitted in 2017 versus 2018 with maximal α-level of 0.05. Linear regression models with robust standard errors were created for each of the three primary outcomes of interest, adjusting for suspected confounders selected a priori including age, Injury Severity Score (ISS), Charlson comorbidity index, and injury mechanism of a fall. Patients with missing data for a given outcome were excluded from the model.
Time from hospital discharge date and survey administration differed slightly between cohorts. A sensitivity analysis was thus performed restricting the sample only to patients who completed the telephone survey within 365 +/− 45 days of the hospital discharge date, and repeating the primary analyses to assess whether the results were robust to differences in time-to-survey.
Additional outcomes of interest that were described but not tested inferentially in regression models included one-year cumulative mortality, independence with all ADLs and IADLs respectively, whether the patient was living in a skilled nursing facility, and binary responses to the questions “Have you returned to your pre-injury level of function?” and “Were there any complications in your recovery process?”. Narrative responses to these two open-ended questions regarding recovery experiences were analyzed using content analysis which entails an iterative approach to identifying central themes in narrative responses through the development of a coding scheme (31). To ensure trustworthiness, all responses were analyzed by three of the co-authors (L.P., J.L., K.O.) and agreement was achieved by consensus.
Results
Survey Administration
One hundred and twenty-nine older patients were admitted to the TICU before Geri-T implementation and 125 patients were admitted after Geri-T implementation. The cumulative in-hospital mortality rate was 14% in both groups. Attempts were made to reach all 218 patients who survived hospitalization by telephone about one-year after hospital discharge (Figure 1). The most common reason that a patient or proxy could not be reached was that the telephone rang with no answer for three attempts at different times of day. Overall, 146 (67%) of patients or their proxies were reached by telephone. Eighteen proxies reported that the patient had died after hospital discharge and two patients had to end the call before all surveys could be completed. Telephone survey administration was complete for 126 patients, with 61 participants having been admitted pre-bundle, and 65 admitted post-bundle implementation.
Figure 1.
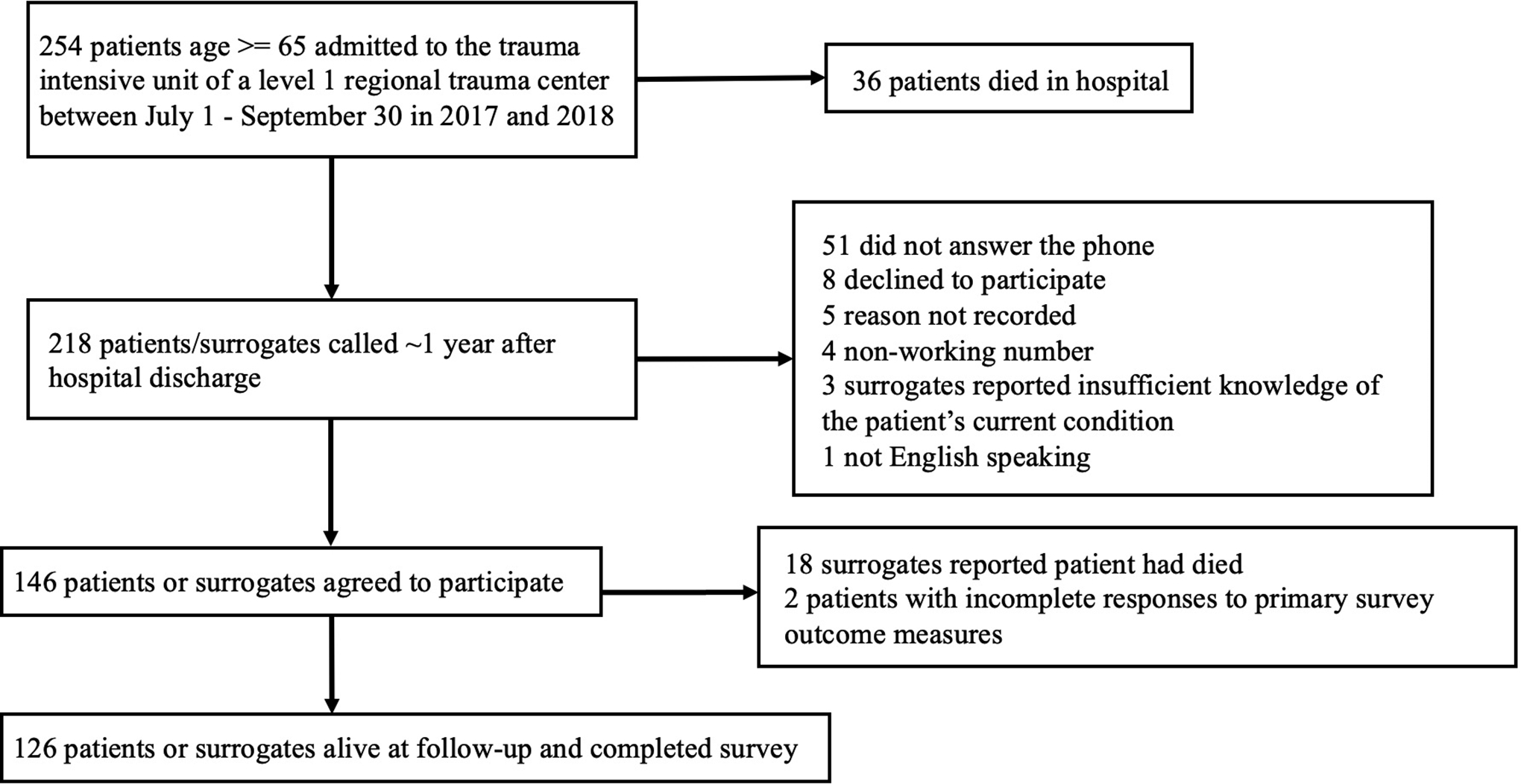
Flow chart of follow-up survey administration
The survey was administered at a median of 13 months after hospital discharge in the pre-bundle group and 11 months after hospital discharge in the post-bundle group. Overall, most (71%) respondents completed the survey within 365± 45 days of hospital discharge. In most cases, the survey was administered directly to the patient (77% and 74% of respondents were patients in the pre-bundle group and post-bundle groups respectively). Most proxy respondents (90%) were immediate family members (56% adult children, 36% partner, 9% other/unknown). Among patients for who the follow-up survey was completed by a proxy respondent, about one-third (31%) were living in a skilled care setting.
Patient Characteristics
Demographic and clinical characteristics of the sample of patients with completed surveys are presented in Table 1. The median age was 74 (IQR 69–83), a minority (36%) were female, and 87% reported that they were white and non-Hispanic. The median Charlson comorbidity index was 1 (IQR 0–2). Most patients had been living in a private residence and were independent with all ADLs prior to admission (97% and 89% respectively). The most common mechanisms of injury were falls (48%) and motor vehicle crashes (29%) and the median ISS was 17 (IQR 10–22). The median hospital length of stay was 7 days (IQR 5–12) and 50% of patients were discharged to a skilled nursing facility.
Table 1.
Characteristicsa of patients admitted before and after implementation of the Geri-T geriatric trauma bundle who completed or had a proxy complete the follow-up survey
| Pre-Bundle (n = 61) |
Post-Bundle (n = 65) |
Total (n = 126) |
p | |
|---|---|---|---|---|
| Age, years, median (IQR) | 73 (69–82) | 75 (70–83) | 74 (69–83) | 0.55 |
| Female, n (%) | 25 (41) | 20 (31) | 45 (36) | 0.23 |
| Race, n (%) | ||||
| White | 57 (93) | 57 (88) | 114 (90) | 0.22 |
| Black | 2 (3) | 1 (2) | 3 (2) | |
| Asian | 2 (3) | 3 (5) | 5 (4) | |
| Other/Unknown | - | 4 (6) | 4 (3) | |
| Hispanic ethnicity, n (%) | 1 (2) | 2 (3) | 3 (2) | 0.71 |
| Charlson comorbidity index, median (IQR) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0.52 |
| Living in private home pre-admission, n (%) | 58 (95) | 64 (98) | 122 (97) | 0.28 |
| Independent with all ADLs pre-admission, n (%)b | 56 (92) | 56 (86) | 112 (89) | |
| Trauma mechanism, n (%) | 0.07 | |||
| Fall | 23 (38) | 38 (58) | 61 (48) | |
| Motorvehicle crash | 25 (41) | 12 (18) | 37 (29) | |
| Struck pedestrian | 6 (10) | 4 (6) | 10 (8) | |
| Bicycle accident | 3 (5) | 5 (8) | 8 (6) | |
| Horseback riding accident | 3 (5) | 3 (5) | 6 (5) | |
| Other | 1 (2) | 3 (5) | 4 (3) | |
| Injury severity score, median (IQR) | 19 (14–25) | 14 (10–20) | 17 (10–22) | 0.02 |
| AIS Head ≥ 3, n (%) | 13 (21) | 7 (11) | 20 (16)) | 0.38 |
| AIS Chest ≥ 3, n (%) | 42 (69) | 40 (62) | 82 (65) | 0.03 |
| AIS Abdomen/Pelvis ≥ 3, n (%) | 7 (11) | 8 (12) | 15 (12) | 0.87 |
| AIS Extremities ≥ 3, n (%) | 20 (33) | 13 (20) | 33 (26) | 0.37 |
| Hospital length of stay, median (IQR) | 9 (5–14) | 7 (4–10) | 7 (5–12) | 0.17 |
| Discharge location, n (%) | 0.09 | |||
| Home | 22 (36) | 36 (55) | 58 (46) | |
| Skilled nursing facility | 36 (59) | 27 (42) | 63 (50) | |
| Other | 3 (5) | 2 (3) | 5 (4) | |
| Who completed survey, n (%) | 0.24 | |||
| Patient | 47 (77) | 48 (74) | 95 (75) | |
| Family member | 14 (23) | 14 (22) | 28 (22) | |
| Friend | 0 (0) | 3 (5) | 3 (2) | |
| Elapsed time between discharge and survey completion, months, median (IQR) | 13 (13–14) | 11 (11–12) | 12 (11–13) | <0.01 |
Demographic and clinical characteristics were abstracted from the electronic health record and state trauma registry
Level of independence with ADLs pre-admission was unknown for two patients, one in the pre-bundle and one in the post-bundle group
Patients in the pre- and post-bundle groups were comparable with regards to age, race, ethnicity, Charlson comorbidity index, pre-admission residence type, and ADL independence. There was a greater proportion of patients in the post-bundle group experiencing a fall as the mechanism of injury (58% vs 38%), and the median (interquartile range (IQR)) ISS in the post-bundle group was 14 (10–20) as compared to 19 (14–25) in the pre-bundle group. A lower proportion of those in the post-bundle group were discharged to a skilled nursing facility compared to those in the pre-bundle group (42% vs 59% respectively). The median (IQR) CFS score recorded at time of hospital admission among patients in the post-bundle group was 3 (managing well) with an interquartile range of 2 (fit) to 5 (mild frailty). Few patients in the post-bundle group had severe frailty (10% with CFS 7–9). Cumulative one-year mortality was similar in the pre- and post-bundle groups (23% and 26% respectively).
Of note, nearly half (42%) of the patients who were frail died within one year of hospital admission and therefore could not be included in the survey sample. Patients with completed surveys were similar by age, ethnicity, Charlson comorbidity index, ISS, hospital length of stay, and discharge location compared to those without completed surveys and who had not died (SDC Table 3). There were differences in the proportion with a fall as the mechanism of injury (48% among those with completed surveys versus 61% among those without completed surveys) and the proportion independent with all ADLs pre-admission (90% vs 75% respectively).
Outcomes One-Year After Hospital Discharge Among Survivors
Exposure to the Geri-T bundle was not found to be statistically associated with HRQOL as measured by the EQ-5D-5L or functional ability as measured by the Katz ADL Index or the Lawton IADL Scale in unadjusted or adjusted analyses. TICU admission post-bundle was associated with a .004 (95% CI −0.07 – 0.07) difference in EQ-5D-5L index score, a −0.29 (95% CI −0.66 – 0.09) difference in Katz ADL Index score, and a 0.29 (95% CI −0.60 – 1.18) difference in Lawton IADL Scale score after adjusting for age, sex, Charlson comorbidity index, ISS, and injury mechanism of a fall. Similar negative results were obtained in the sensitivity analysis limiting the multivariable regression models only to patients with surveys completed within 365 ± 45 days of hospital discharge (SDC Table 5).
The mean EQ-5D-5L index score at time of follow-up among all patients with completed surveys was 0.78 (SD 0.18) (Table 2), comparable to age-adjusted national norms. Review of results by EQ-5D-5L domain revealed prevalent report of problems across all domains, with 63% of patients experiencing pain or discomfort, 51% with difficulty performing usual activities, 46% with difficulty with walking, 27% with difficulty with self-care, and 43% experiencing anxiety or depression (SDC Table 4). The mean Katz ADL score was 5.4 (SD 1.2) and the mean Lawton IADL score was 6.2 (SD 2.8). About a quarter (24%) of patients reported dependence in at least one ADL domain and 63% reported dependence in at least one IADL domain. Among 111 patients who were documented to have been independent with all ADLs prior to hospital admission, survived to one-year, and completed the follow-up survey, 18% reported dependency in at least one ADL domain consistent with loss of ADL function. Most patients (90%) reported living in a private home at time of follow-up and 25% reported a hospital readmission.
Table 2.
Primary and secondary outcomes measured about one-year after hospital discharge
| Pre-bundle (n=61)a |
Post-bundle (n=65)a |
All patients (n=126)a |
Unadjusted difference | Adjustedb difference | 95% CI | |
|---|---|---|---|---|---|---|
| Primary Outcomes a | ||||||
| EQ-5D-5L index score, mean (SD) | 0.77 (0.18) | 0.78 (0.18) | 0.78 (0.18) | 0.01 | 0.004 | −0.07 – 0.07 |
| Katz ADLc score, mean (SD) | 5.7 (0.9) | 5.2 (1.5) | 5.4 (1.2) | −0.50 | −0.02 | −0.05 – 0.01 |
| Lawton IADLd score, mean (SD) | 6.1 (2.9) | 6.3 (2.8) | 6.2 (2.8) | 0.20 | 0.29 | −0.60 – 1.18 |
| Secondary Outcomes | ||||||
| Hospital readmission, n (%) | 16 (29) | 14 (22) | 20 (25) | |||
| Living in private home, n (%) | 52 (85) | 61 (94) | 113 (90) | |||
| Independent with all ADLsc, n (%) | 51 (85) | 44 (67) | 95 (76) | |||
| Independent with all IADLsd, n (%) | 36 (62) | 41 (63) | 77 (63) | |||
| Reported return to pre-injury function, n (%) | 17 (32) | 24 (37) | 41 (35) | |||
| Reported complications in recovery process, n (%) | 20 (38) | 27 (42) | 47 (40) |
≤ 10% missingness for all variables
Results of linear regression adjusting for age, Injury Severity Score, Charlson comorbidity index score, and fall injury mechanism
Activities of daily living
Instrumental activities of daily living
Patient and Proxy Perceptions of Post-Injury Recovery and Complications
Only 35% of survey respondents across both groups reported a return to pre-injury level of function, and 40% reported complications during the recovery process (Table 2). Content analysis of patients or proxy comments in response to the two questions about recovery experiences revealed themes of persistent functional limitations, pain, and cognitive dysfunction (Figure 2). Patients described disappointment with inability to perform activities beyond those of daily living that they enjoyed prior to their injury. Many attributed lack of recovery to their pre-hospitalization baseline to ongoing pain stemming from their injuries. Proxy respondents shared concern about patients’ new or worsening cognitive impairments after injury, in some cases describing cognitive dysfunction that interfered with rehabilitation.
Figure 2.
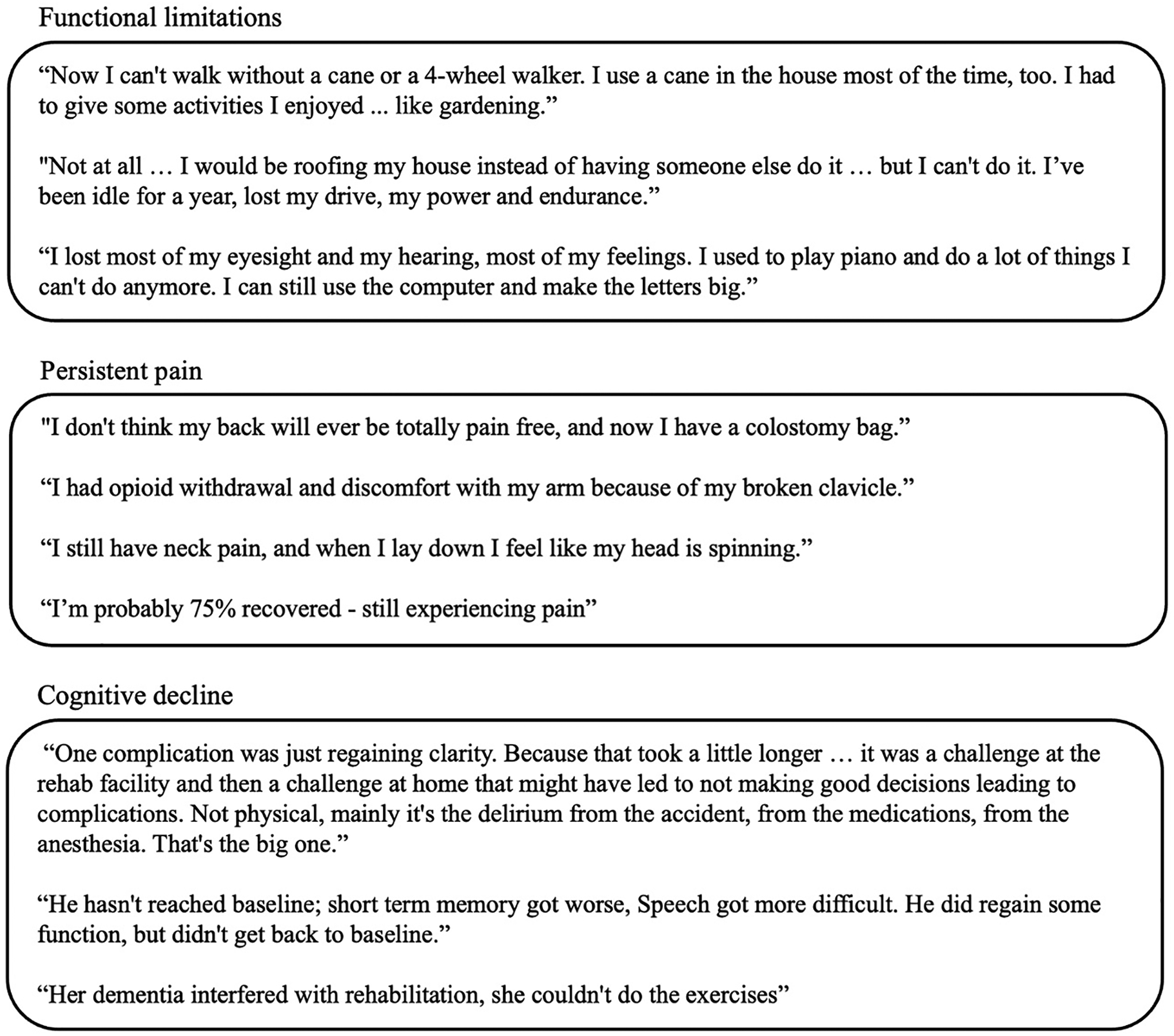
Select patient and surrogate responses to the questions: (1) “Have you returned to your pre-injury level of function?” and (2) “Were there any complications in your recovery process?”
Discussion
This is one of few studies to describe long-term HRQOL, functional independence, and perceptions of recovery among older survivors of severe traumatic injury. Approximately one in five survivors experienced loss of ADL independence at one-year follow-up. Nonetheless, the majority were community-dwelling and independent with most ADLs and IADLs. HRQOL was comparable to age-adjusted U.S. population norms, with mean EQ-5D-5L index score of 0.78 (SD 0.18) in the study sample compared to 0.82 (SD 0.22) among patients age 65 and older nationally (28). There was no association between increased geriatrics-centered multidisciplinary TICU care prompted by the Geri-T care bundle and long-term HRQOL or function among survivors. Despite this high level of independence with ADLs and IADLs, most respondents reported a lack of recovery to pre-injury functional baseline, describing difficulty participating in activities they previously enjoyed, persistent pain, and cognitive dysfunction.
Our inability to detect an improvement in one-year functional ability and HRQOL in patients admitted after Geri-T suggest that multiple other factors not addressed by this care bundle influence long-term outcomes. These factors include but are not limited to the overall injury burden in patients treated in the TICU, patients’ pre-injury health trajectory, other interventions and care delivered in the trauma center, and access to rehabilitation and other post-discharge services. Other possible explanations include the heterogeneity of the older adult trauma population, a restricted focus on patients requiring TICU care, and the possibility of small differences between groups that this study was not powered to detect.
Along these lines, our findings differ from one prior study of long-term ADL function among older survivors of traumatic injury admitted before versus after implementation of a care pathway involving routine geriatrics consultation. Similar to our study, patients included had few functional impairments prior to injury. The authors found that patients exposed to the care pathway demonstrated a difference of 0.67 ADL abilities retained at one-year compared to unexposed patients.(13) Notably, geriatrics consultations were not linked to frailty assessment and the study population was not limited to patients requiring TICU care, suggesting that older trauma patients without TICU needs or frailty may obtain long-term benefit from CGA. This prior work, as well as studies of inpatient geriatrics assessment among older adults hospitalized for hip fracture(32) or medical illness(33) support that hospital-based interventions do have potential to influence long-term functional outcomes. Notably, most similar prior studies of geriatric trauma care pathways have not described pre-injury functional independence among participants. Improved reporting of pre-injury functional status would allow for increased comparability across studies and potentially help to identify which injured older adults are likely to benefit from specialized pathways.
Perceptions of recovery and complications after injury described by respondents highlighted persistent problems not captured by validated surveys of function and HRQOL. Severe injury was described as a life-altering event resulting in ongoing difficulty with activities beyond those of daily living. There is a dearth of literature qualitatively examining the experiences of recovery after injury among older adults and their family members. While standardized and validated assessments are important for comparability across studies, qualitative work could inform allied healthcare providers who care for older patients after injury to tailor post-discharge therapies to individual goals. Persistent pain and new or worsening cognitive deficits were also commonly described by patients and their proxies. While cognitive impairment has been extensively studied among survivors of head injury (34) and of general critical illness (35,36), there is a gap in the literature regarding trajectories in cognition after severe trauma among older adults. A better understanding of long-term cognitive outcomes could inform the development of interventions to address cognitive decline, such as inpatient delirium prevention strategies, and help to set expectations for patients and their families. Prior work has demonstrated a high prevalence of persistent pain after serious injury among adults of all ages, (37) however little is known regarding the incidence of chronic pain among older adults after serious injury. Given rising rates of opioid misuse, dependence, and overdose among older adults, (38,39) future studies might also examine persistent pain post-injury as a risk factor for opioid-related adverse events.
This study has several limitations. While we retained two-thirds of eligible respondents for telephone interviews, the overall sample size was relatively small and TICU survivors not represented in our sample due to loss to follow-up had a slightly lower proportion of complete independence with ADLs prior to hospitalization. This may have biased descriptive findings towards higher mean functional ability scores and HRQOL at 1-year. However, we controlled for baseline characteristics including a fall as the injury mechanism, which has been shown to be associated with frailty (40,41), in inferential analyses. There may be differences in patient groups between 2017 and 2018, but there were no other known changes in trauma care that took place at the hospital where Geri-T was implemented during these years. We lacked data on adherence to recommendations made by geriatrics consultants, as well as on pre-hospitalization IADL function and HRQOL prohibiting a comparison of changes in these specific measures relative to baseline; however we were able to examine changes in ADL function relative to baseline. Participants were aware at the time of the interview of the researchers’ interest in studying trauma care practices, raising the possibility of bias due to the Hawthorne effect. Finally, the two open-ended investigator-developed questions were not cognitively tested prior to survey administration.
Despite these limitations, this study contributes meaningfully to a small body of literature on long-term patient-centered outcomes among older trauma survivors. We demonstrated loss of ADL function in one in five survivors one-year after injury and found patient-reported HRQOL to be close to age-adjusted national norms. Responses to open-ended questions about recovery suggest that further characterization of chronic pain and persistent cognitive dysfunction after serious injury in older adults is needed. Geri-T was not associated with any significant differences in long-term functional ability or HRQOL, suggesting that hospital-based care bundles may not be sufficient to improve long-term patient-centered outcomes in the absence of high-quality post-discharge rehabilitation services.
Supplementary Material
SDC Table 1: STROBE reporting guideline checklist
SDC Table 2. Patient characteristics among those who died during hospitalization, those who died within 1-year of hospital discharge, and those still alive one year after hospital discharge
SDC Table 3. Patient characteristics among those who survived hospitalization by survey completion status
SDC Table 4. Domain-specific health-related quality of life reported by patients or their proxies at time of follow-up
SDC Table 5. Health-related quality of life and functional ability among respondents restricted to those who completed the survey within 365 ± 45 day of hospital discharge
Acknowledgements:
We acknowledge Susan Corvallis and Amanda Sigala for their assistance with electronic health record and state vital records data acquisition and management.
Conflicts of Interest and Source of Funding:
There are no conflicts of interest to declare. Funding sources for this study included the University of Washington Patient Safety and Innovations Program and NHBLI Palliative Care Research Training Grant (5 T32HL 125195-07)
Footnotes
Meeting Presentations: Preliminary findings from this work were presented at the May 2019 Annual Scientific Meeting of the American Geriatric Society in Portland, Oregon in Poster Session D.
Supplemental Digital Content
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com). The SDC includes:
References:
- 1.Centers for Disease Control and Prevention. Leading Causes of Death by Age Group United States 2018. National Center for Injury Prevention and Control, CDC using WISQARS; [Google Scholar]
- 2.Richmond TS, Kauder D, Strumpf N, Meredith T. Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatr Soc. 2002;50(2):215–22. [DOI] [PubMed] [Google Scholar]
- 3.Hashmi A, Ibrahim-Zada I, Rhee P, Aziz H, Fain MJ, Friese RS, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76(3):894–901. [DOI] [PubMed] [Google Scholar]
- 4.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term Survival of Adult Trauma Patients. JAMA. 2011;305(10):1001–7. [DOI] [PubMed] [Google Scholar]
- 5.Huntington CR, Kao AM, Sing RF, Ross SW, Christmas AB, Prasad T, et al. Unseen Burden of Injury: Post-Hospitalization Mortality in Geriatric Trauma Patients. Am Surg. 2021;31348211046886. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman EJ, Zebrowski AM, Holena DN, Loher P, Wiebe DJ, Carr BG. The Short and the Long of it: Timing of Mortality for Older Adults in a State Trauma System. J Surg Res. 2021;268:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maxwell C, Mion L, Mukherjee K, Dietrich M, Minnick A, May A, et al. Preinjury physical frailty and cognitive impairment among geriatric trauma patients determine postinjury functional recovery and survival. J Trauma Acute Care Surg. 2016;80(2):195–203. [DOI] [PubMed] [Google Scholar]
- 8.Jeffery AD, Dietrich MS, Maxwell CA. Predicting 1-year disability and mortality of injured older adults. Arch Gerontol Geriatr. 2018;75:191–6. [DOI] [PubMed] [Google Scholar]
- 9.Eagles D, Godwin B, Cheng W, Moors J, Figueira S, Khoury L, et al. A systematic review and meta-analysis evaluating geriatric consultation on older trauma patients. J Trauma Acute Care Surg. 2020;88(3):446–53. [DOI] [PubMed] [Google Scholar]
- 10.Park C, Bharija A, Mesias M, Mitchell A, Krishna P, Storr-Street N, et al. Association Between Implementation of a Geriatric Trauma Clinical Pathway and Changes in Rates of Delirium in Older Adults With Traumatic Injury. JAMA Surg. 2022;157(8):676–683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bryant EA, Tulebaev S, Castillo-Angeles M, Moberg E, Senglaub SS, O’Mara L, et al. Frailty Identification and Care Pathway: An Interdisciplinary Approach to Care for Older Trauma Patients. J Am Coll Surg. 2019;228(6):852–859.e1. [DOI] [PubMed] [Google Scholar]
- 12.Wong CL, Al Atia R, McFarlan A, Lee HY, Valiaveettil C, Haas B. Sustainability of a proactive geriatric trauma consultation service. Can J Surg. 2017;60(1):14–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tillou A, Kelley-Quon L, Burruss S, Morley E, Cryer H, Cohen M, et al. Long-term postinjury functional recovery: outcomes of geriatric consultation. JAMA Surg. 2014; 149(1):83–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. [DOI] [PubMed] [Google Scholar]
- 15.Crocker TF, Brown L, Clegg A, Farley K, Franklin M, Simpkins S, et al. Quality of life is substantially worse for community-dwelling older people living with frailty: systematic review and meta-analysis. Qual Life Res. 2019;28(8):2041–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang SF, Wen GM. Association of frail index and quality of life among community-dwelling older adults. J Clin Nurs. 2016;25(15–16):2305–16. [DOI] [PubMed] [Google Scholar]
- 17.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186(2):E95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrante LE, Murphy TE, Gahbauer EA, Leo-Summers LS, Pisani MA, Gill TM. Pre-Intensive Care Unit Cognitive Status, Subsequent Disability, and New Nursing Home Admission among Critically Ill Older Adults. Ann Am Thorac Soc. 2018;15(5):622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hwang F, Pentakota SR, McGreevy CM, Glass NE, Livingston DH, Mosenthal AC. Preinjury Palliative Performance Scale predicts functional outcomes at 6 months in older trauma patients. J Trauma Acute Care Surg. 2019;87(3):541–51. [DOI] [PubMed] [Google Scholar]
- 22.Cords CI, Spronk I, Mattace-Raso FUS, Verhofstad MHJ, van der Vlies CH, van Baar ME. The feasibility and reliability of frailty assessment tools applicable in acute in-hospital trauma patients: A systematic review. J Trauma Acute Care Surg. 2022;92(3):615–26. [DOI] [PubMed] [Google Scholar]
- 23.Rockwood K, Theou O. Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources. Can Geriatr J. 2020. 1;23(3):210–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clinical Frailty Scale [Internet]. Dalhousie University. [cited 2022 Sep 8]. Available from: https://www.dal.ca/sites/gmr/our-tools/clinical-frailty-scale.html
- 25.Reimer B, Roth V, Montgomery R. Optimizing Call Patterns for Landline and Cell Phone Surveys. Proc Am Stat Assoc. 2012;2012:4648–60. [PMC free article] [PubMed] [Google Scholar]
- 26.Vallance JK, Eurich DT, Gardiner PA, Taylor LM, Stevens G, Johnson ST. Utility of telephone survey methods in population-based health studies of older adults: an example from the Alberta Older Adult Health Behavior (ALERT) study. BMC Public Health. 2014;14(1):486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy Amst Neth. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 28.Jiang R, Janssen MFB, Pickard AS. US population norms for the EQ-5D-5L and comparison of norms from face-to-face and online samples. Qual Life Res. 2021;30(3):803–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katz S, Downs TD, Cash HR, Grotz RC. Progress in Development of the Index of ADL1. The Gerontologist. 1970;10(1_Part_1):20–30. [DOI] [PubMed] [Google Scholar]
- 30.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–86. [PubMed] [Google Scholar]
- 31.Hsieh HF, Shannon SE. Three Approaches to Qualitative Content Analysis. Qual Health Res. 2005;15(9):1277–88. [DOI] [PubMed] [Google Scholar]
- 32.Pfeufer D, Kammerlander C, Stadler C, Roth T, Blauth M, Neuerburg C, et al. Multidisciplinary inpatient rehabilitation improves the long-term functional status of geriatric hip-fracture patients. Eur J Med Res. 2020;25(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilhelmson K, Andersson Hammar I, Westgård T, Holmquist Henrikson L, Dahlin-Ivanoff S. Positive effects on activities of daily living one year after receiving comprehensive geriatric assessment - results from the randomised controlled study CGA-Swed. BMC Geriatr. 2022;22(1):180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moretti L, Cristofori I, Weaver SM, Chau A, Portelli JN, Grafman J. Cognitive decline in older adults with a history of traumatic brain injury. Lancet Neurol. 2012;11(12):1103–12. [DOI] [PubMed] [Google Scholar]
- 35.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term Cognitive Impairment and Functional Disability Among Survivors of Severe Sepsis. JAMA. 2010;304(16):1787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-Term Cognitive Impairment after Critical Illness. N Engl J Med. 2013;369(14):1306–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rivara FP, MacKenzie EJ, Jurkovich GJ, Nathens AB, Wang J, Scharfstein DO. Prevalence of Pain in Patients 1 Year After Major Trauma. Arch Surg. 2008;143(3):282–7. [DOI] [PubMed] [Google Scholar]
- 38.Wei YJJ, Chen C, Lewis MO, Schmidt SO, Winterstein AG. Trajectories of prescription opioid dose and risk of opioid-related adverse events among older Medicare beneficiaries in the United States: A nested case–control study. PLoS Med. 2022;19(3):e1003947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zullo AR, Danko KJ, Moyo P, Adam GP, Riester M, Kimmel HJ, et al. Prevention, Diagnosis, and Management of Opioids, Opioid Misuse, and Opioid Use Disorder in Older Adults [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2020. [cited 2022 May 26]. (AHRQ Comparative Effectiveness Technical Briefs). Available from: http://www.ncbi.nlm.nih.gov/books/NBK564144/ [PubMed] [Google Scholar]
- 40.Cheng MH, Chang SF. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis. J Nurs Scholarsh. 2017;49(5):529–36. [DOI] [PubMed] [Google Scholar]
- 41.Zaslavsky O, Zelber-Sagi S, Gray SL, LaCroix AZ, Brunner RL, Wallace RB, et al. Comparison of Frailty Phenotypes for Prediction of Mortality, Incident Falls, and Hip Fracture in Older Women. J Am Geriatr Soc. 2016;64(9):1858–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC Table 1: STROBE reporting guideline checklist
SDC Table 2. Patient characteristics among those who died during hospitalization, those who died within 1-year of hospital discharge, and those still alive one year after hospital discharge
SDC Table 3. Patient characteristics among those who survived hospitalization by survey completion status
SDC Table 4. Domain-specific health-related quality of life reported by patients or their proxies at time of follow-up
SDC Table 5. Health-related quality of life and functional ability among respondents restricted to those who completed the survey within 365 ± 45 day of hospital discharge


