Abstract
Background:
Shock index (SI) predicts outcomes after trauma. Prior single center work demonstrated that emergency medical services (EMS) initial SI was the most accurate predictor of hospital outcomes in a rural environment. This study aimed to evaluate the predictive ability of SI in multiple rural trauma systems with prolonged transport times to a definitive care facility.
Methods:
This retrospective review was performed at four ACS-verified level 1 trauma centers with large rural catchment basins. Adult trauma patients who were transferred and arrived >60 minutes from scene during 2018 were included. Patients who sustained blunt chest or abdominal trauma were analyzed. Subjects with missing data or severe head trauma (AIS>2) were excluded. Poisson and binomial logistic regression were utilized to study the effect of SI and delta SI (∆SI) on outcomes.
Results:
After applying criteria 789 patients were considered for analysis, 502 scene patients and 287 transfers. Mean ISS was 8 (IQR 6) for scene and 8.9 (IQR 5) for transfers. Initial EMS SI was a significant predictor of the need for blood transfusion and ICU care in both scene and transferred patients. An increase in ∆SI was predictive of the need for operative intervention (p<0.05). There were increased odds for mortality for every 0.1 change in EMS SI, those changes were not deemed significant among both scene and transfer patients (p<0.1).
Conclusions:
Providers must maintain a high level of clinical suspicion for patients who had an initially elevated SI. EMS SI is a significant predictor for use of blood and ICU care, as well as mortality for scene patients. This highlights the importance of SI and ∆SI in rural trauma care.
Level of Evidence:
Level IV, Prognostic/Epidemiological
Keywords: rural trauma, prehospital care, shock index
Introduction:
Rural Americans comprise nearly 60 million people, 19% of the population. Of these 30 million reside over an hour from high-level trauma care.1,2 To deliver comprehensive care in these environments, states have developed trauma systems to deliver emergency medical services (EMS) care and transport; they also rely on Level III and IV trauma centers to provide initial evaluation and stabilization before transport to a definitive care center. Because of extended travel times to many rural patients, it can take several hours for EMS to both reach and return a patient to definitive and surgical trauma care. En route, patients receive variable levels of resuscitation and intervention. Despite these systems, rural trauma patients continue to have significant disparities and higher mortality than their matched urban counterparts.3–5 How rural patients are optimally triaged and transported remains an area for further research.
Shock index (SI) and delta shock index (∆SI) predict outcomes in trauma patients and have been associated with mortality and the need for blood transfusion.6–8 An elevated shock index is well validated enough in prehospital care that it was added as a new criterion to the 2021 iteration of the national guidelines for field triage.9 Research evaluating the use of prehospital SI showed that increases in ∆SI, that occur from EMS vital signs to hospital arrival, were also associated with poor outcomes.10 Most of the data currently available on SI has been from urban centers. There is however, a prior single-center study which demonstrated that the initial EMS SI was the most accurate predictor of hospital outcomes in a rural environment with prolonged transport times.11 In that study, increased EMS SI predicted the use of blood products, intensive care unit (ICU) need, length of stay (LOS), and mortality. As time from injury increased, shock index on hospital arrival or at a transferring facility was less predictive. This is of critical importance because as en route care and resuscitation continue to advance, there is the potential to mask vital sign changes that are expected with severe injury.
This study builds upon that prior work by evaluating the utility of EMS SI across multiple rural trauma systems. With total time in transport to definitive care routinely over several hours, the authors hypothesized that SI on hospital arrival was less predictive in a rural environment. Therefore, this study aimed to evaluate the predictive ability of SI and ∆SI in rural environments and investigate the impact of prolonged transport times.
Methods:
This was a retrospective registry review performed at four American College of Surgeons-verified Level 1 trauma centers as a portion of a research collaborative. Each center serves as the tertiary referral center for large rural catchment basins. The database was constructed to include all patients in 2018, that arrived as a full or partial trauma team activation; and were transferred from another facility to the Level 1 center or a scene transport that arrived more than 60 minutes after injury. Inpatient transfers, patients operated on at a transferring facility, and subjects less than 18 years old were excluded from the database. For this analysis, the database was queried for all adult subjects presenting after blunt chest or abdominal trauma (AIS≥1). Subjects with missing shock index data, severe head trauma (AIS Head>2), penetrating injuries, missing transport times, and deaths in the emergency department were excluded. Institutional review board approval was obtained at each center prior to database creation. The study was completed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (supplemental digital content 1).
Each center prospectively maintains its trauma database by utilizing trained registrars. Data abstracted included demographics, injury data, injury severity score (ISS), abbreviated injury score (AIS) by region, transport type, time in transport, hospital procedures, EMS and transferring facility data on vital signs and transfusions, and hospital data on operations and procedures.
Shock index was calculated as heart rate divided by systolic blood pressure (SI=HR/SBP). This was calculated from registry vitals from the first set of scene EMS vitals (SI-EMS), transferring facilities (SI-TX), and on arrival for definitive care (SI-DC). Delta SI and SI were determined at each phase of transport to understand the importance of the different time periods associated with outcomes. Hypotension was considered for analysis as well; this was defined as a patient having an SBP<90 for EMS. Primary outcomes were mortality and the need for a hemorrhage control operation within 24 hours. Secondary outcomes focused on resource utilization and included: need for ICU, ICU LOS, need for blood product transfusion, and the number of units transfused.
Statistical analysis was performed utilizing zero inflated Poisson regression for outcomes of ICU length of stay and units of blood utilized. This approach allows for the statistical analysis to simultaneously consider all covariates and the statistical models impact on the binary use of the resource, while also estimating the impact the covariate has on the amount of the resource. A Binomial logistic regression was utilized for outcomes of surgical intervention and mortality. Scene and transfer patients were analyzed separately to study the effect of time in transport and SI/∆SI on resource utilization and outcomes. As this is a multi-center study, fixed effects for each center were included in the regression model for each outcome studied to account for between center differences. The models also included an indicator variable for hypotension, SI-EMS, and relevant ∆SI for each patient group, similar to prior published work.11 As hypotension and SI are related, we also perform an analysis with hypotension omitted from the regression models. P<0.05 was considered significant.
Results:
After applying inclusion and exclusion criteria, a sample of 789 patients was analyzed (Figure 1). This included 502 (63.6%) scene patients and 287 (36.4%) transferred from another facility. Baseline demographics are reported in Table 1. After arrival for definitive care, blood products were transfused in 8.8% of scene patients and 9.4% of transfer patients. Operative intervention was required in 109 (21.7%) of scene patients and 101 (35.2%) of transfers.
Figure 1.
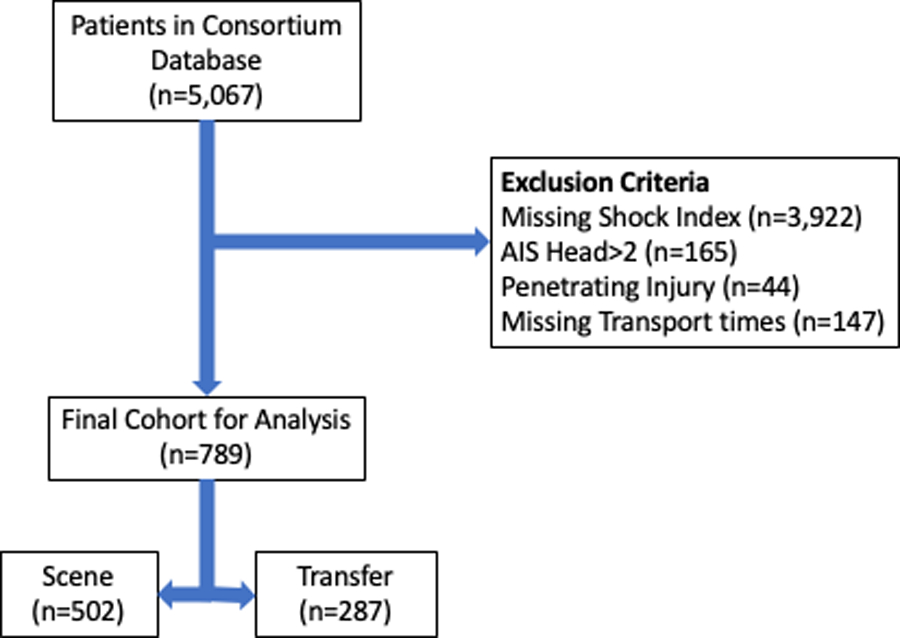
Flow diagram of patients included in final analysis
Table 1.
Baseline Characteristics of Patient Cohort
| SCENE | TRANSFER | |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 51.8 ± 21.4 | 57 ± 20.6 |
| Median | 51 | 57 |
| IQR | 34 | 34 |
| Sex | F: 39.4% M: 60.6% |
F: 53.2% M: 46.8% |
| Time in Transport (minutes) | ||
| Mean ± SD | 96.3 ± 90.9 | 326 ± 140.5 |
| Median | 71 | 308.5 |
| IQR | 30 | 167.75 |
| Mechanism of Injury | ||
|
Auto vs Ped:
Fall: MCC: MVC: Other: |
1.99% 36.45% 7.17% 42.03% 12.35% |
1.05% 49.30% 3.50% 36.71% 9.44% |
| Hypotension at Scene | ||
| 2.39% | 2.80% | |
| ISS | ||
| Mean ± SD | 7.7 ± 6.3 | 8.9 ± 6 |
| Median | 5 | 9 |
| IQR | 6 | 5 |
| AIS Thorax | ||
| Mean ± SD | 0.66 ± 1.1 | 0.64 ± 1.2 |
| Median | 0 | 0 |
| IQR | 1 | 1 |
| AIS Abdomen | ||
| Mean ± SD | 0.30 ± 0.8 | 0.3 ± 0.8 |
| Median | 0 | 0 |
| IQR | 0 | 0 |
| ICU Length-of-Stay (days) | ||
| Mean ± SD | 0.8 ± 2.3 | 1.1 ± 2.7 |
| Median | 0 | 0 |
| IQR | 0 | 1 |
| Days on Ventilator | ||
| Mean ± SD | 0.2 ± 1.0 | 0.5 ± 2.4 |
| Median | 0 | 0 |
| IQR | 0 | 0 |
| Hospital Length of Stay (days) | ||
| Mean ± SD | 5.1 ± 7.8 | 5.1 ± 5.4 |
| Median | 3 | 3 |
| IQR | 4 | 4 |
SD: Standard deviation; IQR: interquartile range; Auto vs Ped: automobile versus pedestrian; MCC: motorcycle collision; MVC: motor vehicle collision; ISS: injury severity score; AIS: abbreviated injury score; ICU: intensive care unit
We investigated SI and corresponding ∆SI as a correlate for injury severity. There was a weak positive correlation (r=0.12) between ISS and SI-EMS, and no correlation between ISS and ∆SI. For scene patients transported to the trauma center SI-EMS had a mean of 0.66 (standard deviation: 0.22), while the patients who were routed through a transferring facility had a mean SI-EMS of 0.65 (standard deviation: 0.19). This difference was not significant (p=0.357). For transferred patients, SI-TX had a mean of 0.63 (standard deviation: 0.19). On arrival for definitive care, the mean SI-DC was 0.65 (standard deviation: 0.20) for scene transports and 0.64 (standard deviation: 0.18) for transfers (p=0.917).
The mean ∆SI from SI-EMS to SI-DC for patients who were transported directly from the scene was –0.010 (standard deviation: 0.18), while those coming through a transfer facility had a mean ∆SI from SI-EMS to SI-DC of 0.0024 (standard deviation: 0.20) (p=0.38). For patients who were transferred, the ∆SI between SI-EMS and the SI-TX had a mean of –0.017 (standard deviation: 0.17).
The effects of SI and ∆SI were then evaluated on the need for blood product transfusion, number of units of packed red blood cells (PRBC) (Table 2), intensive care unit length of stay (ICU LOS) (Table 3, Figure 2), need for surgical intervention (Need for OR), and mortality (Table 4). In scene patients, SI-EMS was a significant predictor (p<0.05) for PRBC transfusion when identifying the need and number of units transfused. A 0.1 change in SI-EMS produced a 25.87% increase in the odds ratio on the use of blood. Similarly, ∆SI for scene patients was also significant (p<0.001), with a 0.1 change in delta SI resulting in a 36.93% increase in the odds ratio of the use of blood. In scene patients, a patient who had hypotension on scene had 41.90% higher odds ratio (p < 0.001) than one who did not present with hypotension. For transfer patients, we find that ∆SI in both legs of the transport is predictive of the use of blood with a 0.1 increase in ∆SI: SI-EMS to SI-TX increasing the odds ratio of blood use by 67.31% (p<.0001) and a 0.1 increase in ∆SI: SI- TX to SI-DC increasing the odds ratio of blood use by 38.28% (p<0.01). For scene patients, we saw a 7.633% (p< 0.01) and 12.08% (p<0.001) increase in the number of units of PRBC transfused with a 0.1 increase in SI and delta SI, respectively. In the case of transfer patients, results show that a 0.1 increase in SI resulted in a 45.79% (p<0.001) increase in the number of units transfused, while a 0.1 increase in the ∆SI between EMS and transfer facility resulted in 14.27% increase in the number of units used (p<0.01).
Table 2.
Evaluation of Use of Blood Products and Number of Units PRBC based on Scene or Transfer Status and the Effect of SI via Regression Coefficients.
| SCENE | TRANSFER | |||
|---|---|---|---|---|
|
| ||||
| VARIABLE╲RESPONSE | Use of Blood (Binomial Logistic) |
Number of Units of PRBC (Poisson) |
Use of Blood (Binomial Logistic) |
Number of Units of PRBC (Poisson) |
| SI-EMS | 2.301 ** | 0.7385 † | −2.724 | 3.771 ‡ |
| 95% CI | 0.4407 – 4.162 | 0.2417 – 1.235 | −6.791 – 1.344 | 1.739 – 5.802 |
|
| ||||
| ΔSI: SI-EMS to SI-DC | 3.547 ‡ | 1.141 ‡ | --- | --- |
| 95% CI | 1.766 – 5.327 | 0.5835 −1.698 | --- | --- |
|
| ||||
| ΔSI: SI-EMS to SI-TX | --- | --- | 5.147 † | 1.421 * |
| 95% CI | --- | --- | 1.809 – 8.486 | −0.0031 – 2.880 |
|
| ||||
| ΔSI: SI-TX to SI-DC | --- | --- | 3.241** | 0.5125 |
| 95% CI | --- | --- | 0.7332 – 5.748 | −0.4780 – 1.505 |
|
| ||||
| Hypotension | 3.500 ‡ | 0.394 | 21.67 | −2.846 † |
| 95% CI | 1.695 – 5.304 | −0.1010 – 0.8890 | −1211 – 1224 | −4.762 - −0.9299 |
|
| ||||
| Transport Time | 0.0001 | −0.0004 | 0.0009 | −0.0002 |
| 95% CI | −0.0037 – 0.0039 | −0.0026 – 0.0018 | −0.0030 – 0.0048 | −0.0031 – 0.0027 |
The significance is indicated by p-value<0.10 (*), p-value<0.05 (**), p-value <0.01 (†), p-value <0.001 (‡)
PRBC: packed red blood cells; SI: shock index, SI-EMS: emergency medical services shock index; ΔSI: change in shock index; SI-DC: shock index at definitive are center; SI-TX: shock index at transferring facility
Table 3.
Evaluation of Use of ICU and Number of ICU Days based on Scene or Transfer Status and the Effect of SI via Regression Coefficients.
| SCENE | TRANSFER | |||
|---|---|---|---|---|
|
| ||||
| VARIABLE╲RESPONSE | Need for ICU Stay (Binomial Logistic) |
Number of Days in ICU (Poisson) |
Need for ICU Stay (Binomial Logistic) |
Number of Days in ICU (Poisson) |
| SI-EMS | 1.022 | 0.6540 † | 1.425 | 1.360 † |
| 95% CI | −2.869 – 2.330 | 0.2480 – 1.060 | −0.5403 – 3.390 | 0.5440 – 2.177 |
|
| ||||
| ΔSI: SI-EMS to SI-DC | 2.883 ‡ | 0.2778 | ---- | ---- |
| 95% CI | 1.430 – 4.335 | −0.1363 – 0.6910 | --- | --- |
|
| ||||
| ΔSI: SI-EMS to SI-TX | --- | --- | 1.114 | 0.4692 |
| 95% CI | --- | --- | −0.9475 – 3.175 | −0.1889 – 1.127 |
|
| ||||
| ΔSI: SI-TX to SI-DC | --- | --- | 2.469 † | 0.8376 † |
| 95% CI | --- | --- | 0.6136 – 4.325 | 0.2954 – 1.380 |
|
| ||||
| Hypotension | 2.671 † | 0.2817 | 1.490 | −0.4995 |
| 95% CI | 1.044 – 4.298 | −0.1442 – 0.7075 | −0.8435 – 3.824 | −1.255 – 0.2559 |
|
| ||||
| Transport Time | 0.0004 | −0.0027 ** | −0.0012 | 0.0016 ‡ |
| 95% CI | −0.0039 – 0.0030 | −0.0052 - −0.0002 | −0.0034 – 0.0012 | 0.0009 – 0.0024 |
The significance is indicated by p-value<0.10 (*), p-value<0.05 (**), p-value <0.01 (†), p-value <0.001 (‡)
ICU: intensive care unit; SI: shock index, SI-EMS: emergency medical services shock index; ΔSI: change in shock index; SI-DC: shock index at definitive are center; SI-TX: shock index at transferring facility
Figure 2.
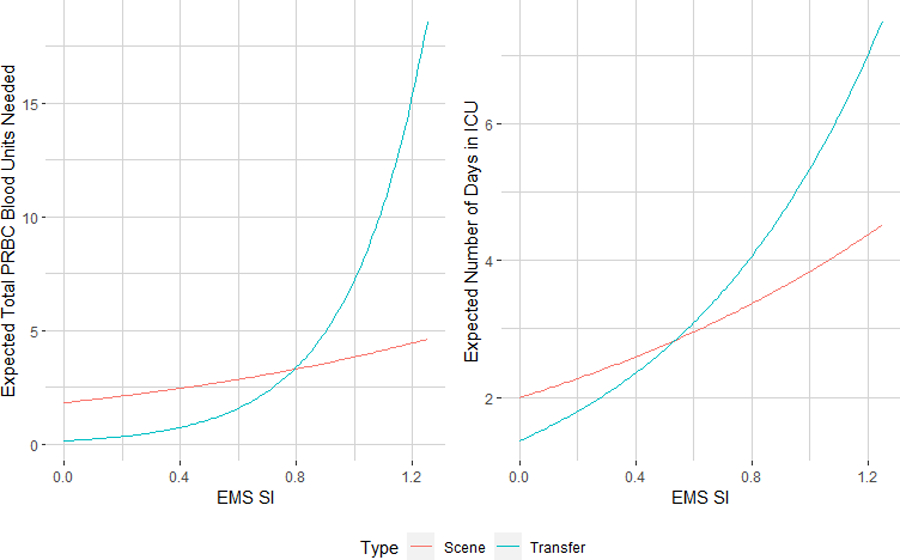
Effect plot demonstrating the expected total number of packed red blood cells (PRBC) transfused, and expected number of days in the intensive care unit (ICU) based on EMS shock index.
Table 4.
Evaluation of Mortality and the Need for Operative Intervention based on Scene or Transfer Status and the Effect of SI via Regression Coefficients.
| SCENE | TRANSFER | |||
|---|---|---|---|---|
|
| ||||
| VARIABLE╲RESPONSE | Need for OR (Binomial Logistic) |
Mortality (Binomial Logistic) |
Need for OR (Binomial Logistic) |
Mortality (Binomial Logistic) |
| SI-EMS | −0.3519 | 2.956 * | 0.4148 | 9.307 |
| 95% CI | −1.683 – 0.9318 | −0.2399 – 6.475 | −1.314 – 2.150 | −2.555 – 24.27 |
|
| ||||
| ΔSI: SI-EMS to SI-DC | 1.363 ** | 2.234 | --- | --- |
| 95% CI | 0.0351 – 2.694 | −1.501 – 5.278 | --- | --- |
|
| ||||
| ΔSI: SI-EMS to SI-TX | --- | --- | 1.391 | 7.917 |
| 95% CI | --- | --- | −0.4791 – 3.322 | −4.243 – 21.52 |
|
| ||||
| ΔSI: SI-TX to SI-DC | --- | --- | 1.907 ** | 11.01 ** |
| 95% CI | --- | --- | 0.2709 – 3.654 | 1.807 – 22.06 |
|
| ||||
| Hypotension | 1.713 ** | 1.377 | 0.275 | −17.73 |
| 95% CI | 0.2353 – 3.213 | −2.229 – 4.352 | −1.428 – 1.858 | −1740 – 1740 |
|
| ||||
| Transport Time | 0.0013 | 0.0034 | 0.0002 | 0.0096 ** |
| 95% CI | −0.0010 – 0.0034 | −0.0047 – 0.0082 | −0.0017 – 0.0022 | 0.0029 – 0.0194 |
The significance is indicated by p-value<0.10 (*), p-value<0.05 (**), p-value <0.01 (†), p-value <0.001 (‡)
OR: operating room; SI: shock index, SI-EMS: emergency medical services shock index; ΔSI: change in shock index; SI-DC: shock index at definitive are center; SI-TX: shock index at transferring facility
When assessing the utilization of ICU resources, we found that ∆SI is also a significant predictor for both scene and transfer patients. In the case of scene patients, we found that a 0.1 change in ∆SI from scene to definitive care led to a 33.45% change in the odds ratio of needing an ICU stay (p<0.001). While in the case of transfer patients the change in SI from transfer to definitive care, results showed a 28.01% (p<0.01) increase in the odds ratio of an ICU stay with a 0.1 increase in SI-EMS to definitive care. Note that the only other significant predictor in identifying the need for an ICU stay was the indicator of hypotension for scene patients which showed an increase of 30.61% in the odds ratio in the need for an ICU stay for patients who presented to EMS with hypotension. When considering the number of days spent in the ICU for scene patients, scene SI and transport time were presented as significant predictors. A 0.1 increase in SI-EMS resulted in a 6.76% (p<0.01) increase in the number of days spent in the ICU, while an increase in transport time led to a 0.003% (p<0.05) decrease in the number of days in the ICU. For transfer patients, a 0.1 increase in SI-EMS led to a 14.56% (p<0.01) increase, a 0.1 increase in delta SI between EMS and definitive care led to an 8.74% (p<0.001) increase in number of ICU days, respectively. Furthermore, an increase in transport time for scene patients by one minute led to a 0.16% (p<0.001) increase in the expected number of ICU days.
The need for operative intervention was then evaluated. We found that ∆SI from EMS to definitive care and hypotension were the significant predictors of the need for OR in scene patients. A 0.1 increase in the ∆SI from EMS to definitive care resulted in a 14.60% (p<0.05) increase and if a patient was hypotension 18.68% (p<0.05) increase in log odds of the need for surgery for scene. For transfer patients the only significant predictor was the change in SI from transfer facility to definitive care where we find that a 0.1 change in SI leads to a 21.01% in the odds ratio of needing surgery.
In the case of mortality, there were increased odds for mortality for every 0.1 change in EMS SI, those changes were not deemed significant among both scene and transfer patients (p<0.1). For transfer patients, we also found that for each minute transport time increased, the odds ratio of mortality increased by 0.093% (p<0.01).
To evaluate the impact of shock index, separate from the effect of hypotension, results with hypotension omitted from each of these models can be found in supplemental digital content (SDC 1, Tables 5-7). These analyses show minor changes in the results, with the most notable being that when hypotension is omitted from the model, SI-EMS is found to be significantly related to scene patient mortality (p<0.001), and the need for ICU in both scene (p<0.001) and transfer patients (p<0.05).
Discussion:
Vital signs remain critical to the triage and treatment of trauma patients. They are an intricate portion of trauma team activation criteria and are utilized in the field to guide treatment and transport decisions.9 Multiple studies have been conducted that evaluated the predictive impact of prehospital hypotension on patient outcomes. Authors have repeatedly found that prehospital hypotension is associated with the need for operative intervention and increases in mortality after trauma.12,13 Seamon et al. demonstrated that even a single report of prehospital hypotension was associated with the presence of severe injuries that required operative intervention.14 That study urged trauma teams not to consider a single reading of hypotension as erroneous and for trauma surgeons to maintain a high index of suspicion until the patients were fully evaluated. Prehospital hypotension was further evaluated by Lipsky et al., who demonstrated that it predicted the need for operation, even if systolic blood pressure was normal on arrival to the trauma center.15
With the increased interest in utilizing shock index, a more dynamic measure encompassing multiple vital signs, authors have previously investigated its use in a rural trauma environment where transport time is routinely hours long.10 In that single-center study, they demonstrated EMS-SI was predictive of the need for transfusion, ICU care, and mortality. It has also been demonstrated that elevated SI and increasing ∆SI were superior to the presence of EMS hypotension alone. This further supports the need for trauma team activation and a high level of clinical suspicion for providers if shock index was abnormal or elevating, regardless of time in transport. The current work was designed to test these observations across multiple rural trauma systems.
This study further supports the use of SI and ∆SI in rural trauma care. By evaluating these values at each phase in a patient’s transport we demonstrate the ability to predict resource need and outcomes. Initial SI-EMS was again associated with blood transfusion in both scene and transfer patients, as well as length of ICU stay. After adjusting for EMS hypotension, the delta shock index variables provided significant insight into resource utilization for both scene and transfer patients. This study was also similar to prior work demonstrating a negative, or worsening, SI during transport for scene patients. By selectively evaluating patients most at risk for non-compressible hemorrhage and this should be expected. Transfer patients demonstrated an improvement in SI by arrival at the level 1 trauma center, underscoring the resuscitation and interventions that occur prior to arrival for definitive care. However, over one-third of these patients would require operative intervention and 9% would require blood transfusion after arrival at the Level I trauma center. This is an important observation, until a patient is fully evaluated, improving vital signs and SI-DC are not indicative of patient condition or severity of injury.
The most important findings are the association between SI and the need for operative intervention. In scene patients, delta SI and hypotension are the two biggest indicators of the need for an operation. Amongst transfer patients delta SI from transferring facility to definitive care was significantly associated with the need for an operation. In these cases, the patients’ vital sign changes exceeded the ability of EMS to resuscitate or intervene during transportation, or for the transferring facility to provide the needed care. When EMS reports an elevated SI, this presents an opportunity for the receiving trauma surgeon to alert operating room staff and mobilize necessary resources. For transferred patients, ∆SI from transferring facility to definitive care and increased time were shown to be associated with mortality. This finding is significant, given that transferred patients went nearly five and half hours from injury to definitive care. Furthermore, the results of our study do show the robustness of the conclusions as the effects of SI and ∆SI for both scene and transfer patients remain important when hypotension is accounted for or omitted from the analysis.
This study has all the usual limitations of a retrospective study. The lack of serial vital signs and reliable data from transferring facilities and EMS with regard to interventions and fluid resuscitation must also be considered. As is common in many rural trauma studies there is the potential for survivor bias. Data was not available for patients that expired prior to arrival for definitive care, this may explain why EMS-SI was not as useful in transfer patients but ∆SI was. Further study utilizing more comprehensive EMS databases, and ones linked to trauma center databases are warranted to fully describe the effect of SI and ∆SI in trauma care. Improved granularity in these datasets would allow further exploration of the effects of ∆SI and outcomes associated with different intervals of change.
Shock index and delta shock index are significant predictors for resource need, operations, and mortality after blunt torso trauma in a rural environment. These data build upon prior work and demonstrate the use of SI use across multiple rural trauma systems. Shock index was also predictive of resource utilization despite a low average ISS. Based on these results, SI and ∆SI show potential as rural triage tools as well, warranting further research. Future research will be supported by the addition of SI as portion of the national field triage guidelines to further evaluate its use during prolonged transport. With time shock index can be the common language between EMS, rural transferring facilities, and the receiving tertiary care center. Trauma surgeons in similar settings must maintain a high index of clinical suspicion if initial EMS SI was elevated, or SI has been elevating during transport.
Supplementary Material
Sources of Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942.
Footnotes
This work was presented as a podium during the 81st Annual Meeting of AAST and Clinical Congress of Acute Care Surgery, September 22, 2022, Chicago, Illinois.
The authors have no conflicts of interest to report.
References:
- 1.Census Urban and Rural Classification and Urban Area Criteria. 2010. [July 14, 2022]. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html Accessed.
- 2.Carr B, Bowman A, Wolff C, Mullen MT, Holena D, Branas CC, et al. Disparities in Access to Trauma Care in the United States: A Population-Based Analysis. Injury. 2017. Feb;48(2):332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashmi ZG, Jarman MP, Uribe-Leitz T, Goralnick E, Newgard CD, Salim A, et al. Access Delayed Is Access Denied: Relationship Between Access to Trauma Center Care and Pre-Hospital Death. J Am Coll Surg 2019. Jan;228(1):9–20. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez RP, Cummings G, Mulekar M, Rodning CB. Increased Mortality in Rural Vehicular Trauma: Identifying Contributing Factors Through Data Linkage. J Trauma Inj Infect Crit Care 2006. Aug;61(2):404–409. [DOI] [PubMed] [Google Scholar]
- 5.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: Geographic disparities in trauma mortality. Surgery 2016. Dec;160(6):1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph B, Haider A, Ibraheem K, Kulvatunyou N, Tang A, Azim A, et al. Revitalizing Vital Signs: The Role of Delta Shock Index. Shock 2016. Sep;46(3S):50–54. [DOI] [PubMed] [Google Scholar]
- 7.Schroll R, Swift D, Tatum D, Couch S, Heaney JB, Llado-Farrulla M, et al. Accuracy of shock index versus ABC score to predict need for massive transfusion in trauma patients. Injury 2018. Jan;49(1):15–19. [DOI] [PubMed] [Google Scholar]
- 8.Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the Shock Index in Predicting Mortality in Traumatically Injured Patients. J Trauma Inj Infect Crit Care 2009. Dec;67(6):1426–1430. [DOI] [PubMed] [Google Scholar]
- 9.Newgard CD, Fischer PE, Gestring M, Michaels HN, Jurkovich GJ, Lerner EB, et al. National guideline for the field triage of injured patients: Recommendations of the National Expert Panel on Field Triage, 2021. J Trauma Acute Care Surg 2022. Aug;93(2):E49–E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schellenberg M, Strumwasser A, Grabo D, Clark D, Matsushima K, Inaba K, et al. Delta Shock Index in the Emergency Department Predicts Mortality and Need for Blood Transfusion in Trauma Patients. Am Surg 2017. Oct;83(10):1059–62. [DOI] [PubMed] [Google Scholar]
- 11.Bardes JM, Price BS, Adjeroh DA, Doretto G, Wilson A. Emergency medical services shock index is the most accurate predictor of patient outcomes after blunt torso trauma. J Trauma Acute Care Surg 2022. Mar;92(3):499–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bilello JF, Davis JW, Lemaster D, Townsend RN, Parks SN, Sue LP, et al. Prehospital hypotension in blunt trauma: Identifying the “crump factor.” J Trauma - Inj Infect Crit Care 2011. May;70(5):1038–1042. [DOI] [PubMed] [Google Scholar]
- 13.Franklin GA, Boaz PW, Spain DA, Lukan JK, Carrillo EH, Richardson JD. Prehospital Hypotension as a Valid Indicator of Trauma Team Activation. J Trauma Acute Care Surg 2000. Jun;48(6). [DOI] [PubMed] [Google Scholar]
- 14.Seamon MJ, Feather C, Smith BP, Kulp H, Gaughan JP, Goldberg AJ. Just one drop: The significance of a single hypotensive blood pressure reading during trauma resuscitations. J Trauma - Inj Infect Crit Care 2010. Jun;68(6):1289–1294. [DOI] [PubMed] [Google Scholar]
- 15.Lipsky AM, Gausche-Hill M, Henneman PL, Loffredo AJ, Eckhardt PB, Cryer HG, et al. Prehospital Hypotension is a Predictor of the Need For an Emergent, Therapeutic Operation in Trauma Patients With Normal Systolic Blood Pressure in the Emergency Department. J Trauma Acute Care Surg 2006. Nov;61(5). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


