Abstract
Background:
Cardiac rehabilitation (CR) is scantly available in Iran, although it is the cost-benefit strategy in cardiac patients, It has not been established how CR is delivered within Iran. This study aimed to determine: (a) availability, density and unmet need for CR, and (b) nature of CR services in Iran by province.
Materials and Methods:
In this cross-sectional sub-study of the global CR audit, program availability was determined through cardiovascular networks. An online survey was then disseminated to these programs in June 2016–2017 which assessed capacity and characteristics; a paper-based survey was disseminated in 2018 to nonresponding and any new programs. CR density and need was computed based on annual incidence of acute myocardial infarction (AMI) in each province.
Results:
Of the 31 provinces, 12 (38.7%) had CR services. There were 30 programs nationally, all in capital cities; of these, programs in 9 (75.0%) provinces, specifically 22 (73.3%) programs, participated. The national CR density is 1 spot per 7 incident AMI patients/year. Unmet need is greatest in Khuzestan, Tehran and west Azerbaijan, with 44,816 more spots needed/year. Most programs assessed cardiovascular risk factors, and offered comprehensive services, delivered by a multi-disciplinary team, comprised chiefly of nurses, dietitians and cardiologists. Median dose is 14 sessions/program in supervised programs. A third of programs offered home-based services.
Conclusion:
Where programs do exist in IRAN, they are generally delivered in accordance with guidelines. Therefore, we must increase capacity in CR services in all provinces to improve secondary prevention services.
Keywords: Capacity building, cardiac rehabilitation, international health, Iran, quality of health care
INTRODUCTION
Cardiovascular diseases (CVD) are the most prevalent noncommunicable disease and the leading cause of death worldwide.[1] In 2017, CVD affected 126.5 million people worldwide.[2] According to the Global Burden of Disease study, CVD is among the ten leading causes of disability. Specifically, in 2019, the percentage of disability-adjusted life years (DALYs) due to ischemic heart disease (IHD) was 7.2 (6.5–7.9); that ranks second worldwide.[3]
Iran in particular is experiencing major demographic transitions, such that major causes of morbidity and mortality have changed.[4] The first National Burden of Disease study indicated that 58% of DALYs were due to noncommunicable diseases such as CVD in 2003.[5] With more than 9000 cases of CVD per 100,000 persons, Iran is among the countries with the highest CVD rates in the world.[6,7] Therefore, it is necessary to limit the health, economic and social effects of CVDs. Cardiac rehabilitation (CR) is the main secondary prevention strategy recommended by the World Health Organization.[8]
Studies show that mortality and morbidity of patients using CR services is 20% lower than that among patients not using these services.[9] These programs offer education and structured exercise to also improve the morbidity, quality of life, functional capacity and cardiovascular risk factors of participating patients.[10,11]
Despite the proven advantages of CR, studies show that access to these services is limited, particularly in low and middle-income countries (LMICs) such as Iran. A review of the literature revealed that of 138 LMICs, only 55 (39.3%) had any CR services.[12] In the Eastern Mediterranean region (EMR) specifically, even where available, the density was low, with only one CR “spot” for every 104 incident IHD patient annually.[13]
In 2016/2017, the International Council of Cardiovascular Prevention and Rehabilitation (ICCPR) undertook a global audit of CR (https://globalcardiacrehab.com/Global-CR-Program-Survey). Fourteen of an estimated 34 programs in Iran participated; data on availability and nature of services on a national level has been reported in several publications stemming from the audit, including one on the EMR.[12,13,14,15] Since that time, several CR programs have closed in Iran, and we attempted to collect data from 8 additional programs (that did not participate in on line survey) by phone or in person for an updated information's of CR services in the country.
No previous research has evaluated the nature of CR across Iranian provinces to our knowledge. The purpose of this paper is to summarize: (1) the availability and distribution of CR in Iran, as well as (2) the nature of services delivered, both by province.
MATERIALS AND METHODS
Ethics
Ethical approval was secured from the Ethics Committee of Isfahan Cardiovascular Research Center (Iran; 95116), York University (Toronto, Canada; e2014-078) and Mayo Clinic's Institutional Review Board (Rochester, United States; 16-001110). Informed consent was received from the participants.
Design and procedure
This is a cross-sectional sub-study of ICCPR's global CR audit. Full methodological details are reported elsewhere.[14,15]
In brief, in 2016 the availability of CR was determined in the world; in Iran, this was done with the support of the CR Research Center of Isfahan Cardiovascular Research Institute, the Iranian Network of Cardiovascular Research and Iranian Heart Foundation. An online survey (available as supplementary material 2 here:[14]) was administered to all identified programs to assess program capacity, personnel and the nature of services delivered. As outlined below, further data collection ensued in Iran subsequent to the global audit in 2018, using a paper-based version of the same survey.
Sample
The population comprised all CR programs of Iran. The inclusion criteria were programs that offered: (1) initial assessment, (2) structured exercise, and (3) at least one other strategy to control CV risk factors.
First, a list of all CR programs in Iran was created in 2015 after contacting the deputy of health of all medical science universities. Thirty-four CR programs were identified. After contacting all these programs, it was determined that 4 had closed.
Then in 2016, the manager of each program was E-mailed the link to the survey in English (REDCap), which was preceded by a consent form. Of the 30 CR programs, 14 programs in the cities of Isfahan, Kerman, Kermanshah, Mashhad, Shiraz, Tabriz, Tehran, and Yazd completed the online questionnaire. Results from these programs at a national level are reported in the main ICCPR global audit publications, as summarized in the results section.
After phone calls and visits by a clinician-investigator in 2017/2018, another 8 programs in the cities of Sari (1 program), Mashhad (1 program) and Tehran (6 programs) also completed the questionnaires on paper. Therefore, in total, 22/30 (73.3%) CR programs participated in this study. The 8 programs that did not participate in this study were in the provinces of Tehran (2 programs), Hamedan (1 program), East Azerbaijan (1 program), Qom (1 program), Mazandaran (1 program), Fars (1 program), And Qazvin (1 program); median annual program capacity was used to estimate CR density and unmet need in these provinces.
Measures
With regard to the first objective, provincial and national CR capacity were computed by multiplying the median number of patients a program could serve annually (program-reported in survey described below) among the responding programs in a given province or the country respectively, multiplied by the total number of programs in that jurisdiction. To compute density at a national level, IHD incidence estimates from the Global Burden of Disease study were used.[16] Provincial incidence of myocardial infarction was extracted from North Khorasan (2012 data closest to time our data collected).[17] Unmet need was computed as jurisdictional IHD incidence minus capacity.
Development of the survey is described in detail elsewhere.[14] The following variables were assessed: (i) who funds the program (i.e., private sources such as healthcare insurance, public sources such as government, or a combination of these sources [i.e., hybrid]), (ii) the type (e.g., myocardial infarction, as well as noncardiac indications) and number of patients served per session (as well as staff-to-patient ratio), (iii) the number and types of healthcare professionals on the CR team (part-time staff were counted as 0·5), (iv) dose of CR (in hours; i.e., sessions per week, duration in weeks, duration of exercise sessions in minutes); (v) core components delivered (i.e., initial assessment [including risk factors assessed and type of functional capacity test], risk stratification, supervised exercise, patient education, risk factor management, nutrition counselling, stress management, smoking cessation, prescription of medication, and communication with a primary healthcare provider), (vi) whether the program offers alternative CR models (i.e., home or community-based programs, or hybrid models where patients transition from supervised to unsupervised settings), and (vii) barriers to delivery.
Statistical analyses
Statistical Package for the Social Sciences version 21, Armonk, NY: IBM Corp., USA was used for analysis. All initiated surveys were included. The number of responses for each question varied due to missing data (e.g., respondent did not answer a question due to lack of willingness or potential inapplicability, use of skip logic). Descriptive statistics such as means with standard deviation and frequencies with percentages as applicable were used to characterize volume, capacity, density, as well other closed-ended items in the survey (e.g., funding sources, core components delivered, and healthcare professionals on the CR team). All open-ended responses were coded/categorized.
RESULTS
Response rate/cardiac rehabilitation availability
Of the 31 provinces of Iran, 12 (38.7%) provinces had CR programs; among these 12, CR programs in 9 (75.0% provincial response rate) provinces participated in this study [Table 1]. Of the 30 CR programs across all Iranian provinces, 22 (73.3% program response rate) participated, in Isfahan, Tehran, Fars, East Azarbaijan, Razavi Khorasan, Kerman, Kermanshah, Mazandaran and Yazd (none outside of capitals).
Table 1.
Cardiac rehabilitation availability, response rate and density by province in Islamic republic of Iran
| Province | Population (persons) | Number of CR programs (percentage of all) | Number of programs participating in survey (percentage in province) | Median annual capacity/program | Provincial CR capacity (number spots/year) | Myocardial infarction incidence/100,000 | CR density* | Unmet need |
|---|---|---|---|---|---|---|---|---|
| Alborz | 2,712,400 | 0 | - | 0 | 0 | 73.2 | 0 | 1985 |
| Ardabil | 1,270,420 | 0 | - | 0 | 0 | 91.0 | 0 | 1156 |
| West Azerbaijan | 3,265,219 | 0 | - | 0 | 0 | 108.2 | 0 | 3533 |
| East Azarbaijan | 3,909,652 | 3 (10.0) | 2 (66.7) | 120 | 360 | 35.4 | 3.84 | 1024 |
| Bushehr | 1,163,400 | 0 | - | 0 | 0 | 39.9 | 0 | 464 |
| Chaharmahal and Bakhtiari | 947,763 | 0 | - | 0 | 0 | 85.5 | 0 | 810 |
| Iilam | 580,158 | 0 | - | 0 | 0 | 43.3 | 0 | 251 |
| Isfahan | 5,120,850 | 3 (10.0) | 3 (100.0) | 360 | 1080 | 45.5 | 2.16 | 1080 |
| Fars | 4,851,274 | 2 (6.66) | 1 (50.0) | 300 | 600 | 49.0 | 4.0 | 600 |
| Ghazvin | 1,273,761 | 1 (3.33) | 0 | 263‡ | 263 | 78.8 | 3.81 | 741 |
| Gilan | 2,530,696 | 0 | - | 0 | 0 | 92.0 | 0 | 2328 |
| Golestan | 1,868,619 | 0 | - | 0 | 0 | 69.1 | 0 | 1291 |
| Hamadan | 1,758,268 | 1 (3.33) | 0 | 263‡ | 263 | 51.5 | 3.44 | 643 |
| Hormozgan | 1,776,415 | 0 | - | 0 | 0 | 34.5 | 0 | 613 |
| Kerman | 3,164,718 | 1 (3.33) | 1 (100.0) | 275 | 275 | 118.5 | 6.82 | 275 |
| Kermnanshah | 1,952,434 | 1 (3.33) | 1 (100.0) | 263‡ | 263 | 67.7 | 5.03 | 1059 |
| South Khorasan | 768,898 | 0 | - | 0 | 0 | 76.5 | 0 | 588 |
| Razavi Khorasan | 6,434,501 | 3 (10.0) | 3 (100.0) | 250 | 750 | 44.9 | 3.85 | 2139 |
| North Khorasan | 863,092 | 0 | - | 0 | 0 | 126.7 | 0 | 1094 |
| Khuzestan | 4,710,509 | 0 | - | 0 | 0 | 108.1 | 0 | 5092 |
| Kohgiluyeh and Boyer-Ahmad | 713,052 | 0 | - | 0 | 0 | 61.5 | 0 | 439 |
| Kurdistan | 1,603,011 | 0 | - | 0 | 0 | 39.1 | 0 | 627 |
| Lorestan | 1,760,649 | 0 | - | 0 | 0 | 87.9 | 0 | 1548 |
| Markazi | 1,429,475 | 0 | - | 0 | 0 | 76.7 | 0 | 1096 |
| Mazandaran | 3,283,582 | 2 (6.66) | 1 (50.0) | 140 | 280 | 85.9 | 10.07 | 2581 |
| Qom | 1,292,283 | 1 (3.33) | 0 | 263‡ | 263 | 19.8 | 0.97 | - |
| Semnan | 702,360 | 0 | - | 0 | 0 | 119.0 | 0 | 836 |
| Sistan and Baluchestan | 2,775,014 | 0 | - | 0 | 0 | 32.7 | 0 | 907 |
| Tehran | 13,267,637 | 11 (36.7) | 9 (81.9) | 295 | 3245 | 49.9 | 0.03 | 3376 |
| Yazd | 1,138,533 | 1 (3.33) | 1 (100.0) | 250 | 250 | 121.7 | 5.54 | 1136 |
| Zanjan | 1,057,461 | 0 | - | 0 | 0 | 34.0 | 0 | 360 |
| Total/National | 81,211,323 | 30 (100) | 22 (73.33) | 263 | 7890 | 64.9 | 6.68 | 44,816 |
*Number of CR spots per x patients per year, ‡Province without a response, capacity estimated based on national median program capacity multiplied by number of programs in that province-not applicable. CR=Cardiac rehabilitation
Figure 1 and Table 1 show the distribution of CR programs in Iran by province. CR capacity for individual patients by province is also shown in Table 1. As shown, there were no more than 3 programs in any province with CR except Tehran.
Figure 1.
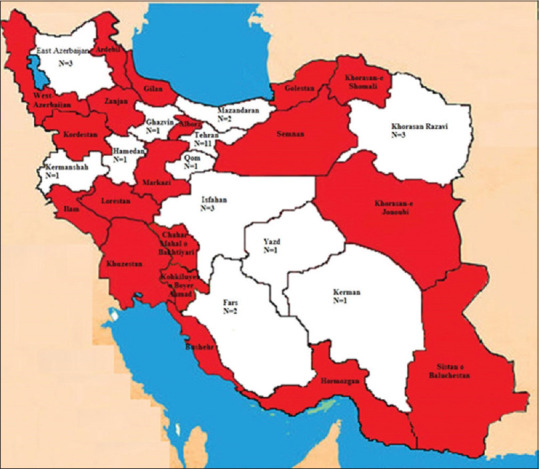
Distribution of CR programs in Iran by province
The global audit revealed a CR density of 1 spot per 15 IHD patients/year, ranking Iran at 20th globally.[15] It was estimated that 219,007 more CR spots are needed in Iran each year to treat all incident IHD patients.[12] Used capacity is also reported elsewhere.[13] Density and unmet need based on myocardial infarction incidence by province is shown in Table 1; Based on this, the national Iranian CR density is 1 spot per 7 myocardial infarction patients, with 44,816 more spots needed per year to treat these patients alone.
Figure 2 shows the barriers to broader delivery of CR in Iran. These results indicate that key barriers include lack of patient referral, lack of financial resources, and lack of human resources in CR programs. Respondents were asked to list other barriers; transportation and long travel distance for patients were cited.
Figure 2.
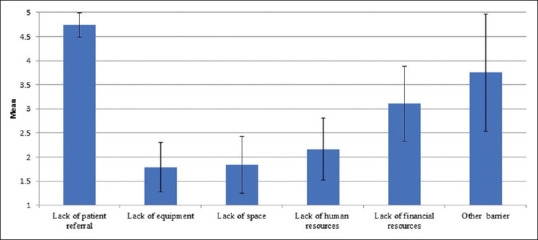
Barriers to broader delivery of cardiac rehabilitation
Nature of cardiac rehabilitation services in Iran
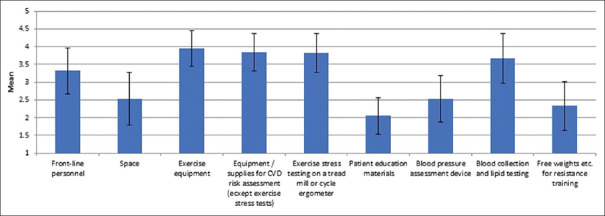
Figure 3 shows the perceived costs of elements required for CR delivery. Results show that the highest expenses were related to exercise equipment, cardiovascular risk assessment, exercise stress testing, blood collection and human resources. On the other hand, costs for space to the programs were low. Costs to deliver CR and reimbursement sources at a national level are compared to other countries internationally elsewhere.[13,18]
Figure 3.
Degree of expensiveness of elements of cardiac rehabilitation delivery in Iran, n=22. Note: scores range from 1 “free” to 5 “very expensive”
Accepted cardiac indications by country are reported elsewhere[14] as well as non-cardiac indications served.[13] Table 2 shows risk factors evaluated in CR programs by province. As displayed, almost all CR programs evaluate obesity, hypertension, hyperlipidemia, poor diet, depression/anxiety, and physical inactivity. However, other risk factors such as obstructive sleep apnea, and body composition are less likely to be evaluated. Risk factors assessed by EMR country is shown elsewhere.[13]
Table 2.
Cardiovascular risk factor evaluation in Iranian cardiac rehabilitation programs by province
| Isfahan (n=3), n (%) | Kerman (n=1), n (%) | Kermanshah (n=1), n (%) | Razavi Khorasan (n=3), n (%) | Mazandaran (n=1), n (%) | Fars (n=1), n (%) | East Azarbaijan (n=2), n (%) | Tehran (n=9), n (%) | Yazd (n=1), n (%) | Total (n=22), n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Body mass index | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 22 (100.0) |
| Cholesterol fractions (HDL-C, LDL-C) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 22 (100.0) |
| Triglycerides | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 22 (100.0) |
| Total cholesterol | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (66.7) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 21 (95.5) |
| Blood pressure | 2 (66.7) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 21 (95.0) |
| Diet | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 8 (88.9) | 1 (100.0) | 21 (95.5) |
| Depression/anxiety | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 8 (88.9) | 1 (100.0) | 21 (95.5) |
| Physical inactivity | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 7 (77.8) | 1 (100.0) | 20 (91.0) |
| Tobacco use | 2 (66.7) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 7 (77.8) | 1 (100.0) | 19 (86.0) |
| HbA1c for diabetic patients | 2 (66.7) | 0 | 0 | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 9 (100.0) | 1 (100.0) | 19 (86.0) |
| Harmful use of alcohol | 2 (66.7) | 0 | 1 (100.0) | 2 (66.7) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 8 (88.9) | 0 | 17 (77.0) |
| Blood glucose for nondiabetic patients | 3 (100.0) | 1 (100.0) | 1 (100.0) | 2 (66.7) | 1 (100.0) | 1 (100.0) | 2 (100.0) | 3 (33.3) | 1 (100.0) | 15 (68.0) |
| Being sedentary | 2 (66.7) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 1 (50.0) | 4 (44.4) | 1 (100.0) | 15 (68.0) |
| Body composition | 2 (66.7) | 0 | 0 | 0 | 1 (100.0) | 0 | 0 | 7 (77.8) | 1 (100.0) | 11 (50.0) |
| Waist circumference | 2 (66.7) | 0 | 1 (100.0) | 1 (33.3) | 1 (100.0) | 1 (100.0) | 1 (50.0) | 3 (33.3) | 1 (100.0) | 10 (45.0) |
| Hip circumference | 2 (66.7) | 0 | 1 (100.0) | 0 | 1 (100.0) | 1 (100.0) | 1 (50.0) | 3 (33.3) | 1 (100.0) | 10 (45.0) |
| Sleep apnea | 1 (33.3) | 0 | 0 | 0 | 1 (100.0) | 0 | 0 | 5 (55.5) | 1 (100.0) | 8 (36.0) |
HDL-C: High-density lipoprotein cholesterol; LDL-C: Low-density lipoprotein cholesterol; HbA1c: Glycated hemoglobin
As can be seen in Table 3, the most common type of healthcare specialists on CR teams in Iran are nurses, nutrition experts, and cardiologists. Most programs in all provinces had specialist physicians, nurses and dietitians. In Kerman, there was no exercise specialist/physiotherapist or mental healthcare provider. In almost have of provinces, programs had no administrative assistance. For comparative purposes, healthcare providers on the CR team is shown in every country, by region, elsewhere.[14]
Table 3.
Healthcare professionals on cardiac rehabilitation teams in Iran, by province
| Isfahan (n=3), n (%) | Kerman (n=1), n (%) | Kermanshah (n=1), n (%) | Razavi Khorasan (n=3), n (%) | Mazandaran (n=1), n (%) | Fars (n=1), n (%) | East Azarbayijan (n=2), n (%) | Tehran (n=9), n (%) | Yazd (n=1), n (%) | Total (n=22), n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Cardiologist | 2 (67.0) | 0 | 1 (100.0) | 3 (100.0) | 0 | 1 (100.0) | 2 (100.0) | 6 (67.0) | 1 (100.0) | 16 (72.7) |
| Physiatrist (physical medicine and rehab) | 1 (33.0) | 0 | 0 | 3 (100.0) | 0 | 0 | 1 (50.0) | 5 (55.0) | 1 (100.0) | 11 (50.0) |
| Sports medicine physician | 2 (67.0) | 1 (100.0) | 1 (100.0) | 2 (67.0) | 1 (100.0) | 1 (100.0) | 0 | 4 (44.0) | 0 | 12 (54.5) |
| Nurse | 3 (100.0) | 1 (100.0) | 1 (100.0) | 3 (100.0) | 0 | 1 (100.0) | 2 (100.0) | 8 (89.0) | 1 (100.0) | 20 (91.0) |
| Nurse practitioner | 0 | 1 (100.0) | 1 (100.0) | 3 (100.0) | 1 (100.0) | 1 (100.0) | 0 | 3 (33.0) | 1 (100.0) | 11 (50.0) |
| Physiotherapist | 1 (33.0) | 0 | 0 | 2 (67.0) | 1 (100.0) | 0 | 2 (100.0) | 6 (67.0) | 1 (100.0) | 13 (59.0) |
| Exercise specialist/kinesiologist | 1 (33.0) | 0 | 1 (100.0) | 2 (67.0) | 0 | 1 (100.0) | 0 | 4 (44.0) | 0 | 9 (41.0) |
| Psychiatrist | 1 (33.0) | 0 | 0 | 2 (67.0) | 1 (100.0) | 0 | 2 (100.0) | 6 (67.0) | 1 (100.0) | 13 (59.0) |
| Psychologist | 1 (33.0) | 0 | 1 (100.0) | 2 (67.0) | 0 | 1 (100.0) | 0 | 6 (67.0) | 1 (100.0) | 12 (54.5) |
| Social worker | 0 | 0 | 0 | 2 (67.0) | 0 | 0 | 1 (50.0) | 3 (33.0) | 1 (100.0) | 7 (32.0) |
| Dietitian | 2 (67.0) | 1 (100.0) | 1 (100.0) | 2 (67.0) | 1 (100.0) | 1 (100.0) | 1 (50.0) | 8 (89.0) | 1 (100.0) | 18 (81.8) |
| Pharmacist | 1 (33.0) | 0 | 0 | 0 | 0 | 0 | 0 | 3 (33.0) | 0 | 4 (18.0) |
| Community health worker | 0 | 0 | 0 | 1 (33.0) | 0 | 0 | 1 (50.0) | 1 (11.0) | 0 | 3 (14.0) |
| Administrative, assistant/secretary | 2 (67.0) | 0 | 0 | 1 (33.0) | 0 | 0 | 2 (100.0) | 7 (78.0) | 1 (100.0) | 13 (59.0) |
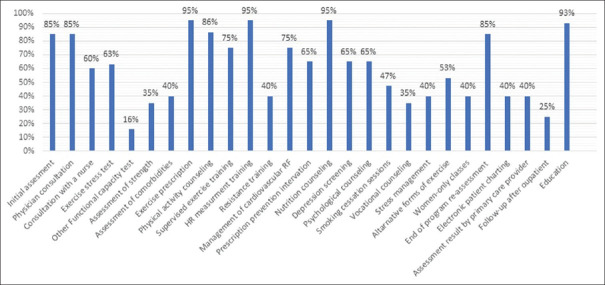
Figure 4 shows the main components of CR that are offered in the programs. The results show that generally all indicators and components of are offered in most CR programs. Most common core components delivered at a national level are compared to other countries and regions elsewhere[14] and Table 3[13].
Figure 4.
Core components of cardiac rehabilitation provided in Iranian programs, n=22
Some characteristics of supervised CR programs in Iran are shown in Table 4 by province. CR dose is compared to other countries internationally elsewhere[19] (14 sessions/programs which is ranked 13th globally for Eastern Mediterranean specifically[13]). Delivery of alternative models at a national level (i.e., 35.7% in Iran offer home-based) is also compared to other countries elsewhere,[20] as is availability of women-only services specifically.[21]
Table 4.
Characteristics of cardiac rehabilitation delivery in Iran, by province
| Isfahan (n=3), n (%) | Kerman (n=1), n (%) | Kermanshah (n=1), n (%) | Razavi Khorasan (n=3), n (%) | Mazandaran (n=1), n (%) | Fars (n=1), n (%) | East Azarbayijan (n=2), n (%) | Tehran (n=9), n (%) | Yazd (n=1), n (%) | Total (n=22), n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of CR programs | 3 | 1 | 1 | 3 | 1 | 1 | 2 | 9 | 1 | 22 |
| CR wait time (weeks) | 5.50±2.12 | 4.00±0.00 | 8.00±0.00 | 3.50±0.87 | 4.00±0.00 | 4.00±0.00 | 3.75±1.06 | 2.75±0.90 | 3.00±0.00 | 3.94±1.06 |
| Cost to serve 1 patient, if they complete the program$ | 194.00±121.25 | 110.00±0.00 | 110.00±0.00 | 143.33±66.58 | 110.00±0.0 | 110.00±0.00 | 215.00±0.00 | 451.22±346.70 | 110.00±0.00 | 291.65±274.76 |
| Number of education sessions | 4.50±2.12 | 1.50±0.00 | 12.00±0.00 | 9.0 0±9.53 | 3.00±0.00 | 9.00±0.00 | 3.00±0.00 | 2.44±1.42 | 10.00±0.00 | 4.52±4.61 |
| How many minutes on average for each education session (min) | 42.50±3.53 | 55.00±0.00 | 60.00±0.00 | 45.00±39.69 | 30.00±0.00 | 15.00±0.00 | 30.00±0.00 | 25.00±32.69 | 30.00±0.00 | 32.62±27.05 |
| CR program duration (weeks) | 13.00±9.900 | 4.00±0.00 | 8.00±0.00 | 6.67±2.31 | 12.00±0.00 | 12.00±0.00 | 9.50±3.54 | 7.75±2.66 | 12.0±0.00 | 8.58±3.89 |
| CR sessions per week | 3.00±0.00 | 3.00±0.00 | 3.00±0.00 | 3.00±0.00 | 2.00±0.00 | 3.00±0.00 | 2.25±1.06 | 2.85±0.37 | 3.00±0.00 | 2.81±0.46 |
| Number of patients/exercise session | 9.50±3.54 | 5.00±0.00 | 16.00±0.00 | 7.80±3.53 | 5.00±0.00 | 8.50±3.50 | 5.50±0.71 | 4.57±3.36 | 6.00±0.00 | 6.41±3.84 |
| Duration of each exercise session (min/session)* | 82.50±10.61 | 55.00±0.00 | 120.00±0.0 | 63.33±35.12 | 90.0±0.00 | 90.0±0.60 | 90.0±42.43 | 61.43±20.35 | 60.00±0.00 | 71.67±26.35 |
| Maximum number of patients per exercise session (patient/session) | 13.00±1.41 | 6.00±0.00 | 20.00±0.00 | 10.33±2.89 | 25.00±0.00 | 12.00±0.00 | 10.00±0.00 | 6.00±4.36 | 10.00±0.00 | 9.61±5.94 |
| Staff-to-patient ratio during supervised exercise | 3.50±0.71 | 2.00±0.00 | 5.00±0.00 | 1.67±1.15 | 1.00±0.00 | 3.50±0.00 | 2.50±0.20 | 4.77±4.50 | 2.00±0.00 | 3.50±3.30 |
$Purchasing power parity 2016, (http://eppi.ioe.ac.uk/costconversion/default.aspx), Mean±SD shown
DISCUSSION
Despite the World Health Organization's recognition of the important role of CR for the secondary prevention of CVD,[8] CR availability is limited[15] and little was known about what is implemented within Iran. This is the first study to provide a comprehensive description of CR availability and the nature of services delivered within Iran. The results indicated that despite the high incidence of CVD,[5] only about a third of the provinces in Iran have any CR programs; there are 19 provinces without CR. Unmet need is greatest in Khuzestan, Tehran and west Azerbaijan. Barriers to broader delivery reported by programs are consistent with other countries; barriers in referring providers have also been elucidated in Iran.[22,23]
Along with the need for an increased number of CR programs, the data suggests there is room to increase the number of patients served in each program in Iran.[13] Given a full third of programs offered alternative models, this could be used to reach patients living in smaller cities and rural areas, which have no programs in Iran. Use of novel technologies such as remote monitoring and telehealth could extend access to these programs outside capital cities.[24] In particular, Iran has implemented hybrid programs at some programs.[25] Whether this could be a model to expand capacity, and particularly to serve patients outside capital cities warrants further research.
It is fortunate that CR is reimbursed through healthcare insurance,[26,27] which hopefully could be exploited to increase capacity. To increase capacity nationally, implementation of simplified rehabilitation in community or primary health care settings could help, as could smartphone and virtual forms of CR as outlined above, initiation of financial incentives (e.g., payment of acute care centers for all rehabilitated patients), and addressing existing barriers (e.g., systematic patient referral, awareness campaigns).
The composition of the CR teams was suitably diverse for providing comprehensive preventive advice and secondary care services.[28] In general, in Iran most programs are managed by physicians, in line with other regions. More investigation of the most efficient mix of professionals to cover each core component safely warrants further investigation.
Programs accepted guideline-indicated patients. Risk factors were comprehensively assessed. Programs were comprehensive, in accordance with guideline recommendations. Dose was somewhat low, but through hybrid delivery this could potentially be augmented.
When compared to the EMR more broadly,[13] Iran has the most programs of any country, and indeed was the first to open CR (in 1994). Similar to Iran, over 100,000 more CR spots are needed per year also in Pakistan Egypt, Morocco, Iraq and Sudan. There is variation in the region in terms of which healthcare professions can refer patients to CR. While there are little data from CR programs in EMR countries other than Iran, there does seem to be consistency in the size of CR teams and the number of components delivered. The only other country than Iran to offer CR in alternative settings in the EMR was Pakistan.
There were several limitations in our study. First, despite our extensive search using various sources and methods, it is possible that some Iranian CR programs could have been missed. However, even if 20% to 30% of the CR programs were missed, the conclusion that there is insufficient distribution and density of CR programs in Iran will not change. Second, provincial and program response rates were high, but we do not know why nonresponding programs were unwilling to participate, and therefore there could be bias in the findings. Third, data about each program was gathered from one individual, and it is possible that what was reported does not reflect the experience of the rest of staff members in CR programs. Moreover, staff responding to the paper survey may have responded in a more socially-desirable way than those completing the online survey, biasing results towards higher-quality delivery than reality. Finally, the sample size is very small, particularly by province, and hence the reader is cautioned against over-interpretation. This is the only and first data available, however.
CONCLUSION
The results of the current study indicate misdistribution and insufficient density of CR programs across all provinces in Iran, which limits access to these services. A significant increase in the number of CR programs in Iran is needed, given the country can serve 7890 incident patients per year yet needs spaces for 44,816 more; greatest unmet need is in Khuzestan. Where programs do exist however, they are generally in accordance with guidelines, demonstrating that if we work together to augment capacity we could address the great burden of CVD in our country.[10]
Financial support and sponsorship
This research was supported by a grant from York University's Faculty of Health, Canada.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This research was supported by a grant from York University's Faculty of Health, Canada.
The authors acknowledge the sincere cooperation of the honorable ICCPR and their global CR program audit/survey through which we identified and reached surveyed programs in Iran. We are also grateful to our colleagues at CR research centers in the cities of Iran, and the Iranian Network of Cardiovascular Research. We are also grateful to the staff of the Cardiac Rehabilitation Research Center of Cardiovascular Research Institute and the individuals participating in this research.
REFERENCES
- 1.WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7:e1332–45. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai H, Much AA, Maor E, Asher E, Younis A, Xu Y, et al. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990-2017: Results from the Global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes. 2022;8:50–60. doi: 10.1093/ehjqcco/qcaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kiani S, Bayanzadeh M, Tavallaee M, Hogg RS. The Iranian population is graying: Are we ready? Arch Iran Med. 2010;13:333–9. [PubMed] [Google Scholar]
- 5.Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metr. 2009;7:9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shams-Beyranvand M, Farzadfar F, Naderimagham S, Tirani M, Maracy MR. Estimation of burden of ischemic heart diseases in Isfahan, Iran, 2014: Using incompleteness and misclassification adjustment models. J Diabetes Metab Disord. 2017;16:12. doi: 10.1186/s40200-017-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talaei M, Sarrafzadegan N, Sadeghi M, Oveisgharan S, Marshall T, Thomas GN, et al. Incidence of cardiovascular diseases in an Iranian population: The Isfahan Cohort Study. Arch Iran Med. 2013;16:138–44. [PubMed] [Google Scholar]
- 8.World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013-2020. Geneva: World Health Organization; 2014. [Last accessed on 2020 Dec 11]. Available from: https://www.who.int/nmh/publications/ncd-action-plan/en/ [Google Scholar]
- 9.Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD007130. doi: 10.1002/14651858.CD007130.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grace SL, Turk-Adawi KI, Contractor A, Atrey A, Campbell N, Derman W, et al. Cardiac rehabilitation delivery model for low-resource settings. Heart. 2016;102:1449–55. doi: 10.1136/heartjnl-2015-309209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kabboul NN, Tomlinson G, Francis TA, Grace SL, Chaves G, Rac V, et al. Comparative effectiveness of the core components of cardiac rehabilitation on mortality and morbidity: A systematic review and network meta-analysis. J Clin Med. 2018;7:514. doi: 10.3390/jcm7120514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pesah E, Turk-Adawi K, Supervia M, Lopez-Jimenez F, Britto R, Ding R, et al. Cardiac rehabilitation delivery in low/middle-income countries. Heart. 2019;105:1806–12. doi: 10.1136/heartjnl-2018-314486. [DOI] [PubMed] [Google Scholar]
- 13.Turk-Adawi K, Supervia M, Pesah E, Lopez-Jimenez F, Afaneh J, El-Heneidy A, et al. Availability and delivery of cardiac rehabilitation in the Eastern Mediterranean Region: How does it compare globally? Int J Cardiol. 2019;285:147–53. doi: 10.1016/j.ijcard.2019.02.065. [DOI] [PubMed] [Google Scholar]
- 14.Supervia M, Turk-Adawi K, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Nature of cardiac rehabilitation around the globe. EClinicalMedicine. 2019;13:46–56. doi: 10.1016/j.eclinm.2019.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. 2019;13:31–45. doi: 10.1016/j.eclinm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.University of Washington, Institute for Health Metrics and Evaluation (IHME) Global Burden of Disease Results. Seattle, WA: IHME; 2016. [Last accessed on 2017 Dec 06]. Available from: http://ghdx.healthdata.org/gbd-results -tool . [Google Scholar]
- 17.Ahmadi A, Soori H, Mehrabi Y, Etemad K, Samavat T, Khaledifar A. Incidence of acute myocardial infarction in Islamic Republic of Iran: A study using national registry data in 2012. East Mediterr Health J. 2015;21:5–12. doi: 10.26719/2015.21.1.5. [DOI] [PubMed] [Google Scholar]
- 18.Moghei M, Pesah E, Turk-Adawi K, Supervia M, Jimenez FL, Schraa E, et al. Funding sources and costs to deliver cardiac rehabilitation around the globe: Drivers and barriers. Int J Cardiol. 2019;276:278–86. doi: 10.1016/j.ijcard.2018.10.089. [DOI] [PubMed] [Google Scholar]
- 19.Chaves G, Turk-Adawi K, Supervia M, Santiago de Araújo Pio C, Abu-Jeish AH, Mamataz T, et al. Cardiac rehabilitation dose around the world: Variation and correlates. Circ Cardiovasc Qual Outcomes. 2020;13:e005453. doi: 10.1161/CIRCOUTCOMES.119.005453. [DOI] [PubMed] [Google Scholar]
- 20.Lima de Melo Ghisi G, Pesah E, Turk-Adawi K, Supervia M, Lopez Jimenez F, Grace SL. Cardiac rehabilitation models around the globe. J Clin Med. 2018;7:260. doi: 10.3390/jcm7090260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turk-Adawi K, Supervia M, Lopez-Jimenez F, Adawi A, Sadeghi M, Grace SL. Women-only cardiac rehabilitation delivery around the world. Heart Lung Circ. 2021;30:135–43. doi: 10.1016/j.hlc.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Ghanbari-Firoozabadi M, Mirzaei M, Nasiriani K, Hemati M, Entezari J, Vafaeinasab M, et al. Cardiac specialists’ perspectives on barriers to cardiac rehabilitation referral and participation in a low-resource setting. Rehabil Process Outcome. 2020:9. doi: 10.1177/1179572720936648. DOI: 10.1177/1179572720936648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moradi B, Esmaeilzadeh M, Maleki M, Sari L. Factors associated with failure to complete phase II cardiac rehabilitation: Survey registry in Rajaie cardiovascular medical and research center. Int Cardiovasc Res J. 2011;5:139–42. [Google Scholar]
- 24.Jin K, Khonsari S, Gallagher R, Gallagher P, Clark AM, Freedman B, et al. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2019;18:260–71. doi: 10.1177/1474515119826510. [DOI] [PubMed] [Google Scholar]
- 25.Najafi F, Nalini M. Hospital-based versus hybrid cardiac rehabilitation program in coronary bypass surgery patients in western Iran: Effects on exercise capacity, risk factors, psychological factors, and quality of life. J Cardiopulm Rehabil Prev. 2015;35:29–36. doi: 10.1097/HCR.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 26.Babu AS, Lopez-Jimenez F, Thomas RJ, Isaranuwatchai W, Herdy AH, Hoch JS, et al. Advocacy for outpatient cardiac rehabilitation globally. BMC Health Serv Res. 2016;16:471. doi: 10.1186/s12913-016-1658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moghei M, Turk-Adawi K, Isaranuwatchai W, Sarrafzadegan N, Oh P, Chessex C, et al. Cardiac rehabilitation costs. Int J Cardiol. 2017;244:322–8. doi: 10.1016/j.ijcard.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 28.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;37:2315–81. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]