Abstract
Background:
Chronic mental illnesses (CMI) are long lasting and reoccurring and require continuous care as well as an integrated and collaborative approach to organize the care. This study sought to examine whether family centered collaborative care is an acceptable treatment option for individuals with CMI.
Materials and Methods:
From the years 2000 to 2021, ten electronic databases relating to family centered collaborative care for mental illness were searched adopting Preferred Reporting Items for Systematic Reviews and Meta Analysis checklist. Twenty seven relevant articles and a thesis from among 6956 studies retrieved, were assessed their quality appraisal through four standardized tools. The studies were rated as good, moderate, or poor. Studies were calibrated, different opinions were discussed, and extracted data were done.
Results:
Evidence included 11 randomized controlled trials (from 19 articles), one randomized control trial, three mixed methods studies (from 3 articles and 1 thesis), and a qualitative study (from 4 articles). The quality of seven studies was good, 15 were moderate quality, and seven were poor quality. According to moderate to high quality qualitative research, family centered collaborative care was considered an acceptable intervention; though a few studies supported it.
Conclusion:
The findings demonstrated that family involvement in the care of patients with CMI affects no recurrence of the disease, and no re hospitalization of patients with this disorder. As a result, engaging family members in the care process can have a positive impact on the health and well being of these patients.
Keywords: Family, long-term care, mental disorders, review
INTRODUCTION
Chronic mental illnesses (CMIs) such as major depressive disorder, schizophrenia, and bipolar mood disorder have significant difficulties for patients and impose a considerable burden on caregivers.[1] For individuals with CMI, drug therapy is a popular treatment option; it is of note that long-term use of antidepressants, antipsychotics, and mood stabilizers can give rise to unpleasant side effects.[2] Therefore, individuals with CMI may struggle to receive therapies and may suffer from social, functional, and psychological problems.[3] In chronic mental health treatment, patients are cared for using a comprehensive system of evidence-based interventions[4] and family has always been the mainstay of care in these patients.[5]
In conjunction with medication and psychotherapy, the World Health Organization (WHO), Ministry of Health, Scottish Intercollegiate Guidelines Network (SIGN), and the National Institute for Health and Clinical Excellence (NICE) recommended involving families at all stages of mental illness to support individuals with CMI.[6,7,8,9,10,11,12] In addition to psychotherapy, it is recommended that individuals with CMI engage in family interventions and caregiver involvement as well. NICE, SIGN, and WHO identify that caregivers of patients with CMI should involve in care planning, decisions, and sharing of information, respectively.[10,11,13] The purpose of using family-centered collaborative care (FCCC) is to enhance an individual's general and social functioning, to achieve appropriate care, communication, adherence to treatment, quality of life, safety, and family support (FS), and to reduce positive and negative symptoms, relapse rate, and re-hospitalization.[14,15,16,17,18,19,20,21,22,23,24]
The focus of this review is on the use of FCCC by individuals with CMI. One of the four major objectives of the Mental Health Action Plan 2013–2020 is to provide comprehensive, integrated, and responsive mental health services and care in community-based settings.[25] Family-centered care is one of the important components to care for patients with special needs, which can be useful for patients, caregivers, and health-care practitioners.[26,27]
Despite our extensive searching, we were unable to find a review that included all of the variables associated with FCCC in patients with CMI. This review endeavors to fill this research lacuna about the influence of involvement of families in patients with CMI by focusing specifically on FCCC research. In this study, FCCC was compared with no therapy, another treatment option, or treatment as usual (TAU) as an intervention for individuals with CMI. The FCCC is evaluated from a stakeholder's perspective, families, and health professionals, through all research methods, to find out if it is meaningful and useful for individuals with CMI.
Considering the prevalence of CMI and the lack of studies related to FCCC in these patients, the present study aims to determine the collaboration of families and the effect of this collaboration in the care for patients with CMI.
METHODS
Reviewing the literature
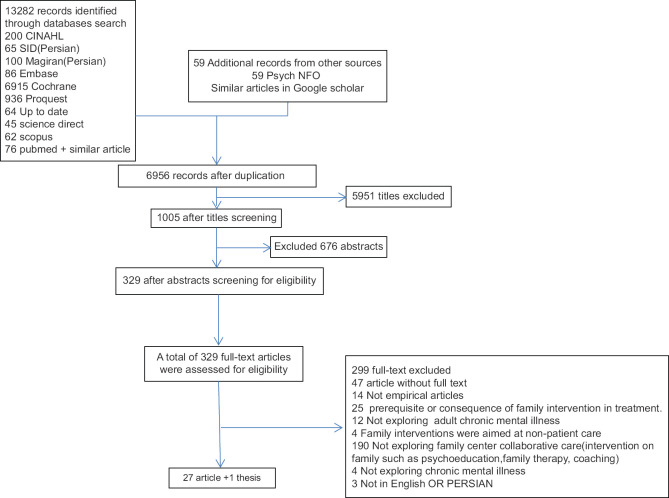
The questions in this review were investigating the acceptability, and meaning and effectiveness of FCCC in kinds of literature. While searching for evidence for this review according to preferred reporting items for systematic reviews and meta-analysis checklist,[28] we used the term “family-centered care“ in line and the term “CMI“ as an umbrella term for schizophrenia, major depressive disorder as well as bipolar mood disorder according to the guidelines in the Diagnostic and Statistical Manual-5.[29] This review discusses 27 relevant articles and a thesis from among 6956 studies retrieved in our search [Figure 1]. FCCC in patients with CMI is the focus of this review. Evidence is included from studies published from the year 2000 until now. The effectiveness of FCCC in all the studies was taken into an account. All types of quantitative and qualitative research were discussed. In screening the literature, we discovered ambiguous definitions of interventions; for that reason, differentiating between family interventions and FCCC was challenging. Following discussion with experts in mental illness, we decided to include the papers about FCCC, which were detected in the search.
Figure 1.
Diagram for the inclusion and exclusion of articles
Selection criteria and search strategy
Ten electronic databases were searched for original articles published since the year 2000 (CINAHL, SID (Persian), Magiran (Persian), Embase, Cochrane, Proquest, Up to date, Science Direct, Scopus, and PubMed). Further searches were done with Google Scholar, reference lists, and other sources (Psych NFO). We used the separate search terms according to each database's rules but in general, we used “collaborative care*“ AND “chronic mental disorder“ OR “severe and persistent mental disorder“ AND “family-center care*.“ RD screened all of these papers by title, abstract, and full text, while MF, MSH, and EM analyzed a sample of the papers to check for ineligibility. Articles published before the year 2000 were excluded, without full text, not empirical articles, prerequisite or consequence of family intervention in treatment, not exploring adult chronic mental illness, family interventions were aimed at nonpatient care, not exploring family center collaborative care (intervention on the family such as psycho-education, family therapy, and coaching), not exploring chronic mental illness, not in English OR Persian. We did our first search on March 21, 2021, and our last search on April 27, 2021.
Quality appraisal methods
The 27 articles and a thesis used various methodologies, so we assessed their quality appraisal through four standardized tools. We used the Verhagen quality appraisal tool[30] for randomized-control trial (RCT) articles, Mixed Methods Appraisal Tool.[31] for Mixed methods studies, critical skills appraisal program[32] for qualitative studies, and Joanna Briggs Institute[33] for Quasi-experimental studies. The reason for using this risk of bias assessment tool was the greater use of these tools by authors in the studies. The tools were scored, and based on their overall quality rating and robustness, the studies were rated as good, moderate, or poor. A sample of 28 studies was calibrated by RD and an independent researcher. Different opinions were discussed. RD (Raziye Dehbozorgi) extracted data from each article and summarized relevant information for the review [Table 1]. MF (Malek Fereidooni-Moghadam), MSH (Mohsen Shahriari), and EM (Ebrahim Moghimi-Sarani) assessed random samples of the extracted summaries for accuracy and consistency. Disagreements between the research team were discussed. In this review, we present a systematic synthesis of the quality and methodological considerations within the studies.
Table 1.
Extracting data from the review’s final studies
| Author name and study year and country | Study type | Study aims | Effectiveness of FCCC (outcome) |
|---|---|---|---|
| Ramírez et al. (2017) Colombiana[34] | RCT | To assess family burden and functioning, patients’ expressed emotions | No difference in results between the TI and the MI |
| Weinstock et al. (2006) Rhode Island[35] | RCT | To determine whether families of patients with MDD and BPAD differ in their functioning during acute and recovered episodes | Families in both diagnosis groups generally recover from acute episodes, their post-recovery scores remain poor to fair |
| Fisher et al. (2018) Sydney[36] | Ph.D. thesis using mixed methods | Developing and evaluating the first DA to treat patients with BPII | Family involvement is essential to consultative practices |
| Kidd et al. (2016) Canada[50] | Mixed methods study | To examine the changes in the outcomes of people with schizophrenia according to self-assessment and caregiver assessment | Improvements in caregivers’ perceptions of community functioning |
| Cohen et al. (2009) USA[51] | Qualitative study | To engage families in the care of their loved ones and to educate them about schizophrenia and its treatment | Families did not take up the family intervention as a result of barriers from stakeholders |
| Kumar et al. (2019) India[37] | Quasi- experimental | Comparison of the effectiveness of a family-assisted home-based cognitive rehabilitation program with a hospital-based cognitive remediation program | Cognitive rehabilitation by carers at home may beneficial |
| Barrowclough et al. (2001) England[14] | RCT | To determine if the program of interventions influenced illness and substance use effects in addition to routine care | Patients’ general functioning improved significantly with an intensive treatment program combining routine treatment with family intervention |
| Kopelawicz et al. (2003) Los Angles[15] | RCT | Evaluating the efficacy of culturally-adapted educational interventions, involving patients and their families separately, in combination with antipsychotic medications | Psychopathology, relapse, re-hospitalization, and social functioning were among key domains of psycho-skills management to produce favorable outcomes |
| Alibeigi et al. (2018) Iran[38] | RCT | To determine whether family-based intervention effects expressed emotion, family coping styles, and severity of bipolar symptoms | Patient symptoms were improved by family-based interventions |
| Tantirangsee et al. (2015) Thailand[39] | RCT | To determine how a short-term intervention for substance use affects family relationships and smoking in patients with schizophrenia and other related disorders | In comparison to the BI alone group, participants in the BI-FS intervention had better family relationship functioning |
| Giro’n et al. (2010) Spain[16] | RCT | To evaluate the effectiveness and efficacy of a family psychosocial intervention after adjusting for variables including prognosis, compliance, and family burden | The intervention reduced relapses, serious incidents, symptomatic episodes, and hospitalizations, enhanced social functioning, and relieved family burdens in comparison with standard treatment |
| Giro’n et al. (2015) Spain[40] | RCT | The efficacy of family-based psychosocial interventions in schizophrenia | Family intervention has been associated with a reduction in guilt induced by relatives, and dominance and increased empathy |
| Mueser et al. (2009) the United States[41] | RCT | To comparing a comprehensive, behaviorally-based FIDD to a short-term FPE | It seems that motivating family members to participate in family interventions, and addressing the disruption of drug use in families can significantly improve family engagement and retention |
| Tas et al. (2012) Turkey[17] | RCT | To investigate the impact of family involvement on social cognition training in patients with schizophrenia who are clinically stable | FSCIT significantly enhanced QOL, social functioning, and social cognition, but SS significantly weakened all outcome variables. SCIT with family assistance can improve social cognition, QOL, and social functioning |
| Farooq et al. (2011) Pakistan[18] | RCT | Evaluating the effectiveness of a treatment method that involves family members STOPS the improvement of treatment adherence and outcome | A STOPS program may enhance adherence to schizophrenia treatment in LAMI regions |
| Glick et al. (2011) America[43] | RCT | To examine the relationship between treatment outcomes and two family factors: family involvement and support for treatment adherence | QOL items on family contact as well as medication adherence indicated that patient improvement correlated with the involvement of the family in medication adherence |
| Leff et al. (2001) London[19] | RCT | To determine whether community psychiatric nurses trained in family work can alter | Insufficient medication compliance and a small sample size made it impossible to |
| emotional climate among families caring for people with schizophrenia, and how much it costs | detect a significant impact on relapse rates. Inpatient care was significantly cheaper than the CPNs’ input to families | ||
| Montero et al. (2001) Spain[44] | RCT | To compare the different outcomes of two different approaches for psychoeducational treatment in families of individuals with schizophrenia | There was no significant difference between the two strategies in terms of relapse rate and hospital stay. Both interventions improved social adjustment, however, BFT impacted more items, such as use of leisure time, self-care, interpersonal friction, household participation, and interest in obtaining a job |
| Miklowitz et al. (2007)[45] | RCT | To evaluate the impact of pharmacological and psychosocial treatment in patients with bipolar disorder 9 months after a depressive episode | Over the course of 9 months, patients receiving intensive psychotherapy had higher total functioning, relationship functionality, and overall life satisfaction than collaborative care patients |
| Miklowitz et al. (2007) NA[46] | RCT | To assess the effects of four disorder-specific psychotherapies combined with pharmacotherapy for time to recovery and the likelihood of remaining well following a bipolar episode | Intensive psychotherapy in addition to pharmacotherapy was more effective than brief treatment in stabilizing bipolar depression |
| Kaselionyte et al. (2019) London[47] | Mixed metods study | To assess feasibility in four inpatient units in East London and explore participants’ experiences | Over half (53) of the patients were able to receive the intervention within one week of admission |
| Berzins et al. (2018) UK[20] | Qualitative study | To investigate family and service users’ perceptions about raising safety concerns, and service users, carer, and health-care professionals’ views about involving in safety interventions | Health professionals and most service users and caregivers saw potential involvement in interventions that improve safety, to sure their experiences were considered |
| Olasoji et al. (2017) Australia[21] | Qualitative study | To investigate carers’ experiences at a major mental health service in providing supportive care | Working collaboratively with informal carers to support relatives with severe mental illness and recognizing their value is important |
| Giacco et al. (2017) London, United Kingdom[48] | Qualitative study | to evaluate patients’, carers’, and clinicians’ perspectives on improving family involvement in inpatient settings | Several participants argued that the early involvement of family members in inpatient treatment should be considered to help patients manage a very acute clinical presentation and their ability to make decisions |
| Asher et al. (2018) Ethiopia[22] | Mixed methods study | To assess the acceptability, feasibility and productivity of RISE CBR intervention | Increased family support, improved healthcare access, income growth, and an increase in self-esteem may all be positive effects of the RISE CBR intervention |
| Zeighami et al. (2019) Iran[23] | RCT | To assess the impact of group family psychological training on the severity and relapse of depression in patients with major depression | The intervention was effective in reducing symptoms and preventing relapses |
| Krgar-Barzi et al. (2019) Iran[49] | Quasi- experimental | To evaluate the impact of Bowen’s family therapy on family development and maladaptive emotional patterns among major depressive disorder patients | The intervention is helpful in enhancing the developmental functioning of family and reducing maladaptive emotions in women with major depression |
| Cheng et al. (2018) China[24] | RCT | To assess the impact of family-centered maternal care nursing on puerperal depression among mothers in the puerperal stage and to alleviate natural delivery women’s burden and reduce postpartum depression in delivery women | FCMC showed less depression than the control group, proving that FCMC was more effective than conventional maternity nursing in improving puerperal depression |
RCT: Randomized-controlled trial, NA: Not available, MI: Multimodal intervention, TI: Traditional intervention, MDD: Major depressive disorder, BPAD: Bipolar affective disorder, DA: Decision aid, BPII: Bipolar II, FIDD: Family intervention for dual disorders program, FPE: Family psychoeducational program, SS: Social stimulation, STOPS: Supervised treatment in outpatients, FSCIT: Family-assisted social cognitive training, for schizophrenia, LAMI: Low- and middle-income, QOL: Quality of life, BFT: Behavioral family therapy, RISE: Rehabilitation intervention for people with schizophrenia in Ethiopia, CBR: Community-based rehabilitation, FCMC: Family-centered maternity care, SCIT: Social cognition and interaction training, BI: Brief Intervention, BI-FS: BI with family support
RESULTS
Analysis of the family-centered collaborative care literature
The quality of studies
In general, the evidence presented in this review was moderate, with 11 randomized-controlled trials (from 19 articles), an analysis of a RCT, three mixed-methods studies (from 3 articles and 1 thesis), and a qualitative study (from 4 articles). The quality of seven studies was good, 15 were moderate quality, and seven were poor quality [Table 2]. To prevent data loss, none of the studies were excluded throughout this review; however, the poor-quality studies were taken into account with caution. This presentation of the data showed that FCCC is most effective in improving patient outcomes.[14,15,16,17,18,19,20,21,22,23,24,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49] Several quotations supporting participants’ experiences were unclear because they were rarely accompanied by references to the source or context of the examples, and quotations were unclear whether they came from patients with psychosis, caregivers, or health system staff in this mixed-methods and qualitative study.[50,51]
Table 2.
Quality of family-center collaborative care studies
| Kind of article | Critical appraisal tool | Score | Quality |
|---|---|---|---|
| RCT | Verhagen | 2/9 | Poor |
| RCT | Verhagen | 5/9 | Moderate |
| Mixed methods | MMAT | 4/5 | Moderate |
| Mixed methods | MMAT | 3/5 | Moderate |
| Qualitative study | CASP | 7/10 | Moderate |
| Quasi experimental | JBI | 8/9 | Good |
| RCT | Verhagen | 6/9 | Moderate |
| RCT | Verhagen | 2/9 | Poor |
| RCT | Verhagen | 5/9 | Moderate |
| RCT | Verhagen | 7/9 | Good |
| RCT | Verhagen | 4/9 | Moderate |
| RCT | Verhagen | 5/9 | Moderate |
| RCT | Verhagen | 6/9 | Moderate |
| RCT | Verhagen | 6/9 | Moderate |
| RCT | Verhagen | 3/9 | Poor |
| RCT | Verhagen | 2/9 | Poor |
| RCT | Verhagen | 4/9 | Moderate |
| RCT | Verhagen | 4/9 | Moderate |
| RCT | Verhagen | 6/9 | Moderate |
| RCT | Verhagen | 7/9 | Good |
| Mixed methods | MMAT | 3/5 | Moderate |
| Qualitative study | CASP | 9/10 | Good |
| Qualitative study | CASP | 9/10 | Good |
| Qualitative study | CASP | 9/10 | Good |
| mixed methods pilot study | MMAT | 4/5 | Good |
| RCT | Verhagen | 3/9 | Poor |
| RCT | Verhagen | 2/9 | Poor |
| RCT | Verhagen | 5/9 | Moderate |
RCT: Randomized-controlled trial, MMAT: Mixed methods appraisal tool, CASP: Critical Appraisal Skills Programme, JBI: The Joanna Briggs Institute
Results were sometimes confounded because a few of these findings are related to interventions that included the engagement of families, but there are other interventions included in this package.[14,16,18,22,34,36,40,45,46,50] These studies failed to analyze possible bias when integrating FCCC with other psychotherapeutic or psychosocial interventions. Most primary studies indicated FCCC requested involving caregivers in supporting the individual at home,[14,15,16,19,22,35,37,38,39,41,44,47,48,50] However, other studies did not mention the need for FS. Several RCTs were single blind; allocation concealment[14,35] or outcome assessor blinding[15,41] was done appropriately in these RCTs, although eight numbers of RCTs were double-checked blindly with allocation concealment and outcome assessor blinding[16,19,39,40,43,44,45,46] and the rest of them were not checked blindly. Besides, research designs were not mentioned in some studies,[23,24,35,39,40,49] while other studies did well with their research designs.
Researchers describe the method of recruitment in their studies, and based on a study by Kumar et al., (2019) randomization was not performed, and Kargar-Barzi was not clearly described.[49] In the rest of the initial studies, randomization was performed and optimal randomization was observed in a number of studies[14,16,17,18,24,38,39,41,46] and in terms of the important prognostic indicators, the groups were similar based on several participants at baseline.[14,16,17,24,35,38,39,40,41,44,45] All RCTs have inclusion and exclusion criteria. In the various study designs, the FCCC or family intervention structure was ambiguous or not clearly described.[16,20,22,34,35,36,37,40,45,46,47,48,50,51] Fisher, Kidd, Asher, Kaselionyte, et al. effectively integrated different components of mixed methods studies to answer the research question.[22,36,47,50] Analyses were not described in Cohen's study, making it hard to ascertain in which reliable analyses were conducted.[51] In the majority of qualitative studies, other researchers were not consulted to confirm analyses.[20,21,51] Among the qualitative studies, consistency has been improved mainly through semi-structured interviews,[36,50] peer checks, and[47] member checks.[36] Overall, the quantitative papers were reliable.[14,15,17,19,35,36,38,39,41,46,50]
According to some studies, family members of patients stayed with them and actively helped them when they were in FCCC.[22,23,24,36,37,38,45,47,49,50] Several studies have proposed implementing educational interventions for family engagement in patient care.[14,15,17,18,23,38,39,41,44,49] Only one qualitative study mentioned bracketing of bias.[21] Most mixed-methods or qualitative studies ignored biases due to researchers acting as facilitators of interventions.[20,22,47,48,50] The results of the quantitative studies were objectively reported as significant and nonsignificant.
Demographics of participants
Participants who were recruited for the review studies were with or without caregivers and health professionals had schizoaffective disorder, schizophrenia, major depressive, or disorder bipolar disorder. A total of 1037 men and 1062 women participated in the articles. This list does not contain studies whose gender demographics have been unclear or not provided.[14,19,37,40,43] Schizophrenic patients were the subjects of most studies (1052 participants) and the rest of the studies focused on participants with major depression disorder (343 participants) and bipolar disorder (763 participants) and several studies did not identify the type of disease.[20,38,47,48] In most cases, the studies were conducted by the same researchers in the USA.[15,35,41,43,51] The rest were done in Colombia,[34] Sydney,[36] India,[37] England,[14,19,47,48] Iran,[23,38,49] Thailand,[39] Spain,[16,40,44] Turkey,[17] China,[24] Pakistan,[18] the UK,[20] Australia,[21] and Ethiopia.[22]
Methods of treatment
Comparison in the study was complicated by the fact that FCCC was part of a series of interventions, each with a different title, including multimodal intervention,[34] outpatient treatment,[35] decision aid (DA),[36] CAT (Cognitive adaptation training) manual,[50] caregiver-assisted home-based cognitive remediation program,[37] intensive treatment program,[14] family-focused treatment,[38] brief intervention with FS (BI-FS),[39] psychosocial family intervention,[16,40] family intervention for dual disorders program and family psychoeducational program (FPE),[41] family-assisted social cognitive training or FSCIT,[17] supervised treatment in outpatient,[18] behavioral family therapy (BFT),[44] intensive psychosocial treatment,[45,46] rehabilitation intervention for people with schizophrenia in Ethiopia and community-based rehabilitation (CBR),[22] family-centered empowerment model,[23] and family-centered maternity care (FCMC).[24] Different theoretical orientations were reflected in some of these titles, for example, there are pragmatic and at-home methods in the CAT manual for easing the cognitive effects of illness, and the family's involvement in patient care depends on the use of this guide.[50] Family engagement in care is emphasized in many of these studies by family education.[14,15,17,18,23,38,39,41,44,49] In some studies, family engagement in patient care has been directly addressed.[17,20,24,43,47,48,51]
Literature frequently has mentioned or described the family's orientation. There was some willingness on the part of some families or patients to participate in care,[22,23,36,37,38,45,47,48,49,50] while others were hesitant.[14,21,51] In Cohen et al.'s study due to barriers from all stakeholders, the family intervention did not succeed. Several factors contributed to no response, including a lack of attention from families, patients’ privacy concerns, clinicians’ misunderstanding of family-patient relationships, and organizations’ unwillingness to free up time or offer incentives.[51] There were also fewer admissions in the last year, the mean age of the patients who refused intensive treatment programs were significantly older and the illness duration was longer.[14] Support services were critical for family cooperation with treatment elsewhere.[21]
Ramírez et al. discuss the level of emotional expression (criticisms and over-interference), family functioning, and how the patient perceives.[34] In another study, family functioning dimensions were communication, roles, problem-solving, emotional responsiveness, emotional involvement, behavior management, and general functioning.[35] There were mixed opinions on the efficacy of the DA section in engaging family members in clinical decision-making in Fisher's study. These sections helped individuals who had recently received a diagnosis or were yet to involve their families or be involved to learn practical ways for engagement.[36] FCMC in Cheng and their colleague's study is centered on family management, integrating health-care workers’ support and families’ emotional support to provide care to mothers and babies and improve delivery compliance.[24]
The purpose of Kidd et al.'s study was to determine the effectiveness of a family-centered approach to providing environmental support, specifically CAT, for managing cognitive and social problems in schizophrenia. To use this guideline, no clinical assistance was required, a chapter in the manual explained how schizophrenia impacts cognitive functioning, and family engagement in recovery, focusing on implementation processes.[50] As described in Cohen's approach, the goal of the family intervention was to improve communication and encourage the families to call and provide contact details.[51] The family members would stay with the patient and assist the patient in cognitive exercises in Kumar's study, with the responsibilities of following the patient's engagement during exercises and giving assistance to the patient as needed.[37]
Several studies have viewed the family education as a significant factor in family engagement[14,15,17,18,23,38,39,41,44,49] or in conjunction with other interventions.[46,47,49,51] FCCC was for increasing effective communication skills and interpersonal relations,[40,45,46,51] encouraging the family members to call and, providing their contact information,[51] other aspects of FCCC were patients and caregivers responsible for monitoring the patient's cognitive rehabilitation received detailed training on what tasks the patient is expected to be accomplished in the next 2 weeks,[37] family's skills to caring from patients,[19] homework assignments,[45] participating in their care and planning their discharge,[47] carer involvement in future safety interventions,[20] involvement in the care of their relative,[21] involvement of carers in patients’ treatment in inpatient settings,[48] and involvement in decision making and caring.[22] Family psycho-social intervention in two studies consist of active listening, clarification of emotion, problems, and needs and diminishing critical attitude, over-involvement, training in empathy, establishing a therapeutic alliance,[16,40] and in three studies consists of the problem-solving technique[16,40,45]
Support from family members for patients’ adherence to treatment is an important aspect of FCCC, according to Glick's study.[43] Family therapy based on Bowen's emotional therapy by informing individuals about their positive and negative emotions is another aspect of FCCC in literature.[49]
The effectiveness of family-centered collaborative care
Several RCTs examined the effectiveness of FCCC exploring family functioning as a primary outcome,[15,16,17,18,34,37,39,40] together with the ability to support treatment adherence on one RCT.[18,43] The measurement of outcome in two good quality studies included best care outcome for consumers[21] and family relationship functioning.[39] Some studies measured caregiver burden after family involvement programs, two of which have relieved family burden after FCCC,[16,34] and one study found caregivers burden scores declined significantly over a large effect size,[50] also, the FCCC improves rates of engagement in family programs and retention.[41] Families’ engagement facilitates treatment decision-making both within, and outside of consultation,[36] reduction in guilt induced by relatives, and increases empathy.[40]
In addition, several studies measured the patient's outcome, such as relapse rate,[15,16,19,23] re-hospitalizations,[15,16] social functioning,[15,16,17] social cognition and quality of life,[17] general well-being,[14] the symptom of patients,[38] and positive and negative symptoms,[16,23] in these studies, all of them were improved. Patients’ improvement was correlated with family help in taking medications, according to a poor-quality study.[43] The outcome measures in other lower-quality studies included adherence to treatment,[18] improving developmental functioning of the family, and reducing maladaptive emotional schemes.[23] Many studies described measurements’ validity, reliability, and standardization for individuals with CMI,[14,17,34,35,36,38,39,41,46,50] other studies do not mention it explicitly or completely.
Based on an intention to treat analysis, Montero et al. illustrated that there was no differences in the relapse rate of relative groups (RG) and BFT and both groups had similar lengths of hospital stay. Although BFT produced significant changes in more items than the RG, such as self-care, leisure time use, household participation, friction in interpersonal relationships, and interest in getting a job.[44] In one study, despite the stakeholders’ barriers, the family intervention did not take place.[51] There was no significant effect on patient relapse rate in another study with moderate quality due to medication compliance and small sample size issues.[19] A good quality study can successfully achieve a home-based program for patients with schizophrenia relying on the help of their caregivers.[37] Carer engagement was effective within a week following the admission of most patients enrolled in the Kaselionyte study.[47]
In the high-quality study by Berzins et al., nearly all health professionals, as well as the majority of patients and caregivers, saw the potential for service users and caregivers to be involved in safety-related interventions.[20] Due to the number of studies with poor design, these provided weak evidence. As a result of the lack of evidence and the variable quality, the review provides preliminary, but not convincing evidence that FCCC in the treatment of CMIs is beneficial for these patients.
The meaningfulness and acceptability of family-centered collaborative care
According to the second research question, multiple themes were identified concerning the acceptability and meaningfulness of FCCCs. A careful interpretation was made of the findings of low-quality studies. A common finding was that the FCCC reduces relapse rate and re-hospitalization.[15,16,19,23] Many caregivers expressed interest in helping the patients in FCCC program,[22,38,44,48,50] monitoring the patient's engagement in the task[37] and the family succeeds in achieving the desired changes in the home's emotional environment.[19] In a high-quality study, caregivers reported that in addition to family activities, support systems were needed.[21] The participant in Giacco et al. good quality study emphasized the necessity of involving caregivers during care planning and discharge process.[48]
In the study of Asher et al., many participants believed CBR with family engagement contributed to increased public awareness and understanding of mental illness signs and treatments, as well as a turning point in changing attitudes toward the illness. Besides, health staff, community leaders, and CBR workers all accepted CBR.[22] Despite the difficulties in raising safety concerns and then engaging family members in safety interventions, over half of the health professionals supported service user and caregiver involvement in safety interventions, predominantly because of their experience,[20] and it was noted that the informal environment during the intervention allowed participants to share their experiences and concerns with one moderate study.[47] One moderate study, however, identified barriers from all stakeholders, which led to the failure of the family therapy project. Families did not respond, individuals were concerned about privacy and burdening their families, clinicians misperceived what patient–family contact was, and healthcare providers did not make time or offer incentives to provide the service.[51]
Interpretation of family-centered collaborative care
There has not been conclusive evidence for the effectiveness of FCCC for participants with CMI, according to our review of the literature. Kidd indicated that there was no change in the self-reported ratings of supported individuals between baseline and 4 months, nor in quality of life or medication compliance and there was a significant reduction in caregiver burden scores with a large effect size with no significant difference depending on the type of manual[50] and according to Cohen, the family intervention failed because stakeholder barriers prevented it.[51]
In contrast, in a good quality study by Tantirangsee et al., BI-FS helped participants improve their family relationships,[39] and one study found that a combination of psychosocial treatment and family engagement was more effective in promoting recovery from bipolar depression than a brief treatment alone,[45] carers engagement in other study showed promoting the in patient safety levels,[20] and mental health professionals should recognize the caregiver's role and collaboration in the care planning to provide the best care. An intervention involving community-CBR with family involvement may enhance FS, improve access to health-care services, increase income, and promote self-esteem in a good quality mixed-methods study.[22] The other studies in our review examining effectiveness had little effect on our conclusions.[21] In most studies in this review, clients and therapists experienced FCCC as meaningful and acceptable. Most commonly, FCCC decreases relapse rate, and re-hospitalization, modifying caregiver burden, improving family and patient functioning and symptom of patients, and adherence to the treatment of patients. However, most of our results are based on only a small number of high-quality studies and should be interpreted carefully.
Future research considerations and clinical practice
Due to the limited number of robust studies and the disconnection between the evidence concerning FCCC's utility, and the fact that this concept has not been utilized by researchers, further rigorous research is required. Several theoretical-methodological and clinical concerns were raised here that need consideration.
The definition of family-centered collaborative care
It was difficult to compare across studies because family-centered collaborative care was described in different ways and titles that were not always clear. A clear description is important since FCCC consists of complex components that interact with the patients, caregivers, and related professionals. Two studies that define family-centered collaborative care in a series of interventions relating to those studies have referred only to the “family functioning“ concept without additional explanation.[34,50] Most definitions were assessed functioning within the dimensions such as roles, problem-solving, affective engagement, behavior control, emotional responsiveness, and a general dimension as well,[35] involving family in decision-making,[36] increase communication,[16,35,40,45,46,51] encourage the family to call, and provide contact information,[51] responsibility for monitoring the patient's task,[37] problem-solving technique,[16,40,45] clarification of emotion, problems, and needs, diminishing critical attitude, over engagement, training in empathy, establishing a therapeutic alliance,[16,40] family presence and support patient's treatment adherence,[43] and family's skills for caring.[19] The engagement of caregivers should entail such activities as engaging them early in the admission process, providing them with information, and engaging them in the care process and discharge plan,[47] future safety interventions,[20] in patients’ treatment in inpatient contexts,[48] in decision-making and caring,[22] Taking care of mothers and babies by combining individual management with technical support of medical workers and FS,[24] and caregivers education.[14,15,17,18,23,38,39,41,44,46,51]
The mechanisms of family-centered collaborative care
The mechanisms of FCCC were not well defined in this review, and these mechanisms were not easily identified by professionals. Although according to one, caregivers were participating in supporting individuals and maintaining regular contact with them,[35] another suggests a manual to guide the family to involve in caring for the patient[50] or encouraging the family is another way for family engagement,[51] as well as FPE.[14,15,17,18,23,38,39,41,44,46,51] This review highlights several mechanisms for involving family, but they need further investigation. Robust qualitative and mixed-methods studies through interviews and focus groups can provide insight into what participants believe triggers change.[20,21,22,48]
Outcome measures
A study of high quality demonstrated that FCCC outcomes can be obtained through processes in which families are willing to help the patient during the intervention.[37,38] Caregiver involvement in monitoring the patient's involvement in the tasks as well as providing assistance when necessary might influence outcomes.[37] Other factors may include barriers from stakeholders,[51] acceptability of intervention,[50] old age, longer duration of illness and few admission in the past 3 months,[14] presence or absence of support from the family,[39] medication compliance and sample size,[19] calm circumstances during the intervention,[47] and the existence of support services.[21] The primary outcome measures in these RCTs might not have been the best targets for FCCC. Primary outcome measures, such as career burden and relapse rates, were not justified from clinical and theoretical perspectives. This review demonstrated that the participants were able to improve their social functioning, positive and negative symptoms, adherence to treatment, as well as safety, and enhancing FS through FCCC.
Intervention design
Overall, statistical power is required to identify a smaller difference among groups to minimize errors of type II. For future RCTs, it might be important to consider carefully FCCC group dynamics. A therapeutic group is often initiated by families engaging individually to form an effective relationship. The preparation can facilitate integration into the group, which can be beneficial for families, patients, and professional workers. Several studies offered FCCC with other psychosocial, community-based, or therapeutic interventions; it can be difficult to distinguish FCCC interventions from others. In future research, addressing this overlap may make the results more valid. Due to a wide range of interventions from 14 weeks to 28 months and varying efficacy, the correct duration of FCCC remains unclear. Incorporating regular follow-up periods into research could clarify the ultimate goals of FCCC that were not reflected in the papers that have been reviewed. In this review, the duration of follow-up in a study was a time in 3–22 range,[35] 3, 6, and 12[18] or 2 and 6[23] months after intervention and in another study were 6, 12, 18, and 24[45] months after intervention, in others there was no follow-up time shown,[17,34,37,40,41,44,49] while another study demonstrated follow-up at 3 month,[4,14,36,38] 4,[50] 6,[15,39] 12,[22] 15,[51] and 24[16,19,46] months after intervention in another study.
Review limitations
There are several studies written in languages other than English and Persian included in the study, so their findings may have a limited application to the general population. As well as overlooking any particular differences within this population, consideration of the various forms of CMI may have also been overlooked. All studies of participants with CMI, such as schizophrenia, major depression, and bipolar mood disorder, were included in this review. We had to treat poor-quality studies with caution. In addition, because there were relatively few studies and small samples in qualitative and mixed methods and only four articles were of high quality, we need to interpret these results with caution. We had to treat poor-quality studies with caution. In addition, because there were relatively few studies and small samples in qualitative and mixed methods and only four articles were of high quality, we need to interpret these results with caution.
DISCUSSION AND CONCLUSION
Inconclusive evidence exists regarding the efficacy of FCCC in reducing symptoms and functioning for participants with CMI.[36,37,50] However, discounting family engagement might deprive participants with CMI of a meaningful intervention such as that suggested by quantitative, qualitative, and mixed method studies. Differences between the evidence for efficacy and stakeholders’ and clinicians’ experience highlight a gap in the understanding of why, how, and to who FCCC is beneficial, and how this can be addressed.[14,15,51] Towards this end, this review suggests that exploring the effectiveness of FCCC through RCTs is important to gain stakeholder support due to prevent relapse rates and re-hospitalization RCTs should be conducted based on qualitative evidence gathered through the review of qualitative literature.[17,38,40,41,43] Ethnographic, grounded theory, and phenomenology research show how individuals are engaged in caring, and whether FCCC can support them, recognize the live experiences of stakeholders, and can show the process of engaging caregivers in caring.[52] An understanding of how collaborative care works may enhance the theoretical understanding of collaborative care and guide controlled research. Families are key members in the care of patients with chronic conditions. Overall, the reported results emphasize the need for the involvement of family in the care of patients with CMI.
Financial support and sponsorship
This review article was funded by the Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This paper was extracted from Ph.D. thesis with an ethical approval number (IR.MUI.RESEARCH.REC.1399.502). We appreciate the support of Isfahan University of Medical Sciences for this study. MSH has full access to the study data and is ultimately responsible for its publication.
REFERENCES
- 1.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Cutler JL. Kaplan and Sadock’s Synopsis of Psychiatry. New York: LWW; 2016. [Google Scholar]
- 3.Thornicroft G, Tansella M, Becker T, Knapp M, Leese M, Schene A, et al. The personal impact of schizophrenia in Europe. Schizophr Res. 2004;69:125–32. doi: 10.1016/s0920-9964(03)00191-9. [DOI] [PubMed] [Google Scholar]
- 4.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–8. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 5.Sharma N, Chakrabarti S, Grover S. Gender differences in caregiving among family – Caregivers of people with mental illnesses. World J Psychiatry. 2016;6:7–17. doi: 10.5498/wjp.v6.i1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NIH. Bipolar disorder: Assessment and management. In: NICE. England: National Institute for Health and Care Excellence; 2019. [PubMed] [Google Scholar]
- 7.NICE. Depression in adults: Recognition and management. In: Clinical Guideline [CG90] England: National Institute for Health and Clinical Excellence Published; 2009. [PubMed] [Google Scholar]
- 8.NICE. Service User Experience in Adult Mental Health: NICE Guidance on Improving the Experience of Care for People Using Adult NHS Mental Health Services. England: National Collaborating Centre for Mental Health; 2012. [Google Scholar]
- 9.NCCMH. editor. Violence and Aggression: Short-Term Management in Mental Health, Health and Community Settings. UK: British Psychological Society; 2015. [PubMed] [Google Scholar]
- 10.WHO. Management of Physical Health Conditions in Adults with Severe Mental Disorders: WHO Guidelines. Switzerland: WHO; 2018. [PubMed] [Google Scholar]
- 11.SIGN. Management of schizophrenia, a National clinical guideline. In: Spn, editor. Scottish Intercollegiate Guidelines. Network. Edinburgh: Scottish Intercollegiate Guidelines Network; 2013. [Google Scholar]
- 12.Chua HC, Chan LL, Chee KS, Chen YH, Chin SA, Chua PL, et al. Ministry of health clinical practice guidelines: Depression. Singapore Med J. 2012;53:137–43. [PubMed] [Google Scholar]
- 13.NICE. Bipolar Disorder in Adults. England: NICE; 2015. [Google Scholar]
- 14.Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry. 2001;158:1706–13. doi: 10.1176/appi.ajp.158.10.1706. [DOI] [PubMed] [Google Scholar]
- 15.Kopelowicz A, Zarate R, Gonzalez Smith V, Mintz J, Liberman RP. Disease management in Latinos with schizophrenia: A family-assisted, skills training approach. Schizophr Bull. 2003;29:211–27. doi: 10.1093/oxfordjournals.schbul.a006999. [DOI] [PubMed] [Google Scholar]
- 16.Girón M, Fernández-Yañez A, Mañá-Alvarenga S, Molina-Habas A, Nolasco A, Gómez-Beneyto M. Efficacy and effectiveness of individual family intervention on social and clinical functioning and family burden in severe schizophrenia: A 2-year randomized controlled study. Psychol Med. 2010;40:73–84. doi: 10.1017/S0033291709006126. [DOI] [PubMed] [Google Scholar]
- 17.Tas C, Danaci AE, Cubukcuoglu Z, Brüne M. Impact of family involvement on social cognition training in clinically stable outpatients with schizophrenia – A randomized pilot study. Psychiatry Res. 2012;195:32–8. doi: 10.1016/j.psychres.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 18.Farooq S, Nazar Z, Irfan M, Akhter J, Gul E, Irfan U, et al. Schizophrenia medication adherence in a resource-poor setting: Randomised controlled trial of supervised treatment in out-patients for schizophrenia (STOPS) Br J Psychiatry. 2011;199:467–72. doi: 10.1192/bjp.bp.110.085340. [DOI] [PubMed] [Google Scholar]
- 19.Leff J, Sharpley M, Chisholm D, Bell R, Gamble C. Training community psychiatric nurses in schizophrenia family work: A study of clinical and economic outcomes for patients and relatives. J Ment Health. 2001;10:189–97. [Google Scholar]
- 20.Berzins K, Louch G, Brown M, O’Hara JK, Baker J. Service user and carer involvement in mental health care safety: Raising concerns and improving the safety of services. BMC Health Serv Res. 2018;18:644. doi: 10.1186/s12913-018-3455-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olasoji M, Maude P, McCauley K. Not sick enough: Experiences of carers of people with mental illness negotiating care for their relatives with mental health services. J Psychiatr Ment Health Nurs. 2017;24:403–11. doi: 10.1111/jpm.12399. [DOI] [PubMed] [Google Scholar]
- 22.Asher L, Hanlon C, Birhane R, Habtamu A, Eaton J, Weiss HA, et al. Community-based rehabilitation intervention for people with schizophrenia in Ethiopia (RISE): A 12 month mixed methods pilot study. BMC Psychiatry. 2018;18:250. doi: 10.1186/s12888-018-1818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeighami R, Javdani H, Alipoor Heydar M, Ghadami E. He effect of family centered empowerment model on the severity of symptoms in patients with major depressive disorder. J Urmia Nurs Midwifery. 2019;17:535–45. [Google Scholar]
- 24.Cheng H, Yu L, Wang P, Jia X, Kong W. Influences of family-centered maternity care nursing on puerperal depression of delivery women during puerperal period. Biomed Res. 2018;29:654–7. [Google Scholar]
- 25.WHO. Investing in Mental Health: Evidence for Action. Switzerland: WHO; 2013. [Last accessed on 2021 Aug]. Available from: https://www.who.int/ [Google Scholar]
- 26.Feinberg LF. Moving toward person-and family-centered care. Public Policy Aging Rep. 2014;24:97–101. [Google Scholar]
- 27.Knapp M, Cambridge P, Thomason C, Beecham J, Allen C, Darton R. Care in the community: Challenge and demonstration. London: Routledge; 2018. [Google Scholar]
- 28.EQUATOR. Enhancing the Quality and Transparency of Health Research University of Oxford. England:UK: EQUATOR Centre; 2021. [Last accessed on 2021 Mar 21]. Available from: https://www.equator-network.org . [Google Scholar]
- 29.First MB. DSM-5 Handbook of Differential Diagnosis. Washington, DC: American Psychiatric Pub; 2013. [Google Scholar]
- 30.Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51:1235–41. doi: 10.1016/s0895-4356(98)00131-0. [DOI] [PubMed] [Google Scholar]
- 31.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285–91. [Google Scholar]
- 32.Oxford. Critical Appraisal Skill Program, Qualitative Study Oxford. 2018. [Last accessed on 2021 Aug]. Available from: http://creativecommons.org/licenses/by-nc-sa/3.0/www.casp-uk.net .
- 33.Critical Appraisal Tools South Australia: The University of Adelaide. 2019. [Last accessed on 2021 Mar 25]. Available from: https://jbi.global/critical-appraisal-tools .
- 34.Ramírez A, Palacio JD, Vargas C, Díaz-Zuluaga AM, Duica K, Agudelo Berruecos Y, et al. Expressed emotions, burden and family functioning in schizophrenic and bipolar I patients of a multimodal intervention program: PRISMA. Rev Colomb Psiquiatr. 2017;46:2–11. doi: 10.1016/j.rcp.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Weinstock LM, Keitner GI, Ryan CE, Solomon DA, Miller IW. Family functioning and mood disorders: A comparison between patients with major depressive disorder and bipolar I disorder. J Consult Clin Psychol. 2006;74:1192–202. doi: 10.1037/0022-006X.74.6.1192. [DOI] [PubMed] [Google Scholar]
- 36.Fisher A. Enhancing treatment decision-making in bipolar II disorder: Development and evaluation of a treatment decision-aid for patients and their families [Mixed methods design]: Univ Syd 2018;The University of Sydney, Ph.D. Philosophy thesis, 424 pages, Protocol No. 2015/197 and 2016/763. [Google Scholar]
- 37.Kumar D, Ashwini K, Hegde S, Prasanna L, Joseph B, Bose A, et al. Caregiver assisted home-based cognitive remediation for individuals diagnosed with schizophrenia: A pilot study. Asian J Psychiatr. 2019;42:87–93. doi: 10.1016/j.ajp.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alibeigi N, Momeni F. The effectiveness of family-based intervention on symptom severity, expressed emotion and coping styles of bipolar patients. Iran Red Crescent Med J. 2018;20:0. [Google Scholar]
- 39.Tantirangsee N, Assanangkornchai S, Marsden J. Effects of a brief intervention for substance use on tobacco smoking and family relationship functioning in schizophrenia and related psychoses: A randomised controlled trial. J Subst Abuse Treat. 2015;51:30–7. doi: 10.1016/j.jsat.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 40.Girón M, Nova-Fernández F, Mañá-Alvarenga S, Nolasco A, Molina-Habas A, Fernández-Yañez A, et al. How does family intervention improve the outcome of people with schizophrenia? Soc Psychiatry Psychiatr Epidemiol. 2015;50:379–87. doi: 10.1007/s00127-014-0942-9. [DOI] [PubMed] [Google Scholar]
- 41.Mueser KT, Glynn SM, Cather C, Zarate R, Fox L, Feldman J, et al. Family intervention for co-occurring substance use and severe psychiatric disorders: Participant characteristics and correlates of initial engagement and more extended exposure in a randomized controlled trial. Addict Behav. 2009;34:867–77. doi: 10.1016/j.addbeh.2009.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gensichen J, Petersen JJ, Karroum T, Rauck S, Ludman E, König J, et al. Positive impact of a family practice-based depression case management on patient's self-management. Gen Hosp Psychiatry. 2011;33:23–8. doi: 10.1016/j.genhosppsych.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 43.Glick ID, Stekoll AH, Hays S. The role of the family and improvement in treatment maintenance, adherence, and outcome for schizophrenia. J Clin Psychopharmacol. 2011;31:82–5. doi: 10.1097/JCP.0b013e31820597fa. [DOI] [PubMed] [Google Scholar]
- 44.Montero I, Asencio A, Hernández I, Masanet MJ, Lacruz M, Bellver F, et al. Two strategies for family intervention in schizophrenia: A randomized trial in a Mediterranean environment. Schizophr Bull. 2001;27:661–70. doi: 10.1093/oxfordjournals.schbul.a006905. [DOI] [PubMed] [Google Scholar]
- 45.Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. Am J Psychiatry. 2007;164:1340–7. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419–26. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaselionyte J, Conneely M, Giacco D. “It's a matter of building bridges…“ – Feasibility of a carer involvement intervention for inpatients with severe mental illness. BMC Psychiatry. 2019;19:268. doi: 10.1186/s12888-019-2257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Giacco D, Dirik A, Kaselionyte J, Priebe S. How to make carer involvement in mental health inpatient units happen: A focus group study with patients, carers and clinicians. BMC Psychiatry. 2017;17:101. doi: 10.1186/s12888-017-1259-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krgar Barzi H, Choubdary A, Samari Safa J. The effectiveness of family therapy based on Bowen's emotional treatment on developmental functions of family and maladaptive emotional schemes among women with major depressive disorder. Family Psychol. 2019;6:3–14. [Google Scholar]
- 50.Kidd SA, Kerman N, Ernest D, Maples N, Arthur C, de Souza S, et al. A pilot study of a family cognitive adaptation training guide for individuals with schizophrenia. Psychiatr Rehabil J. 2018;41:109–17. doi: 10.1037/prj0000204. [DOI] [PubMed] [Google Scholar]
- 51.Cohen AN, Glynn SM, Hamilton AB, Young AS. Implementation of a family intervention for individuals with schizophrenia. J Gen Intern Med. 2010;25(Suppl 1):32–7. doi: 10.1007/s11606-009-1136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Speziale HS, Streubert HJ, Carpenter DR. Qualitative Research in Nursing: Advancing the Humanistic Imperative. China: Lippincott Williams and Wilkins; 2011. [Google Scholar]