Abstract
Background
Vertebral body tethering (VBT) has been originally developed as a growth modulation technique for the surgical management of skeletally immature patients with adolescent idiopathic scoliosis (AIS). Given the positive results obtained in this setting, the use of VBT is gradually expanding to other patient categories, such as those with no or limited remaining growth or with non-idiopathic scoliosis. Aim of this manuscript is to offer an overview over the current applications of VBT, along with imaging and comments derived from the clinical experience. The work was based on a literature search conducted in January 2023 on Pubmed, Scopus and Web of Science databases. Following keywords were used for the search: vertebral body tethering, adolescent idiopathic scoliosis, early onset scoliosis, neuromuscular scoliosis, syndromic scoliosis.
Results
Three patient categories in which VBT has been applied have been highlighted: VBT for growth modulation in AIS, VBT as anterior scoliosis correction in AIS and VBT for non-idiopathic curves or early-onset scoliosis.
Conclusion
While growth modulation in AIS still represents the most widespread use of VBT, the use of this technique has yielded positive results in different settings as well, such as scoliosis correction in AIS or temporary or definitive curve management in non-AIS curves. While long-term results are lacking, patient selection seems to play a central role to reduce the complication rate and ensure predictable and stable results.
Keywords: VBT, Scoliosis, Growth modulation, VBT-ASC, Anterior scoliosis correction, EOS, AIS
1. Introduction
Vertebral Body Tethering (VBT) is a relatively new and increasingly popular technique for scoliosis correction in selected adolescent idiopathic scoliosis (AIS) patients. VBT has been originally engineered for the correction of scoliosis through growth modulation1,2 and represents a development of vertebral body stapling (VBS). This approach was developed based on the experience with unilateral growth modulation in knee joint deformities, aiming to limit the vertebral growth on the convex side of the curve to obtain curve correction as skeletal maturity progresses.3, 4, 5 While posterior spinal fusion still represents the gold standard for the surgical management of scoliosis, this technique only allows the restoration of a correct alignment of the spine and not of its function. The aim of VBT is more ambitious, as the goal is to get as close as possible to a normal spine not only in terms of shape, but also in terms of function.
In the past years, numerous studies have reported positive radiographic outcomes after VBT,6,7 not only on the coronal but also on the sagittal plane.8 It has also been shown that, when successful, VBT can indeed induce growth modulation5 and maintain spine mobility.9,10 Further advantages of VBT over posterior spine fusion (PSF) are that VBT allows a full and quick resumption of activities of daily living and sports11 and, so far, does not lead to adjacent segment degeneration.12,13 Despite being an anterior technique, VBT does not impact the pulmonary function even in case of bilateral surgery with deflation of both lungs.14
Given the positive experience with VBT as a growth modulation technique and its potential advantages over PSF, the employment of VBT is gradually being tested in other patient groups, such as non-idiopathic scoliosis or AIS patients who have already reached skeletal maturity. However, the current different possible applications of VBT have not yet been summarized. Aim of this narrative review is to offer an overview and clinical examples of different applications for VBT, from the most common and studied use for AIS correction in skeletally immature patients with flexible curves to new frontiers such as curve correction in AIS patients who have reached skeletal maturity, management of non-idiopathic curves or temporary curve control in early onset scoliosis (EOS) patient.
The present work is based on literature research performed in January 2023. Following databases were accessed: Pubmed, Scopus, Web of Science. The following keywords were used in combination: vertebral body tethering, adolescent idiopathic scoliosis, early onset scoliosis, neuromuscular scoliosis, syndromic scoliosis. Only clinical studies were included in the work.
2. Results
2.1. VBT for growth modulation in AIS
Growth modulation in skeletally immature AIS patients with flexible curves represents the classic indication for VBT,15 and thus also the one that has been most extensively performed and studied. In this setting, curve correction is achieved by the asymmetrical growth modulation guided by the Hueter-Volkmann principle.
Many data regarding the use of VBT for growth modulation have been obtained from a highly selected patient cohort defined by the FDA humanitarian device exemption (HDE).16 These AIS patients are 8–16 years old, skeletally immature (Sanders ≤4) and present 35–60° thoracic curves or lumbar curves <35°.6,16,17 However, only about 20% of AIS patients requiring surgery meet these criteria18 and various authors outside the USA have published positive data on larger thoracic and lumbar curves as well.7,8,19, 20, 21, 22
Overall, comprehensive reviews reported optimistic data on the radiographic results for VBT in growing patients. A recent work reported data on 843 patients with a minimum 1-year follow-up23: VBT showed positive results both for thoracic and lumbar curves, with correction rates ranging from 50 to 80%.23 Another review with a minimum 2 years follow-up including data from 163 patients calculated that 72% of the treated subjects had a non-progressive curve at skeletal maturity.24
However, VBT still shows a relatively high complications rate (18%), with most complications being represented by pulmonary or implant-related issues.23,25 The rate of pulmonary complications has been reported to be up to 10%,26 but all patients have recovered without long-term sequelae.26,27
The revision rate has been reported at up to 18%, with most reoperations being conducted for overcorrection, lumbar add-on or loss of correction after tether breakage.17,24,25,28 The rate of overcorrection is strongly related to the level of skeletal maturity at index surgery, with the frequency of this complication plummeting when VBT is not performed until the triradiate cartilage (TRC) is closed.29 Tether breakage occurs more frequently in the lumbar spine and in larger, less flexible curves.30 While this complication is fairly common, only ruptures occurring within one year from index surgery seem to lead to a consistent loss of correction.31 However, the exact factors leading to loss of correction or add-on scoliosis have not yet been clearly identified.
The comparisons between VBT and posterior spine fusion (PSF) are still limited. PSF allowed a better curve correction and more stable results over time,32,33 but VBT could prevent or delay PSF in most cases.33 The rate of complication and revision rate after VBT was higher than that observed after PSF.28,33 Spine mobility was, as expected, better preserved after VBT,11,34,35 and patient reported outcome measures (PROMs) were equal to or better than those recorded after PSF.33,34,36
In sum, VBT for growth modulation showed very promising clinical results and was proved to deliver the promises of a preserved mobility and high postoperative quality of life. The rate of complications and reoperations were still higher than those observed for PSF and patient selection process likely plays a critical role in improving the success rate. However, the complication rate needs to be interpreted in regard of the different considered parameters (geometry, motion and growth). The ultimate goal of VBT is to normalize the spine in terms of shape and function, so the question is: what is acceptable for the surgeon and the patient to reach that objective? For example, removal of the screws after normalization of the lower limb axis is not considered a complication of femoral epiphysiodesis. In the same way, cutting the tether in case of overcorrection would normalize the alignment of the spine. Still, we would like to stress that complications or reoperations that could be avoided with an improvement of the patient selection process should not be accepted and that not all curves are eligible for VBT. The patients and their families need to be informed of the different options available and the expected outcomes, complications, and revisions. Because there is a choice, patients and parents need to be involved in the decision.
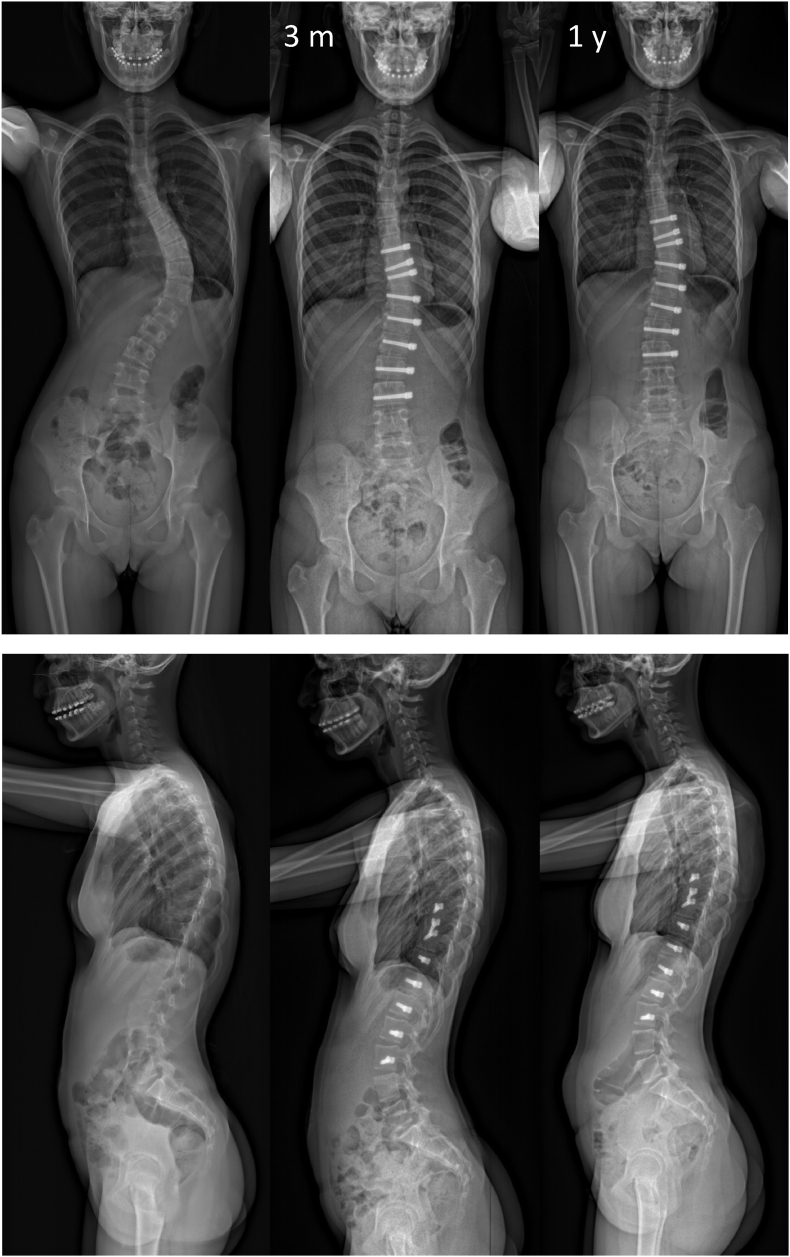
Examples of the use of VBT for growth modulation is shown in Fig. 1, Fig. 2.
Fig. 1.
Example of a 12 year-old girl, Risser 0, with a Lenke 1A curve. One year after VBT, the curve is well corrected and the patient is Risser 4.
Fig. 2.
Example of a 14-year-old boy (Risser 0) with a Lenke 5C curve measuring 52° at index surgery. At the last, 2-year follow-up the curve measured 12° and the patient was Risser 4. The sagittal parameters remained stable and, in particular, the lumbar lordosis was not affected by the use of an anterior instrumentation.
2.2. VBT for curve correction, a.k.a. anterior scoliosis correction (ASC), in AIS
A more recent and still debated use of VBT is that of curve correction in young AIS patients who have already reached or are approaching skeletal maturity. The term VBT-ASC has been recently introduced to differentiate this approach from the traditional growth modulation technique.37 However, a consensus on the definition of “skeletal maturity” in this setting has not yet been obtained, with the threshold varying between Risser ≥3 37,38 and Risser ≥4 39. From a biologic point of view, ASC probably relies on soft tissue modulation (Davis’ law) rather than bone remodeling to achieve curve correction,40 so that a direct intraoperative correction of the curve is required for these patients. The objective is to keep motion where it is still present: flexibility is mandatory. In this regard, most lumbar curves and some thoracic curves are eligible.
Four manuscripts have specifically focused on the use of VBT in this setting: all have shown positive results, however, as expected, no further curve improvement was obtained after index surgery.37, 38, 39,41 At the last available follow-up (1–5 years), curves treated with VBT-ASC measured between 16° and 29° on average.37, 38, 39 While tether breakage was documented in most series,38,41 only one patient required revision surgery for loss of correction.41
Two works compared the results obtained in immature and mature patients.37,38 Bernard et al. observed very similar radiographic results in the two cohorts (19° vs 16° at a mean 5-year follow-up in immature and mature patients, respectively); the failure rate (Cobb >35°) was also the same in the two groups, but secondary surgery or conversion to fusion were reported only among skeletally immature patients.37 Von Treuheim et al. observed a better curve correction (15° vs 29°) and a better success rate (Cobb <35°, 94% vs 79%) in the skeletally immature group, but a similar rate of tether breakage (12%) and no revision surgeries at the 2-year follow-up.38 As age and skeletal maturity do not represent risk factors for early tether breakage,30 the rate of this complication is not expected to differ among immature and mature patients and von Treuheim's study confirms this finding.
As the instrumented curves are not expected to further improve and as overcorrection is not a concern in this group of patients,29 surgeons should aim for full correction of the curve at index surgery40 (Fig. 3). It is important to highlight that, as growth is a continuous rather than a dichotomous variable, a balancing of growth modulation and intraoperative correction is present in almost all VBT surgeries.
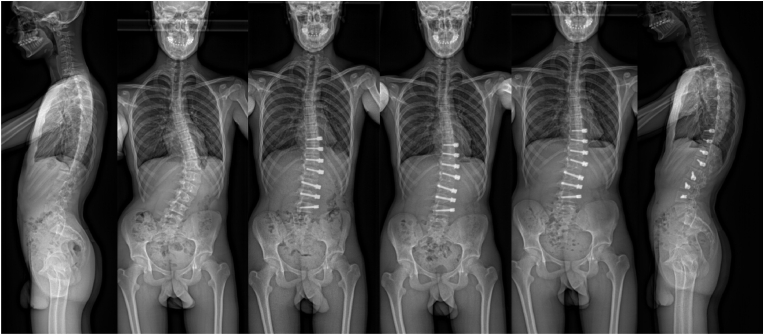
Fig. 3.
Schematic representation of the per-operative correction needed in relationship to the remaining growth modulation. The more growth is expected, the smaller the intraoperative correction required – also to limit the risk of overcorrection. However, in more mature patients with limited or no growth potential, a higher amount of intraoperative correction is required as a further improvement after surgery will likely not occur or be very limited.
Overall, while first reports are optimistic, data are still too limited to reach a definite conclusion on the use of VBT in skeletally mature patients. VBT-ASC might be of particular interest in skeletally mature patients with lumbar curves, in an effort to avoid PSF of the lumbar spine. In this case, the philosophy of VBT is similar to that of selective thoracic fusion (STF), where the focus is placed on maintaining the lumbar spine unfused. However, long term data on the ability of lumbar VBT-ASC to prevent curve progression or degeneration are not yet available.
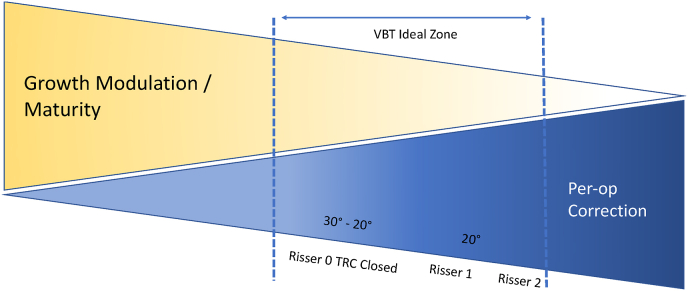
Fig. 4 shows an example of the use of VBT-ASC.
Fig. 4.
Example of a 14 years-old patient (Risser 4) with a Lenke 1A curve measuring 41° at index surgery. At the 2-year follow-up, the curve is well corrected and the compensatory lumbar curve is completely straightened.
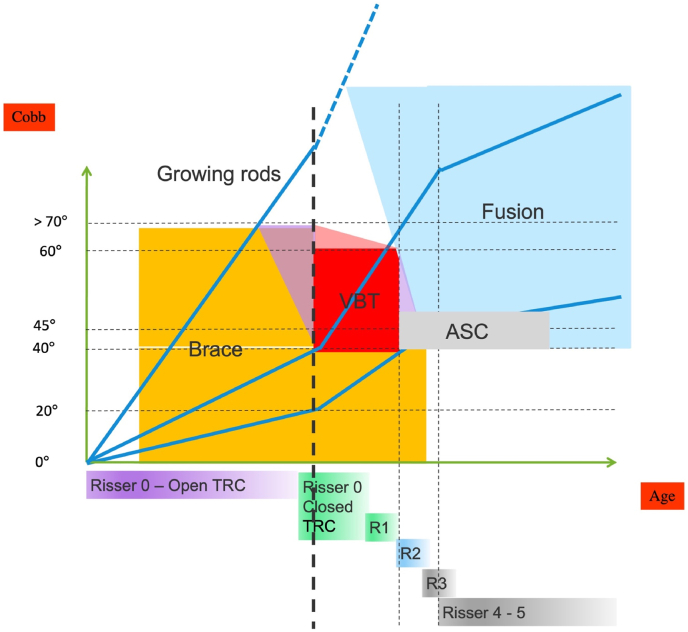
Fig. 5 offers an overview of the different available management strategies for idiopathic scoliosis. It is clear from this image that the treatment options sometimes overlap and it is thus important to discuss with the patients and their families what techniques are available and what the risk/benefit ratio of each treatment is in each patient.
Fig. 5.
Schematic representation of the different treatment options for scoliosis based on the skeletal maturity of the patients and their curve magnitude. The blue lines represent the Duval-Beaupère evolution of three different evolutive curve patterns, while the thick dotted black line represents the start of growth spurts. The ideal VBT curve is the one already severe (<40°) at Risser 0. Other patients have slower-evolving curves that are not severe enough at Risser 0, but will cross the 40–45° threshold later. These patients will require either PSF or ASC, depending on curve type and flexibility.
2.3. VBT for non-AIS cases
While VBT has originally been developed for AIS patients, a recent publication described its use in patients with non-idiopathic scoliosis.42 For idiopathic-like curves, the selection process would be similar to that used for AIS. The use of VBT in neurological or neuromuscular cases is more complex, but of value is some specific cases and in particular for ambulant patients. When considering VBT for these patients, the surgeon must take into account the natural evolution of the curve in the specific pathology, along with spine geometry, motion, and growth. This complexity explains the heterogeneity of the published series. Furthermore, this patient collective is often more prone to infections than AIS patients43,44 and may thus profit from a less invasive surgical approach. VBT may also help reducing postoperative pain and improve mobilization, thus limiting the risk for pulmonary complications, which are also not infrequent among non-idiopathic patients.45
The available data are encouraging, with 45% of patients who achieved a <35° curve after surgery.42 However, patients with neuromuscolar scoliosis and those with larger curves obtained poorer results.42 Further research will be required to better identify which non-idiopathic patients can profit the most from VBT.
Another multicentric study investigated the results of VBT in EOS patients and compared them to those obtained with magnetically-controlled growing rods (MCGR).46 MCGR is knowingly associated with a high complication and reoperation rate,47 which in turn may lead to conspicuous soft tissue scarring, problematic wound healing and in most cases spontaneous fusion. The employment of VBT instead of MCGR would hopefully show a lower complication rate and would allow to maintain mobility and intact dorsal tissue until definitive PSF can be performed. Mackey et al. observed a better curve correction and a lower rate of implant-related complications and unplanned surgeries than in patients who underwent MCGR.46 The number of planned surgeries was also smaller for VBT patients, but this might have been partially due to the slightly older age and smaller curve magnitude of the subjects in this group.46 However, performing VBT in small patients may lead to technical issues as vertebral bodies are small and medical devices available are bulky in regard to the rib cage.
Another advantage of VBT in EOS treatment is to prevent the development of structural lumbar curves and leave the possibility of STF at skeletal maturity. In fact, growth modulation first occurs at the thoraco-lumbar junction, where flexibility is key and vertebral bodies are not wedged. Thus, VBT could control the progression of the curve in the lumbar spine thus prevent the necessity of lumbar fusion at skeletal maturity. This is not possible with MCGR constructs, where instrumentation of the lumbar spine is a common requirement.
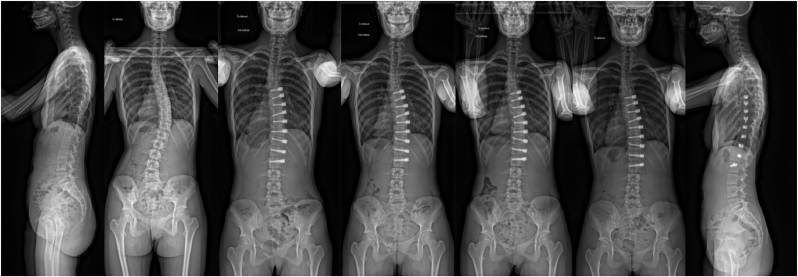
These first studies suggest that VBT might be an option for the management of selected non-AIS patients, but the outcomes might be less predictable that in AIS patients. Also in this setting, patient information plays a central role to ensure the understanding of the surgical strategy and the perception of what a success will be. Clinical examples are shown in Fig. 6, Fig. 7.
Fig. 6.
Example 12-years old patient affected by Williams-Beuren syndrome. At index surgery the TRC were open and the patient presented a 65° Lenke 2B curve. At the last, 4-year follow up, both the main thoracic and the compensatory curve are stable and, if necessary, thoracic fusion could still be performed at skeletal maturity.
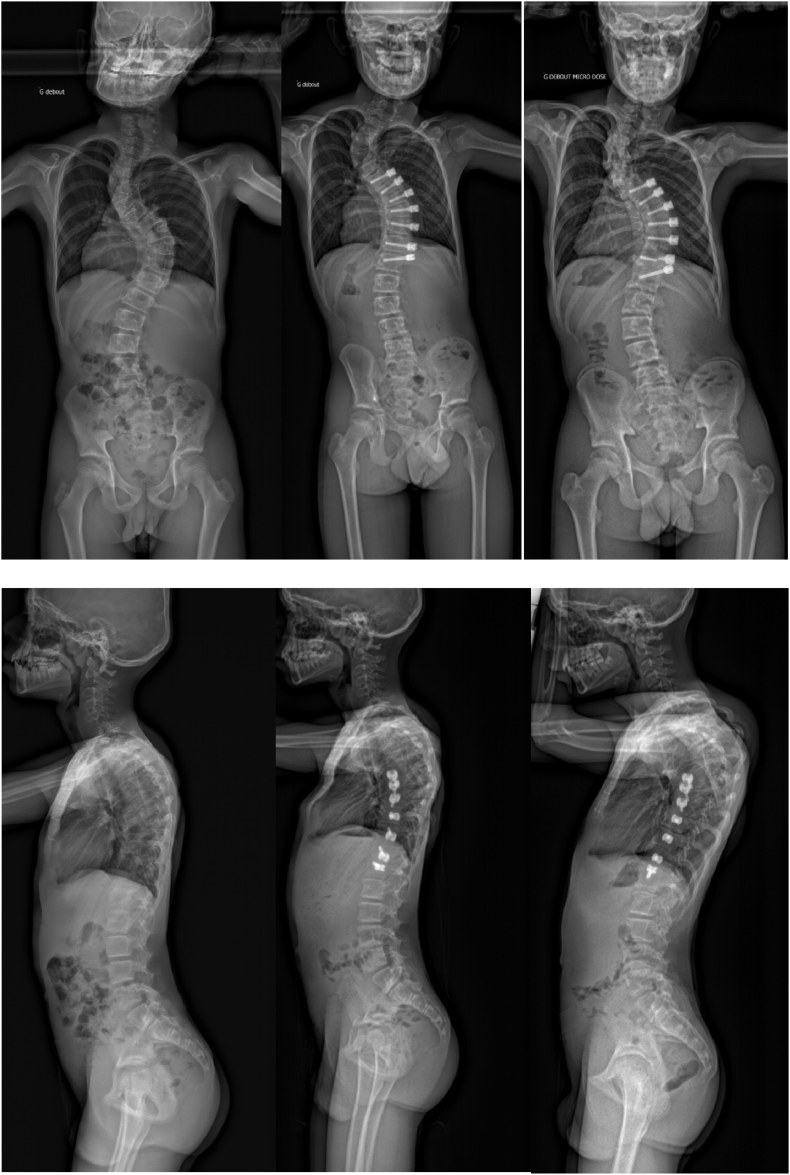
Fig. 7.
Example of a 14-years-old patient (Risser 0, closed TRC) affected by a genetic disorder and with a progressing 65° lumbar curve. At the last, 3-year follow-up, the lumbar curve is controlled and, while there is a slight overcorrection at the thoracolumbar junction, this allows for a better coronal balance. As the patient is almost non-ambulant, a maintained coronal alignment is of particular significance as it facilitates sitting.
3. Conclusion
VBT is proving to be a flexible tool that may, in the future, be employed in different settings than those for which it was originally developed. However, VBT is a more subtle technique than fusion and patient selection is critical to ensure success. Research for the identification of the ideal candidate for VBT is still ongoing and potentially different uses of VBT will require different patients’ characteristics in terms of curve type, magnitude and flexibility in order to be successful.
Institutional ethical committee approval (for all human studies)
Not applicable.
Funding/sponsorship
This research did not obtain any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Authors contribution
AB conceptualization, data acquisition, original draft; AC conceptualization, data acquisition, critical draft revision.
Informed consent
The parents gave their written informed consent for X-ray publication.
Declaration of competing interest
AB, AC: none.
Acknowledgements
None.
References
- 1.Samdani A.F., Ames R.J., Kimball J.S., et al. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine. 2014;39(20):1688–1693. doi: 10.1097/BRS.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 2.Samdani A.F., Ames R.J., Kimball J.S., et al. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24(7):1533–1539. doi: 10.1007/s00586-014-3706-z. [DOI] [PubMed] [Google Scholar]
- 3.Betz R.R., Kim J., D'Andrea L.P., Mulcahey M.J., Balsara R.K., Clements D.H. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine (Phila Pa 1976. 2003;28(20):S255–S265. doi: 10.1097/01.BRS.0000092484.31316.32. [DOI] [PubMed] [Google Scholar]
- 4.Newton P.O., Farnsworth C.L., Faro F.D., et al. Spinal growth modulation with an anterolateral flexible tether in an immature bovine model: disc health and motion preservation. Spine (Phila Pa 1976. 2008;33(7):724–733. doi: 10.1097/BRS.0b013e31816950a0. [DOI] [PubMed] [Google Scholar]
- 5.McDonald T.C., Shah S.A., Hargiss J.B., et al. When successful, anterior vertebral body tethering (VBT) induces differential segmental growth of vertebrae: an in vivo study of 51 patients and 764 vertebrae. Spine Deform. 2022;10(4):791–797. doi: 10.1007/s43390-022-00471-2. [DOI] [PubMed] [Google Scholar]
- 6.Abdullah A., Parent S., Miyanji F., et al. Risk of early complication following anterior vertebral body tethering for idiopathic scoliosis. Spine Deform. 2021;9(5):1419–1431. doi: 10.1007/s43390-021-00326-2. [DOI] [PubMed] [Google Scholar]
- 7.Miyanji F., Pawelek J., Nasto L.A., Rushton P., Simmonds A., Parent S. Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. The bone & joint journal. 2020;102-B(12):1703–1708. doi: 10.1302/0301-620X.102B12.BJJ-2020-0426.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baroncini A., Courvoisier A., Berjano P., et al. The effects of vertebral body tethering on sagittal parameters: evaluations from a 2-years follow-up. Eur Spine J. 2022;31(4):1060–1066. doi: 10.1007/s00586-021-07076-9. [DOI] [PubMed] [Google Scholar]
- 9.Buyuk A.F., Milbrandt T.A., Mathew S.E., Larson A.N. Measurable thoracic motion remains at 1 Year following anterior vertebral body tethering, with sagittal motion greater than coronal motion. J Bone Jt Surg Am Vol. 2021;103(24):2299–2305. doi: 10.2106/JBJS.20.01533. [DOI] [PubMed] [Google Scholar]
- 10.Mathew S.E., Milbrandt T.A., Larson A.N. Measurable lumbar motion remains 1 Year after vertebral body tethering. J Pediatr Orthop. 2022;42(8):e861–e867. doi: 10.1097/BPO.0000000000002202. [DOI] [PubMed] [Google Scholar]
- 11.Baroncini A., Trobisch P.D., Berrer A., et al. Return to sport and daily life activities after vertebral body tethering for AIS: analysis of the sport activity questionnaire. Eur Spine J. 2021;30(7):1998–2006. doi: 10.1007/s00586-021-06768-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yucekul A., Akpunarli B., Durbas A., et al. Does vertebral body tethering cause disc and facet joint degeneration? A preliminary MRI study with minimum two years follow-up. Spine J. 2021;21(11):1793–1801. doi: 10.1016/j.spinee.2021.05.020. [DOI] [PubMed] [Google Scholar]
- 13.Jackson T.J., Milbrandt T.A., Mathew S.E., Heilman J.A., Larson A.N. Intervertebral disk health following vertebral body tethering for adolescent idiopathic scoliosis: a preliminary study. J Pediatr Orthop. 2022;42(7):347–353. doi: 10.1097/BPO.0000000000002172. [DOI] [PubMed] [Google Scholar]
- 14.Baroncini A., Trobisch P., Blau C., et al. Analysis of the pulmonary function in patients undergoing vertebral body tethering for adolescent idiopathic scoliosis. Eur Spine J. 2022;31(4):1022–1027. doi: 10.1007/s00586-021-07029-2. [DOI] [PubMed] [Google Scholar]
- 15.Newton P.O. Spinal growth tethering: indications and limits. Ann Transl Med. 2020;8(2):27. doi: 10.21037/atm.2019.12.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cahill P. ClinicalTrials.gov. Vertebral Body Tethering Outcomes for Pediatric Idiopathic Scoliosis.
- 17.Samdani A.F., Pahys J.M., Ames R.J., et al. Prospective follow-up report on anterior vertebral body tethering for idiopathic scoliosis: interim results from an FDA IDE study. J Bone Jt Surg Am Vol. 2021;103(17):1611–1619. doi: 10.2106/JBJS.20.01503. [DOI] [PubMed] [Google Scholar]
- 18.Krakow A.R., Magee L.C., Cahill P.J., Flynn J.M. Could have tethered: predicting the proportion of scoliosis patients most appropriate for thoracic anterior spinal tethering. Spine Deform. 2021;9(4):1005–1012. doi: 10.1007/s43390-021-00296-5. [DOI] [PubMed] [Google Scholar]
- 19.Pehlivanoglu T., Oltulu I., Erdag Y., et al. Double-sided vertebral body tethering of double adolescent idiopathic scoliosis curves: radiographic outcomes of the first 13 patients with 2 years of follow-up. Eur Spine J. 2021;30(7):1896–1904. doi: 10.1007/s00586-021-06745-z. [DOI] [PubMed] [Google Scholar]
- 20.Hoernschemeyer D.G., Boeyer M.E., Robertson M.E., et al. Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2 to 5-year postoperative results. J Bone Jt Surg Am Vol. 2020;102(13):1169–1176. doi: 10.2106/JBJS.19.00980. [DOI] [PubMed] [Google Scholar]
- 21.Rushton P.R.P., Nasto L., Parent S., Turgeon I., Aldebeyan S., Miyanji F. Anterior vertebral body tethering for treatment of idiopathic scoliosis in the skeletally immature: results of 112 cases. Spine (Phila Pa 1976. 2021;46(21):1461–1467. doi: 10.1097/BRS.0000000000004061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trobisch P.D., Baroncini A. Preliminary outcomes after vertebral body tethering (VBT) for lumbar curves and subanalysis of a 1- versus 2-tether construct. Eur Spine J. 2021;30(12):3570–3576. doi: 10.1007/s00586-021-07009-6. [DOI] [PubMed] [Google Scholar]
- 23.Raitio A., Syvänen J., Helenius I. Vertebral body tethering: indications, surgical technique, and a systematic review of published results. JCM. 2022;11(9):2576. doi: 10.3390/jcm11092576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bizzoca D., Piazzolla A., Moretti L., Vicenti G., Moretti B., Solarino G. Anterior vertebral body tethering for idiopathic scoliosis in growing children: a systematic review. World J Orthoped. 2022;13(5):481–493. doi: 10.5312/wjo.v13.i5.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baroncini A., Trobisch P.D., Birkenmaier C., Da Paz S., Migliorini F. Radiologische Ergebnisse nach Vertebral Body Tethering. Z für Orthop Unfallchirurgie. 2022;160(4):387–392. doi: 10.1055/a-1387-8334. [DOI] [PubMed] [Google Scholar]
- 26.Trobisch P., Migliorini F., Vanspauwen T., Baroncini A. Pulmonary complications after vertebral body tethering: incidence, treatment, outcomes and risk factor analysis. JCM. 2022;11(13) doi: 10.3390/jcm11133778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyers J., Eaker L., Di Treuheim TP von, Dolgovpolov S., Lonner B. Early operative morbidity in 184 cases of anterior vertebral body tethering. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-02358-0. Published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shin M., Arguelles G.R., Cahill P.J., Flynn J.M., Baldwin K.D., Anari J.B. Complications, reoperations, and mid-term outcomes following anterior vertebral body tethering versus posterior spinal fusion: a meta-analysis. JB JS Open Access. 2021;6(2) doi: 10.2106/JBJS.OA.21.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alanay A., Yucekul A., Abul K., et al. Thoracoscopic vertebral body tethering for adolescent idiopathic scoliosis: follow-up curve behavior according to sanders skeletal maturity staging. Spine (Phila Pa 1976. 2020;45(22):E1483–E1492. doi: 10.1097/BRS.0000000000003643. [DOI] [PubMed] [Google Scholar]
- 30.Baroncini A., Trobisch P., Eschweiler J., Migliorini F. Analysis of the risk factors for early tether breakage following vertebral body tethering in adolescent idiopathic scoliosis. Eur Spine J. 2022;31(9):2348–2354. doi: 10.1007/s00586-022-07231-w. [DOI] [PubMed] [Google Scholar]
- 31.Baroncini A., Migliorini F., Eschweiler J., Hildebrand F., Trobisch P. The timing of tether breakage influences clinical results after VBT. Eur Spine J. 2022;31(9):2362–2367. doi: 10.1007/s00586-022-07321-9. [DOI] [PubMed] [Google Scholar]
- 32.Mathew S.E., Hargiss J.B., Milbrandt T.A., Stans A.A., Shaughnessy W.J., Larson A.N. Vertebral body tethering compared to posterior spinal fusion for skeletally immature adolescent idiopathic scoliosis patients: preliminary results from a matched case-control study. Spine Deform. 2022;10(5):1123–1131. doi: 10.1007/s43390-022-00519-3. [DOI] [PubMed] [Google Scholar]
- 33.Newton P.O., Bartley C.E., Bastrom T.P., Kluck D.G., Saito W., Yaszay B. Anterior spinal growth modulation in skeletally immature patients with idiopathic scoliosis: a comparison with posterior spinal fusion at 2 to 5 Years postoperatively. J Bone Jt Surg Am Vol. 2020;102(9):769–777. doi: 10.2106/JBJS.19.01176. [DOI] [PubMed] [Google Scholar]
- 34.Pehlivanoglu T., Oltulu I., Erdag Y., et al. Comparison of clinical and functional outcomes of vertebral body tethering to posterior spinal fusion in patients with adolescent idiopathic scoliosis and evaluation of quality of life: preliminary results. Spine Deform. 2021;9(4):1175–1182. doi: 10.1007/s43390-021-00323-5. [DOI] [PubMed] [Google Scholar]
- 35.Pahys J.M., Samdani A.F., Hwang S.W., Warshauer S., Gaughan J.P., Chafetz R.S. Trunk range of motion and patient outcomes after anterior vertebral body tethering versus posterior spinal fusion: comparison using computerized 3D motion capture technology. J Bone Jt Surg Am Vol. 2022;104(17):1563–1572. doi: 10.2106/JBJS.21.00992. [DOI] [PubMed] [Google Scholar]
- 36.Qiu C., Talwar D., Gordon J., Capraro A., Lott C., Cahill P.J. Patient-reported outcomes are equivalent in patients who receive vertebral body tethering versus posterior spinal fusion in adolescent idiopathic scoliosis. Orthopedics. 2021;44(1):24–28. doi: 10.3928/01477447-20201119-02. [DOI] [PubMed] [Google Scholar]
- 37.Bernard J., Bishop T., Herzog J., et al. Dual modality of vertebral body tethering. Bone Jt Open. 2022;3(2):123–129. doi: 10.1302/2633-1462.32.BJO-2021-0120.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Di Treuheim TP von, Eaker L., Markowitz J., Shankar D., Meyers J., Lonner B. Anterior vertebral body tethering for scoliosis patients with and without skeletal growth remaining: a retrospective review with minimum 2-year follow-up. Internet J Spine Surg. 2022 doi: 10.14444/8357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hegde S.K., Venkatesan M., Akbari K.K., Badikillaya V.M. Efficacy of anterior vertebral body tethering in skeletally mature children with adolescent idiopathic scoliosis: a preliminary report. Internet J Spine Surg. 2021;15(5):995–1003. doi: 10.14444/8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baroncini A., Trobisch P.D., Migliorini F. Learning curve for vertebral body tethering: analysis on 90 consecutive patients. Spine Deform. 2021;9(1):141–147. doi: 10.1007/s43390-020-00191-5. [DOI] [PubMed] [Google Scholar]
- 41.Meyers J., Eaker L., Zhang J., Di Pauli von Treuheim T., Lonner B. Vertebral body tethering in 49 adolescent patients after peak height velocity for the treatment of idiopathic scoliosis: 2-5 Year follow-up. J Clin Med. 2022;11(11) doi: 10.3390/jcm11113161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pulido N.A., Vitale M.G., Parent S., et al. Vertebral body tethering for non-idiopathic scoliosis: initial results from a multicenter retrospective study. Spine Deform. 2022 doi: 10.1007/s43390-022-00575-9. [DOI] [PubMed] [Google Scholar]
- 43.Sponseller P.D., Shah S.A., Abel M.F., Newton P.O., Letko L., Marks M. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res. 2010;468(3):711–716. doi: 10.1007/s11999-009-0933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fruergaard S., Ohrt-Nissen S., Pitter F.T., et al. Length of stay, readmission, and mortality after primary surgery for pediatric spinal deformities: a 10-year nationwide cohort study. Spine J. 2021;21(4):653–663. doi: 10.1016/j.spinee.2021.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Samdani A.F., Belin E.J., Bennett J.T., et al. Major perioperative complications after spine surgery in patients with cerebral palsy: assessment of risk factors. Eur Spine J. 2016;25(3):795–800. doi: 10.1007/s00586-015-4054-3. [DOI] [PubMed] [Google Scholar]
- 46.Mackey C., Hanstein R., Lo Y., et al. Magnetically controlled growing rods (MCGR) versus single posterior spinal fusion (PSF) versus vertebral body tether (VBT) in older early onset scoliosis (EOS) patients: how do early outcomes compare? Spine (Phila Pa 1976. 2022;47(4):295–302. doi: 10.1097/BRS.0000000000004245. [DOI] [PubMed] [Google Scholar]
- 47.Lebel D.E., Rocos B., Helenius I., et al. Magnetically controlled growing rods graduation: deformity control with high complication rate. Spine (Phila Pa 1976. 2021;46(20):E1105–E1112. doi: 10.1097/BRS.0000000000004044. [DOI] [PubMed] [Google Scholar]