INTRODUCTION
Previous studies have shown that low-value imaging for uncomplicated acute low back pain may trigger cascades of spine-related medical services with uncertain value and potential for harm1 among injured workers,2 veterans,3 and Medicare Advantage members.4 Building on this work, we examined cascades fully (e.g., including incidental extra-spinal findings) to estimate both total and out-of-pocket spending on cascades following low-value X-rays and magnetic resonance imaging (MRI) for uncomplicated acute low back pain among commercially-insured adults.
METHODS
We analyzed 100% medical claims (1/1/2017–12/31/2019) for Blue Cross Blue Shield of Massachusetts members 18–50-year-olds who received a 2018 diagnosis of uncomplicated acute low back pain for which imaging was considered inappropriate per the National Committee for Quality Assurance Healthcare Effectiveness Data and Information Set (HEDIS) “Use of Imaging Studies for Low Back Pain” criteria. We required continuous enrollment over a lookback period of 365 days preceding each low back pain diagnosis and over subsequent cascade periods of 3, 6, or 12 months.
Among eligible members, we compared service utilization and spending (allowed charges) between those who did and did not have an index low-value imaging study (X-ray or MRI) 0–28 days after their low back pain diagnosis. We defined cascade-associated services narrowly (services billed with spinal or extra-spinal diagnoses that literature suggested may follow from low back imaging)3,5 and broadly (all medical services during cascade period). Using linear probability models, we controlled for member age, sex, socioeconomic status, plan type, Charlson Comorbidity Index, prior year (2017) total medical expenditure, and calendar year quarter of diagnosis. We performed falsification tests by examining adjusted associations between low-value low back pain imaging and two services—knee X-ray and antibiotics (HEDIS utilization measure)—that reflect clinician ordering propensity yet would not plausibly follow from low back imaging.
We stratified cascade-associated out-of-pocket spending by high deductible health plan (HDHP) status. We compared distributions of spending across medical service categories (excluding spending on index imaging) in the 3-month cascade period between members with and without index imaging.
We followed STROBE reporting guidelines. Mass General Brigham institutional review board waived review.
RESULTS
In 2018, 30,892 members were eligible for low-value imaging (52.0% were female; mean age 35.8). Of these, 6009 (19.5%) received low-value imaging: 5091 (16.5%) X-ray and 787 (2.5%) MRI. Mean spending per index imaging study was $124 for X-ray and $952 for MRI.
Compared to patients without low-value imaging, those with low-value X-ray or MRI had higher adjusted probabilities of receiving cascade services and greater adjusted total spending at 3, 6, and 12 months ($220 for X-ray and $1093 for MRI narrowly-defined at 12 months, $470 for X-ray and $4391 broadly-defined; Table 1). These results were robust to falsification testing: knee X-ray and antibiotic use were not associated with low-value low back pain imaging receipt.
Table 1.
Characteristics, Cascade Service Utilization, and Cascade-Associated Spending Among Recipients with No Imaging versus Low-value X-ray or MRI for Low Back Pain
| Cascade period, months* | No imaging N= 23,715 | X-ray N=5091 | MRI N=787 | X-ray – no imaging, adjusted difference, 95% CI † | MRI – no imaging, adjusted difference, 95% CI † | |
|---|---|---|---|---|---|---|
| Age group (years), no. (%) | ||||||
| 18–25 | 4183 (17.6) | 1007 (19.8) | 98 (12.5) | |||
| 26–35 | 6841 (28.8) | 1321 (25.9) | 160 (20.3) | |||
| 36–45 | 8374 (35.3) | 1810 (35.6) | 347 (44.1) | |||
| 46–50 | 4317 (18.2) | 953 (18.7) | 182 (23.1) | |||
| Sex, no. (%) | ||||||
| Male | 11,283 (47.6) | 2480 (48.7) | 436 (55.4) | |||
| Female | 12, 432 (52.4) | 2611 (51.3) | 351 (44.6) | |||
| SES Index, no. (%)‡ | ||||||
| Lowest (Q1) | 5738 (24.2) | 1431 (28.1) | 147 (18.7) | |||
| Q2 | 5518 (23.3) | 1237 (24.3) | 185 (23.5) | |||
| Q3 | 5378 (22.7) | 1123 (22.1) | 182 (23.1) | |||
| Q4 | 5197 (21.9) | 906 (17.8) | 207 (26.3) | |||
| Plan type, no. (%) | ||||||
| Health Maintenance Organization | 9176 (38.7) | 1583 (31.1) | 298 (37.9) | |||
| Preferred Provider Organization | 14,539 (61.3) | 3508 (68.9) | 489 (62.1) | |||
| Charlson Comorbidity Index, mean (SD) | 0.30 (0.68) | 0.33 (0.70) | 0.43 (0.91) | |||
| Prior year total medical expenditure ($) | ||||||
| Mean (SD) | 2303 (9,317) | 2249 (7,737) | 2349 (5877) | |||
| Median (IQR) | 461 (1,557) | 420 (1,487) | 501 (1923) | |||
| Members with one or more cascade-associated service, narrowly defined, no. (%) | 3 | 6403 (27.0) | 1833 (36.0) | 324 (41.2) | 9.0 (7.5, 10.5) | 12.9 (9.4, 16.4) |
| 6 | 7345 (33.0) | 1997 (41.8) | 362 (49.4) | 8.8 (7.2, 10.4) | 14.2 (10.5, 18.0) | |
| 12 | 7240 (41.3) | 1877 (50.3) | 329 (57.0) | 9.0 (7.2, 10.9) | 12.7 (8.4, 17.1) | |
| Cascade-associated total spending, narrowly defined ($)§ | 3 | 195 | 368 | 1180 | 167 (150, 183) | 973 (934, 1013) |
| 6 | 311 | 510 | 1390 | 183 (154, 212) | 1,050 (982, 1119) | |
| 12 | 501 | 735 | 1662 | 220 (168, 271) | 1,093 (973, 1213) | |
| Cascade-associated out-of-pocket spending, narrowly defined ($)§ | 3 | 61 | 125 | 351 | 61 (54, 67) | 282 (268, 296) |
| 6 | 84 | 151 | 390 | 63 (56, 71) | 298 (280, 317) | |
| 12 | 120 | 189 | 426 | 67 (55, 79) | 297 (271, 323) | |
| Cascade-associated total spending, broadly defined ($)§ | 3 | 1543 | 1910 | 4619 | 341 (230, 452) | 2,865 (2,605, 3124) |
| 6 | 2934 | 3284 | 6540 | 317 (133, 501) | 3,280 (2,848, 3711) | |
| 12 | 5461 | 5962 | 10,750 | 470 (138, 802) | 4,391 (3,616, 5167) | |
| Cascade-associated out-of-pocket spending, broadly defined ($)§ | 3 | 278 | 421 | 772 | 134 (118, 150) | 469 (431, 507) |
| 6 | 482 | 631 | 1002 | 137 (113, 162) | 490 (433, 547) | |
| 12 | 852 | 1015 | 1449 | 152 (112, 193) | 539 (445, 634) | |
We excluded 131 (0.4% of 30,892 members) receiving low-value computerized tomography scan for uncomplicated acute low back pain due to the infrequency of this imaging modality
*Cascade periods were defined as 3, 6, or 12 months after the index date of service (for imaging groups) or 3, 6, or 12 months after low back pain diagnosis date (for no imaging group, chosen because there was a median of 0 days between imaging and diagnosis dates in the imaging groups). Analyses of the 6-month cascade period included 27,770 members (N=22,259 with no imaging, N=4778 with x-ray, N=733 with MRI). Analyses of the 12-month cascade period included 21,838 members (N=17,530 with no imaging, N=3731 with x-ray, N=577 with MRI)
†Adjusted differences were estimated using multivariable ordinary least squares regression models adjusting for age, sex, socioeconomic status (SES) index (quartiles using 2018 data, composite score calculated from Principal Component Analysis with census block group-level factors including race/ethnicity, education, unemployment status, single-family household, income and poverty level), plan type (Health Maintenance Organization versus Preferred Provider Organization), Charlson Comorbidity Index (calculated during the lookback period), prior year total medical expenditure (calculated during the lookback period), and calendar year quarter of the date of low back pain diagnosis (to account for seasonal shifts in utilization patterns)
‡SES Index missing for 2344 members (7.9%). Missing values were included in the models using an indicator variable
§Cascade-associated spending estimates included spending on index imaging (if performed) to account for non-independence of the index and cascade-associated service spending
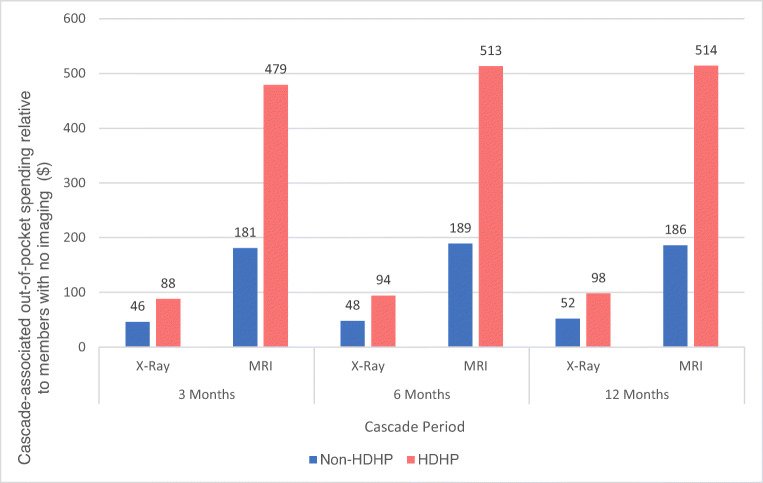
Members with HDHP insurance had higher narrowly-defined cascade-associated out-of-pocket spending than those in other plans ($98 vs $52 for X-ray, $514 vs $186 for MRI at 12 months; Figure 1). The most common sources of narrowly-defined cascade-associated spending were physical therapy, office visits, radiology studies, laboratory studies, and surgery. Relative to those without imaging, MRI and X-ray recipients spent a larger share on office visits (11.6% and 11.9% vs 7.9%), X-ray recipients spent a larger share on downstream radiology (7.0% vs 3.4% no imaging and 3.5% MRI), and MRI recipients spent a larger share on injections (8.9% vs 0.6% no imaging and 1.8% X-ray) and surgery (9.1% vs 3.6% no imaging and 2.9% X-ray) (all p values <0.001).
Figure 1.
Cascade-associated narrowly-defined out-of-pocket spending by x-ray and MRI recipients relative to members with no imaging for low back pain, stratified by health plan type. “HDHP” indicates a high deductible health plan with an individual deductible greater than or equal to $1350. “Non-HDHP” indicates a health plan with an individual deductible lower than $1350. This $1350 cut-off was based on the 2018 and 2019 Internal Revenue Service definition of a high deductible health plan.
DISCUSSION
Among commercially-insured adults with uncomplicated low back pain, imaging recipients were 9–14 percentage points likelier to receive downstream services potentially related to low back pain or to spinal or extra-spinal imaging results. X-ray and MRI recipients had substantially higher total and out-of-pocket spending on cascade-associated services post-imaging.
Study limitations include potential unobserved confounding and limited generalizability to non-commercially-insured populations. Claims data lack details confirming clinician intent and are susceptible to human billing errors and shortcuts. Nevertheless, while no measure is perfect, evidence suggests that HEDIS criteria-defined low-value imaging offers minimal if any potential for benefit and significant potential for harm.6
In sum, we find substantial total and out-of-pocket spending following low-value low back pain imaging in healthy commercially-insured adults that can inform efforts to reduce low-value imaging and cascades.
Funding
This work was supported by the Agency for Healthcare Research and Quality grant 1R01HS023812 and grant K23AG068240 from The National Institute on Aging.
Data Availability
Not available.
Declarations
Conflict of Interest
Ishani Ganguli reported receiving consulting fees from F-Prime and Blue Cross Blue Shield of Massachusetts.
Ishani Ganguli and Kathleen Mulligan reported receiving a grant from the Robert Wood Johnson Foundation outside of the submitted work.
Wei Ying, Tara Shakley, James A. Colbert, and Mark W. Friedberg are employed by Blue Cross Blue Shield of Massachusetts.
Reproducible Research Statement
Study Protocol: Not applicable.
Statistical Code
Available upon request.
Footnotes
Prior presentations
Poster presentation, Academy Health Annual Research Meeting 2022
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ganguli I, Simpkin AL, Lupo C, et al. Cascades of care after incidental findings in a US National Survey Of Physicians. JAMA Netw Open. 2019;2(10):e1913325. 10.1001/jamanetworkopen.2019.13325. [DOI] [PMC free article] [PubMed]
- 2.Webster BS, Choi Y, Bauer AZ, Cifuentes M, Pransky G. The Cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine (Phila Pa 1976). 2014;39(17):1433-1440. [DOI] [PMC free article] [PubMed]
- 3.Jacobs JC, Jarvik JG, Chou R, et al. Observational study of the downstream consequences of inappropriate MRI of the lumbar spine. J Gen Intern Med. 2020;35(12):3605-3612. 10.1007/s11606-020-06181-7. [DOI] [PMC free article] [PubMed]
- 4.Comino EJ, Davies GP, Krastev Y, et al. A systematic review of interventions to enhance access to best practice primary health care for chronic disease management, prevention and episodic care. BMC Health Serv Res. 2012;12(1):415. 10.1186/1472-6963-12-415. [DOI] [PMC free article] [PubMed]
- 5.Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol. 2015;36(4):811-816. 10.3174/ajnr.A4173. [DOI] [PMC free article] [PubMed]
- 6.Chou R, Qaseem A, Owens DK, Shekelle P. Diagnostic imaging for low back pain: Advice for high-value health care from the American college of physicians. Ann Intern Med. 2011;154(3):181-189. 10.7326/0003-4819-154-3-201102010-00008. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not available.