Abstract
Purpose
Increasing ownership and use of mobile phones has been recently linked to reports of hand and wrist pain from overuse, as well as more serious injuries related to distracted behaviors, such as falls and texting while driving. We describe the epidemiology of hand and wrist injuries presenting to US emergency departments from 2011 to 2020, which were associated with cell phone use using the Consumer Product Safety Commission’s National Electronic Injury Surveillance System.
Methods
The National Electronic Injury Surveillance System database was queried for treatment records from 2011 through to 2020 for all cell phone-related injuries of the lower arm, wrist, hand, and fingers. Using parameters provided by the National Electronic Injury Surveillance System database, there were 1,213 unique cases, yielding a total weighted estimate of 50,487 national cases presenting to emergency departments in the United States.
Results
Between 2011 and 2020, the weighted estimate of annual cell phone-related injuries ranged from 3,389 to 7,320 cases. Falls were the most common cause of injury, accounting for 29.8% of estimated cases. The most common types of injuries were lacerations (22.3%). The national estimate of cell phone-related injury was the highest in the age range of 11–20 years (26.4%), followed by 21–30 years (22.2%). Women were affected more frequently than men (59.6% vs 40.4%).
Conclusions
Upper extremity injuries related to cell phone use represent an increasing burden of disease to the US healthcare system. Raising awareness regarding cell phone-related injuries and in-home fall-prevention strategies, especially among elderly individuals, should be considered as means of decreasing the number of such injuries. Strategies for decreasing the burden of cell phone−related injuries occurring as a result of falls among teenagers and young adults should focus on minimizing distractions while using a cell phone. Limitations of the study include inaccuracies related to probability-weighted case estimation and limitations in reporting injuries.
Clinical relevance
Knowledge of the burden of upper extremities injuries associated with this common handheld device can help to both raise awareness of this issue, as well as to potentially inform injury-prevention strategies.
Key words: Cell phone, Epidemiology, Hand, Hand trauma, Wrist
The advent of mobile phones in 1973, and particularly the smartphone in 1995, revolutionized communication systems around the world. In 2018, an estimated 4.57 billion people, approximately 67% of the global population, owned a cell phone.1 Mobile devices have also changed behaviors; in 2016, a poll revealed that 50% of teenagers and 27% of parents reported feeling addicted to their cell phones.2 A subsequent study by Parasuraman et al3 revealed that 70% of college students used cell phones for longer than intended and women were significantly more likely to be dependent on their phones than men.
Addictive cell phone use has recently been linked to reports of injuries related to overuse. A survey of a large population in Finland identified self-reported wrist and finger aches and pains in 723 people, 80% of whom reported frequent phone use.4 Excessive gaming on a cell phone has been linked to tendon rupture,5 and smartphone overuse has been linked to the enlarged median nerve, thumb pain at rest, and decreased pinch strength.6 Among college-aged students, 46% of those who felt addicted to their cell phones reported symptoms similar to De Quervain tenosynovitis and 26% reported other hand and wrist pains.3 Mobile phone overuse can cause more serious injuries and even death. A retrospective review by Dokur et al7 reviewed the cases of 159 individuals worldwide who had been reported in the media for selfie-related injuries. Of these, the most common injuries were caused by falling off a height, such as a cliff side, and the most frequent causes of death were accidental drowning or polytrauma.7 Selfies have also been linked to less severe upper extremity trauma; a small case series by Lyona et al8 identified 4 cases of distal radius fractures after accidents that occurred while taking a selfie. These articles were widely publicized in late 2018 by media websites such as Microsoft Network and Fox News as an emerging hazard of smartphone overuse, particularly affecting the hand and wrist.
The role of cell phones in motor vehicle accidents has been widely documented, as is the relationship between frequent cell phone use and mental health disorders. However, to date, cell phone-related injuries of the hand and wrist have only been investigated through self-reported surveys or case series. There is no large-scale epidemiological study in the literature detailing the injury patterns and diagnoses associated with cell phone use. Based on previous case reports associating cell phone use with hand and wrist pain, we sought to characterize the demographics, injury patterns, and mechanism of injury in a large population with cell phone-related hand or wrist injuries.
We hypothesized that the disease burden of cell phone-related hand and wrist injuries presenting to US emergency departments would have increased from 2011 to 2022, and in this study, sought to characterize national trends in cell phone-related hand and wrist injuries presenting to US emergency departments from 2011 through 2022 using the Consumer Product Safety Commission’s (CPSC) National Electronic Injury Surveillance System (NEISS) and determine national case estimates for injuries by diagnosis, injury mechanism, and location (ie, distal to the forearm, wrist, hand, and finger).
Materials and Methods
The NEISS is an electronic database maintained by the US CPSC, which queries a sample of hospitals in the United States.9 Data are collected from 100 emergency departments of varying capacities across the country to represent a probable sample of all hospital emergency rooms nationwide. Data collected include patient demographics (age, sex, and race); injury characteristics, such as diagnosis, body part involved, a brief description of the injury, and date of injury; and location of the accident occurrence. Hospitals are stratified by the number of annual emergency room visits and assigned a sample weight for each injury as a predictor for the true number of similar injuries nationwide. The CPSC updates this sampling frame and strata annually. The ratio-adjusted sampling weights are validated by CPSC statisticians to represent appropriately the total number of emergency room visits for an injury in a given year.9
For this study,9 the NEISS database was queried for all injuries pertaining to the “lower arm” (code: 33), “wrist” (code: 34), “hand” (code: 82), or “finger” (code: 92), associated with products pertaining to cell phones over a 10-year period from January 1, 2010 to December 31, 2020. Cell phones are represented by the NEISS code 550. This code also applies to telephone accessories, such as phone cases, answering machines, chargers, pagers, and telephone speaker devices.10 The ratio-adjusted weight estimates were summed to produce an estimate of the total number of national cases annually and combined for an overall 10-year analysis.
Each case in the queried data was assigned a unique identifier to prevent cases from being counted multiple times. Patients who had injuries unrelated to cell phones or smartphones, such as those caused by landlines, pay phones, or answering machines, were excluded. Injuries proximal to the forearm were excluded. Each of the corresponding patient narratives were reviewed independently and the diagnosis and mechanism of injury were confirmed.
National estimates were derived from the NEISS database survey parameters. A Mann-Kendall trend test was used to assess the presence of a trend in the annual estimate of cell phone-related injuries occurring in the United States, with the significance of two-tailed testing set at α = .05.
In the subgroup analysis of cell phone-related injuries in which the mechanism of injury was falling, cases describing injuries of the distal upper extremities were further stratified into 10-year age groups and subdivided using the following preset NEISS categories: “falling while distracted on phone,” “falling while reaching for phone,” and “falling while trying to answer phone.”
Results
Study cohort
The query of the NEISS database for cell phone-related injuries of the lower arm, wrist, hand, and finger(s) yielded a total of 1,213 unique emergency department visits. Based on the NEISS ratio-adjusted algorithms, this represented a total weighted estimate of 50,487 cases presenting to emergency departments in the United States between January 1, 2011 and December 31, 2020. A total of 44 individual cases were excluded following narrative screening because their injuries did not pertain to a cell phone, or the location of their injury did not involve the lower arm, hand, wrist, or finger(s). Cell phone-related injuries were the most prevalent in the age range of 11–20 years (26.4%), followed by 21–30 years (22.2%), and women were affected more frequently than men (59.6% vs 40.4%) (Table 1). Most of the estimated cases (97%) were discharged directly from the emergency department, with or without treatment.
Table 1.
Demographic Characteristics of Weighted National Estimates, Grouped According to Sex, Age, and Race
| Characteristics | N (%) |
|---|---|
| Total | 50,487 (100) |
| Sex | |
| Male | 20,409 (40.4) |
| Female | 30,078 (59.6) |
| Age, (y) | |
| 1–10 | 2,454 (4.9) |
| 11–20 | 13,334 (26.4) |
| 21–30 | 11,223 (22.2) |
| 31–40 | 6,968 (13.8) |
| 41–50 | 5,046 (10) |
| 51–60 | 3,304 (6.5) |
| 61–70 | 3,331 (6.6) |
| 71–80 | 1,955 (3.9) |
| >80 | 2,874 (5.7) |
| Race | |
| White | 23,704 (47) |
| Black/African American | 8,284 (16.6) |
| Asian | 323 (9.6) |
| Native American | 142 (0.3) |
| Native Hawaiian or Pacific Islander | 91 (0.2) |
| Other | 2,201 (4.4) |
| Not stated | 15,642 (31) |
National trend for cell phone-related injuries of the hand and wrist
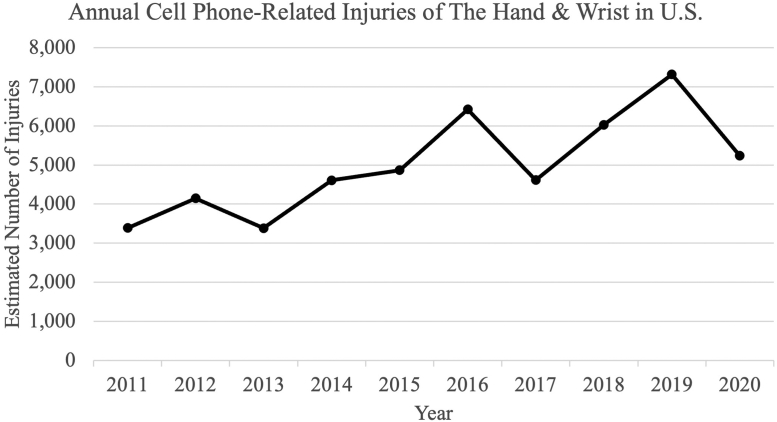
Between 2011 and 2020, the weighted estimate of annual cell phone-related injuries ranged from 3,389 to 7,320 cases (Fig. 1), with Mann-Kendall testing demonstrating that there was a trend in the national estimates of cell phone-related injuries of the hand and wrist occurring annually from 2011 to 2020 (P = .007).
Figure 1.
The annual national estimate of hand and wrist injuries related to cell phones and cell phone accessories in the United States (US) (as weighted case estimates) occurring between January 1, 2011 and December 31, 2020.
Analysis of injury mechanisms
Table 2 depicts the national estimate of each mechanism of cell phone-related injuries of the distal upper extremity (lower arm, wrist, hand, and finger[s]). Falls were the most common cause of injury, accounting for an estimated 15,047 (29.8%) cases nationwide. Injury from a broken phone or attempts made to repair a broken phone accounted for 8,412 (16.7%) injuries, followed by 7,124 (14.1%) injuries as a consequence of texting (Table 2).
Table 2.
Mechanism of Cell Phone-Related Injuries of the Hand and Wrist in the United States Between January 1, 2011, and December 31, 2020, by Incidence
| Injuries Related to Cell Phone Use | National Case Estimate N (%) |
|---|---|
| Total (2011–2020) | 50,487 (100) |
| Falls | 15,047 (29.8) |
| Broken phone∗ | 8,412 (16.7) |
| Texting | 7,124 (14.1) |
| Phone accessory–related† | 2,897 (5.7) |
| MCC or MVC while distracted on the phone | 2,117 (4.2) |
| Altercation over phone | 1,780 (3.5) |
| Cutting | 1,485 (2.9) |
| Gaming | 1,298 (2.6) |
| Burns (nonscalding) or explosion | 832 (1.6) |
| Bites and/or stings (animal, insect) | 333 (0.7) |
| Overuse of cell phone | 315 (0.6) |
| Burns (scalding) | 232 (0.5) |
| Other | 8615 (17.1) |
MCC, motorcycle crash; MVC, motor vehicle crash.
Includes injuries occurring due to attempts made to fix a broken phone.
Includes injuries occurring as a result of exposure to a cell phone accessory (eg, charging device or phone case) or attempted repair thereof, rather than an injury resulting directly from the association with a cell phone.
Comparative estimates of fall-related injuries among different age groups
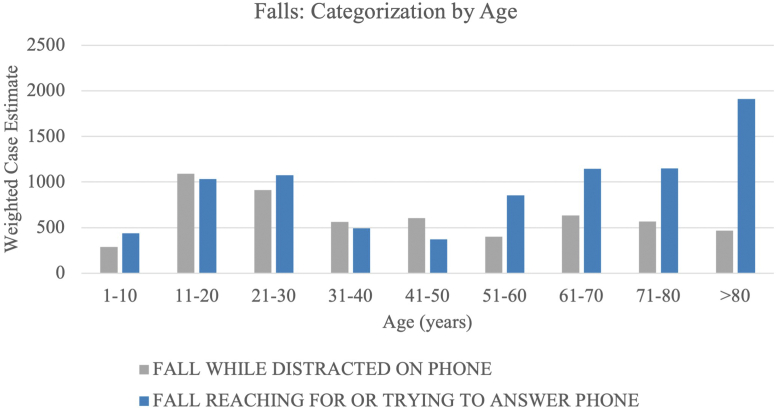
Overall, the weighted national estimate for the total cell phone-related injuries of the distal upper extremities with a fall-related mechanism between 2011 and 2020 was the greatest in the >80-years age group (n = 2,378 [17%]), followed by the 11–20-year (n = 2,126 [15.2%]) and 21–30-years (n = 1,988 [14.2%]) age groups.
Figure 2 presents a distribution of the weighted national estimate of cell phone-related injuries with a fall-related mechanism occurring in US emergency departments between January 1, 2011 and December 31, 2020, stratified by the 10-year age groups (ie, categorization by age). Preset NEISS categories for the fall-related injury mechanisms “fall while reaching for phone” and “fall while trying to answer phone,” were combined into 1 mechanism-of-injury category, namely, “fall reaching for or trying to answer phone,” which had the highest case estimate among individuals aged >80 years (n = 1,909). In contrast, cell phone-related injuries of the distal upper extremity with falling as the mechanism of injury were more commonly categorized as “falls while distracted on phone” for the 11–20-year and 21–30-year age groups, for which the estimated number of cases in the United States from 2011 to 2022 was 1,092 and 912, respectively.
Figure 2.
Categorization of estimated cell phone-related injuries with falling as the mechanism of injury occurring in the United States between January 1, 2011 and December 31, 2020, stratified by 10-year age groups.
Cell phone-related injury patterns
For each unique emergency department visit, a primary diagnosis was coded for the encounter within the NEISS database, as provided by each participating hospital. Table 3 provides a distribution of the weighted national estimate for cell phone-related injuries of the distal upper extremity, stratified by primary diagnosis and body part affected.
Table 3.
Distribution of Weighted National Estimate for Cell Phone-Related Injury Cases by NEISS-Coded Primary Diagnosis
| Primary Diagnosis | Overall Case Estimate N (%) |
Lower Arm | Wrist | Hand | Finger |
|---|---|---|---|---|---|
| Total, n (%) | 50,487 (100.0) | 6,785 (13.4) | 10,800 (21.4) | 15,511 (30.7) | 17,391 (34.4) |
| Laceration | 11,235 (22.3) | 1,114 (2.2) | 741 (1.5) | 4,012 (7.9) | 5,369 (10.6) |
| Fracture | 7,610 (15.1) | 2,002 (4.0) | 2,379 (4,7) | 1,972 (3.9) | 1,257 (2.5) |
| Contusion | 7,587 (15.0) | 1,377 (2.7) | 1,276 (2.5) | 3,378 (6.7) | 1,555 (3.1) |
| Strain or sprain | 5,664 (11.2) | 254 (0.5) | 2,541 (5.0) | 635 (1.3) | 2,235 (4.4) |
| Nerve damage | 2,064 (4.1) | 363 (0.7) | 1,014 (2.0) | 458 (0.9) | 229 (0.5) |
| Foreign body | 1,982 (3.9) | 0 (0.0) | 0 (0.0) | 262 (0.5) | 1,720 (3.4) |
| Thermal burns | 1,272 (2.5) | 239 (0.5) | 135 (0.3) | 565 (1.1) | 333 (0.7) |
| Avulsion | 1,056 (2.1) | 0 (0.0) | 0 (0.0) | 675 (1.3) | 381 (0.8) |
| Electrical burns | 840 (1.7) | 0 (0.0) | 0 (0.0) | 284 (0.6) | 556 (1.1) |
| Puncture | 826 (1.6) | 0 (0.0) | 0 (0.0) | 372 (0.7) | 453 (0.9) |
| Dislocation | 676 (1.3) | 55 (0.1) | 67 (0.1) | 84 (0.2) | 471 (0.9) |
| Hematoma | 170 (1.3) | 0 (0.0) | 71 (0.1) | 17 (0.0) | 82 (0.2) |
| Scald burns | 104 (0.3) | 0 (0.0) | 0 (0.0) | 104 (0.2) | 0 (0.0) |
| Electric shock | 80 (0.2) | 0 (0.0) | 0 (0.0) | 80 (0.2) | 0 (0.0) |
| Frostbite | 78 (0.2) | 32 (0.0) | 0 (0.0) | 47 (0.0) | 0 (0.0) |
| Crushing | 78 (0.2) | 0 (0.0) | 62 (0.1) | 0 (0.0) | 16 (0.0) |
| Dermatitis | 67 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 67 (0.1) |
| Amputation | 15 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 15 (0.0) |
| Other/not stated | 9,085 (18.0) | 1,349 (2.7) | 2,514 (5.0) | 2,567 (5.1) | 2,654 (5.3) |
Laceration was the most common primary diagnosis (n = 11,235 [22.3% of estimated total injuries]) and was most common in the finger(s) (n = 5,369 [10.6%]), followed by the hand (n = 4,012 [7.9%]), lower arm (n = 1,114 [2.2%]), and wrist (n = 741 [1.5%]). It is estimated that 15 individuals were trying to carve a steak in the dark while using their cell phone as a flashlight, whereas another 16 were attempting to grab a phone out of their back pocket and instead grabbed a knife (Table 3).
Fracture was the second most common injury (n = 7,610 [15.1%]), followed by contusion (n = 7,587 [15.0%]), and strain or sprain (n = 5,664 [11.2%]). Nerve damage accounted for 2, 064 (4.1%) of the injuries, of which 1,210 injuries (63.3%) were diagnosed as carpal tunnel syndrome and 159 (8.3%) as radial nerve palsy.
Uncommon injuries were also reported. Electric sparks from cell phone chargers caused 1,036 (48.6%) of the estimated 2,132 burn injuries. Self-inflicted gunshot wounds while using a cell phone were reported in an estimated 35 patients. An estimated 78 individuals sustained frostbite to their fingers, 32 of whom sustained frostbite after losing a cell phone in the snow and then searching for it without gloves.
Discussion
This descriptive epidemiological study demonstrated that cell phone-related injuries occurred more commonly in women than men, and the most common age groups in which cell phone-related injuries were estimated to occur nationally were among teenagers and young adults. This is consistent with a previous study by Parasuraman et al,3 who reported that young women were significantly more dependent on their phones than men. Our study also found that the national estimate of cell phone-related injuries of the distal upper extremities has been increasing over the study period.
The most common mechanism for cell phone-related injuries of the distal upper extremities was falling, and the injury burden among individuals who fell while reaching for or trying to answer a cell phone was highest in those aged >80 years, followed by the 71–80- and 61–70-year age groups. This underscores the importance of increasing awareness of cell phone-related injuries in these age groups, as well as instituting in-home preventative strategies that would allow individuals aged >60 years to safely obtain and use their cell phones. These preventative strategies could support the aim of decreasing injury burden and may include strategies, such as ensuring an obstacle-free path to reach one’s phone, which would otherwise cause individuals in these cohorts to experience fall-related injuries. The national estimate of cell phone-related injuries occurring as a result of falls while being distracted on a cell phone was the highest among teenagers and young adults, which suggests that the number of falls occurring among teenagers and young adults has risen with the increasing adoption of and addiction to cell phone use. Furthermore, falls occurring in these groups as a result of being distracted while using cell phones underscores the importance of increased awareness and education regarding the safe use of cell phones and minimizing distraction, such as avoiding multitasking, to reduce the burden of cell phone-related injuries resulting from falls in this group.
The most common primary diagnosis for cell phone-related injuries of the distal upper extremities in the study cohort was laceration (34.4%), especially of the finger(s) (10.7%). These injuries can result in significant amounts of lost work time as well as functional limitations.11,12
An estimated 832 individuals were injured by cell phone explosions and nonscalding burns (ie, thermal and electrical) during the study period. This period coincides with the media-related panic due to an apparent rise in “exploding smartphones” that were linked to lithium battery-powered cellular devices.13,14 It is concerning that a device that is so readily available can have the potential to cause such a catastrophic injury.
Electric sparks from cell phone chargers caused half of the of the 2,000 burn injuries estimated to have occurred nationally due to cell phone use over the study period. To our knowledge, no literature to date has described this phenomenon. Future studies should address the safety of chargers and preventative measures.
This study reports cell phone-related injuries of the hand and wrist at a national level. It offers insight and potential foreshadowing for increasing injuries and at-risk persons. However, our study has certain limitations. We relied on a stratified probability sample of a consortium of hospitals to collectively represent US emergency departments. Although probability-weighted case estimates are likely to differ from the actual number of hand and wrist injuries linked to cell phone usage, assuming that the consortium of hospitals comprising the sample of US emergency departments represents the whole of US emergency departments, the NEISS database provides the most robust system for estimating injury cases presenting to US emergency departments. Furthermore, this study was meant to reflect cell phone-related hand and wrist injury cases presenting to US emergency departments. As with several forms of injury, the actual number of injury cases is not adequately represented by cases presenting to US emergency departments, as many cases do not present to emergency departments, and those presenting to emergency departments can be biased (eg, injuries presenting to emergency departments are possibly more severe than those that do not present). The most common injuries (eg, tendonitis) may have been underestimated due to the fact that they are less likely to present to the emergency department. Additionally, within the NEISS database, smaller case numbers are less weighted, and thus, may be less reliable or underestimated. Finally, there will always be a degree of uncertainty accompanying estimates from a probability sample, as well as biases of a dataset that are open to interpretation.
In summary, upper extremity injuries related to cell phone use represent an increasing burden of disease to the US healthcare system. Raising awareness regarding cell phone-related injuries and in-home fall-prevention strategies, especially among elderly individuals, should be considered as a means of decreasing the number of such injuries. Strategies for decreasing the burden of cell phone-related injuries due to falls in teenagers and young adults should focus on minimizing distractions while using a cell phone.
Footnotes
Declaration of Interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Statista Research Department Mobile phone users worldwide 2015-2020. Statista. November 23, 2016 https://www.statista.com/statistics/274774/forecast-of-mobile-phone-users-worldwide/ [Google Scholar]
- 2.Wallace Kelly. Half of teens think they’re addicted to their smartphones. Cable News Network. July 29, 2016 https://www.cnn.com/2016/05/03/health/teens-cell-phone-addiction-parents/index.html [Google Scholar]
- 3.Parasuraman S., Sam A.T., Yee S.W.K., Chuon B.L.C., Ren L.Y. Smartphone usage and increased risk of mobile phone addiction: a concurrent study. Int J Pharm Investig. 2017;7(3):125–131. doi: 10.4103/jphi.JPHI_56_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korpinen L., Pääkkönen R., Gobba F. Self-reported wrist and finger symptoms associated with other physical/mental symptoms and use of computers/mobile phones. Int J Occup Saf Ergon JOSE. 2018;24(1):82–90. doi: 10.1080/10803548.2017.1282030. [DOI] [PubMed] [Google Scholar]
- 5.Gilman L., Cage D.N., Horn A., Bishop F., Klam W.P., Doan A.P. Tendon rupture associated with excessive smartphone gaming. JAMA Intern Med. 2015;175(6):1048–1049. doi: 10.1001/jamainternmed.2015.0753. [DOI] [PubMed] [Google Scholar]
- 6.İnal E.E., Demİrcİ K., Çetİntürk A., Akgönül M., Savaş S. Effects of smartphone overuse on hand function, pinch strength, and the median nerve. Muscle Nerve. 2015;52(2):183–188. doi: 10.1002/mus.24695. [DOI] [PubMed] [Google Scholar]
- 7.Dokur M., Petekkaya E., Karadağ M. Media-based clinical research on selfie-related injuries and deaths. Ulus Travma Acil Cerrahi Derg. 2018;24(2):129–135. doi: 10.5505/tjtes.2017.83103. [DOI] [PubMed] [Google Scholar]
- 8.Lyona R.F., Kelly J.C., Murphy C.G. The selfie wrist–selfie-induced trauma. Ir Med J. 2017;110(6):589. [PubMed] [Google Scholar]
- 9.US Consumer Product Safety Commission Division of Hazard and Injury Data Systems The National Electronic Injury Surveillance System a tool for researchers. March 2000. https://www.cpsc.gov/s3fs-public/pdfs/blk_media_2000d015.pdf
- 10.US Consumer Product Safety Commission Division of Hazard and Injury Data Systems National Electronic Injury Surveillance System coding manual. January 2021. https://www.cpsc.gov/s3fs-public/January-2021-NT-CPSC-only-NEISS-Coding-Manual.pdf?xa_nMM1kB4SGpuSMOwf0NHkkkIqNcn8F
- 11.Lilly S.I., Messer T.M. Complications after treatment of flexor tendon injuries. J Am Acad Orthop Surg. 2006;14(7):387–396. doi: 10.5435/00124635-200607000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Sorock G.S., Lombardi D.A., Courtney T.K., Cotnam J.P., Mittleman M.A. Epidemiology of occupational acute traumatic hand injuries: a literature review. Saf Sci. 2001;38(3):241–256. [Google Scholar]
- 13.Mankowski P.J., Kanevsky J., Bakirtzian P., Cugno S. Cellular phone collateral damage: a review of burns associated with lithium battery-powered mobile devices. Burns. 2016;42(4):e61–64. doi: 10.1016/j.burns.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Nicole Bogart. Why lithium-ion smartphone batteries keep exploding. Globalnews. December 8, 2014 https://globalnews.ca/news/1714748/why-lithium-ion-smartphone-batteries-keep-exploding/ [Google Scholar]