Abstract
Here, we present a novel emergency department reduction for a rare case of dissociative scaphoid and lunate dislocation with an ipsilateral elbow dislocation. Dissociative scaphoid and lunate dislocations have rarely been described in the literature. Most often, the reduction is performed on an urgent basis in the operating room because of the difficulty of closed reduction and associated complications, such as acute carpal tunnel syndrome. We illustrate and describe the setup and stepwise reduction techniques of ipsilateral elbow, scaphoid, and lunate dislocations, without the use of an assistant. A review of the current literature, a description of the patient’s operative management, and 2-year follow-up data are provided.
Key words: Dislocation, Elbow, Lunate, Reduction, Scaphoid
Carpal dislocations are high-energy injuries that are rarely encountered in the emergency department. The literature documenting simultaneous scaphoid and lunate dislocation is limited. Domeshek et al1 reported 17 documented cases of simultaneous scaphoid and lunate dislocations. Of these cases, more than half resulted in the scaphoid and lunate dislocating as a unit.2 However, to our knowledge, there are no reported cases describing palmar dissociative scaphoid and lunate dislocations with an additional ipsilateral elbow dislocation. With patient informed consent, we present a closed reduction technique for a unique case of a palmar dissociative dislocation of the scaphoid and lunate in the presence of an ipsilateral elbow dislocation.
Case Report
A 45-year-old healthy right handed man presented to a level 1 trauma center after being involved in a pedestrian versus automobile accident. The patient had acute right elbow pain and deformity. On orthopedic assessment, he also had significant right wrist pain and swelling. Subsequent radiographs demonstrated a right posterolateral elbow dislocation and ipsilateral scaphoid and lunate dislocations (Fig. 1). There were no associated fractures. Although the patient’s physical examination demonstrated significant dysesthesias in the median nerve distribution, he maintained full motor function.
Figure 1.
Injury films of A AP and B lateral radiographs demonstrating a simple posterior elbow dislocation. C AP and D lateral radiographs demonstrating volar dislocation of the lunate and the scaphoid. AP, anterior-posterior.
Injury acuity necessitated a closed reduction of each involved dislocation. He was placed under propofol sedation by emergency medical staff. First, the right elbow dislocation was reduced with the standard technique, including supination and axial traction, whereas the elbow was flexed to approximately 25°. Postreduction radiographs are presented in Figure 2. Next, the patient was placed in finger traps made from Kerlix bandage to simultaneously apply gravity distraction across the radiocarpal joint and maintain elbow reduction (Fig. 3A), which was stable at 90° of flexion.
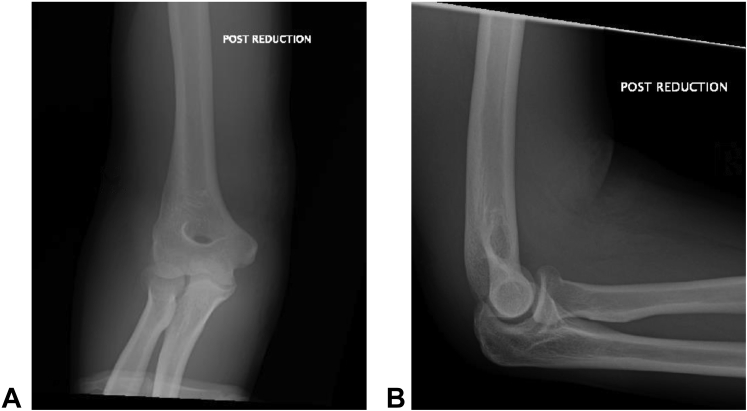
Figure 2.
Postreduction elbow films, including A AP and B lateral radiographs demonstrating congruent closed reduction of the posterior elbow dislocation. AP, anterior-posterior.
Figure 4.
A Lateral view showing volar dislocation of the lunate and the scaphoid. Sequential films demonstrating closed reduction of B the scaphoid first, then C the lunate.
The reduction of the scaphoid and lunate dislocations was difficult. A 2-hand technique was used by a single individual, which consisted of both thumbs placed on the volar aspect of the wrist to “milk” the lunate into and through the carpal tunnel (Fig. 3B, C). The wrist was simultaneously flexed, and the ulnar deviated with a distally directed volar-to-dorsal pressure, now on both the lunate and scaphoid. The scaphoid was reduced at this stage and confirmed with radiographs (Fig. 4A, B). Certainly, the lunate could have reduced first or simultaneously, but the initial scaphoid position made it more susceptible to falling into place first. The lunate was easily palpated and still stuck at the volar lip of the distal radius. With both thumbs pressing proximal to distal on the lunate, combined with a reduction maneuver consisting of wrist flexion–traction–extension, the lunate reduced into the lunate fossa with a palpable clunk (Fig. 3D, E). Postreduction radiographs demonstrated a reduction of both the lunate and scaphoid without fracture complications (Fig. 4C).
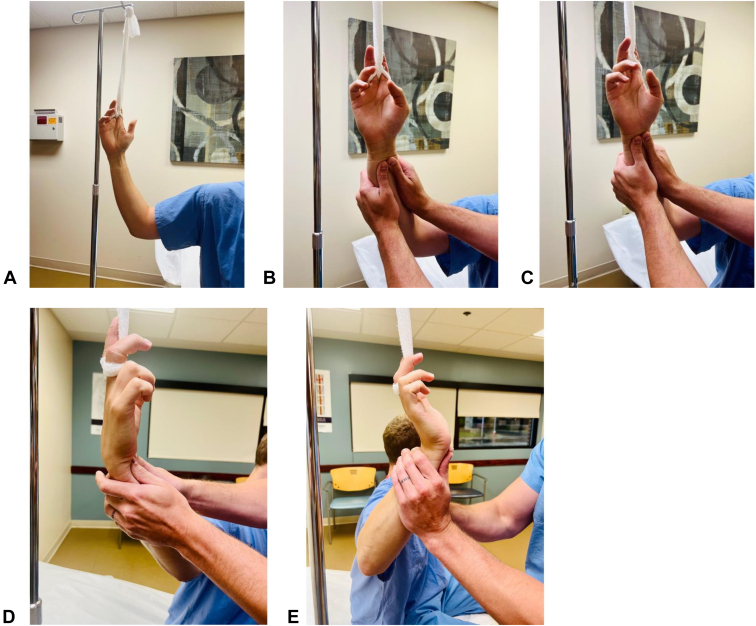
Figure 3.
A Clinical photographs showing the emergency department setup using an IV pole and Kerlix to hang the upper extremity from the index and middle fingers. B–E Photographs demonstrating the reduction technique with traction, B, C milking the distal forearm from proximal to distal, D followed by traction, flexion, and a volar-to-dorsal force on the scaphoid-lunate complex, E then wrist extension. IV, intravenous.
The patient was then placed into a combination long-arm and reverse sugar-tong orthosis. The following day, the surgery was performed. It included the percutaneous placement of four 1.6 mm (0.62-in) K-wires, open repair of the scapholunate ligament with suture anchors, and direct ligament repair as described by Ozyurekoglu et al.3 The lunotriquetral ligament was not reconstructed; rather, the interval was closed with direct suture repair of the available interosseous ligament. A long-arm orthosis and volar forearm slab were applied in the operating room. Postoperative images were obtained in the postanesthesia care unit and demonstrated stable reduction (Fig. 5).
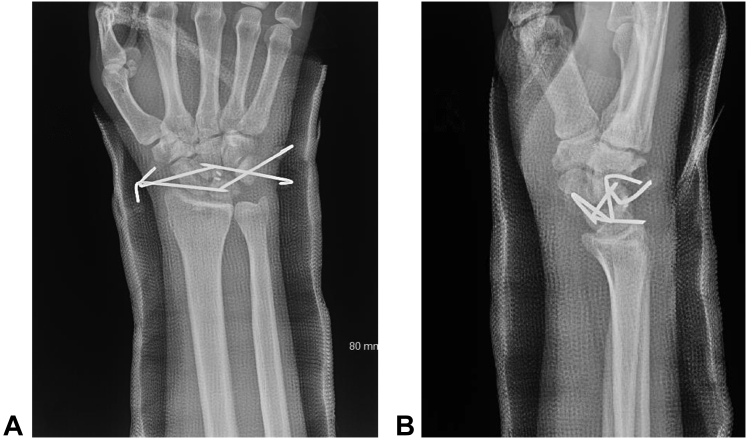
Figure 5.
Postoperative A AP and B lateral radiographs demonstrating pin fixation of the scaphoid and the lunate with additional scapholunate ligament repair using suture anchors. AP, anterior-posterior.
The patient was instructed not to lift, push, or pull anything with his right upper extremity for a total of 10 weeks. At 2 weeks after the surgery, his orthoses were transitioned to a single short-arm cast for 4 additional weeks. The cast was removed, and his pins were taken out at the 6-week postoperative visit. The patient was placed into formal hand therapy to improve his elbow and wrist range of motion. His 10-month postoperative elbow and wrist range of motion was equivalent to the contralateral extremity, and radiographs demonstrated minimal degenerative changes (Fig. 6). His 2-year postoperative Disabilities of the Arm, Shoulder and Hand (DASH) score was 50.8, and the patient fully returned to his original occupation as a fork-lift operator at 10-months after the surgery.
Figure 6.
A, B 10-month and C, D 2-year postoperative AP and lateral films demonstrating minimal degenerative changes to the radiocarpal and intercarpal joints. No obvious avascular necrosis of the lunate or the scaphoid. AP, anterior-posterior.
Discussion
Scaphoid and lunate dislocations are rare circumstances to encounter in the emergency department. Moreover, an ipsilateral elbow dislocation adds to the complexity of reducing and maintaining reduction prior to operative intervention. The literature vaguely discusses reduction maneuvers for lunate or scaphoid dislocations and none with an ipsilateral elbow dislocation. It has been reported that axial traction across the wrist and simultaneous extension while pushing distally on the scaphoid-lunate unit can reduce the unit if the scapholunate ligament is intact.4 Here, there was a disruption of the scapholunate ligament, which made this maneuver less successful. Another technique for palmar dissociative dislocation of the scaphoid and lunate described in the literature was performed in the operating room under general anesthesia. The lunate was reduced first, followed by the scaphoid.5 The difficulty of closed reduction of this injury is further described with many failing closed reduction in the emergency department, followed by open reduction via volar and or dorsal approaches.6
To date, we are aware of only 9 described palmar-divergent dislocations of the scaphoid and lunate.5,7 None of these had an ipsilateral elbow dislocation or thoroughly described a successful, combined reduction maneuver by a single person. Moreover, this technique shows the challenges with a closed reduction when there is complete interosseous ligament disruption of the scaphoid and lunate. In addition, this technique is advantageous when there is significant proximal lunate displacement within the forearm.
As shown in the report by Kao et al,5 many prior patients with palmar dissociative dislocation of the scaphoid and lunate treated with open reduction, K-wire fixation, and ligament repair have sequelae that include either some pain or dorsal intercalated segment instability deformity. Here, our patient had a minimal clinical impact, as demonstrated by his wrist range of motion. However, the patient’s DASH score was surprisingly high, which likely accounts for his ipsilateral complex multilevel joint injury. Although his wrist range of motion was full, his elbow was limited to a 20° to 135° arc of motion. Certainly, this was functional, but it may have impacted his DASH score. Radiographically, no scapholunate widening or dorsal intercalated segment instability deformity was present at 2 years after surgery. Importantly, this report shows that a closed reduction of this unique injury pattern can be accomplished with a single person, without assistance or the need for an urgent open procedure.
Acknowledgments
We acknowledge the patient for allowing us to include this case into the literature to add to global medical knowledge.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Domeshek L.F., Harenberg P.S., Rineer C.A., Hadeed J.G., Marcus J.R., Erdmann D.E. Total scapholunate dislocation with complete scaphoid extrusion: case report. J Hand Surg Am. 2010;35(1):69–71. doi: 10.1016/j.jhsa.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Idrissi K.K., Galiua F. Palmar dislocation of scaphoid and lunate. Clin Pract. 2011;1(4):e87. doi: 10.4081/cp.2011.e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozyurekoglu T., Acar M.A. Treatment of acute perilunate dislocation or fracture dislocation using dorsal approach and diamond-shaped Kirschner-wire fixation. Jt Dis Relat Surg. 2021;32(1):42–50. doi: 10.5606/ehc.2021.74838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarrafian S.K., Breihan J.H. Palmar dislocation of scaphoid and lunate as a unit. J Hand Surg Am. 1990;15(1):134–139. doi: 10.1016/s0363-5023(09)91121-2. [DOI] [PubMed] [Google Scholar]
- 5.Kao S.W., Chang I.C., Wu C.L. Palmar-divergent dislocation of the scaphoid and lunate treated using percutaneous pinning and pin-in-plaster: a case-report. Acta Orthop Traumatol Turc. 2020;54(3):348–352. doi: 10.5152/j.aott.2020.03.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang H.J., Shim D.J., Hahn S.B., Kang E.S. Palmar divergent dislocation of the scaphoid and lunate. Yonsei Med J. 2003;44(6):1091–1093. doi: 10.3349/ymj.2003.44.6.1091. [DOI] [PubMed] [Google Scholar]
- 7.Komura S., Yokoi T., Suzuki Y. Palmar-divergent dislocation of the scaphoid and the lunate. J Orthop Traumatol. 2011;12(1):65–68. doi: 10.1007/s10195-011-0131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]