Abstract
Tumoral pulmonary hypertension is a rare cause of pulmonary hypertension. We report a patient who was thought to have idiopathic pulmonary arterial hypertension, but later developed fulminant right heart failure ultimately leading to death. Autopsy revealed substantial pulmonary tumor embolism burden originating from liver adenocarcinoma. (Level of Difficulty: Advanced.)
Key Words: pulmonary hypertension, acute heart failure, cancer
Central Illustration
Case Presentation
A 65-year-old man with a history of hypertension, hypothyroidism, diabetes mellitus, and obstructive sleep apnea presented to the emergency room with progressive exertional dyspnea for 1 year. His oxygen saturation was 88% on room air. His physical exam and basic labs were unremarkable, including a chest radiograph, high-resolution lung computed tomography scan, chest computed tomography angiography, lung V/Q scan, and echocardiogram. He underwent right and left heart catheterization, which revealed precapillary pulmonary hypertension with a mean pulmonary artery pressure of 40 mm Hg, pulmonary capillary wedge pressure and left ventricular end-diastolic pressure of 10-12 mm Hg, right atrial pressure of 3 mm Hg, pulmonary vascular resistance of 6.8 WU, cardiac output of 4.88 L/min, and cardiac index of 2.3 L/min/m2. Laboratory testing for secondary causes of pulmonary arterial hypertension, including HIV, hepatitis serologies, and connective tissue disease serologies, was unrevealing. He was diuresed and started on sildenafil with mild subjective improvement in his dyspnea.
Two months later, he re-presented with acute dyspnea, syncope, and hypotension requiring pressors and fluid resuscitation. Repeat transthoracic echocardiography revealed severe right ventricular (RV) systolic dysfunction. Although his hypotension improved with treatment, he had a persistent O2 requirement (6 L/min). Chest computed tomography angiography showed no pulmonary embolism. His liver function tests were notable for elevated transaminases. A computed tomography scan of the abdomen revealed multiple hepatic masses. While awaiting liver biopsy, he became acutely hypoxic and hypotensive, and developed asystolic pulseless electrical activity arrest.
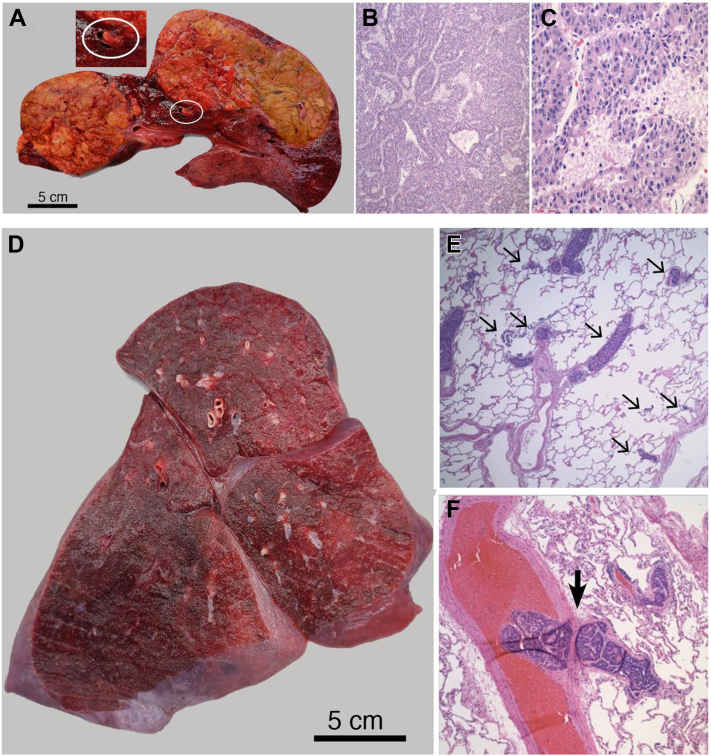
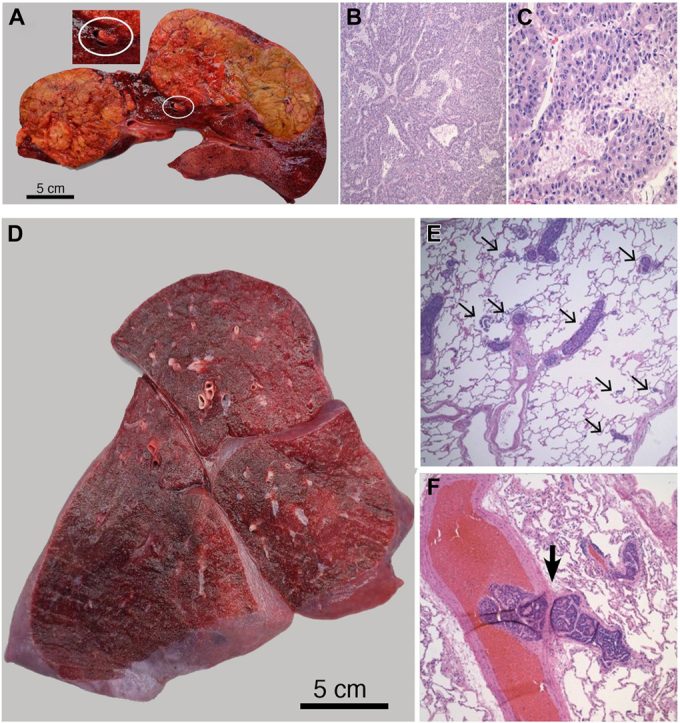
A full, unrestricted autopsy was performed. There were two large, circumscribed liver masses with central necrosis and gross vascular invasion (Figures 1A to 1C). The histological and immunohistochemical features were diagnostic of hepatocellular carcinoma. No thrombi or emboli were identified in the main pulmonary arteries grossly. However, microscopic examination of both lungs demonstrated extensive tumor emboli in the smaller pulmonary vasculature (Figures 1D to 1F). The final diagnosis was death owing to right heart failure from extensive pulmonary tumor emboli originating from primary liver cancer.
Figure 1.
Gross and Microscopic Images of the Liver and Lungs
(A) Cut surface of the liver showing 2 soft yellow-green predominantly circumscribed masses replacing much of the normal liver. Vascular invasion into a vessel is circled and also shown at 2× (inset). (B and C) Microscopic images of liver masses showing a neoplasm arranged in a pseudo-acinar pattern with abundant eosinophilic cytoplasm and prominent nucleoli. (D) Cut surface of the right lung is tan-red and crepitant without gross lesions. (E and F) Microscopic examination of both lungs revealed extensive hepatocellular carcinoma emboli in the pulmonary vasculature. Both medium sized vessels and alveolar capillaries were obstructed. A tumor embolus blocking the exit from a larger vessel is shown (F, large arrow). Objective magnification: B, ×100; C, ×400; E, ×40; F, ×100.
Pulmonary hypertension with fulminant right heart failure owing to extensive pulmonary vascular tumor emboli is extremely rare, and the diagnosis is often missed antemortem in patients with cancer.1 The pathophysiology of tumor pulmonary hypertension includes a combination of mechanical obstruction and vascular remodeling.2 The ensuing pulmonary hypertension results in RV pressure overload and ultimately RV failure.
This case is unique because the patient presented before the diagnosis of his cancer with unexplained hypoxemia, pulmonary hypertension, along with rapid development of right heart failure. He posed a particularly difficult diagnostic challenge because none of the lung imaging raised a clinical suspicion for pulmonary tumor embolism (PTE), presumably reflecting the microvascular obstruction. Cytology of blood aspirated from a wedged pulmonary artery catheter can sometimes reveal malignant cells, although its diagnostic accuracy is unknown.3
This case was also challenging from a treatment perspective. An empiric trial of sildenafil was attempted and had limited symptomatic impact. Additionally, depending on the stage of RV failure, diuresis was initially helpful, but later volume depletion likely compromised his preload and may have contributed to his syncope.
In conclusion, this case highlights that a high index of suspicion is required to diagnose PTE when the workup fails to explain the etiology of precapillary pulmonary hypertension. Early consideration for possible PTE is critical because addressing the underlying malignancy is the only potentially effective treatment.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Winterbauer R.H., Elfenbein I.B., Ball W.C., Jr. Incidence and clinical significance of tumor embolization to the lungs. Am J Med. 1968;45(2):271–290. doi: 10.1016/0002-9343(68)90044-2. [DOI] [PubMed] [Google Scholar]
- 2.Bassiri A.G., Haghighi B., Doyle R.L., et al. Pulmonary tumor embolism. Am J Respir Crit Care Med. 1997;155(6):2089–2095. doi: 10.1164/ajrccm.155.6.9196119. [DOI] [PubMed] [Google Scholar]
- 3.Masson R.G., Krikorian J., Lukl P., Evans G.L., McGrath J. Pulmonary microvascular cytology in the diagnosis of lymphangitic carcinomatosis. N Engl J Med. 1989;321(2):71–76. doi: 10.1056/NEJM198907133210202. [DOI] [PubMed] [Google Scholar]