Abstract
Polytrauma, a patient’s condition with multiple injuries that involve multiple organs or systems, is the leading cause of mortality in young adults. Trauma-related injuries are a major public health concern due to their associated morbidity, high disability, associated death, and socioeconomic consequences. Management of polytrauma patients has evolved over the last few decades due to the development of trauma systems, improved pre-hospital assessment, transport and in-hospital care supported by complementary investigations. Recognising the mortality patterns in trauma has led to significant changes in the approach to managing these patients. A structured approach with application of advanced trauma life support (ATLS) algorithms and optimisation of care based on clinical and physiological parameters has led to the development of early appropriate care (EAC) guidelines to treat these patients, with subsequent improved outcomes in such patients. The journey of a polytrauma patient through the stages of pre-hospital care, emergency resuscitation, in-hospital stabilization and rehabilitation pathway can be associated with risks at any of these phases. We describe the various risks that can be anticipated during the management of polytrauma patients at different stages and provide clinical insights into early recognition and effective treatment of these to improve clinical outcomes.
Keywords: polytrauma, resuscitation, abbreviated injury scale, early appropriate care, trauma related coagulopathy, shock
Introduction
Polytrauma remains a global health concern and has been identified as a key issue in the future health care by the World Health Organisation (WHO).1 Despite advances in diagnostic and treatment algorithms, trauma remains a leading cause of mortality and disability worldwide.2,3
It is a prominent cause of mortality in young adults due to increased Road Traffic Accidents (RTA).4 However, with changing demographics and an older population, elderly patients involved in polytrauma are increasingly being seen.5
The health care costs spent in acute and emergency settings are statistically proven to be significantly higher in polytrauma.6
The precise definition of polytrauma has been refined over the last few decades due to the recognition of clinical patterns, organ system involvement and associated physiochemical changes. Border et al, in 1975 introduced the first formal definition of “Polytrauma” wherein a polytrauma patient was defined as having two or more significant injuries.7 However, for a considerable period, definitions of polytrauma were based on Injury Severity Score (ISS) with its modifications.8 The Abbreviated Injury Score (AIS) which specifies the involvement of more than one ISS body region- gained recognition to enhance the definition of patients with Polytrauma.9 Polytrauma was acknowledged as an injury with AIS >2 in at least two ISS body regions. Following a call for a universally accepted definition of polytrauma, an international consensus process to develop a database-supported definition of polytrauma has been developed.10,11 As per the new “Berlin definition”, Polytrauma is defined as patients with an Abbreviated Injury Scale (AIS) ≥3 for two or more different body regions with one or more additional features from five physiologic parameters of age, consciousness, hypotension, coagulopathy, and acidosis.12
Management of Polytrauma patients begins at the trauma site and should always follow a continuum of care through the prehospital phase, Accident and Emergency Unit and necessary damage control surgical interventions.13,14 The timing of interventions and strategies in the management have evolved due to a better understanding of clinical, physio pathological and immunological response in trauma.15,16 This has led to a paradigm shift in delivering trauma care from “Early Total Care”, ‘Damage Control Orthopaedics’ to the current philosophy of “Early Appropriate Care” and “Prompt individualized safe management (PRISM)”.17,18
The goals of a trauma team are to register the patient’s problems, institute priorities to save lives by using Advanced Trauma Life Support (ATLS) protocol and stabilize the patient before transferring the patient for specialized care.
Multi-modality approach in managing Polytrauma has been proven to reduce the mortality rate significantly, however there are various risks involved in each stage of Polytrauma patient care.
This review article provides an insight into the management of polytrauma patients from a team approach perspective with a focus on the risks involved at each stage, provides early recognition and suggests effective treatment of these to improve patient-related outcomes.
Polytrauma Management: Stages and Risks Associated with Each Stage in the Management of Patients with Polytrauma
The journey of a patient with Polytrauma can be highlighted in the following stages described here individually although some or more of the phases may occur concurrently.
Stages Representing Polytrauma Care Include
1) Pre-hospital Care
2) Accident and Emergency Department Resuscitation and management
3) Models of Polytrauma care, Damage Control Orthopaedics (DCO) and Definitive Fracture fixation
4) Rehabilitation Phase
1) Pre-Hospital Care
Pre-hospital care has evolved significantly with periods of military conflicts. The advent of ATLS in 1978 was shortly followed by Pre-Hospital Trauma Life Support in 1984, aimed at training prehospital providers in a systematic approach to injured patients.19,20 Pre-hospital care has dramatically changed the outcome of polytrauma patients globally with the utilisation of PHTLS (Pre –hospital trauma Life Support). PHTLS is a standardised algorithm aimed at improving the outcome of trauma patients by focusing on prioritizing medical demands in patients.21 As proposed in the trimodal distribution of deaths following polytrauma by Baker et al, the first peak occurs at the scene of injury and hence the patient should receive definitive care to decrease the morbidity and mortality.3,22
Prehospital care has been evolving since its formulation, and it includes stepwise assessment of the patient for administration of vasoactive medications. Teuben et al in 2019 compared the efficacy of pre-hospital care with the following end points: percentage of emergency doctor involvement, total operation time (time difference between arrival of healthcare professionals on spot and departure of paramedics) and transfer time (time difference between the time of trauma team departure from trauma scene and hospital arrival team). All three components have shown an increased efficacy with the use of PHTLS.21
The prehospital environment presents several challenges that could range from hostile patients to hostile environment. Pre-hospital care is based on ATLS principles.
Strategies to Mitigate Risks in the Pre-Hospital Care
The maintenance of the airway with cervical spine immobilization is the first step to be performed in the pre-hospital phase.
Prehospital infusion in polytrauma patients: Management of hypovolemic shock should be started after securing intravenous lines to decrease in-hospital mortality in trauma patients.23 Intravenous fluid (IV) administration has been a key component of the prehospital management of trauma patients since the advent of the EMS (emergency medical systems). It is intended to hemodynamically stabilize trauma patients by replacing intravascular volume and maintaining vital organ perfusion. However, there has been increasing evidence that IV fluid administration would cause more harm than good and hence to be discouraged.24 Few theories, supporting the statement, include delays in rapid transportation to definitive care and the other main reason being a rise in systolic pressure upon administration of IV fluids resulting in hypertension and vasodilatation affecting the tamponade effect and further bleeding. In patients with traumatic brain injury, the focus should be to prevent development of secondary brain injury, and hence, IV fluid administration has to be used cautiously. In summary, prehospital IV fluid administration is to be restricted to penetrating injuries, severe head injury and patients requiring emergency surgery. Routine use of IV placement and fluid administration for all trauma patients should be discouraged.
Pre-Hospital Hemorrhage control: The control of external bleeding, patient immobilization, and rapid transport to the nearest facility should be done at this stage. Hemorrhage is the leading cause of preventable death in combat trauma (90%) and secondary cause of death in civilian trauma (30–40%).24. External hemorrhage is one of the preventable causes of death in polytrauma patients with evidence-based guidelines published in the literature.25 Hemorrhage can be controlled with direct pressure or a pressure bandage. If direct pressure fails to control bleeding, a tourniquet with or without a hemostatic substance can be used to stop the bleeding. Extensive research and trials are in place globally in assessing the effectiveness of hemostatic agents, surgical adjuncts, and blood products for hemostatic resuscitation in pre-hospital setting. The hemostatic agents are broadly classified as systemic agents and local application agents. It has been shown that tranexamic acid can improve the survival in severely injured patients if given within 3 hours of injury.26 Local hemostatic agents though may decrease the time to treatment and adverse effects but not very effective in cases of severe bleeding. Klein et al (2020)24 on their research into emerging therapies for prehospital hemorrhage control elaborated on nanoscale injectable therapies and syntho plates. However, further human trials with these products are in need for them to effectively made use in both combat and civilian trauma.
Emphasis is focused on collecting background information such as time, mechanism of injury and a focused patient history including details of co-morbidities, allergies, and ability to access data from centralised online Electronic Patient Records (EPR).
2) Accident and Emergency Department Resuscitation and Management
Adequate resuscitation remains one of the key aspects in decreasing acute deaths in polytrauma patients. The Airway, Breathing, Circulation, Disability and Exposure (ABCDE) assessment algorithm advocated by Advanced Trauma Life Support (ATLS) increases efficiency and quality of care in Polytrauma patients in the Accident and Emergency Department (AED). The priority remains the identification and stabilisation of potentially life-threatening injuries. ATLS-based systematic approach allows rapid assessment and management of any compromise in airway, breathing, circulation and neurological insults. The aim is to prevent the development of lethal triad of coagulopathy, hypothermia, and acidosis.
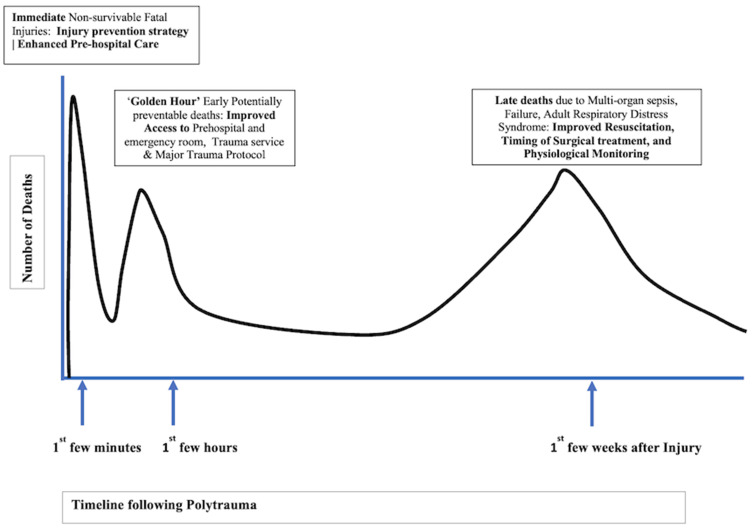
Modern trauma management is based on good teamwork and leadership. In UK trauma practice, emergency medicine doctors tend to lead the trauma team. When there is a history of significant mechanism of injury suggestive of or signs of significant trauma causing airway injuries, it is important to get the anaesthetist’s to join the Trauma team at this crucial stage. Following Professor Richard Cowley’s observation in the Second World War, the initial 60 minutes following major trauma is described as the “Golden Hour”. “Golden Hour is the period of time when life threatening injuries should be treated in order of severity to decrease mortality”. An estimated 60% of avoidable deaths can occur during this period, and optimal care of the trauma victim is crucial for good outcome.4 Figure 1 depicts the ‘Trimodal peaks distribution of deaths after Polytrauma and suggested interventions to mitigate these risks”.
Figure 1.
The figure illustrates the “Tri-modal Peaks Distribution’ of deaths after polytrauma. The timeline of these events in on the Horizontal axis and contributed deaths on the “Y” Axis. The ‘Text boxes’ highlight the period following the trauma and suggested Interventions that can be undertaken to mitigate these Risks.
Going by the sequence of primary survey based on the ATLS trauma, patients pose several challenges. The aim of the primary survey is to detect life-threatening injuries and manage them immediately and to identify potential injuries which can deteriorate to become life-threatening injuries.
Airway Management (Including Cervical Spine Protection)
Airway assessment and management remain the priority in the ATLS algorithm during polytrauma resuscitation.27 Any trauma victim is considered to have a difficult airway unless the mechanism of injury does not suggest cervical spine trauma. Careful consideration of cervical spine injury should dictate the airway interventions required which in most cases will require cervical spine stabilisation with cervical collar. During advanced airway management, the cervical collar must be removed and replaced with in-line immobilisation provided by a suitable trained team member. The management of the airway can be complicated by facial injuries, fractures to the mandible and maxilla, bleeding, burns to the face and upper airway, dislodgement of teeth and dentures and injury to the upper airway. This can also be complicated by the presence of gunshot or open bleeding injuries of the neck injuries or the presence of an undetected pneumothorax which can become worse after endotracheal intubation. Hence, the biggest life-threatening injury in the airway is “Airway obstruction causing hypoxemia”.
A careful management of the airway with oxygen and airway adjuncts or a “definitive airway” intervention is indicated in patients with facial burn involving the upper airway, the presence of an unstable facial bone fractures and laryngeal injuries, which have the potential to cause total airway obstruction. Maintaining a definitive airway is one of the key steps in reducing the mortality rates in polytrauma and restricting the progress of the inflammatory cascade. Although, there is a debate that no significant association between a successful definitive airway and the prehospital setting and survival, but it is one of the key parameters in improving the survival rate in the hospital setting. The availability of adequate equipment and trained personnel in the emergency department are two important factors aiding the success rate of securing a definitive airway, as it could be quite challenging in prehospital settings. Securing an airway is crucial for the survival of complex trauma patients, especially in patients with traumatic brain injury and burn patients. “Definitive airway” interventions might include the option of needle and surgical cricothyroidotomy, tracheostomy and endotracheal intubation. Rapid Sequence Intubation is the technique practised globally in emergency settings. It has to be emphasized that securing a definitive airway in an emergency setting is one of the critical factors predicting the survival of polytrauma patients.
In addition to traumatic injury, the patient may present with full stomach on board due to the lack of adequate starvation period and prolonged gastric emptying time in trauma.28 Standard practice is to treat them as full stomach and perform rapid sequence induction with a cricoid pressure application by a suitably trained operative department practitioner or an anaesthetic nurse or Emergency Medicine nurse specifically trained for providing this.29
Breathing and Ventilation
Chest injuries can complicate the anaesthetic management of the trauma victims. The extent of the chest injuries depends on the mechanism of injury, speed of the vehicle involved in the crash, the impact, and if there is entrapment of the victim in the vehicle. The following are the life-threatening injuries: tension pneumothorax, untreated open pneumothorax, massive haemothorax, cardiac tamponade and tracheobronchial injury.
Positive pressure ventilation using an endotracheal tube in a patient with undetected pneumothorax can lead to life-threatening tension pneumothorax. Any pneumothorax should be carefully considered and if in doubt needs to be dealt with in emergency needle thoracocentesis followed by urgent chest drain insertion. This can happen in patients with a simple pneumothorax, untreated open pneumothorax or undetected small tension pneumothorax.30 Persistent pneumothorax with bubbling of air synchronising with the positive pressure ventilation indicates a major tracheobronchial injury that will require an emergency advance management of the airway including one lung ventilation and a transfer to a centre capable of performing cardiothoracic surgery.31
In the absence of life-threatening injuries, these patients might present with high impact chest injuries. The signs and symptoms of all the thoracic injuries may not be obvious due to the concomitant presence of significant hypovolaemia due to the blood loss.
Simultaneous radiological investigations should be carried out while resuscitation is in progress.
Circulation with Hemorrhage Control
Haemorrhage is one of the most common risks in the management of polytrauma patients. Rapid identification of the site of haemorrhage (external or internal) is crucial in reducing mortality in polytrauma patients.
Definitive control of haemorrhage should be the goal with rapid replacement of blood volume, and Damage Control Resuscitation (DCR) should be initiated efficiently.32 An incorrect DCR has the potential to exacerbate the lethal triad of acidosis, coagulopathy, and homeostatic imbalances. Initiative-taking steps such as external direct compression and judicial use of a tourniquet to stop the bleeding distally in limbs can be undertaken.33
Source of bleeding should be considered carefully by looking for confined spaces and external bleeding. The source of external bleeding can be as simple as extensive blood loss due to scalp lacerations or cutaneous bleeding in the head/neck region. Massive haemothorax can produce bleeding up to and above 1.5 L which can easily be missed by clinical examination due to lack of percussion over the mid-axillary area.
A Focused Assessment with Sonography for Trauma (FAST) scan can help in detecting blood around the liver or the spleen or in the abdominal pockets and in the pelvis. Early applications of pelvic binder in a trauma patient are key to minimise blood loss. A significant amount of blood loss can occur due to the long bone fractures. An application of the appropriate splints to reduce the fracture will help in reducing the pain as well as excessive bleeding. Importance has to be given to seeking information about blood loss at the scene from the paramedics.
Assessment of circulation and restoration of the intravascular volume with balance resuscitation should be supported by early blood transfusion and administration of haemostatic agents like tranexamic acid.
Other exogenous methods have been used to control bleeding such as Antifibrinolytic agents, eg, Tranexamic acid, Junctional Emergency Treatment Tool™, Combat Ready Clamp, XSTAT®, ResQFoam, Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA), an invasive technique of aortic occlusion has been reported to be safe and effective in patients with traumatic haemorrhage with hemodynamic instability.34 The definitive treatment for hypovolaemia should be considered simultaneously. In addition, massive bleeding patient may present with disseminated intravascular coagulation (DIC), resulting in significant coagulation disorders requiring blood and its components for resuscitation.
The presence of muffled heart sounds in a patient with distended neck veins is any indication of cardiac tamponade which requires urgent treatment. These patients tend to have significant anterior chest wall impact injuries with multiple fractures, flail chest and contusion of the underlying lung predisposing to Acute Respiratory Distress Syndrome (ARDS).35
Disability
A patient with trauma can present with reduced level of consciousness which complicates the assessment of patient. The reduced level of consciousness can be due to the head injury which we should always be considered as the first cause even when the evidence of excessive alcohol intake is obvious.36
A patient with the reduced GCS will always be considered to have cervical spine injury, and neck is triple immobilised using cervical collar, blocks, and tape. Airway intervention may need to be considered in patients with reduced GCS. When the patient presents with multiple life-threatening injuries, a careful team discussion should follow appropriate clinical decision-making and prioritising immediate life-threatening problems with consideration given to simultaneously managing multiple life-threatening injuries.
Exposure and Environment
Depending on the severity of the injury, the time taken for the extrication of the patient from the motor vehicle or recovering from the debris can expose the patient to very low temperatures causing significant hypothermia and crush injuries. Early warming and careful management of crash injuries is paramount in managing these patients.
One of the biggest risks of traumatic injury is loss of skin and exposure to infected material and debris associated with the injury. Early strategic management of trauma victims can prevent deaths. However, catastrophic delayed outcome can be prevented by combining the best care in the initial stages with careful crucial measures to prevent wound contamination and bacterial infection leading to sepsis.37 Otherwise, most trauma victims can suffer significant morbidity or mortality due to sepsis.
Managing Specific Risks During Polytrauma Management: Lethal Triad of Coagulopathy, Hypothermia and Acidosis
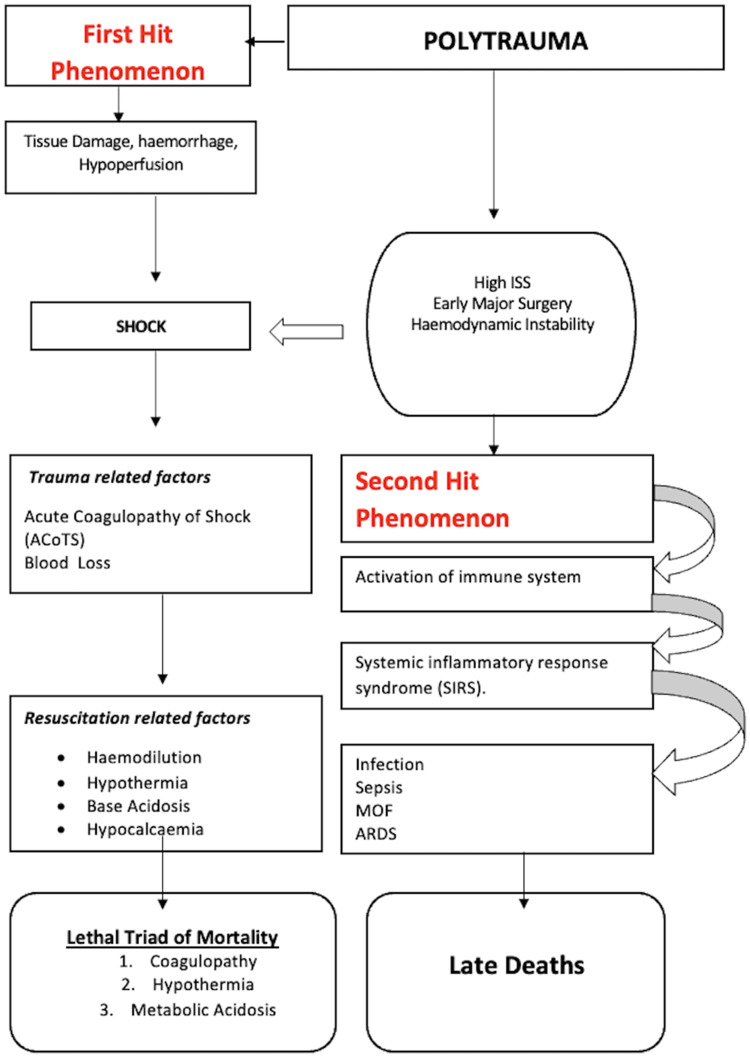
The Pathophysiology leading to Lethal Triad and late deaths in Polytrauma patients is depicted in a flowchart Figure 2.
- Trauma associated coagulopathy – Trauma associated coagulopathy (TAC) in polytrauma patients could be due to acute coagulopathy of trauma shock (ACoTS) or Resuscitation Associated Coagulopathy (RAC). Undetected, it forms one (of) the components of the lethal triad associated with mortality.38
- ACoTS develops following an injury before resuscitative measures are initiated. The risk factors associated with a higher probability of developing ACoTS include high ISS, ph. below 7.10, hypothermia and hypotension below a systolic blood pressure of 70 mm of mercury (Hg).39 Activation of the protein C pathway is the proposed mechanism. Early detection of ACoTS with standard bleeding profile, coagulation tests [platelet count, activated partial thromboplastin time (APTT), the prothrombin time (PT), international normalised ratio (INR)], “clotting cascade” components and point of care coagulometers may direct efforts towards targeted clotting factor replacement in these patients.
- Resuscitation Associated Coagulopathy (RAC) is dilution of procoagulant factors following rapid infusion of crystalloids and colloids. Hypothermia, acidosis, and hypocalcemia exacerbate RAC.
- Disseminated intravascular coagulation (DIC) is a devastating complication of polytrauma. DIC is typified by the in vivo activation of the coagulation system, resulting in the intravascular deposition of fibrin and consumption bleeding ultimately, which can lead to development of multiple organ dysfunction syndrome (MODS).
- Role of Viscoelastic Tests: APTT, PT, INR are the traditional tests to diagnose coagulation abnormalities. However, these tests only assess the initial phase of blood coagulation. Hence, viscoelastic tests (VET) such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM) which can dynamically assess coagulation abnormalities for effective correction and reversal have been introduced. Coagulation profile and VET are thus used to guide the administration of platelets, cryoprecipitate, fresh-frozen plasma, and blood products.
Figure 2.
The figure depicts the pathophysiology and mechanisms leading to lethal triad of mortality and late deaths in polytrauma patients.
Abbreviations: ISS, Injury Severity Score; MOF, Multi-organ Failure; ARDS, Adult Respiratory Distress Syndrome.
Damage Control Resuscitation (DCR) involves rapid control of hemorrhage, prevention/correction of acidosis, correction of hypothermia, hemostatic resuscitation and correction of hypocalcemia. The intention of DCR is to mitigate RAC and correct existing coagulopathy. A balanced transfusion ratio of fresh frozen plasma: platelets: RBCs in a ratio of 1:1:1 is advocated with early administration of tranexamic acid to counteract the possibility of RAC.40
Metabolic Acidosis: It is one of the lethal triads of coagulopathy, hypothermia, and acidosis.41 Poorer outcomes have been observed if the base deficit exceeds 6 mmol/L in trauma patients.42 Mild metabolic acidosis may develop due to early hypovolemic shock and correctable with volume resuscitation and monitoring. Severe metabolic acidosis occurs due to prolonged, severe hypovolemic shock and tissue hypoxia. Activation of anaerobic respiratory mechanisms and the formation of lactic acid are the underlying mechanisms. Reversal of these mechanisms with control of hemorrhage, fluid resuscitation, and blood products will establish the acid–base imbalance.
Hypothermia: In patients with polytrauma, the risk of hypothermia is substantial and can be fatal. Additionally, it can exacerbate coagulopathy and lead to the development of dysrhythmias.43,44 Prevention is the best treatment for hypothermia with close monitoring of the core body temperature. Hypotension and hypothermia should be managed with rapid control of hemorrhage, a warm environment, external warming devices, warm intravenous fluids, and blood transfusion.
Managing Associated Risks During Polytrauma Management
Hypoxia: The pathophysiological mechanism in polytrauma is characterized by a discrepancy between oxygen supply and demand leading to tissue hypoxia. Variables such as pain, anxiety, blood loss, reduced cardiac output, anaemia, and head and vital organ injuries can all contribute to reduced oxygen supply. Reversal of the underlying cause of tissue hypoxia is the essential principle in its management. In the interim, supplemental oxygen therapy via mask-reservoir device with flow rate of 15L/min for polytrauma patients undoubtedly prevents the mortality and morbidity associated with hypoxia.45 Target oxygen therapy should be considered after initial stabilization in trauma patients.
Hypocalcemia: This can occur in patients with polytrauma due to rhabdomyolysis and massive blood transfusion.46 Platelet function, intrinsic and extrinsic clotting cascades, and cardiac contraction are all disrupted by hypocalcemia.47 Further, it adds another arm to the lethal triad of coagulopathy, hypothermia and acidosis to make the situation worse in polytrauma patients. In critically ill, polytrauma patients with moderate-to-severe hypocalcemia, short-term infusion of 4 g of intravenous (IV) calcium gluconate appears to have shown promising results.48
3) Models of Polytrauma Care and Definitive Fracture Fixation
As the definition and classification of polytrauma has evolved over the decades, so have the models and principles for the definitive management of associated injuries including fractures15,17 The initial concept of Early Total Care (ETC) proposed by Bone LB et al advocated definitive fracture fixation of long bone within 24 hours of injury.49 Although the randomised controlled trial showed a decrease in pulmonary complications, a second hit (surgical intervention) led to the amplification of the degree of damage, thus leading to the prospect of increased morbidity and mortality. The concept of Damage Control Orthopaedics (DCC) of managing initial haemodynamic instability with staged interventions led to improvements but still necessitated further surgeries and a longer length of hospital stay.50 The reality that decision-making should be driven by the management of physiological response to the injury led to the current most applied philosophy of early appropriate care (EAC).51 Utilising physiological markers in polytrauma treatment algorithms has been effective in rationalising interventions safely. EAC is more a concept of metabolic permissiveness and appropriate management based on physiological response to injury.17,52 Pape et al in 2015 and Giannoudis PV et al in 2017 have provided variations in the clinical application of EAC. The Safe definitive surgery (SDS) by Pape et al provides a dynamic concept for fracture fixation in polytrauma patients based on primary trauma assessment.53 The Prompt individualized safe management (PRISM) proposed by Giannoudis PV et al uses the basic principles of EAC combined with the application of strategies around the availability of health care resources.18 Acknowledging, addressing and balancing of all the above-mentioned risks has reduced mortality in polytrauma patients over the last few decades, but timing of definitive stabilisation of major fractures is still a crucial decision-making process.15 The application of Artificial Intelligence (AI), Machine Learning (ML) algorithms and patient-specific genomics present emerging possibilities for the development of trauma management protocols based on individual response to injury13,54 These may also help to predict risk stratification of polytrauma patients. Table 1 highlights the characteristics and risks associated with Evolving Models of Polytrauma patient care.
Table 1.
Characteristics and Risks Associated with Evolving Models of Polytrauma Patient Care
| Concept | Philosophy | Risk |
|---|---|---|
| Early total care (ETC) |
|
|
| Damage control orthopaedics (DCO) |
|
|
|
Early appropriate care (EAC) |
|
|
| Safe definitive surgery (SDS) |
|
|
| Prompt individualized safe management (PRISM) | Based on the availability of health care resources in different countries and local guidelines
|
Individualized treatment plan – be it ETC or DCO with their inherent risks |
4) Rehabilitation Phase
As the frequency, severity and complexity of polytrauma injuries has become apparent, the need for specialised, intensive rehabilitation and coordination of care during recovery and rehabilitation has become clear. Ideal outcomes for survivors of polytrauma depend on the organization of complex medical, psychosocial, and socio-economic factors.55
A well-functioning and well-trained multidisciplinary team is critical in offering polytrauma rehabilitation care. Hanna et al in 2020 in their systematic review concluded that there is an urgent need for robust studies to support evidence for the crucial role of multidisciplinary rehabilitation in enhancing clinical outcomes following polytrauma.56
Deep Venous Thrombosis (DVT) prophylaxis in polytrauma patients including rehabilitation phase:
A systematic review of 12 studies relating the incidence of DVT in polytrauma patients reported an overall incidence of DVT in polytrauma patients as 20%. Adding on to their analysis was an incidence of 38% in patients without prophylaxis and 13% patients with prophylaxis.57 A recent study by Peng et al has derived a DVT scoring system to guide clinicians on the choice of DVT prophylaxis in polytrauma patients.58 Venous thromboembolism (VTE) as a late complication of polytrauma should be kept in mind during the rehabilitation phase of polytrauma patients. As a general rule, early full weight bearing mobilisation and multidisciplinary rehabilitation are the key to prevent such events. Continual VTE prophylaxis should be based on “Risk Assessment” and guided by the age and co-morbidities of the patient amongst other factors.
Internationally accepted guidelines for rehabilitation in polytrauma patients are necessary to provide resource recommendations such as training programmes, performance improvement strategies and effective organisation of rehabilitation services.
Conclusion
Polytrauma care and care of the multiply injured patient have evolved over the last few decades. The application of a structured approach with application of advanced trauma life support (ATLS) algorithms, major trauma protocols, pre-hospital and in-hospital resuscitation has improved patient outcomes. However, as the review suggests, there are identifiable risks associated with each stage in the management of patients with Polytrauma. A high index of suspicion and proactive mitigation of risks will be crucial in further improving morbidity and mortality figures. The advent of Artificial Intelligence and patient-specific genomics present exciting opportunities for the development of management protocols based on individual differences in response to injury.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr Madapura K Shashidhara is ACS and RCS England approved ATLS Director and Instructor. The authors report no conflicts of interest in this work.
References
- 1.United Nations Road Safety Collaboration. Decade of Action for Road Safety 2011–2020. Available from: https://www.who.int/publications/i/item/decade-of-action-for-road-safety-2011-. Accessed 15, June 2022.
- 2.van Breugel JMM, Niemeyer MJS, Houwert RM, Groenwold RHH, Leenen LPH, van Wessem KJP. Global changes in mortality rates in polytrauma patients admitted to the ICU – a systematic review. World J Emerg Surg. 2020;15(1):55. doi: 10.1186/s13017-020-00330-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients – has anything changed? Injury. 2009;40(9):907–911. doi: 10.1016/j.injury.2009.05.006 [DOI] [PubMed] [Google Scholar]
- 4.Marsden NJ, Tuma F. Polytraumatized Patient 2021. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 5.de Vries R, Reininga IHF, Pieske O, Lefering R, El Moumni M, Wendt K. Injury mechanisms, patterns, and outcomes of older polytrauma patients – an analysis of the Dutch Trauma Registry. PLoS One. 2018;13(1):e0190587. doi: 10.1371/journal.pone.0190587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koller M, Ernstberger A, Zeman F, Loss J, Nerlich M; Trauma Network Eastern Bavaria (TNO). Outcome after polytrauma in a certified trauma network: comparing standard vs. maximum care facilities concept of the study and study protocol (POLYQUALY). BMC Health Serv Res. 2016;16:242. doi: 10.1186/s12913-016-1468-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Border JR, LaDuca J, Seibel R. Priorities in the management of the patient with polytrauma. Prog Surg. 1975;14:84–120. [DOI] [PubMed] [Google Scholar]
- 8.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 9.Butcher N, Balogh ZJ. AIS > 2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury. 2012;43:196–199. [DOI] [PubMed] [Google Scholar]
- 10.Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40(Suppl 4):S12–22. doi: 10.1016/j.injury.2009.10.032 [DOI] [PubMed] [Google Scholar]
- 11.Pape H-C, Lefering R, Butcher N, et al. The definition of polytrauma revisited: an international consensus process and proposal of the new ‘Berlin definition’. J Trauma Acute Care Surg. 2014;77(5):780–786. doi: 10.1097/TA.0000000000000453 [DOI] [PubMed] [Google Scholar]
- 12.Rau C-S, Wu S-C, Kuo P-J, et al. Polytrauma defined by the new Berlin definition: a validation test based on propensity-score matching approach. Int J Environ Res Public Health. 2017;14(9):1045. doi: 10.3390/ijerph14091045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devendra A, Nishith PG, Dilip Chand Raja S, Dheenadhayalan J, Rajasekaran S. Current updates in management of extremity injuries in polytrauma. Journal of Clinical Orthopaedics and Trauma. 2021;12(1):113–122. doi: 10.1016/j.jcot.2020.09.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Payal P, Sonu G, K GA, Prachi V. Management of polytrauma patients in emergency department: an experience of a tertiary care health institution of northern India. World Journal of Emergency Medicine. 2013;4(1):15–19. doi: 10.5847/wjem.j.issn.1920-8642.2013.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pape HC, Halvachizadeh S, Leenen L, Velmahos GD, Buckley R, Giannoudis PV. Timing of major fracture care in polytrauma patients – an update on principles, parameters, and strategies for 2020. Injury. 2019;50(10):1656–1670. doi: 10.1016/j.injury.2019.09.021 [DOI] [PubMed] [Google Scholar]
- 16.Moore TA, Simske NM, Vallier HA. Fracture fixation in the polytrauma patient: markers that matter. Injury. 2020;51(Suppl 2):S10–S14. doi: 10.1016/j.injury.2019.12.024 [DOI] [PubMed] [Google Scholar]
- 17.Upadhyaya GK, Iyengar KP, Jain VK, Garg R. Evolving concepts and strategies in the management of polytrauma patients. J Clin Orthop Trauma. 2021;12(1):58–65. doi: 10.1016/j.jcot.2020.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giannoudis PV, Giannoudis VP, Horwitz DS. Time to think outside the box:’ Prompt-Individualized-Safe Management’ (PRISM) should prevail in patients with multiple injuries. Injury-Int J Care Injured. 2017;48(7):1279–1282. [DOI] [PubMed] [Google Scholar]
- 19.Carmont MR. The Advanced Trauma Life Support course: a history of its development and review of related literature. Postgrad Med J. 2005;81(952):87–91. doi: 10.1136/pgmj.2004.021543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown J, Sajankila N, Claridge JA. Prehospital assessment of trauma. Surg Clin North Am. 2017;97(5):961–983. doi: 10.1016/j.suc.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 21.Teuben M, Löhr N, Jensen KO, et al. Improved pre-hospital care efficiency due to the implementation of pre-hospital trauma life support (PHTLS®) algorithms. Eur J Trauma Emerg Surg. 2020;46(6):1321–1325. doi: 10.1007/s00068-019-01141-1 [DOI] [PubMed] [Google Scholar]
- 22.Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD. Epidemiology of trauma deaths. Am J Surg. 1980;140(1):144–150. doi: 10.1016/0002-9610(80)90431-6 [DOI] [PubMed] [Google Scholar]
- 23.Hampton DA, Fabricant LJ, Differding J, Diggs B, Underwood S, De La Cruz D; PROMMTT Study Group. Prehospital intravenous fluid is associated with increased survival in trauma patients. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klein MK, Tsihlis ND, Pritts TA, Kibbe MR. Emerging therapies for prehospital control of hemorrhage. J Surg Res. 2020;248:182–190. doi: 10.1016/j.jss.2019.09.070 [DOI] [PubMed] [Google Scholar]
- 25.Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):163–173. [DOI] [PubMed] [Google Scholar]
- 26.Fischer PE, Bulger EM, Perina DG, et al. Guidance document for the prehospital use of tranexamic acid in injured patients. Prehosp Emerg Care. 2016;20(5):557–559. [DOI] [PubMed] [Google Scholar]
- 27.Carley S, Gwinnutt C. Stepwise airway management in the trauma patient. Trauma. 2004;6(3):177–185. doi: 10.1191/1460408604ta311oa [DOI] [Google Scholar]
- 28.Sise MJ, Shackford SR, Sise CB. Early intubation in the management of trauma patients: indications and outcomes in 1000 consecutive patients. J Trauma. 2009;66:32–40. [DOI] [PubMed] [Google Scholar]
- 29.Bhatia N, Bhagat H, Sen I. Cricoid pressure: where do we stand? J Anaesthesiol Clin Pharmacol. 2014;30(1):3–6. doi: 10.4103/0970-9185.125683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25(1):42. doi: 10.1186/s13049-017-0384-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leigh-Smith S, Harris T. Tension pneumothorax – time for a re-think? Emerg Med J. 2005;22(1):8–16. doi: 10.1136/emj.2003.010421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fecher A, Stimpson A, Ferrigno L, Pohlman TH. The pathophysiology and management of hemorrhagic shock in the polytrauma patient. J Clin Med. 2021;10(20):4793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vishwanathan K, Chhajwani S, Gupta A, Vaishya R. Evaluation and management of hemorrhagic shock in polytrauma: clinical practice guidelines. J Clin Orthop Trauma. 2020;5(13):106–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Granieri S, Frassini S, Cimbanassi S, et al. of resuscitative endovascular balloon occlusion of the aorta (REBOA) in traumatic abdominal and pelvic exsanguination: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2022. doi: 10.1007/s00068-022-01955-6 [DOI] [PubMed] [Google Scholar]
- 35.Chu CP, Chen PP. Tracheobronchial injury secondary to blunt chest trauma: diagnosis and management. Anaesth Intensive Care. 2002;30(2):145–152. doi: 10.1177/0310057X0203000204 [DOI] [PubMed] [Google Scholar]
- 36.Suresh MR, Chung KK, Schiller AM, Holley AB, Howard JT, Convertino VA. Unmasking the hypovolemic shock continuum: the compensatory reserve. J Intensive Care Med. 2019;34(9):696–706. doi: 10.1177/0885066618790537 [DOI] [PubMed] [Google Scholar]
- 37.Orso D, Vetrugno L, Federici N, D’Andrea N, Bove T. Endotracheal intubation to reduce aspiration events in acutely comatose patients: a systematic review. Scand J Trauma Resusc Emerg Med. 2020;28(1):116. doi: 10.1186/s13049-020-00814-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55(1):39–44. doi: 10.1097/01 [DOI] [PubMed] [Google Scholar]
- 39.Savioli G, Ceresa IF, Macedonio S, et al. Trauma coagulopathy and its outcomes. Medicina. 2020;56(4):205. doi: 10.3390/medicina56040205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma. Crit Care. 2019:23(1);98. doi: 10.1186/s13054-019-2347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrara A, MacArthur JD, Wright HK, Modlin IM, McMillen MA. Hypothermia and acidosis worsen coagulopathy in the patient requiring massive transfusion. Am J Surg. 1990;160(5):515–518. doi: 10.1016/s0002-9610(05)81018-9 [DOI] [PubMed] [Google Scholar]
- 42.Ibrahim I, Chor WP, Chue KM, et al. Is arterial base deficit still a useful prognostic marker in trauma? A systematic review. Am J Emerg Med. 2016;34(3):626–635. doi: 10.1016/j.ajem.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 43.Jurkovich GJ, Greiser WB, Luterman A, Curreri PW. Hypothermia in trauma victims: an ominous predictor of survival. J Trauma. 1987;27(9):1019–1024. [PubMed] [Google Scholar]
- 44.Rohrer MJ, Natale AM. Effect of hypothermia on the coagulation cascade. Crit Care Med. 1992;20(10):1402–1405. [DOI] [PubMed] [Google Scholar]
- 45.Douin DJ, Anderson EL, Dylla L, et al. Association between hyperoxia, supplemental oxygen, and mortality in critically injured patients. Crit Care Explor. 2021;3(5):e0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ditzel RM, Anderson JL, Eisenhart WJ, et al. A review of transfusion- and trauma-induced hypocalcemia: is it time to change the lethal triad to the lethal diamond? J Trauma Acute Care Surg. 2020;88(3):434–439. [DOI] [PubMed] [Google Scholar]
- 47.Vasudeva M, Mathew JK, Groombridge C, et al. Hypocalcemia in trauma patients: a systematic review. J Trauma Acute Care Surg. 2021;90(2):396–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dickerson RN, Morgan LM, Croce MA, Minard G, Brown RO. Treatment of moderate to severe acute hypocalcemia in critically ill trauma patients. JPEN J Parenter Enteral Nutr. 2007;31(3):228–233. doi: 10.1177/0148607107031003228 [DOI] [PubMed] [Google Scholar]
- 49.Bone LB, Johnson KD, Weigelt J, Scheinberg R. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am. 1989;71(3):336–340. [PubMed] [Google Scholar]
- 50.Guerado E, Bertrand ML, Cano JR, Cerván AM, Galán A. Damage control orthopaedics: state of the art. World J Orthop. 2019;10(1):1–13. doi: 10.5312/wjo.v10.i1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic surgery in multiple trauma patients: development of a protocol for early appropriate care. J Orthop Trauma. 2013;27(10):543–551. [DOI] [PubMed] [Google Scholar]
- 52.Berwin JT, Pearce O, Harries L, Kelly M. Managing polytrauma patients. Injury. 2020;51(10):2091–2096. doi: 10.1016/j.injury.2020.07.051 [DOI] [PubMed] [Google Scholar]
- 53.Pape HC, Pfeifer R. Safe definitive orthopaedic surgery (SDS): repeated assessment for tapered application of Early Definitive Care and Damage Control? An inclusive view of recent advances in polytrauma management. Injury-Int J Care Injured. 2015;46(1):1–3. [DOI] [PubMed] [Google Scholar]
- 54.Liu NT, Salinas J. Machine learning for predicting outcomes in trauma. Shock. 2017;48(5):504–510. doi: 10.1097/SHK.0000000000000898 [DOI] [PubMed] [Google Scholar]
- 55.Strasser DC, Uomoto JM, Smits SJ. The interdisciplinary team and polytrauma rehabilitation: prescription for partnership. Arch Phys Med Rehabil. 2008;89(1):179–181. doi: 10.1016/j.apmr.2007.06.774 [DOI] [PubMed] [Google Scholar]
- 56.Al Hanna R, Amatya B, Lizama LE, Galea MP, Khan F. Multidisciplinary rehabilitation in persons with multiple trauma: a systematic review. J Rehabil Med. 2020;52(10):jrm00108. doi: 10.2340/16501977-2737 [DOI] [PubMed] [Google Scholar]
- 57.Venet C, Berger C, Tardy B, Viallon A, Decousus H, Bertrand JC. Prophylaxie de la maladie veineuse thromboembolique chez le patient polytraumatisé. Epidémiologie et intérêt [Prevention of venous thromboembolism in polytraumatized patients. Epidemiology and importance]. Presse Med. 2000;29(2):68–75. [PubMed] [Google Scholar]
- 58.Peng G, Wang Q, Sun H, et al. Development and prospective validation of a novel risk score for predicting the risk of lower extremity deep vein thrombosis among multiple trauma patients. Thromb Res. 2021;201:116–122. doi: 10.1016/j.thromres.2021.02.020 [DOI] [PubMed] [Google Scholar]