Abstract
Introduction
COVID-19 has trickle-down psychological effects on multiple strata of society, particularly university students. Apart from the worry of contracting or spreading COVID-19, Malaysian university students were also locked down on their campuses, suffering significant psychological distress. Hence, an online mindfulness intervention was proposed to alleviate psychological distress and improve psychological flexibility and mindfulness.
Methods
This was a quasi-experimental study with university students as participants. Intervention group participants were instructed to complete online questionnaires which covered basic demographics and instruments assessing depression, anxiety, stress, mindfulness, psychological flexibility, and fear of COVID-19 before and after the one-hour intervention. The control group also completed before and after questionnaires and were subsequently crossed over to the intervention group. Repeated measures ANOVA was conducted to assess time*group effects.
Results
118 participants were involved in this study. There were significant differences in anxiety (F(1,116) = 34.361, p < 0.001, partial eta-squared = 0.229) and psychological flexibility between the two groups (F(1,116) = 11.010, p = 0.001, partial eta-squared = 0.087), while there were no differences in depression, stress, mindfulness, or fear of COVID-19.
Conclusion
The results of this study corroborate the efficacy of online single-session mindfulness therapy as a viable short-term psychological intervention under financial and time constraints. Since university students are in the age group with the highest incidence of depressive and anxiety disorders, it is crucial to utilize resources to address as many students as possible to ensure maximum benefit.
Keywords: Mindfulness, online, single-session, anxiety, psychological flexibility, university student
Introduction
The novel SARS-CoV-2 virus, currently known as COVID-19, was first reported in Wuhan, China in December 2019. 1 Subsequently, it exponentially spread all across the globe, resulting in the World Health Organization (WHO) declaring the disease as a pandemic on 11th March 2020. 2 Malaysia was not spared, recording the highest number of positive cases in the South East Asia region in March 2020, with the latest figures of 42,872 positive cases and 302 total deaths as of 11th November 2020. 3
In view of rampant transmission, the Malaysian government enforced strict social and movement restrictions and mandatory quarantine or isolation for persons under investigation and positive cases respectively. 4 , 5 Although retrospectively swift actions were essential to blunt the progression of spread, nevertheless, such lockdowns have crippled the economy, causing untold social and psychological impairment. 6 This corroborates with existing literature that psychological illnesses are on the rise during the COVID-19 pandemic. 7 , 8 Early Chinese data from the initial phase of the outbreak showed that more than half of respondents had suffered moderate to severe psychological impact. 9 This can be due to direct causes such as stress, fear of contamination, depression, and grief evoked by exposure to the virus as well as indirect consequences of the socioeconomic impact. 10
Undergraduate students in Malaysia in particular are in unusual circumstances. Due to a sudden explosion in cases related to two less fortuitous coincidences, namely a prison outbreak of Covid-19 and a concurrent general election in the same state, 11 students in Sabah were uniquely locked down on campus and all teaching and learning was converted to online mode, whereas their counterparts in all other universities in Malaysia were allowed to continue face to face teaching and learning as usual. This was especially compounded in the sample population investigated in this study, because they were all medical students. Since the medical degree program is a highly vocational course of study, it is by nature highly dependent on bedside teaching and face to face work. 12 - 14 Hence, for medical students who are locked down physically and educationally with no conceivable end in sight, there may be a strong sense of loss of purpose, 15 perceived loss of ability and skillset, 16 and potential recriminations or self-blame, 17 especially for those who have friends at other medical universities in other parts of the country that have not been locked down. As such, there is a high possibility of psychopathologies developing. 18 Such psychological issues can present a major obstacle to academic performance, which can affect students’ concentration, motivation, and social interactions, which all play vital roles in enabling students to succeed in their higher education. 19 , 20 Recent intra-pandemic data indicate that Covid-19 has negative impacts on higher education such as fear of infection of self and loved ones, difficulty concentrating, sleep disruptions, reduced social interactions, and worse academic results. 21 , 22 It is therefore instrumental to prevent such deteriorations from perpetuating further and interventions with known efficacy can be employed to serve as crucial public health primary prevention interventions to promote psychological wellness in quarantined and anxious university students. 23 Mindfulness-based interventions constitute one such intervention with known efficacy and can increase mindfulness and psychological flexibility. 24 , 25
Mindfulness can be defined as attending to one’s present-moment thoughts, feelings, and sensations, with an open and curious mind, and without attempting to change the experience. 26 Mindfulness techniques are currently incorporated into many therapies in mental health care, namely mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT), dialectical behavior therapy (DBT), and acceptance and commitment therapy (ACT). 27 Psychological flexibility is a similar construct involving the ability to fully experience the present moment, including observing one’s thoughts and feelings, without struggling to control or change them, and the ability to either persist or change behavior in the given context in a manner that is consistent with one’s values and goals. 28 Hence, mindfulness techniques can be employed to assist with all three aspects of psychological flexibility. They enable the aforementioned observation of one’s thoughts impartially and non-judgmentally, which then allows full and rich experiences of the present moment. An individual is thus able to persist with value-congruent behavior, because mindfulness techniques facilitate acceptance of the inevitable accompanying pain. 29 , 30 Literature shows that mindfulness and psychological flexibility are related in terms of psychological distress, 31 and psychological distress is significantly reduced in individuals with higher psychological flexibility. 28
Due to the distancing requirements during this pandemic, there has been renewed interest in development and assessment of the use of digital and online tools as viable alternatives for care delivery. 32 - 34 Online mindfulness meditation (MM) training has demonstrated equal benefits to face-to-face MBSR training for reduction of depression, stress, and anxiety. 35 , 36 Culturally closer to home, evidence from Singapore reports similar effectiveness for mindfulness training conducted through videoconferencing and traditional in-person modalities. 37 In the specific context of university students, there were significant reductions in depression and anxiety, but not stress, after web-based mindfulness performed over 8 weeks. 38 Similar evidence showing that online interventions reduced psychological stress, enhancing mental health, sleep disturbance, life satisfaction, and energy level was demonstrated in college students and working adults. 39 , 40 However, in the recent pandemic, there has been no evidence from Malaysian settings that corroborates the aforementioned findings. There are however descriptive studies of ultra-brief psychological intervention modules that adapt mindfulness techniques, allowing them to be delivered in shorter-format single interventions outside of formalized psychotherapeutic protocols. 41 From a public health perspective, with finite psychological resources, running a single-session protocol with proven efficacy delivers far greater benefits from a utilitarian perspective than only delivering multi-session tertiary interventions for individuals with known psychological morbidity. The objectives of this project were to assess the efficacy of a single-session mindfulness intervention adopted from ACT and measure changes in levels of general and Covid-19-related psychopathology. The hypotheses were that there would be lower levels of depression, anxiety, and stress, and higher levels of psychological flexibility and higher levels of state mindfulness after a single session mindfulness-based intervention, compared to a matched control group.
Methodology
Ethics
Ethical approval was obtained from the Universiti Malaysia Sabah Medical Research Ethics Committee prior to commencement of this project. All participants provided informed consent.
Study design and setting
This was a quasi-experimental study conducted with university students during the Malaysian Conditional Movement Control Order (CMCO) period, when social gatherings were not permitted. During the CMCO period, participants attended a one-hour single-session online mindfulness intervention. Questionnaires were answered before and after the online session. Since this was a psychological intervention, it was impossible to blind participants, therefore both intervention and control groups received the same intervention at different times. The intervention group attended the session prior to the posttest, while the control group attended it afterwards.
Participants and sample size
By applying the nonequivalent groups design approach, and to ensure both groups were as similar as possible, equal numbers of participants from batches of undergraduate medical students were divided into intervention and control groups based on each year’s student roll. The sample size calculation was based on a formula described by Lehr, 42 using a significance criterion of 0.05, statistical power of 0.8, and effect size of 0.63. 43 The required sample size was 41 in each group, hence 82 participants cumulatively. The inclusion criteria were university students over the age of 18 who were locked down on campus, were willing to participate in the study, and were able to read and converse fluently in Malay. The exclusion criteria were non-consent and acute medical or psychiatric illness, which was obtained from the electronic medical records of the university hospital and corroborated with self-reported symptoms as a second-level safety net.
Questionnaires
Fear of Covid-19 Scale (FCV-19S)
The Fear of Covid-19 Scale 44 consists of seven items (e.g. “It makes me uncomfortable to think about coronavirus-19”). It is scored on a five-item Likert response scale ranging from 1 (strongly disagree) to 5 (strongly agree), with possible scores ranging from 7 to 35. Higher scores indicate more severe fears of COVID-19. 44 , 45 In this study, a validated Malay version 46 was administered that has very good internal consistency, with Cronbach alpha of 0.893 and McDonald’s omega of 0.894. 46
Depression anxiety and stress scales 21-item (DASS-21)
The DASS-21 47 measures the severity of depression, anxiety, and stress. It consists of 21 items that measure three different domains: depression (e.g. “I felt downhearted and blue”), anxiety (e.g. “I was worried about situations in which I might panic and make a fool of myself”), and stress (e.g. “I found it hard to calm down after something upset me”). Each item is scored on a four-point Likert scale ranging from 0 (did not apply to me at all over the last week) to 3 (applied to me very much or most of the time over the past week). Higher scores in each domain correlate with greater severity of emotional distress. In this study, the Malay version of the DASS-21 48 was administered, which has achieved acceptable Cronbach’s alpha values of 0.84, 0.74 and 0.79, respectively, for the depression, anxiety and stress scales, as well as a Cronbach’s alpha of 0.904 for the overall score. In addition, it had good factor loading values for most items (0.39 to 0.73). 48
Acceptance and Action Questionnaire (AAQ-II)
The AAQ-II 49 is a widely-used measure of experiential avoidance and psychological inflexibility. It was developed and revised from the original AAQ. 50 It is a unidimensional scale with 7 items rated on a 7-point Likert scale ranging from 1 (Never true) to 7 (Always true). Possible scores range from 7 to 49. Higher scores on the AAQ-II indicate higher levels of psychological inflexibility. The Malay version of AAQ-II used in this study has a Cronbach alpha of 0.910, excellent parallel reliability, and adequate concurrent validity. 51 We elected to use the unifactorial AAQ-II instead of the longer equivalents because the extant literature suggests that it is psychometrically superior and thus more reliable and valid. 49 , 51
Mindfulness, Attention, and Awareness Scale (MAAS)
The Mindful Attention Awareness Scale (MAAS) is used to assess awareness and attention in everyday life. It is a 15-item scale that measures the frequency of mindful states in day-to-day life using both general and situation-specific statements. A range of scores between 1 to 6 are allocated for each item. Totals range from 15 to 90, with higher scores indicating greater mindfulness. 26 In this study, the Malay version of the MAAS (MMAAS) was administered. The MMAAS has good internal consistency (Cronbach’s α = 0.851) and satisfactory psychometric properties. 52
Procedure
All interactions were online because social contact was not permitted. After the respondents had been divided into groups, they were presented with study information and gave consent. The intervention group was required to complete 2 sets of questionnaires, one before the intervention and one after the intervention. These were the Fear of Covid-19 Scale (FCV-19S), the Depression Anxiety and Stress Scales 21-item (DASS-21), the Acceptance and Action Questionnaire (AAQ-II), and the Mindfulness, Attention, and Awareness Scale (MAAS).
The pre-intervention forms were completed an hour before the intervention. After completing the pre-intervention forms, members of the intervention group participated in an hour-long online mindfulness session conducted via the Google Meet videoconferencing platform (https://meet.google.com/). The session was led by a moderator (Clinical Psychiatrist) and was based on the mindfulness components of the ultra-brief psychological interventions manual, which adopts ACT techniques. 41 All participants were involved in a group session online, but each was able to receive individualized feedback as required. The size of each group was 30 individuals.
During the first five minutes of the session, the moderator began by explaining the core principles behind mindfulness and tying it in to the three processes underlying psychological flexibility. Next, over the subsequent 45 minutes, the moderator demonstrated 3 different mindfulness techniques, allocating roughly 15 minutes to each technique: (1) the breathing technique, (2) the tactile sensation technique, and (3) the focusing on a specific musical instrument technique, all in relation to psychological flexibility. All three techniques were then practiced in smaller breakout rooms of 5-6 people, with various participants demonstrating to the moderator how they would perform it, and the moderator giving them feedback for improvement and periodically relating the practical activities back to psychological flexibility. The final 10 mins of the session were used for a Question and Answer (QnA) session during which the participants could raise any doubts and discuss their concerns. After the intervention, the respondents were required to fill in the post-intervention questionnaire at a time corresponding to 24 hours after the online session. The control group filled in the pre-intervention and post-intervention questionnaires at the same times as the intervention group and then subsequently crossed over to participate in the same intervention.
Data analysis
Data were analyzed according to the intention-to-treat principle. All participants were analyzed according to the condition (Intervention or Control) they were initially allocated to. IBM SPSS version 26.0 was employed for all statistical analysis. Descriptive statistics were used, with skewness and kurtosis calculated to assess whether normality criteria were met. Subsequently, repeated measures ANOVA was performed to assess whether there were differences between control and intervention groups. F values were reported with significance at p < 0.05 and partial eta-squared was also reported to indicate effect size. Estimated marginal means for each measured parameter were plotted on a graph for two time points – pre-intervention (T1) and post-intervention (T2).
Results
A total of 118 participants volunteered for the mindfulness intervention. They were divided into intervention and control groups, containing 61 and 57 participants respectively. The demographics of the students are as described in Table 1 . Table 2 illustrated that all continuous data for depression, anxiety, stress, FCV-19S, MAAS, and AAQ-II scores were normally distributed with skewness and kurtosis within appropriate ranges (+/-2 and +/-10 respectively) as per normality requirements. 53
Table 1. Demographics of the participants.
| Frequency | Percent | |
|---|---|---|
| Gender | ||
| Female | 74 | 62.700 |
| Male | 44 | 37.300 |
| Total | 118 | 100.000 |
| Age | 104 | 35.600 |
| 19-25 | 13 | 0.800 |
| 31-35 | 1 | 0.800 |
| 42 | 118 | 100.000 |
| Total | 22.310 | |
| Mean | ||
| Standard deviation | 4.523 |
Table 2. Descriptive statistics for the results (intervention and control).
| FCV-19S pre-test score | FCV-19S post-test score | Depression pre-test score | Depression post-test score | Anxiety pre-test score | Anxiety post-test score | Stress pre-test score | Stress post-test score | AAQ-II pre-test score | AAQ-II post-test score | MAAS pre-test score | MAAS post-test score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 61) | ||||||||||||
| Skewness | 1.148 | 1.806 | 0.812 | 2.665 | 1.666 | 1.606 | 1.026 | 1.219 | 0.796 | 1.803 | -0.694 | -1.028 |
| Kurtosis | 1.852 | 3.964 | -0.570 | 9.676 | 2.569 | 2.593 | 0.662 | 0.645 | -0.765 | 3.294 | -0.764 | -0.333 |
| Control (N = 57) | ||||||||||||
| Skewness | -0.100 | 0.318 | 0.960 | 1.258 | 0.651 | 0.875 | 0.695 | 0.641 | 0.617 | 0.973 | -0.401 | -0.428 |
| Kurtosis | -0.849 | -0.626 | 0.415 | 1.018 | -0.562 | 0.105 | -0.236 | -0.045 | -0.003 | 0.907 | -0.880 | -0.880 |
AAQ-II = Acceptance and Action Questionnaire; FCV-19S = Fear of Covid-19 Scale; MAAS = Mindfulness, Attention, and Awareness Scale.
As shown in Table 3 , normality checks were carried out on the residuals for FCV-19 scores and depression, stress, and mindfulness scores, which were all approximately normally distributed. A repeated measures ANOVA showed that there was no significant difference between control and intervention groups for any of these 4 variables.
Table 3. Tests for within-subjects effects.
| Measure | Type III sum of squares | Df | Mean square | F | Sig. | Partial eta squared |
|---|---|---|---|---|---|---|
| Depression | 1.714 | 1 | 1.714 | 0.637 | 0.426 | 0.005 |
| Anxiety | 223.716 | 1 | 223.716 | 34.361 | 0.000 | 0.299 |
| Stress | 8.970 | 1 | 8.970 | 2.859 | 0.094 | 0.024 |
| Fear of Covid-19 | 0.741 | 1 | 0.741 | 0.117 | 0.733 | 0.001 |
| Psychological flexibility | 143.781 | 1 | 143.781 | 11.010 | 0.001 | 0.087 |
| Mindfulness | 132.826 | 1 | 132.826 | 1.391 | 0.241 | 0.012 |
Source: test group.
* Sphericity assumed in all measures.
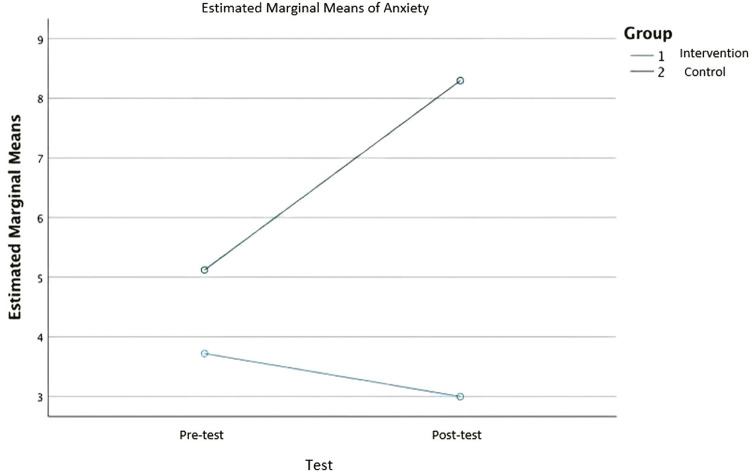
Normality checks were also carried out on the residuals for anxiety scores, which were approximately normally distributed. A repeated measures ANOVA showed that the anxiety scores differed significantly between control and intervention groups, F(1,116) = 34.361, p < 0.001, partial eta-squared = 0.299 ( Figure 1 ).
Figure 1. Estimated marginal means for anxiety.
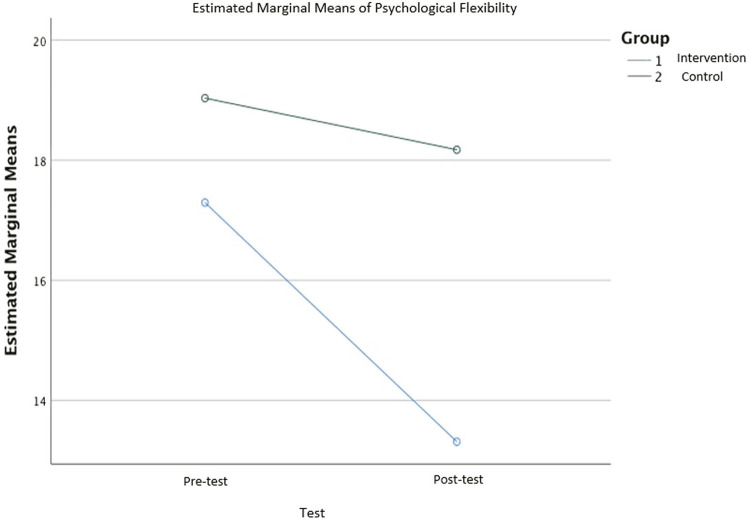
Normality checks were carried out on the residuals for psychological flexibility scores, which were approximately normally distributed. A repeated measures ANOVA showed that psychological flexibility differed significantly between control and intervention groups, F(1,116) = 11.010, p = 0.001, partial eta-squared = 0.087 ( Figure 2 ).
Figure 2. Estimated marginal means for psychological flexibility.
Discussion
This study demonstrates key findings, namely that a single-session online mindfulness intervention adopting ACT principles demonstrated efficacy in terms of reducing anxiety and improving psychological flexibility. This is also reflected in the literature, where other online single-session interventions have been equally efficacious. 54 - 56 This again underscores the importance of psychological flexibility as a construct that can be worked on in a pandemic situation. In view of the never-ending nature of the successive waves of Covid-19 and the uncertainty affecting almost all aspects of life, be it national quarantine and lockdown regulations, standard operating procedures, ability to travel, and/or the possibility of pursuing education and relationships, it is crucial that this intervention can boost psychological flexibility significantly, in order to enable people to achieve less rigid, more experientially open thought processes regarding the unpredictable and uncontrollable future. 57
Interestingly, there were no effects for depression, stress, fear of Covid-19, or mindfulness scores. This suggests that anxiety may be the key construct that is significantly higher in the population, 58 , 59 and therefore more amenable to reduction. Also, it may suggest that a longer number of sessions might be needed to show significant reductions in the above constructs. However, we need to balance cost effectiveness in terms of providing one efficacious intervention to more people versus many more efficacious interventions, but to fewer people. Moreover, the results of this study echo findings from other literature that suggests that single session interventions are of equal efficacy to longer multi-session ones. 60 , 61
This study certainly has certain limitations. Firstly, all of the participants are medical students, who might have higher awareness and knowledge regarding updates about COVID-19, compared to other students on different courses or to the general public. 62 - 64 This could therefore represent a selection bias. Secondly, the sample size of 118, including both the intervention and the control group, was relatively small, partly due to internet access limitations and time constraints and also because three batches of medical students had already undergone mindfulness intervention training pre-research, thus raising the possibility that their inclusion would unduly distort the final results. As it stood, only 183 students had not undergone mindfulness training before. One more limitation includes the lack of an active control group. The significant effects on reduction of anxiety and increasing psychological flexibility may have simply been caused by the fact that there was interaction with a caring and supportive professional, rather than being related to any specific effect of the mindfulness technique used.
On the other hand, the absence of effects on the other scales may also simply represent the need for sustained practice to modify the aspects measured. This can be tested with one or more follow-up assessments. Lastly, since the participants were locked down on campus and staying in proximity to each other in the hostel, it was difficult to blind participants and there was a possibility of the intervention group participants sharing the techniques taught during the mindfulness intervention with the control group, hence affecting the results.
In conclusion, the results of this single-session intervention study are crucial because there is a need for evidence-based short interventions that can be provided to the largest number of people to yield the greatest good, rather than for multiple-session interventions which no doubt have unquestionably higher efficacy due to the additive effect of multiple sessions, but are exhaustive to run and have high attrition rates, and may result in fewer individuals getting the benefits of mindfulness training and thus have less public health impact. 65 ACT techniques have been successfully delivered in single-session modalities with good evidence for multiple indications 66 - 70 and it is especially crucial we offer them to undergraduate populations, because they are in the age group with the highest incidence of depressive and anxiety disorders. 71 Therefore, it is our greatest hope that this single session intervention will be adopted in other universities as this intervention has shown limited efficacy, albeit in a single center, and larger sample sizes would be ideal to explore the efficacy of this intervention further.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med . 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 . 2020. [cited 2020 Mar 11]. Internet. www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .
- 3.Malasya. Ministry of Health Malaysia Current COVID-19 pandemic situation in Malaysia . 2021. [cited 2021 Jan 1]. Internet. covid-19.moh.gov.my/
- 4.Tang A. Malaysia announces movement control order after spike in Covid-19 cases (updated) 2020. Mar 16, Internet. www.thestar.com.my/news/nation/2020/03/16/malaysia-announces-restricted-movement-measure-after-spike-in-covid-19-cases .
- 5.Pang NT, Kamu A, Mohd Kassim MA, Chong Mun H. Analyses of the Effectiveness of Movement Control Order (MCO) in reducing the COVID-19 confirmed cases in Malaysia. J Health Transl Med . 2021;(1):16–27. [Google Scholar]
- 6.Salvaraji L, Abdul Rahim SS, Jeffree MS, Omar A, Tze Ping Pang N, Ahmedy F, et al. The importance of high index of suspicion and immediate containment of suspected COVID-19 cases in institute of higher education Sabah, Malaysia Borneo. Malaysian J Public Heal Med . 2020;20:74–83. [Google Scholar]
- 7.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. 102066 Asian J Psychiatr . 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shanmugam H, Juhari JA, Nair P, Chow SK, Ng CG. Impacts of COVID-19 pandemic on mental health in Malaysia: a single thread of hope. Malaysian J Psychiatry . 2020;29:1–7. [Google Scholar]
- 9.Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM . 2020;113:311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wind TR, Rijkeboer M, Andersson G, Riper H. The COVID-19 pandemic_ The ‘black swan’ for mental health care and a turning point for e-health. 100317 Internet Interv . 2020;20 doi: 10.1016/j.invent.2020.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sukumaran T. Coronavirus Malaysia: PM blames Sabah election as among causes of huge infection surge. South China Morning Post . 2020. [cited 2020 Oct 6]. Internet. www.scmp.com/week-asia/health-environment/article/3104421/coronavirus-malaysia-pm-blames-sabah-election-among .
- 12.Peters M, ten Cate O. Bedside teaching in medical education: a literature review. Perspect Med Educ . 2014;3:76–88. doi: 10.1007/s40037-013-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med . 2009;4:304–307. doi: 10.1002/jhm.540. [DOI] [PubMed] [Google Scholar]
- 14.Salam A, Siraj HH, Mohamad N, Das S, Yousuf R. Bedside teaching in undergraduate medical education: Issues, strategies, and new models for better preparation of new generation doctors. Iran J Med Sci . 2011;36:1–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Levin J. In: Psychiatry of pandemics . Huremović D, editor, editor. Nova Iorque: Springer International Publishing; 2019. Mental health care for survivors and healthcare workers in the aftermath of an outbreak; pp. 127–141. [Google Scholar]
- 16.Mian A, Khan S. Medical education during pandemics: a UK perspective. 100 BMC Med . 2020;18 doi: 10.1186/s12916-020-01577-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rubin GJ, Wessely S. The psychological effects of quarantining a city. m313 BMJ . 2020;368 doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 18.Kassim MAM, Pang NTP, Mohamed NH, Kamu A, Ho CM, Ayu F, et al. Relationship between fear of COVID-19, psychopathology and sociodemographic variables in Malaysian population. 10.1007/s11469-020-00444-4 Int J Ment Health Addict . 2022;20(3):1303–1310. doi: 10.1007/s11469-020-00444-4. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kupferman SI, Schultz JC. Supporting students with psychiatric disabilities in postsecondary education: important knowledge, skills, and attitudes. J Postsecond Educ Disabil . 2015;28:25–40. [Google Scholar]
- 20.Mohd Kassim MA, Pang N, James S. COVID-19 Pandemic - a review and assessing higher education institution undergraduate student’s mental health. Borneo Epidemiol J . 2020;1:96–103. [Google Scholar]
- 21.Son C, Hegde S, Smith A, Wang X. Effects of COVID-19 on college students ’ mental health in the United States: interview survey study. J Med Internet Res . 2020;22:e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus . 2020;12:e7541. doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hafiz Mukhsam M, Saffree Jeffree M, Tze Ping Pang N, Sharizman Syed Abdul Rahim S, Omar A, Syafiq Abdullah M, et al. A university-wide preparedness effort in the alert phase of COVID-19 incorporating community mental health and task-shifting strategies: experience from a Bornean institute of higher learning. Am J Trop Med Hyg . 2020;103:1201–1203. doi: 10.4269/ajtmh.20-0458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baiano C, Zappullo I, Conson M, Di Mauro G, Petra M, Piacenti M, et al. Tendency to worry and fear of mental health during Italy’s COVID-19 lockdown. 5928 Int J Environ Res Public Health . 2020;17 doi: 10.3390/ijerph17165928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marazziti D, Pozza A, Di Giuseppe M, Conversano C. The psychosocial impact of COVID-19 pandemic in Italy: a lesson for mental health prevention in the first severely hit European country. Psychol Trauma Theory, Res Pract Policy . 2020;12:531–533. doi: 10.1037/tra0000687. [DOI] [PubMed] [Google Scholar]
- 26.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol . 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 27.Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Pract . 2003;10:125–143. [Google Scholar]
- 28.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther . 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev . 2010;30:865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palladino CL, Ange B, Richardson DS, Casillas R, Decker M, Gillies RA, et al. Measuring psychological flexibility in medical students and residents: a psychometric analysis. 20932 Med Educ Online . 2013;18 doi: 10.3402/meo.v18i0.20932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masuda A, Tully EC. The role of mindfulness and psychological flexibility in somatization, depression, anxiety, and general psychological distress in a nonclinical college sample. J Evidence-Based Complement Altern Med . 2012;17:66–71. [Google Scholar]
- 32.Laurie J, Blandford A. Making time for mindfulness. Int J Med Inform . 2016;96:38–50. doi: 10.1016/j.ijmedinf.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 33.Moore S, Barbour R, Ngo H, Sinclair C, Chambers R, Auret K, et al. Determining the feasibility and effectiveness of brief online mindfulness training for rural medical students: a pilot study. 104 BMC Med Educ . 2020;20 doi: 10.1186/s12909-020-02015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohd Kassim MA, Pang NTP, Shoesmith WD, Tseu MWL, Malindoi EA, Yeoh YX. Validation of Bahasa Malaysia Version of psychological mindedness in a university population. IIUM Med J Malaysia . 2021;20:81–88. [Google Scholar]
- 35.Spijkerman MPJ, Pots WTM, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin Psychol Rev . 2016;45:102–114. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 36.Cavanagh K, Strauss C, Cicconi F, Griffiths N, Wyper A, Jones F. A randomised controlled trial of a brief online mindfulness-based intervention. Behav Res Ther . 2013;51:573–578. doi: 10.1016/j.brat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Lim J, Leow Z, Ong JC, Pang L-S, Lim E. The effects of online group mindfulness training on stress and sleep quality during the COVID-19 pandemic in Singapore: a retrospective equivalence trial. JMIR Ment Heal . 2021;8:e21757. doi: 10.2196/21757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.El Morr C, Maule C, Ashfaq I, Ritvo P, Ahmad F. Design of a mindfulness virtual community: a focus-group analysis. Health Informatics J . 2020;26:1560–1576. doi: 10.1177/1460458219884840. [DOI] [PubMed] [Google Scholar]
- 39.Mak WWS, Chio FHN, Chan ATY, Lui WWS, Wu EKY. The efficacy of internet-based mindfulness training and cognitive-behavioral training with telephone support in the enhancement of mental health among college students and young working adults : randomized controlled trial corresponding author. J Med Internet Res . 2017;19:e84. doi: 10.2196/jmir.6737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El Morr C, Ritvo P, Ahmad F, Moineddin R. Effectiveness of an 8-week web-based mindfulness virtual community intervention for university students on symptoms of stress, anxiety, and depression: randomized controlled trial. JMIR Ment Heal . 2020;7:e18595. doi: 10.2196/18595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pang NTP, Shoesmith WD, James S, Nor Hadi NM, Eugene Boon Yau K, Loo JL. Ultra brief psychological interventions for COVID-19 pandemic: introduction of a locally-adapted brief intervention for mental health and psychosocial support service. Malays J Med Sci . 2020;27:51–56. doi: 10.21315/mjms2020.27.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lehr R. Sixteen S-squared over D-squared: a relation for crude sample size estimates. Stat Med . 1992;11:1099–1102. doi: 10.1002/sim.4780110811. [DOI] [PubMed] [Google Scholar]
- 43.Öst LG. The efficacy of acceptance and commitment therapy: an updated systematic review and meta-analysis. Behav Res Ther . 2014;61:105–121. doi: 10.1016/j.brat.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 44.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. 10.1007/s11469-020-00270-8 Int J Ment Health Addict . 2020;20(03):1537–1545. doi: 10.1007/s11469-020-00270-8. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mohd Kassim MA, Ayu F, Kamu A, Pang NTP, Ho CM, Algristian H, et al. Indonesian version of the fear of COVID-19 scale: validity and reliability. Borneo Epidemiol J . 2020;1:124–135. [Google Scholar]
- 46.Pang NTP, Kamu A, Hambali NL, Ho CM, Mohd Kassim MA, Mohamed NH, et al. Malay version of the fear of COVID-19 scale: validity and reliability. Int J Ment Health Addict . 2022;20:263–272. doi: 10.1007/s11469-020-00355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales . Sydney: Psychology Foundation of Australia; 1995. [Google Scholar]
- 48.Musa R, Fadzil MA, Zain Z. Translation, validation and psychometric properties of Bahasa Malaysia version of the Depression Anxiety and Stress Scales (DASS) ASEAN J Psychiatry . 2007;8:82–89. [Google Scholar]
- 49.Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire--II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther . 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 50.Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Rec . 2004;54:553–578. [Google Scholar]
- 51.Shari NI, Zainal NZ, Guan NC, Sabki ZA, Yahaya NA. Psychometric properties of the acceptance and action questionnaire (AAQ II) Malay version in cancer patients. PLoS One . 2019;14:e0212788. doi: 10.1371/journal.pone.0212788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zainal N, Nor-Aziyan Y, Subramaniam P. Psychometric properties of the Malay-translated Mindfulness, Attention and Awareness Scale (MAAS) in a Malaysian population. Malaysian J Psychiatry . 2015;24:33–41. [Google Scholar]
- 53.Baron RM, Kenny DA. The moderator--mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. 1173 J Pers Soc Psychol . 1986;51 doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 54.Mahmood L, Hopthrow T, De Moura GR. A moment of mindfulness: computer-mediated mindfulness practice increases state mindfulness. PLoS One . 2016;11:e0153923. doi: 10.1371/journal.pone.0153923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kemper KJ, Khirallah M. Acute effects of online mind–body skills training on resilience, mindfulness, and empathy. J Evidence-Based Complement Altern Med . 2015;20:247–253. doi: 10.1177/2156587215575816. [DOI] [PubMed] [Google Scholar]
- 56.Kemper KJ. Brief online mindfulness training: immediate impact. J Evidence-Based Complement Altern Med . 2017;22:75–80. doi: 10.1177/2156587216639199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dawson DL, Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Context Behav Sci . 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. 112954 Psychiatry Res . 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hassannia L, Taghizadeh F, Moosazadeh M, Zarghami M, Taghizadeh H, Dooki AF, et al. Anxiety and depression in health workers and general population during COVID-19 in IRAN: a cross-sectional study. Neuropsychopharmacol Reports . 2021;41:40–49. doi: 10.1002/npr2.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shikatani B, Fredborg BK, Cassin SE, Kuo JR, Antony MM. Acceptability and perceived helpfulness of single session mindfulness and cognitive restructuring strategies in individuals with social anxiety disorder: a pilot study. Can J Behav Sci . 2019;51:83–89. [Google Scholar]
- 61.Mrazek MD, Smallwood J, Schooler JW. Mindfulness and mind-wandering: finding convergence through opposing constructs. Emotion . 2012;12:442–448. doi: 10.1037/a0026678. [DOI] [PubMed] [Google Scholar]
- 62.Ding Y, Du X, Li Q, Zhang M, Zhang Q, Tan X, et al. Risk perception of coronavirus disease 2019 (COVID-19) and its related factors among college students in China during quarantine. PLoS One . 2020;15:e0237626. doi: 10.1371/journal.pone.0237626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wong JGWS, Cheung EPT, Cheung V, Cheung C, Chan MTY, Chua SE, et al. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med Teach . 2004;26:657–659. doi: 10.1080/01421590400006572. [DOI] [PubMed] [Google Scholar]
- 64.Ashcroft J, Byrne MHV, Brennan PA, Davies RJ, Davies RJ. Preparing medical students for a pandemic: a systematic review of student disaster training programmes. Postgrad Med J . 2021;97:368–379. doi: 10.1136/postgradmedj-2020-137906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kroska EB, Roche AI, O’Hara MW. How much is enough in brief acceptance and commitment therapy? A randomized trial. J Context Behav Sci . 2020;15:235–244. [Google Scholar]
- 66.Murthy V, Hussey I, McHugh L. A single-session acceptance and commitment therapy intervention targeting shame in people experiencing homelessness: a randomized multiple baseline. Psyarxiv . 2020 May 18;:1–13. doi: 10.31234/osf.io/3hpuq. Online ahead of print. [DOI] [Google Scholar]
- 67.Hadlandsmyth K, Dindo LN, Wajid R, Sugg SL, Zimmerman MB, Rakel BA. A single-session acceptance and commitment therapy intervention among women undergoing surgery for breast cancer: a randomized pilot trial to reduce persistent postsurgical pain. Psychooncology . 2019;28:2210–2217. doi: 10.1002/pon.5209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barreto M, Tran TA, Gaynor ST. A single-session of acceptance and commitment therapy for health-related behavior change: an open trial with a nonconcurrent matched comparison group. J Context Behav Sci . 2019;13:17–26. [Google Scholar]
- 69.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med . 2009;37:58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 70.Dindo L, Marchman J, Gindes H, Fiedorowicz JG. A brief behavioral intervention targeting mental health risk factors for vascular disease: a pilot study. Psychother Psychosom . 2015;84:183–185. doi: 10.1159/000371495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bewick B, Koutsopouloub G, Miles J, Slaad E, Barkham M. Changes in undergraduate students’ psychological well-being as they progress through university. 63345 Stud High Educ . 2010;35 [Google Scholar]