“Out of intense complexities, intense simplicities emerge” (W. Churchill)
In the last decade, we have been witnessing a paradigm shift in the approach to the management of individuals with atrial fibrillation (AF). This change has been grounded mainly on the increasing aging of the world-wide population and the improvements in the net-clinical benefit of direct oral anticoagulants, as well as the now available options for rhythm and rate control. The clinical scenario in AF that needs to be handled by clinical cardiologists is becoming much more complex than expected. Furthermore, pushed on by the COVID-19 pandemic outbreak, innovative solution for providing the best care in any situation has been envisioned and applied counting on the help of technological tools. From a disease-centered approach almost focused on the risk of thromboembolism and heart failure, to a patient-centered way to look at health problems unrevealed a wealth of complexity that cardiologists are deemed to simplify. In this light, the “Atrial Fibrillation Better Care” (ABC) pathway approach proposed in the most updated European Society of Cardiology Guidelines is a roadmap that highlights how facing complexity is very much needed to improve outcomes of individuals with AF [1]. Thus, the contemporary implementation of patient care of AF imposes to pursue equitable solutions accounting for the multidimensional aspects that encompasses any individual, primarily recognizing the differential impact of biological sex and sociocultural gender of cardiovascular health that deserves consideration to reach high-quality scientific outputs [2]. In 2023, the efficacy and safety of cardiovascular interventions must be tested in both sexes to recognize similarities or differences when present.
In this context, we read with great interest the paper of Guo Y et al. [3], a secondary analysis of the mAFA-II (Mobile Health Technology for Improved Screening and Optimized Integrated Care in AF) trial aimed at exploring whether the effectiveness of mobile-Health implemented ABC intervention varies by patient’s biological sex. While a significant risk reduction of 1-year adverse events (i.e., stroke, thromboembolism, all-cause death, and rehospitalization) was evident in patients allocated to mAFA intervention regardless of sex; yet the sex-by-intervention interaction analysis unrevealed differences in terms of the occurrence of all-cause death and bleeding events.
We applaud the effort of questioning using the lens of sex if men and women differentially benefit from this mobile tech solution to implement the translation in practice of the ABC pathway. It is already known how the current assessment of clinical complexity among patients with cardiovascular disease implies the understanding that both biological sex and sociocultural gender can extern a widely different effect on cardiovascular outcome [4]. The integration of sex and gender considerations in AF research is even more clinically relevant as women with AF are more likely to be undertreated with anticoagulants, to be symptomatic, to have a higher comorbidities burden and finally to disproportionally experience adverse outcome overtime; thus, women are those individuals that would benefit the most from an ABC approach delivered through mobile health technology. A holistic approach to AF care was successful in achieving a reduction of the risk of worse outcome, regardless of sex suggesting that a multidimensional management help in overcoming unbiased. Nevertheless, it is intriguing how male individuals benefited the most by the mAFA-II intervention versus the usual care in terms of bleeding events, all cause death, acute heart failure, acute coronary syndrome or recurrent AF as showed by model adjusted for many confounders. Beyond the underpowered sample size, only 38% of female participants, unmeasured biases in the approach to women with AF might be related to the impact of more detrimental social determinants of health. In fact, prior data on AF patients have showed how the social vulnerability of women as compared to men plays a major role in the occurrence of adverse cardiovascular health events [5]. Unfortunately, such information was not available missing the opportunity to identify the contributing mediation effect of social determinants of health (SDOH) in explaining the results.
The descriptive analyses of the mAFA-II trial clearly confirmed a different clinical phenotype of AF patients by sex. Specifically, male participants allocated to mAFA intervention were younger and less comorbid as those in the usual care while women had a higher burden of comorbidities than their female counterpart in the usual care group. Different clinical complexity might be relevant in identifying the subgroup of patients that benefit the most from an intervention. As expected, as opposed to usual care, the optimization the ABC pathway resulted in a higher proportion of both female and male anticoagulated and receiving rhythm control. The cluster randomized trial design suited the need of testing differences in a method to provide patient care, as opposed to individually randomized controlled trials. Therefore, the inference of conclusions that are applicable at individual level might be particularly challenging.
In the clinical prognosis of individuals with AF, inequitable access to cardiovascular health is a timely matter of concern, with many intertwined determinants that can be difficult to unravel and define. Mobile solution can overcome the many barriers and obstacles in delivering high-quality integrated care in AF regardless of any individual features. It has already reported the existence of sex differences in the adoption of technology, with men adopting more medical applications as they perceived it as more useful than women. Beyond it, although increasing digital access was massive under the wave of COVID-19 pandemic, there can be issues with digital competence and literacy that cannot be simply assumed, amongst users and healthcare providers. Furthermore, the mAFA-II trial enrolled exclusively Chinese patients with AF that might have a very different sociocultural background that seems to limit the generalizability of the reported findings.
The contribution of Guo Y et al. is deed to remember ourselves how much room for improvement is available for understanding and tailoring sex-specific intervention in cardiovascular health. After all, in the upcoming years, to envision solutions for AF care, we must apply an intersectional approach to consider the impact of all biological and non-biological factors influencing the health of every person with cardiovascular disease. “Out of intense complexities, intense simplicities emerge”, sex-specific integrated ABC pathway might be the simple avenue to handle complexity (Fig. 1).
Fig.1.
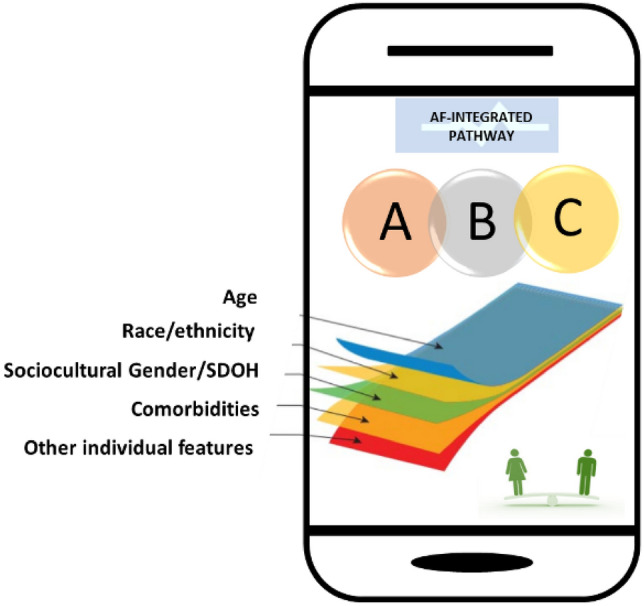
Integration of the ABC pathway with biological and non-biological factors
Availability of data and materials
Not applicable.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Human and animal rights statement and Informed consent
This article does not contain any studies directly involving human participants. Thus, formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. 2021;42:373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 2.Tannenbaum C, Ellis RP, Eyssel F, Zou J, Schiebinger L. Sex and gender analysis improves science and engineering. Nature. 2019;575:137–146. doi: 10.1038/s41586-019-1657-6. [DOI] [PubMed] [Google Scholar]
- 3.Guo Y, Corica B, Romiti GF, Proietti M, Zhang H, Lip GYH. Efficacy of mobile health-technology integrated care based on the ‘atrial fibrillation better care’ (ABC) pathway in relation to sex: a report from the mAFA-II randomized clinical trial. Intern Emerg Med. 2023 doi: 10.1007/s11739-022-03188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raparelli V, Wright CX, Corica B, Sharma G, Lindley K, Brackett A, Pilote L, Wood MJ, Dreyer RP. Interventions targeted to address social determinants of health in ischemic heart disease: a sex- and gender-oriented scoping review. Can J Cardiol. 2022;38:1881–1892. doi: 10.1016/j.cjca.2022.06.025. [DOI] [PubMed] [Google Scholar]
- 5.Lindley KJ, Aggarwal NR, Briller JE, et al. Socioeconomic determinants of health and cardiovascular outcomes in women: JACC review topic of the week. J Am Coll Cardiol. 2021;78:1919–1929. doi: 10.1016/j.jacc.2021.09.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


