Abstract
Introduction
Mediterranean countries experience frequent desert dust storm (DDS) events originating from neighbouring Sahara and Arabian deserts, which are associated with significant increase in mortality and hospital admissions, mostly from cardiovascular and respiratory diseases. Short-term exposure to ambient air pollution is considered as a trigger for symptomatic exacerbations of pre-existing paroxysmal atrial fibrillation (AF) and other types of heart arrhythmia. The Mitigating the Health Effects of Desert Dust Storms Using Exposure-Reduction Approaches clinical randomised intervention study in adults with AF is funded by EU LIFE+programme to evaluate the efficacy of recommendations aiming to reduce exposure to desert dust and related heart arrhythmia effects.
Methods and analysis
The study is performed in three heavily exposed to desert dust regions of the Eastern Mediterranean: Cyprus, Israel and Crete-Greece. Adults with paroxysmal AF and implanted pacemaker are recruited and randomised to three parallel groups: (a) no intervention, (b) interventions to reduce outdoor exposure to desert dust, (c) interventions to reduce both outdoor and indoor exposure to particulate matter during desert dust episodes. Eligible participants are enrolled on a web-based platform which communicates, alerts and makes exposure reduction recommendations during DDS events. Exposure changes are assessed by novel tools (smartwatches with Global Positioning System and physical activity sensors, air pollution samplers assessing air quality inside and outside participant’s homes, etc). Clinical outcomes include the AF burden expressed as the percentage of time with paroxysmal AF over the total study period, the incidence of ventricular arrhythmia episodes as recorded by the participants’ pacemakers or cardioverters/defibrillators and the disease-specific Atrial Fibrillation Effect on QualiTy-of-Life questionnaire.
Ethics and dissemination
Local bioethics’ authorities approved the study at all sites, according to national legislations (Cyprus: National Bioethics Committee, Data Protection Commissioner and Ministry of Health; Greece, Scientific Committee and Governing Board of the University General Hospital of Heraklion; Israel: Institutional Review Board (‘Helsinki committee’) of the Soroka University Medical Center). The findings will be publicised in peer-reviewed scientific journals, in international conferences and in professional websites and newsletters. A summary of the results and participants’ interviews will be included in a documentary in English, Greek and Hebrew.
Trial registration number
ClinicalTrials.gov Identifier; NCT03503812.
Keywords: Pacing & electrophysiology, PUBLIC HEALTH, Protocols & guidelines, Health policy, Clinical Trial
STRENGTHS AND LIMITATIONS OF THIS STUDY
Throughout the study, personal monitoring through wearable sensors assesses the compliance of adults with atrial fibrillation (AF) to recommendations aiming to reduce the exposure to desert dust storms (DDS).
Air cleaning devices continuously filter indoor air in homes of adults with AF during DDS events.
Personalised assessment reduces the risk of exposure misclassification.
The study uses validated tools to assess health outcomes, including AF burden and quality of life.
Advanced age and/or other comorbidities (eg, impaired vision) of study participants may compromise the use of wearable devices and smartphones.
Introduction
Exposure to air pollution is a well-established risk factor for cardiorespiratory morbidity and mortality.1 2 Among other outcomes, exposure to particulate matter (PM) is associated with higher incidence of cardiac infarction3 and ventricular arrythmias.4 Furthermore, ambient air pollution is also associated with atrial fibrillation (AF), the most common heart rate disturbance, affecting almost 2% of the population worldwide, and a known risk factor for heart failure, stroke, hospital admission and mortality.5–8
Although the evidence on the relationship between PM and incidence of heart arrhythmias comes from studies of anthropogenic particulate pollution (road traffic, industry, etc), particulate pollution in urban settlements may have substantial contributions from non-anthropogenic sources, such as desert dust storms (DDS).9 This is very common for regions with geographical proximity to the global desert dust belt, such as the Mediterranean basin. In Mediterranean countries, DDS events may appear in more than 15% of the days of the year with the greater frequency and intensity of the events recorded in the south-eastern Mediterranean.10 11
Despite the natural origin of DDS events, recent evidence supports their strong association with adverse health outcomes such as increased all-cause and cause-specific mortality and morbidity.12–16 Even though, direct evidence linking the incidence of AF episodes with DDS exposure is still lacking, recent studies have identified short term exposure to ambient air pollution as a trigger for AF episodes.17–19
The current public health strategy across many countries during anthropogenic high pollution events is to issue alerts or warnings to the population, targeting vulnerable groups such as the known cardiac patients. These alerts usually are accompanied by recommendations to avoid vigorous outdoor activity and stay indoors during the events.20 21 Although there is a well-established rationale behind these recommendations,22 adherence has been found to vary widely, depending on several personal and other parameters.23 In the case of DDS events, a similar strategy of alerts and recommendations is followed on their appearance,20 but to date, there is no real-life evidence supporting the efficacy of these recommendations in reducing personal exposure to dust, either in the outdoor or the indoor environments, not or their role in mitigating the related health risks.
The ‘Mitigating the Health Effects of Desert Dust Storms Using Exposure-Reduction Approaches (MEDEA) Atrial Fibrillation study’ has been designed to study the feasibility and effectiveness of simple exposure reduction recommendations (including behavioural changes with/without indoor air cleaners vs no intervention) in a randomised cohort of AF patients in parallel groups during DDS events in South-Eastern Mediterranean countries. This behavioural intervention study will quantify the impact of these recommendations both in terms of change in personal exposure to air pollution and in terms of AF burden reduction and improvement in health-related quality of life (HRQoL). The project is carried out by an eight-partner consortium across three heavily DDS-exposed sites in the Eastern Mediterranean, Cyprus, Israel and Crete-Greece. The study benefits from a series of novel environmental exposure assessment tools such as smartwatches equipped with Global Positioning System (GPS) and physical activity sensors that enable the objective assessment of personal compliance to the recommendations, while the availability of air pollution samplers allows the quantification of outdoor and indoor air pollution exposure among the study population.
Methods and analysis
The Standard Protocol Items: Recommendations for Interventional Trials checklist has been used for this report.24
Population
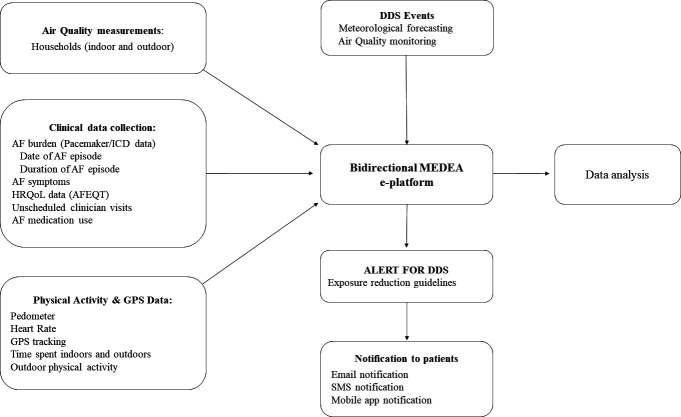
The target population is men and women with AF and previously implanted dual lead (atrial and ventricular) pacemaker or implantable cardioverter defibrillator (ICD), who attend the heart arrhythmia clinics at Nicosia General Hospital in Cyprus, Soroka Clinical Research Center in Beer-Sheba, Israel and University Hospital of Heraklion, Crete, Greece. Additional details on the recruitment of participants are provided in online supplemental material. Screening of the AF patients at each site started in Fall 2018 and Mitigating the Health Effects of Desert Dust Storms Using Exposure-Reduction Approaches (MEDEA) personnel continues to identify and follow-up eligible AF patients throughout the three follow-up periods in 2019, 2021 and 2022. The SPIRIT flow diagram for the AF study is presented in figure 1.
Figure 1.
MEDEA Atrial fibrillation study SPIRIT flow diagram: the schedule of enrolment, allocation, interventions and assessments in the AF panel study according to SPIRIT template. AF, atrial fibrillation; ICD, implantable cardioverter defibrillator; MEDEA, Mitigating the Health Effects of Desert Dust Storms Using Exposure-Reduction Approaches; SPIRIT, Standard Protocol Items: Recommendations for Interventional Trials.
bmjopen-2022-069809supp001.pdf (74.6KB, pdf)
Eligibility criteria
Eligible for the study are patients with permanent atrial or dual chamber pacemakers or ICDs implanted at least 2 months prior to randomisation, with:
History of paroxysmal AF.
Detection of AF episodes in pacemaker/ICD monitoring of >6 min in duration.
The study puts no limitations on patients’ medication regimens during the study period.
Exclusion criteria are permanent AF, reversible causes of AF (eg, hyperthyroidism), inability to understand and use study tools (smartphones, software applications), active smoking, terminal illness or not living at least 5 days per week in the same household.
Study design
Patients are randomised with a 1:1:1 ratio, using a random assignment tool, into three parallel groups: group 1: no additional intervention during DDS (‘business as usual’ scenario), group 2: interventions for outdoor exposure reduction, group 3: combined interventions for both outdoor and indoor exposure reduction. The study design offers the opportunity to assess (a) outdoor exposures to PM, (b) indoor exposures to PM and (c) related health outcomes in three parallel groups during the same events of DDS with and without intervention measures.
Study interventions and recommendations
To reduce the outdoor and indoor exposure to DDS pollution, relevant recommendations have been developed. In brief, for outdoor exposure reduction intervention, it is recommended to the participants to stay indoors and avoid any intense physical activity outdoors, competitive sports and unnecessary walks (group 2 and group 3). For indoor exposure reduction intervention, it is recommended to close doors and windows, to seal possible openings around doors and windows minimising outdoor air penetration and to filter indoor air by using continuously an air cleaning device (Coway Storm 1516D, Coway, South Korea, see online supplemental material for further details). Indoor exposure reduction measures are implemented at the households of the participants in group 3. In order to enhance uptake and acceptability of the recommendations, we produced relevant audiovisual spots with animated guidelines in Greek, Hebrew and English languages. The English version for the outdoor exposure reduction intervention (group 2, online supplemental video S1) and for the outdoor and indoor exposure reduction intervention (group 3, online supplemental video S2) are available in online supplemental material.
bmjopen-2022-069809supp002.mov (44.7MB, mov)
bmjopen-2022-069809supp003.mov (73.5MB, mov)
MEDena Health-Hub
For the purposes of the project, a patient-centred web-based platform (the MEDena Health-Hub) and a smart phone application (the MEDEApp) have been developed. These tools receive input from existing models that forecast DDS events in the countries that take part in the study and provide alerts to participants and researchers with the appearance of DDS events through text messaging and smartphone applications, coupled with relevant exposure reduction recommendations (personalised to each participant, according to the randomisation group, they belong—group 1, 2 or 3). The forecasting models for desert dust rely on the transport scheme of the desert dust, the proximity of the given area to the desert source and other factors.25 The platform algorithm takes into account these forecasts for DDS and issues alert to participants based on increased PM concentrations (including both particles of desert dust and anthropogenic origin) compared with site-specific background levels as described previously.26 Of note, so far, there is no well-established classification system for DDS severity, thus the forecasting models and alert algorithms treat all DDS events equally.27
Using cloud technologies, the above-mentioned tools offer the opportunity to store health and exposure data from all participants (groups 1, 2 and 3), as these are recorded through the wearable sensors and online questionnaires.
Following randomisation, participant’s sociodemographic characteristics, medical and medication history as well as information on household location and characteristics, are uploaded to the MEDena Health-Hub. In addition, a wearable sensor (EMBRACE smartwatch (Embrace Tech LTD, Cyprus) is provided to the participant, who is asked to wear it daily throughout the study period, except during bedtime, bathing and swimming. The study personnel are responsible to train the AF patients in the tools and procedures to be followed during the study. A leaflet with instructions on the use of the EMBRACE smartwatch and MEDEApp is also provided to the participants. Additional details on the MEDena Health-Hub and MEDEA App have been published previously.26
Exposure assessment
Wearable sensors: physical activity as well as time spent outdoors are assessed by the sensors of the EMBRACE smartwatch. The smartwatch is supplied with GPS, which records continuously the time the participant spends indoors and outdoors, and activity tracking (pedometer) hardware and software, which records steps and heart rate. In addition, the smartwatch also includes an embedded sim card and Wi-Fi connectivity and can be used as a stand-alone device. Finally, the software can synchronise the sensors, so that data are transferred to the cloud database marked with the same timestamp.
Air pollution sensors: particle samplers (Harvard High Volume Cascade Impactors, Harvard University, USA) are placed outside and inside representative participants’ houses. Furthermore, indoor, commercial low volume air quality sensors (OPC-N3 Optical Particle Counters, Alphasense, United Kingdom) are used to assess the levels of indoor exposure to PM across the three intervention groups. The indoor and outdoor particle samplers use Teflon filters which are analysed to give the concentrations of PM10, PM2.5, black carbon and elements inside and outside representative houses during DDS and DDS-free days.
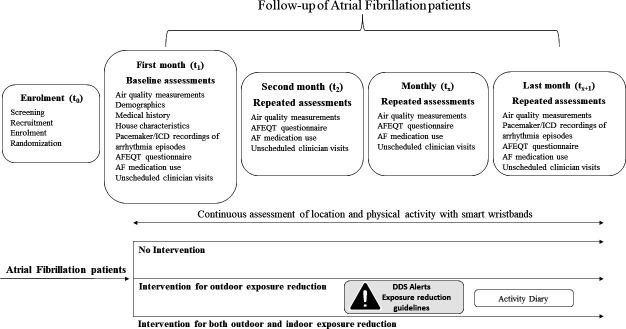
Questionnaires: each participant is asked to complete an activity questionnaire following each DDS event, which assesses the reported compliance to the recommendations. A schematic of the AF study is presented in figure 2.
Figure 2.
MEDEA atrial fibrillation study schematic diagram. The bidirectional MEDena Health-Hub is updated with meteorological forecasting and air-quality information regarding DDS events and sends alerts and exposure reduction guidelines to AF patients. At the same time, the cloud database is automatically collecting the physical activity and GPS data from the smartwatches worn by the participants. Researchers also manually upload participants’ clinical data and air quality measurements. AF, atrial fibrillation; AFEQT, Atrial Fibrillation Effect on QualiTy of Life questionnaire; DDS, Desert Dust Storm; GPS, global positioning system; HRQoL, Health Related Quality of Life; SMS, short messaging service text message.
The recordings of wearable GPS and activity sensors are coupled with the measurements collected from the air pollution samplers and the questionnaires to provide a much higher spatiotemporal accuracy for personal air pollution exposure and an estimate of the compliance to the intervention. To ensure minimal technical problems with the wearables and devices, as well as to facilitate the compliance of the participants, we maintain an extended support system characterised by frequent communication with participants and their families and implement simple and cost-effective setting adjustments to the device to ensure systematic activation of the data collection application at regular time intervals, increase battery duration and facilitate uninterrupted operation of smartwatch background process.28
Baseline and follow-up clinical assessments
Eligible AF patients after screening are invited for a baseline clinical assessment, which includes detailed questions on sociodemographic characteristics, health symptoms, particularly heart arrhythmias symptoms, utilisation of medical care, medication history and household environmental characteristics, including tobacco smoke exposure. A baseline assessment of the AF/ventricular arrhythmia episodes is obtained after downloading relevant data from the participants’ pacemakers or ICDs.
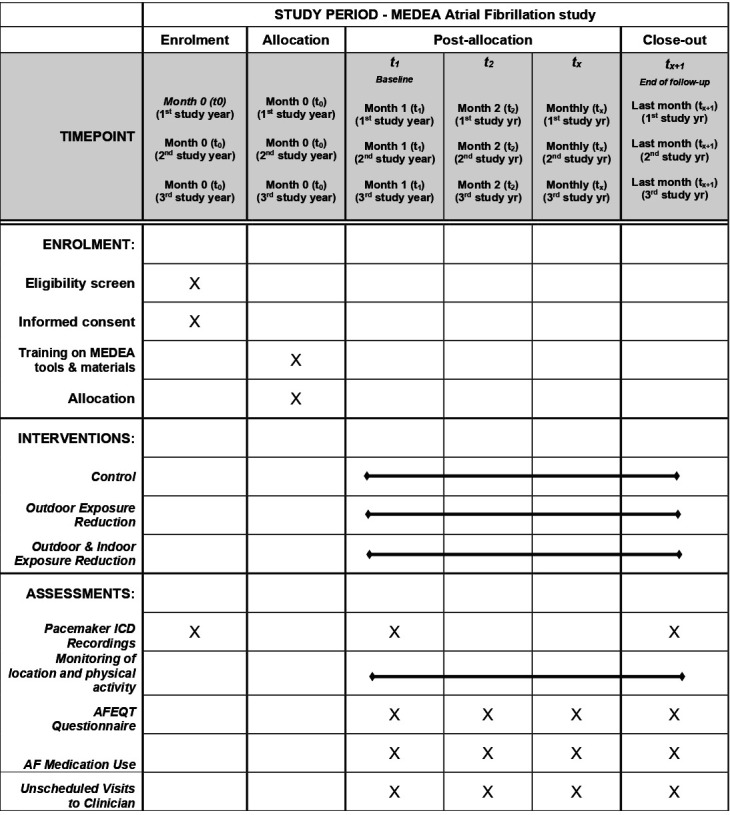
Follow-up periods span for 6 months and include monitoring of the daily location and physical activity of AF patients using the smartwatches. Phone interviews at baseline and then at every 1 month throughout the follow-up period are performed collecting information on heart arrhythmia symptoms control, medication use, unscheduled visits to health professional for arrhythmias and health-related quality of life using the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT, license number: 20171404) questionnaire.29 Incidence of AF/ventricular arrhythmia episodes is recorded daily using the already implanted participants’ pacemaker or ICD during the follow-up period. The recorded episodes are downloaded by interrogation of the pacemaker or ICD after the end of the study period during a visit to the Hospital Arrhythmia Clinic. The timeline and description of baseline and follow-up assessments in the AF panel study are presented in figure 3. Non-participation to the clinical visits was the only reason for discontinuation of the study participation. Additional details on the intervention implementation are provided in online supplemental material.
Figure 3.
MEDEA atrial fibrillation study assessments timeline. Timeline of baseline and follow-up assessments in atrial fibrillation panel study. AFEQT, Atrial Fibrillation Effect on QualiTy of Life questionnaire; DDS, Desert Dust Storm; GPS, global positioning system; HRQoL, Health Related Quality of Life; ICD, implantable cardioverter defibrillator.
AF outcomes and data analysis
The primary health outcome in the study is the reduction in the AF burden defined as the percentage of time with AF during the whole study period. A 20% reduction in the AF burden is considered as clinically significant. For the primary analysis, we will compare the combined effect in the two intervention groups versus the control group. Next, we will make comparisons between each of the intervention groups and the control group and between the intervention groups. Furthermore, for HRQoL, changes equal or greater than (±) five points in the AFEQT questionnaire score are considered clinically significant. Other health outcomes include the presence or absence of arrhythmia symptoms in the prior 4-week period, heart rate variability, arrhythmia medication use and unscheduled hospital visits for heart arrhythmias. Apart from the health outcomes, the exposure reduction across the intervention groups will be assessed as an outcome of this study, estimating directly the compliance and the effectiveness of the recommendations.
Sample size calculation: there are no studies that evaluated the reduction in AF burden attributed to the reduction in exposure to ambient air pollution. Nevertheless, assuming a mean follow-up period of 6 months and an effect size of 20% change in the outcome, a study sample size of 118 is required to demonstrate a statistically significant result. This number is estimated for performing a two-way repeated measures Analysis of Variance (ANOVA) statistical test for the comparison of the intervention and control groups and assuming an alpha value at 0.05, power of 80% and a 50% correlation between repeated measurements.
Statistical analysis plan: descriptive statistics will be presented using summaries of key variables in the form of mean (SD) and median (range) for normally and non-normally distributed variables, respectively. For categorical variables, the distribution in percentages will be presented. Comparisons between intervention and control groups will be carried out using the two-way repeated measures ANOVA statistic test for continuous variables and the χ2 test for categorical variables. The statistical analysis plan for the impact of intervention on exposure will include the estimation of the fraction of outdoor particles that penetrate indoors and remain suspended using the infiltration factor approach as described previously30 and will employ multiple linear regression models to quantify the effect of intervention measures on indoor PM levels. The statistical analysis for the impact of intervention on HRQoL (AFEQT score) will rely on a linear mixed effects (hierarchical) regression model, which will include fixed effects for intervention group and subject-specific random intercepts. The model will be adjusted for several covariates including age, gender, year of study, site of study and climatic factors.
Ethics and dissemination
The MEDEA AF panel study has been approved by national authorities at all sites. In Cyprus, approvals have been obtained from the Cyprus National Bioethics Committee (EEBK EΠ 2017.01.141), by the Data Protection Commissioner (No. 3.28.223) and Ministry of Health (No 5.34.01.7.2E). In Greece, approvals have been obtained from the Scientific Committee (25/04/2018, No: 1748) and the Governing Board of the University General Hospital of Heraklion (25/22/08/2018). In Israel, approval has been obtained from the Institutional Review Board (‘Helsinki committee’) of the Soroka University Medical Center (No 0374–17-SOR). Participants sign the informed consent from the corresponding centre at recruitment. The study has been registered and approved by the clinicaltrials.gov online repository.
Dissemination plan
The study findings will be disseminated according to the predefined dissemination plan of the LIFE MEDEA project. The project dissemination plan includes publication of the study findings in international peer-reviewed scientific journals, as well as international scientific conferences, with authorship eligibility as defined by the International Committee of Medical Journal Editors recommendations. In addition, the findings will be also communicated to the scientific community, regulatory authorities, patient organisations and the general public through publication of a series of short-piece articles for professional websites and newsletters as well as through the organisation of educational activities and open public fairs in the three study sites. Finally, the LIFE MEDEA project dissemination plan also includes the production of 50 min documentary with a summary of the study findings that will be made available in English, Greek and Hebrew languages. The anonymised study data set and the statistical code will be made available online in an appropriate, open access, public repository.
Patient and public involvement
The above-mentioned documentary will include interviews from study participants and participating clinicians reporting their experiences during the study.
Supplementary Material
Acknowledgments
The authors are grateful to the members of the MEDEA Advisory Committee for the continuous feedback provided to the LIFE MEDEA project, the hospital administrations for their support to carry out the project and the participants and their family members for their contribution to the project.
Footnotes
Contributors: PAn: methodology, data curation, writing—original draft preparation, review and editing; PK: methodology, investigation, software, data curation, project administration writing—original draft preparation, review and editing; SP: conceptualisation, methodology, data curation, writing—original draft preparation; NM: methodology, writing—review and editing; IP: data curation, investigation, writing—review and editing; PAv: data curation, investigation, writing—review and editing; ES: conceptualisation, methodology, investigation, resources, writing—review and editing; IA: data curation, investigation, writing—review and editing; VN: conceptualisation, methodology, writing—review and editing, project administration; GS: conceptualisation, data curation, software, visualisation, writing—review and editing; ER: conceptualisation, data curation, software, visualisation, writing—review and editing; CK: visualisation, resources, writing—review and editing; FT: conceptualisation, methodology, resources, software, writing—review and editing; CS: conceptualisation, methodology, resources, writing—review and editing; PKo: conceptualisation, methodology; software, validation, resources, writing—review and editing; PY: conceptualisation, methodology; software, validation, writing—review and editing, supervision, funding acquisition.
Funding: This work was supported by the LIFE 2016 Programme (LIFE16 CCA/CY/000041) of the European Commission. The funders had and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Funder contact info: easme-life@ec.europa.eu
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Di Q, Dai L, Wang Y, et al. Association of short-term exposure to air pollution with mortality in older adults. JAMA 2017;318:2446–56. 10.1001/jama.2017.17923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 2006;56:709–42. 10.1080/10473289.2006.10464485 [DOI] [PubMed] [Google Scholar]
- 3.Wu Y, Li M, Tian Y, et al. Short-term effects of ambient fine particulate air pollution on inpatient visits for myocardial infarction in beijing, china. Environ Sci Pollut Res Int 2019;26:14178–83. 10.1007/s11356-019-04728-8 [DOI] [PubMed] [Google Scholar]
- 4.Folino F, Buja G, Zanotto G, et al. Association between air pollution and ventricular arrhythmias in high-risk patients (ARIA study): a multicentre longitudinal study. Lancet Planet Health 2017;1:e58–64. 10.1016/S2542-5196(17)30020-7 [DOI] [PubMed] [Google Scholar]
- 5.Camm AJ, Kirchhof P, Lip GYH, et al. Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the european society of cardiology (ESC). Eur Heart J 2010;31:2369–429. 10.1093/eurheartj/ehq278 [DOI] [PubMed] [Google Scholar]
- 6.Meyre P, Blum S, Berger S, et al. Risk of hospital admissions in patients with atrial fibrillation: a systematic review and meta-analysis. Can J Cardiol 2019;35:1332–43. 10.1016/j.cjca.2019.05.024 [DOI] [PubMed] [Google Scholar]
- 7.Lowres N, Olivier J, Chao T-F, et al. Estimated stroke risk, yield, and number needed to screen for atrial fibrillation detected through single time screening: a multicountry patient-level meta-analysis of 141,220 screened individuals. PLoS Med 2019;16:e1002903. 10.1371/journal.pmed.1002903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruddox V, Sandven I, Munkhaugen J, et al. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol 2017;24:1555–66. 10.1177/2047487317715769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodsite ME, Hertel O, Johnson MS, et al. Urban air quality: sources and concentrations. In: Anonymous. Air Pollution Sources, Statistics and Health Effects: Springer. 2021: 193–214. 10.1007/978-1-0716-0596-7 [DOI] [Google Scholar]
- 10.Stafoggia M, Zauli-Sajani S, Pey J, et al. Desert dust outbreaks in southern europe: contribution to daily PM₁₀ concentrations and short-term associations with mortality and hospital admissions. Environ Health Perspect 2016;124:413–9. 10.1289/ehp.1409164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Querol X, Pey J, Pandolfi M, et al. African dust contributions to mean ambient PM10 mass-levels across the mediterranean basin. Atmospheric Environment 2009;43:4266–77. 10.1016/j.atmosenv.2009.06.013 [DOI] [Google Scholar]
- 12.Griffin DW. Atmospheric movement of microorganisms in clouds of desert dust and implications for human health. Clin Microbiol Rev 2007;20:459–77. 10.1128/CMR.00039-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Middleton N, Yiallouros P, Kleanthous S, et al. A 10-year time-series analysis of respiratory and cardiovascular morbidity in nicosia, cyprus: the effect of short-term changes in air pollution and dust storms. Environ Health 2008;7:39. 10.1186/1476-069X-7-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neophytou AM, Yiallouros P, Coull BA, et al. Particulate matter concentrations during desert dust outbreaks and daily mortality in nicosia, cyprus. J Expo Sci Environ Epidemiol 2013;23:275–80. 10.1038/jes.2013.10 [DOI] [PubMed] [Google Scholar]
- 15.Domínguez-Rodríguez A, Báez-Ferrer N, Abreu-González P, et al. Impact of desert dust events on the cardiovascular disease: A systematic review and meta-analysis. J Clin Med 2021;10:727. 10.3390/jcm10040727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al B, Bogan M, Zengin S, et al. Effects of dust storms and climatological factors on mortality and morbidity of cardiovascular diseases admitted to ED. Emerg Med Int 2018;2018:3758506. 10.1155/2018/3758506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Link MS, Luttmann-Gibson H, Schwartz J, et al. Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol 2013;62:816–25. 10.1016/j.jacc.2013.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yitshak Sade M, Vodonos A, Novack V, et al. Can air pollution trigger an onset of atrial fibrillation: a population-based study. Air Qual Atmos Health 2015;8:413–20. 10.1007/s11869-014-0295-2 [DOI] [Google Scholar]
- 19.Lee HH, Pan SC, Chen BY, et al. Atrial fibrillation hospitalization is associated with exposure to fine particulate air pollutants. Environ Health 2019;18:117. 10.1186/s12940-019-0554-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinni P, Kouis P, Dimitriou H, et al. Health effects of desert dust storm events in the south-eastern mediterranean: perceptions and practices of local stakeholders. East Mediterr Health J 2021;27:1092–101. 10.26719/emhj.21.037 [DOI] [PubMed] [Google Scholar]
- 21.Kelly FJ, Fuller GW, Walton HA, et al. Monitoring air pollution: use of early warning systems for public health. Respirology 2012;17:7–19. 10.1111/j.1440-1843.2011.02065.x [DOI] [PubMed] [Google Scholar]
- 22.Holgate S. Review of the UK air quality index. A report by the committee on the medical effects of air pollutants. In: Health Protection Agency, London. 2011. [Google Scholar]
- 23.D’Antoni D, Smith L, Auyeung V, et al. Psychosocial and demographic predictors of adherence and non-adherence to health advice accompanying air quality warning systems: a systematic review. Environ Health 2017;16:100. 10.1186/s12940-017-0307-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Querol X, Tobías A, Pérez N, et al. Monitoring the impact of desert dust outbreaks for air quality for health studies. Environ Int 2019;130:104867. 10.1016/j.envint.2019.05.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kouis P, Papatheodorou SI, Kakkoura MG, et al. The MEDEA childhood asthma study design for mitigation of desert dust health effects: implementation of novel methods for assessment of air pollution exposure and lessons learned. BMC Pediatr 2021;21:13. 10.1186/s12887-020-02472-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benedetti A, Reid JS, Knippertz P, et al. Status and future of numerical atmospheric aerosol prediction with a focus on data requirements. Atmos Chem Phys 2018;18:10615–43. 10.5194/acp-18-10615-2018 [DOI] [Google Scholar]
- 28.Michanikou A, Kouis P, Karanicolas K, et al. Setup of consumer wearable devices for exposure and health monitoring in population studies. J Vis Exp 2023;192:e63275. 10.3791/63275 [DOI] [PubMed] [Google Scholar]
- 29.Spertus J, Dorian P, Bubien R, et al. Development and validation of the atrial fibrillation effect on quality-of-life (AFEQT) questionnaire in patients with atrial fibrillation. Circ Arrhythm Electrophysiol 2011;4:15–25. 10.1161/CIRCEP.110.958033 [DOI] [PubMed] [Google Scholar]
- 30.Diapouli E, Chaloulakou A, Koutrakis P. Estimating the concentration of indoor particles of outdoor origin: A review. J Air Waste Manag Assoc 2013;63:1113–29. 10.1080/10962247.2013.791649 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-069809supp001.pdf (74.6KB, pdf)
bmjopen-2022-069809supp002.mov (44.7MB, mov)
bmjopen-2022-069809supp003.mov (73.5MB, mov)