Abstract
There is a current global push to identify and implement best practice for delivering maximum impact from development research in low-income and middle-income countries. Here, we describe a model of research and capacity building that challenges traditional approaches taken by western funders in Africa. Tackling Infections to Benefit Africa (TIBA) is a global health research and delivery partnership with a focus on strengthening health systems to combat neglected tropical diseases, malaria and emerging pathogens in Africa. Partners are academic and research institutions based in Ghana, Sudan, Rwanda, Uganda, Kenya, Tanzania, Zimbabwe, Botswana, South Africa and the UK. Fifteen other African countries have participated in TIBA activities. With a starting budget of under £7 million, and in just 4 years, TIBA has had a verified impact on knowledge, policy practice and capacity building, and on national and international COVID-19 responses in multiple African countries. TIBA’s impact is shown in context-specific metrics including: strengthening the evidence base underpinning international policy on neglected tropical diseases; 77% of research publications having Africa-based first and/or last authors; postgraduate, postdoctoral and professional training; career progression for African researchers and health professionals with no net brain drain from participating countries; and supporting African institutions. Training in real-time SARS-CoV-2 viral genome sequencing provided new national capabilities and capacities that contributed to both national responses and global health security through variant detection and tracking. TIBA’s experience confirms that health research for Africa thrives when the agenda and priorities are set in Africa, by Africans, and the work is done in Africa. Here, we share 10 actionable recommendations for researchers and funders from our lessons learnt.
Keywords: Control strategies, Epidemiology, Health policy, Health services research, Health systems
Summary box.
Evaluations of global health research partnerships and collaboration have identified potential structural and systemic biases that can compromise the partnership’s function, productivity, output, impact and sustainability.
Tackling Infections to Benefit Africa (TIBA), a global health research and delivery partnership focusing on neglected tropical diseases, malaria and emerging pathogens, succeeded in solving some of these challenges.
TIBA’s approach was based on four guiding principles; Africa-led research and delivery agendas; doing the work for Africa in Africa; inclusivity, ‘leaving no-one behind’; and delivery through equitable partnerships.
TIBA’s impact shown in context-specific metrics including: strengthening the evidence base underpinning international policy on neglected tropical diseases; 77% of research publications having Africa-based first and/or last authors; postgraduate, postdoctoral and professional training; career progression for African researchers and health professionals; supporting African institutions and policy makers; building pandemic response capacity, including real-time genome sequencing.
TIBA’s approach has demonstrated what equitable global health research and delivery looks like and what it can achieve.
From our lessons learnt, we share 10 actionable recommendations for researchers and funders for successful equitable global health research partnerships, which generate sustained gains, buy-in, trust and impact.
Introduction
Contextualised research and innovation are critical contributors to economic growth and improved livelihoods. In Africa, research improving health and health systems is especially important because the continent suffers a disproportionate burden of infectious diseases. These have a huge impact on childhood mortality rates1 and compromise progress towards the United Nations (UN) Sustainable Development Goals (SDGs). Endemic diseases, notably the neglected tropical diseases (NTDs) and malaria, place a heavy burden on health systems with limited budgets, and negatively impact livelihoods, especially in the most marginalised communities, and they also compromise global health security by reducing local capacity to respond to epidemics such as Ebola, measles and COVID-19.
In order to generate effective health interventions and build resilient health systems to tackle infectious diseases, Africa needs a strong knowledge ecosystem comprising scientific research, innovation and appropriately trained personnel. We have previously highlighted the obstacles to achieving this2 including domestic funding and financing. The latter is often provided by international partners including richer western countries.
Conducting research, capacity building/strengthening and technological transfer with international funding and partners in low and middle-income countries (LMICs) as are the majority of African countries can be challenging.3 The arena is replete with several structural biases (box 1) and there are often difficulties associated with the outputs of the research itself. Evaluations of development aid-funded health research and delivery programmes have identified some systemic limitations4 and proposed various mitigation strategies. These include: focusing on recipient country priorities and needs; translation of research results into context-relevant interventions; monitoring impact; and making sustainable and sustained gains on development.4 While these recommendations are obvious and non-controversial, implementing them is not so simple. That requires a cultural change in the ways the collaborations and partnerships work and engage with affected communities and local stakeholders. Here, we explore how these challenges can be effectively addressed using a case study of the TIBA (Tackling Infections to Benefit Africa) partnership. We aim to demonstrate how we built an equitable and impactful global health research and delivery partnership and share recommendations from the lessons we learnt.
Box 1. Structural biases in international development research.
External rather than local research funding and priority setting. This can lead to research without local buy-in or uptake because it does not speak to local priorities and needs.22
Unequal power dynamics between research partners where donor country partners are the primary beneficiaries. This translates to several factors including the reported23 under-representation in first and last authorship positions in papers published from collaborative research done in Africa16 and the consequent poorer career progression for the African partners.
Ineffective translation of research findings into policy and practice and poor deployment of innovations. For example, the 2022 Final Evaluation Report of the UK Newton Fund24 stated: ‘…several ‘translation’ challenges …including that it is too early; that it takes time; that many projects did not include translation in their design or budgets; and that there are often contextual barriers inhibiting translation’.
Failure to engage with all stakeholders at every stage of the research, including affected communities and partners who implement the changes. This requires contextualising international best practice (eg,25 with local knowledge and participation).
Unsustained capacity building whose measures of success do not go beyond the number of people trained26 despite the clear demonstration of successful capacity building models from Africa.10
What is TIBA?
In 2016, the UK government launched several research funding schemes to support cutting-edge research and innovation to address global challenges in LMICs as part of the UK’s official development assistance programme. These schemes included the Global Challenges Research Fund and National Institute of Health Research (NIHR)’s Global Health Research Fund.
In 2017, with the belief that having access to the best science and technology locally would facilitate African governments to respond to local and continental health challenges better, a group of UK and Africa-based scientists already conducting human health-related research in Africa put together a partnership called TIBA to address health research and delivery needs in Africa. TIBA stands for Tackling Infections to Benefit Africa and is the KiSwahili verb among others ‘to cure an infection’. The partnership applied for and obtained funding of just under £7 million from the UK’s NIHR Global Health Programme. The funding scheme required a UK lead applicant that legally managed the finances while having co-applicants from LMICs. Accordingly, we put together a programme of work that harnessed the combined expertise and technical capabilities in biomedical and social sciences at ten partner institutions and the University of Edinburgh to deliver research to help reduce the burden and threat of infectious diseases by informing health policy and practice, as well as strengthening health systems.
TIBA focused on tackling NTDs, malaria and emerging pathogens within African health systems. Partners were academic and research institutions (see figure 1) based in Botswana, Ghana, Kenya, Rwanda, South Africa, Sudan, Tanzania, Uganda, Zimbabwe and the UK. Researchers and professionals in health-related fields from 15 other African countries participated in TIBA research, capacity building and professional development.
Figure 1.
Tackling Infections to Benefit Africa (TIBA) partners and principles.
TIBA took an approach that would inherently avoid those pitfalls characteristic of extractive research partnerships/collaborations (box 1). TIBA’s approach was defined by our guiding principles (figure 1) designed to embed the values that would propel TIBA into a progressive, impactful and equitable partnership.
The two critical ingredients for TIBA partners buying into these guiding principles were common purpose and trust. The partnership grew out of existing collaborations among the various researchers, some of which had been running for as long as 20 years. Building relationships of trust and accruing social capital does not happen in an instant. Rather, mutually respectful, equitable and sustainable collaborations are built on the foundation of social capital with trust being the currency that sustains the relationships.
In terms of common purpose, TIBA wanted a working model that would maximise the benefit to the Africa partners and communities. So we took the little used path of: first, conducting our research in the broader context of the lived experience and expertise of partners in local health systems; and, second, shifting the prioritisation of health research agendas for Africa to institutions, organisations and experts in Africa. The partnership’s PIs had over 200 years of cumulative experience of conducting research in Africa and internationally competitive academic reputations. Their expertise spanned the complete healthcare system research spectrum: clinical, basic scientific research (human and experimental), operational research, social science and health service and products delivery science. Almost all the PIs had trained in Africa at some stage of their careers (undergraduate, postgraduate and postdoctoral) and most had made use of an African healthcare system. This lived experience of both health research and health systems in Africa was instrumental in designing contextualised research projects that addressed local health needs. This was the foundation for ensuring the research agenda was led by the African partners and addressed locally agreed health needs, thus speaking to our first two guiding principles (figure 1).
TIBA purposively took a multidisciplinary, multiple disease approach to encompass activities spanning the full innovation to application pathway addressing local knowledge or technological capabilities gaps across diseases and countries. This also included all aspects of infectious diseases management—from basic research to uptake by local communities—in a single, unified framework. This met an often articulated but rarely addressed need to view infectious disease management not in isolation but in the context of local health systems and wider societal issues. The broad approach might be criticised for lack of focus, but the results and impact it achieved which are described below will demonstrate its advantages.
TIBA practises a policy of inclusion, speaking to our third guiding principle of leaving no-one behind (figure 1), through the grant application and research work,5 to translation and dissemination. Consultations were conducted with affected communities, researchers and their institutions, policy makers and practitioners through seminars, focus group discussions, panel discussions and regular meetings. Communication of study findings and knowledge exchange was tailored to the audience and includes academic publications, policy briefs6 edutainment7 and film.8
Finally, TIBA wanted to ensure that the partnership was equitable and not just a vehicle that relegates African expert scientists to data gatherers for international researchers.9 Thus, for everyone involved, TIBA was a partnership of equals, reflected in the make-up of the directorate, PIs and external advisory group. Eighty percent of TIBA’s budget was earmarked for spending in Africa, with the African partner PIs deciding on how the funding was spent in accordance with their country’s health research priorities to ensure agency for all the partners. This approach speaks to our fourth guiding principle (figure 1). Thus, TIBA aimed for demonstrably equitable partnerships which we defined as partnerships with local agency, local control of the majority of resources, local prioritisation of research and impact areas and mutual respect between south-south and between south-north partners.
The how: delivering a research, training and translation agenda
TIBA’s programme of work was set out in work packages feeding into a clearly articulated theory of change (figure 2). The work plan includes (1) world-class basic scientific research, (2) capacity building; (3) proactively translating research into health technologies and policies benefiting target populations/communities; (4) responding to health emergencies by supporting diagnostics development and deployment, data sharing and real-time analysis of pathogen genomes and (5) engaging in two-way communication with all relevant stakeholders.
Figure 2.
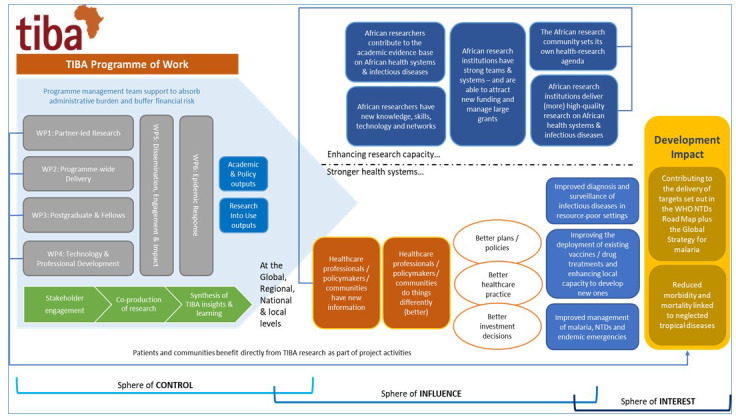
TIBA’s theory of change. Graphic produced by LTSI International. NTDs, neglected tropical diseases; TIBA, Tackling Infections to Benefit Africa.
Each work package is led by a TIBA PI with world-class expertise in the specific area. For example, our technology transfer and training is led by two PIs who have been running large training programmes for African postgraduate students and postdoctoral research over several years10 and our community engagement lead of the dissemination for action work package has developed best practice based on his research in Southern Africa11
For our research work packages, TIBA commissioned two types of projects: first, rapid impact projects undertaken by each partner institution addressing a specific local need.6 They addressed a specific current knowledge gap that was resulting in either non-deployment of diagnostics or interventions or a lack of operational knowledge to improve the health of affected populations. The second group were flagship collaborative projects between multiple partner countries, harnessing local expertise to contribute to reducing the burden of infectious diseases on the continent.6 These projects were purposively designed to engender south–south collaborations. All projects were reviewed within the partnership ensuring a fit with national and international priorities. We explicitly required all projects to have a clear pathway to impact such as changes to national or international health policy to benefit affected communities prior to commencement.
TIBA conducted conventional postgraduate and postdoctoral fellowship training alongside workshops and professional development activities to strengthen the knowledge and technical ecosystem at individual, institutional, national and regional and international levels. Notably, apart from short-term visiting fellowships, all of TIBA’s training was delivered in African institutions. This avoided us outsourcing training, thus enabling us to build local capacity to deliver these in Africa. Our training and capacity building adhered to the ‘Seven Principles for Strengthening Research Capacity in LMICs’.12 In keeping with all our activities being Africa-led, skills and professional practice training responded to needs identified by the African partners.
TIBA included a work package focusing on strengthening the partnership’s ability to contribute to health emergency responsiveness. For this, we identified tools and capabilities required for future health emergencies and set out to build local capabilities in managing those emergencies. We leveraged technological advancement to build an ecosystem that equipped local scientists and health service professionals to respond quickly and effectively. One such example was the real-time genome sequencing workshop in 2018 that provided training, equipment, reagents and support to TIBA partners in collaboration with the ARTIC Network. By providing the complete packake of training, equipment, reagents and bioinformatic support, TIBA enabled the partner labs to be self-suffient and scale-up in-country acttivities.13 Local challenges addressed included investigating chikungunya virus14 rotavirus, Ebola and measles outbreaks. The corollary of this in the advent of the SARS-CoV-2 pandemic was that TIBA partners were well prepared to generate evidence that informed the response of both national governments and international agencies.15
We worked closely with Ministries of Health in all partner countries as well as the African Union Development Agency (AUDA)-NEPAD, WHO African Region and the African Academy of Sciences. This ensured TIBA’s work was aligned to both national and continental health strategies and priorities including the WHO NTD roadmap, the Global Technical Strategy for Malaria, the African Union’s Agenda 2063 (and its domestication of the UN SDGs) and the WHO AFRO’s Research for Health: a strategy for the African region, 2016–2025. We took on responsive research and advisory roles, and engaged with relevant national and supranational policy makers, as articulated in our sphere of influence in figure 2, to translate our research into policy and practice. Details of how we delivered each of these aspects of TIBA’s work and the sturctures we used for this are available on our web page on https://tiba-partnership.org/.
The outcomes: TIBA’s impact
TIBA’s two desired outcomes were to strengthen health systems in the partner countries and to enhance health research capacity. This was to be achieved through scientific research, capacity building, research translation into health practice and policies benefiting target populations/communities, responding to health emergencies, and engaging with relevant stakeholders to enhance the knowledge ecosystem. TIBA’s outcomes are summarised in figure 3 and were assessed against our theory of change (figure 2).
Figure 3.
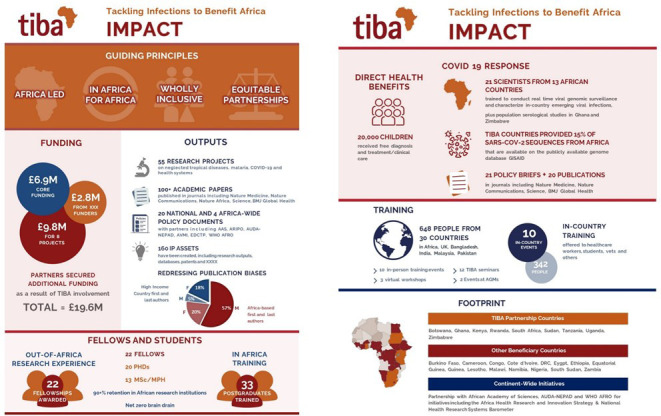
Summary of TIBA’s 4-year impact (2017–2021). TIBA, Tackling Infections to Benefit Africa.
In terms of our research, our key outputs included: (1) 55 research projects delivered, all aligned with national and Africa-wide health priorities; (2) over 100 academic papers published including many in leading journals such as Nature, Nature Medicine, Nature Communications and Science and in discipline leaders such as PLOS NTDs and BMJ Global Health. Of particular note, 77% of our publications had Africa-based first or last authors, clearly demonstrating that the programme was primarily benefiting the careers of African rather than UK researchers—increasing the representation of African first and last authors on research conducted in Africa remains an ambition for many partnerships that has yet to be achieved16; (3) contributions to 20 national and four Africa-wide policy documents, including AUDA-NEPAD’s Health Research & Innovation Strategy for Africa 2018–2030—this was particularly important for the COVID-19 response as will be described later; (4) 160 IP assets including databases and software code mostly owned by the African partners and (5) 20 000 people directly benefiting from NTD and malaria treatment, diagnosis or health education in Africa using tools or policies delivered by the partnership.
Our basic research has contributed to international policy guidelines including the new WHO NTD Roadmap, international and national policy briefs on the deworming of adolescent girls and women of childbearing age and SARS-CoV-2 national responses.
In terms of training and capacity building, key outputs included 20 PhD and 13 MSc/MPH degrees awarded, all at African institutions, and 22 postdoctoral fellowships providing overseas research experience for 3–12 months, with all fellows returning to their home countries. There was over 90% retention of African researchers, fellows and students over the first 4 years of the partnership, with an effective zero net contribution to brain drain in the partner countries (as some of the UK-based TIBA members returned to Africa). TIBA provided training to 638 people from 30 counties through 12 in-country technical training events benefiting African researchers, healthcare workers and students. These included a Good Financial Grant practice workshop led by the African Academy of Sciences with 80 participants from 20 countries including the UK, Bangladesh, India, Malaysia and Pakistan.
A most recent example of our translation and emergency response was TIBA’s contribution to the COVID-19 responses at national, continental and global level. TIBA PIs were able to pivot their expertise and work to the COVID-19 responses in various ways. For example, several partner PIs were involved in national SARS-CoV-2 genome sequencing, providing new national capacities that helped generate 15% of virus sequences from Africa. These were all made freely available as soon a they were obtained, so contributing to global health security through variant detection and tracking. TIBA partners also conducted research on diagnostics, protection of healthcare workers17 manufacturing and procurement analyses18 and provision of medical oxygen.15 We produced over 20 scientific publications on SARS CoV-2, 14 technical reports, 21 policy briefs and two open access databases.6 We continue to provide analytics support for WHO AFRO through a weekly situational report.6
The verdict: independent evaluations of TIBA’s impact
The impact of TIBA’s research and training activities was regularly monitored and periodically reviewed independently through our Monitoring, Evaluation & Learning (MEL) framework.6 Our End of Programme MEL report concluded ‘TIBA’s ambitious aim to shift the centre of gravity of health research remained central to TIBA activities and there is strong evidence that TIBA has achieved this. TIBA’s governance and management processes enabled African partner institutions to define the agenda and direction of their research, while enabling African-led peer review to ensure academic excellence and rigour. African leadership was a very real and valued part of TIBA. The programme made very positive and tangible impact in relation to capacity building of African scientists and health researchers and to contributing to the academic evidence base on African health systems and infectious disease. All TIBA partners have benefited from access to training and capacity-building opportunities, with all TIBA training events held in Africa, in Edinburgh or online to build local capacity to deliver training’.
TIBA’s model of an effective progressive research partnership has been commended by the WHO Regional Director for Africa, the President of the African Academy of Sciences and the WHO Director General. For example, TIBA’s contributions to the COVID-19 response in Africa were acknowledged in the Annual Report of the Regional Director on the work of the Africa Region presented during the 72nd session of the WHO Regional Committee for Africa in September 2022.19
Added value from the TIBA approach
One of the challenges in many African countries is maintaining the continuity and vibrancy of the talent pipeline regardless of discipline.20 TIBA took a vertical approach, providing professional development and exchange opportunities for all health/science career stages—postgraduate training, junior, middle and senior levels. This approach provided multilayered knowledge and talent recharging which is critical for building intergenerational expertise resilience, allowing continuity of operations.
TIBA’s emphasis on collaboration between African countries to work on regional health challenges for our larger projects encouraged South-to-South linkages. Sharing expertise between southern partners has improved methodologies for fieldwork, use of techniques and knowledge sharing, and has generated new collaborations.
TIBA went beyond co-production of knowledge and responsive research to solve real-life problems beyond the partnership through policy formulation, professional development and co-delivery of knowledge exchange to organisations. We created a community of practice through our training of global health researchers and the funders on good financial grants management as well as introducing the theory of change and 4Es practice for development grant applications used by our main funder (NIHR).
It is also important to recognise that global health security is built on strong local health security. TIBA demonstrated the value of this through the real-time viral genome sequencing training and technology transfer. This provided new national capacities that allowed TIBA partner countries in Africa to generate 15% of the SARS CoV-2 virus sequences that contributed to global variant detection and tracking. This is an example of the added value of world-class health technologies and capabilities in Africa for global health security.
In terms of expanding the research footprint while also giving professional agency independence and sustainability to partners, several TIBA partners were able to leverage their capital from the partnership to secure additional funding amounting a total of just under £12M. In-country buy-in led to in-kind support from local philanthropists, local government and pharma. For example, one of TIBA’s industry partners, Merck KgA, donated COVID-19 PPE to health workers in Zimbabwe through TIBA as part of their face mask donations programme.21 We are now applying for funding to expand TIBA’s research and translation network into other African countries with weaker research ecosystems and leverage on the strengths and expertise of the current nine partners to build a stronger regional research ecosystem,
Lessons learnt and recommendations
Throughout the 5 years of TIBA’s work, we learnt critical lessons on the attributes necessary for successful equitable global health research partnerships that generate sustained gains, buy-in, trust and impact. These lessons are valuable for both researchers and funders, and we have summarised them into 10 actionable recommendations in figure 4.
Figure 4.
Recommendations from lessons learnt. ODA, official development assistance.
Conclusions
A common approach in attempts to address the structural biases and challenges in internationally funded collaborative health research in Africa (highlighted in box 1) is to set targets addressing specified individual issues. Researchers and funders can be equally guilty of this, for example, prerequisite demands to address specific issues that might not apply in the local context or to local communities whether regarding age group or gender or even research questions. This approach often addresses symptoms but not causes of much deeper research cultural or operational challenges. Gains made in this way can be temporary and unsustainable.
TIBA was able to make a demonstrable impact directly on health and health research, knowledge ecosystem and community of practice in Africa because of the approach we took and the culture we fostered within the partnership as described in figure 1. We did not set targets for numbers of papers published, number of African or female lead authors, or reducing brain drain. These were all emergent products of our approach and way of working. When LMIC scientists have agency, focus and agenda-setting power to address their local health priorities, they thrive and solve their national development priorities. This in turn leads to buy-in and support from local governments/stakeholders and sustainability, as has happened to several TIBA programmes including national real-time SARS-CoV-2 sequencing and pathogen surveillance programmes in partner countries. We should be raising questions when, as is often the case, funding and partnerships for development research disproportionately progress the science and careers of researchers in the developed countries compared with the LMIC partners. TIBA’s approach demonstrated what equitable global health research looks like and what an Africa-led global health research partnership can achieve. In terms of our community of practice we share 10 actionable recommendations for researchers and funders (figure 4) based on the lessons we have learnt from TIBA’s work.
Acknowledgments
This manuscript has been prepared on behalf of the TIBA Partnership based on the work and contributions of the TIBA PIs, our teams of fellows and students, stakeholders, service providers (admin, communications, legal and MEL) and local grants and admin support teams. The authors thank the academic and support members of the TIBA for their work whose outputs are described here, our Monitoring, Evaluation & Learning (MEL) providers LTSI International who designed our Theory of Change Framework (figure 2), our communication team who designed our infographics including figure 4, our legal team Ingentium, our industry partners and our implementation and training partners: WHO AFRO, African Union’s AUDA-NEPAD and African Academy of Sciences. We are also grateful to all the health workers and people who participated in our research in the TIBA partner countries.
Footnotes
Handling editor: Seye Abimbola
Twitter: @PIG_Edinburgh, TibaPartnership, @TibaPartnership, @TibaPartnership
Contributors: FM, GB and MW were involved in conceptualisation. FM, GB and MW prepared the draft manuscript and all authors were involved in review and editing of the manuscript. All authors read and approved the final manuscript.
Funding: The work and research reported here was commissioned in part, by the National Institute for Health Research (NIHR) Global Health Research Program (16/136/33) using UK AID from the UK Government. FM is funded by a Royal Society Grant ICA\R1\201399 and UKRI ODA Impact and Development Grant to UoE.
Disclaimer: The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. All data and metrics referred to in this manuscript are available on our webpage on: https://tiba-partnership.org/.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . Child health. 2022. Available: www.afro.who.int/health-topics/child-health
- 2.Mutapi F. Africa needs to speed up research excellence: here’s how. The Conversation; 2021. [Google Scholar]
- 3.Munung NS, Mayosi BM, de Vries J. Equity in international health research collaborations in africa: perceptions and expectations of african researchers. PLoS One 2017;12:e0186237. 10.1371/journal.pone.0186237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UK Collaborative on Development Research . Research capacity strengthening: lessons from UK-funded initiatives in low- and middle-income countries; 2022.
- 5.Voller S, Chitalu C-CM, Nyondo-Mipando AL, et al. “We should be at the table together from the beginning”: perspectives on partnership from stakeholders at four research institutions in sub-saharan africa. Int J Equity Health 2022;21:111. 10.1186/s12939-022-01707-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tackling Infections to Benefit Africa (TIBA). 2023. Available: tiba-partnership.org [DOI] [PMC free article] [PubMed]
- 7.Mindu T, Kabuyaya M, Chimbari MJ, et al. Edutainment and infographics for schistosomiasis health education in ndumo area, KwaZulu-Natal, South Africa. Cogent Med 2020;7. 10.1080/2331205X.2020.1794272 [DOI] [Google Scholar]
- 8.NTDs UtC . Film launched on bilharzia, WASH and the impact on women and children. 2022. Available: https://unitingtocombatntds.org/news/film-launched-on-bilharzia-wash-and-the-impact-on-women-and-children/
- 9.Mutapi F. Africa should set its own health-research agenda. Nature 2019;575:567–67. 10.1038/d41586-019-03627-9 [DOI] [PubMed] [Google Scholar]
- 10.Whitworth JAG, Kokwaro G, Kinyanjui S, et al. Strengthening capacity for health research in Africa. Lancet 2008;372:1590–3. 10.1016/S0140-6736(08)61660-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Musesengwa R, Chimbari MJ. Community engagement practices in southern africa: review and thematic synthesis of studies done in botswana, zimbabwe and south africa. Acta Trop 2017;175:20–30. 10.1016/j.actatropica.2016.03.021 [DOI] [PubMed] [Google Scholar]
- 12.Seven principles for strengthening research capacity in low- and middle-income countries: simple ideas in a complex world. 2022. Available: https://www.gov.uk/research-for-development-outputs/seven-principles-for-strengthening-research-capacity-in-low-and-middle-income-countries-simple-ideas-in-a-complex-world
- 13.Botswana Institite for Technology Research and Innovation. 2020. Available: www.bitri.co.bw/bitri-nhl-collaboration/
- 14.Nyamwaya DK, Otiende M, Omuoyo DO, et al. Endemic chikungunya fever in Kenyan children: a prospective cohort study. BMC Infect Dis 2021;21:186. 10.1186/s12879-021-05875-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stein F, Perry M, Banda G, et al. Oxygen provision to fight COVID-19 in sub-Saharan Africa. BMJ Glob Health 2020;5:e002786. 10.1136/bmjgh-2020-002786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hedt-Gauthier BL, Jeufack HM, Neufeld NH, et al. Stuck in the middle: a systematic review of authorship in collaborative health research in Africa, 2014-2016. BMJ Glob Health 2019;4:e001853. 10.1136/bmjgh-2019-001853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rusakaniko S, Sibanda EN, Mduluza T, et al. SARS-cov-2 serological testing in frontline health workers in Zimbabwe. PLoS Negl Trop Dis 2021;15:e0009254. 10.1371/journal.pntd.0009254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Banda G, Mugwagwa J, Wanjala C, et al. Local manufacturing, local supply chains and health security in Africa: lessons from COVID-19. BMJ Glob Health 2021;6:e006362. 10.1136/bmjgh-2021-006362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . AFR-RC72-3 annual report of the regional director on the work of WHO in the african region. 2022. Available: www.afro.who.int/about-us/governance/sessions/seventy-second-session-who-regional-committee-africa
- 20.Google . Africaa developer ecosystem report 2021. 2022. Available: explode.africa/google-launches-africa-developer-ecosystem-report-2021/
- 21.Merck KGaA . Merck donates two million FFP2 masks. 2020. Available: www.merckgroup.com/en/news/masks-donation-12-05-2020.html
- 22.Nordling L. African researchers confirm inequities in global health research. Research Professional News; 2019. [Google Scholar]
- 23.Mbaye R, Gebeyehu R, Hossmann S, et al. Who is telling the story? A systematic review of authorship for infectious disease research conducted in Africa, 1980-2016. BMJ Glob Health 2019;4:e001855. 10.1136/bmjgh-2019-001855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Newton Fund: final evaluation report. Department for Science, Innovation and Technology & Department for Business, Energy & Industrial Strategy; 2022. [Google Scholar]
- 25.Loewenson R, Laurell AC, Hogstedt C, et al. Participatory action research in health systems: a methods reader. World Health Organization; 2014. [Google Scholar]
- 26.Izugbara CO, Kabiru CW, Amendah D, et al. “ It takes more than a fellowship program”: reflections on capacity strengthening for health systems research in sub-saharan africa. BMC Health Serv Res 2017;17:696. 10.1186/s12913-017-2638-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. All data and metrics referred to in this manuscript are available on our webpage on: https://tiba-partnership.org/.




