Abstract
Background
Vaccination plays an imperative role in protecting public health and preventing avoidable mortality. Yet, the reasons for vaccine hesitancy in African countries are not well understood. This study investigates the factors associated with the acceptance of COVID-19 vaccine in Mozambique, with a focus on the role of institutional trust.
Methods
The data came from the three waves of the COVID-19 Knowledge, Attitudes and Practices (KAP) survey which followed a cohort of 1,371 adults in Mozambique over six months (N = 3809). We examined vaccine acceptance based on three measurements: willingness to take vaccine, perceived vaccine efficacy, and perceived vaccine safety. We conducted multilevel regression analysis to investigate the trajectories of, and the association between institutional trust and vaccine acceptance.
Results
One third of the survey participants (37%) would definitely take the vaccine. Meanwhile, 31% believed the vaccine would prevent the COVID-19 infection, and 27% believed the vaccine would be safe. There was a significant decrease in COVID-19 vaccine acceptance between waves 1 and 3 of the survey. Institutional trust was consistently and strongly correlated with different measures of vaccine acceptance. There was a greater decline in vaccine acceptance in people with lower institutional trust. The positive correlation between institutional trust and vaccine acceptance was stronger in younger than older adults. Vaccine acceptance also varied by gender and marital status.
Conclusions
Vaccine acceptance can be volatile even over short periods of time. Institutional trust is a central driver of vaccine acceptance and contributes to the resilience of the health system. Our study highlights the importance of health communication and building a trustful relationship between the general public and the institutions in the context of a global pandemic.
Keywords: Vaccine acceptance, COVID-19 vaccine, Institutional trust, Mozambique
1. Introduction
The speed with which vaccines have been developed, trialed, and approved during the global COVID-19 pandemic has demonstrated the global health community’s capacity to act quickly to contain the spread of SARS-CoV-2. Despite safe and effective vaccines becoming increasingly available [1], [2] their acceptance and uptake in some populations have been lower than expected, with vaccine hesitancy recognized as a key barrier to uptake [3]. Given the important role of vaccination in protecting public health, it is crucial to better understand the factors that may lead to vaccine acceptance or hesitancy. This is especially the case in the Global South, where evidence about COVID-19 vaccine acceptance in the population has to-date been limited.
Vaccine hesitancy, often referred to as the delay in or refusal of vaccine acceptance [4], has been identified by the WHO as one of the top 10 threats to world health [5]. Multiple factors have been associated with increased vaccine hesitancy, including the proliferation of misinformation on social media [6], a lack of trust in public health institutions (in one French study) [7], mistrust in biomedicine (in Italy) [8], and sociodemographic differences (in the UK) [9]. While the majority of research to date has been focused on the Global North, recent work in Mozambique suggests COVID-19 vaccine hesitancy was lower among health workers than others surveyed (86.6% and 64.9% saying they would take the vaccine, respectively) in one cross-sectional online survey [10]. Evidence from other contexts has suggested that institutional trust is a key component of health service utilization [11]. Building public trust in multisectoral actors through health communication, therefore, presents a potentially fruitful way to increase service utilization, including vaccine acceptance and uptake, which can lead to a more resilient health system [12].
According to the Mozambican national vaccination plan, the introduction of a safe and effective vaccine represents a national priority to alleviate the negative impact of the COVID-19 pandemic on the health and socioeconomic system [10], [13]. The aim of the national COVID-19 vaccination communication campaigns has been to disseminate prevention measures through traditional and new media including radio, television, newspapers, SMS, WhatsApp, and Facebook. The communication plan focuses on providing fast and up-to-date information on vaccination and explains, whenever possible, the process associated with the campaign, including vaccination sites, target groups, the safety and efficacy of vaccines, associated risks, and adverse reactions.
Against this backdrop, this paper investigates how vaccine acceptance or hesitancy has changed over six months in Mozambique using three waves of longitudinal survey data. The study also examines the factors associated with that change, with a focus on the role of institutional trust in driving vaccine acceptance.
2. Methods
2.1. Data and sample
A cohort of 1,371 respondents was recruited for this study to complete an initial structured phone interview. Follow-up bi-monthly panel surveys were conducted for six months between September 2020 and March 2021 (three rounds in total). When the first two rounds of the follow-up surveys were taking place, the positivity index of COVID-19 in Mozambique was around 2%-3%. The fatality rate was 0.7%, lower than the global and African rates. Both positivity index and fatality rate increased when the third round of the survey took place (January – March 2021). The COVID-19 vaccination started in the first quarter of 2021. Mozambique intended to vaccinate everyone aged 15 years old and over. Children under the age of 15 and pregnant women were excluded.
The sample size of 1371 respondents was powered to detect a generic change of 10% from a baseline proportion of 50% for each of the three regions of Mozambique (i.e., Northern, Central, and Southern Regions). The target sample size was estimated to result in 390 participants per region by the final wave, assuming a 10% loss to follow-up between the first and second wave, and then a 5% loss thereafter. Attrition from the cohort occurred if the participant was not contactable, unavailable for interview, or if they did not re-consent to participate in a given round of data collection. The total sample size across the three rounds was 3809. Detailed information about the sample size and other characteristics for the three waves of data can be found in the supplemental materials.
Interviews lasted between 20 and 30 min, collecting information on COVID-19 prevention behaviors and barriers, knowledge of COVID-19 symptoms, care-seeking, vaccine acceptance, and demographic data. Data collection was through a structured questionnaire using CATI (Computer Assisted Telephone Interview). The cohort included those with phone access who were able to complete the survey via telephone interviews. The cohort were recruited from a sample of participants of a COVID-19 Knowledge, Attitudes and Practices (KAP) baseline survey in Mozambique who consented to be contacted for future research (approximately 97% of baseline participants consented to be re-contacted). The panel sample was stratified by gender and province of residence to achieve approximately equal numbers of male and female respondents, and even geographical coverage across all provinces of the country.
2.2. Key variables of interest
Vaccine acceptance is a multi-faceted concept. The questionnaire asked three questions about vaccine acceptance, constituting the outcome variables for the present analysis. These questions have been frequently used in previous studies and capture different domains of vaccine acceptance or hesitancy [4]. The first related to the willingness to receive the vaccine: “If a vaccine to prevent COVID-19 were available today, would you get it?” with response options: “definitely get it”, “probably get it”, “probably not”, and “I do not know”. We created a binary variable: 1 = definitely get it and 0 = other responses. This question captures the general acceptance. Second, perceived vaccine efficacy was captured with the question: “what is your level of concern that a COVID-19 vaccine does not prevent the disease?”, with response options: “very worried”, “worried”, “not worried”, and “I believe the vaccine would prevent the disease”. We created a binary variable: 0 = (very) worried and 1 = not worried or believing in the vaccine. The third question, concerning perceived vaccine safety, asked: “how worried are you that a COVID-19 vaccine is not safe?”, with response options: “very worried”, “worried, “not worried”, and “I believe the vaccine is safe”. We created a binary variable: 0 = (very) worried and 1 = not worried or believing in the vaccine’s safety. Since the three domains (i.e., general acceptance, perceived efficacy, and perceived safety) belong to the same measurement, we also created a summary measure by adding together these three binary variables (range: 0–3). Doing so also allowed us to investigate vaccine acceptance from a holistic perspective and appraise the extent to which the analyses results were robust to different specifications of the outcome variables.
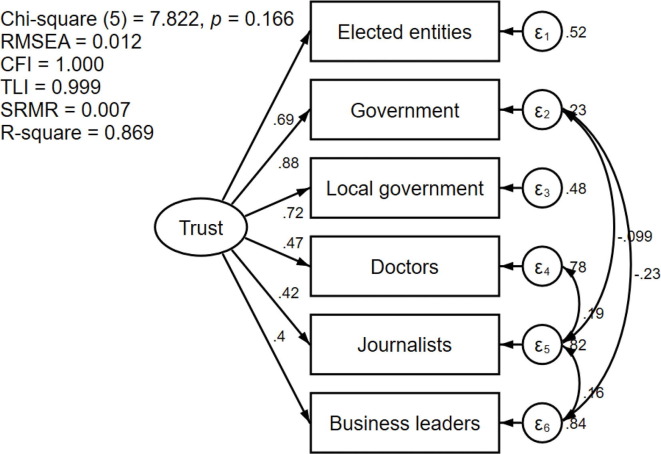
The key independent variable of interest is institutional trust. The questionnaire included a six-item institutional trust battery, based on the WHO’s COVID-19 Global Risk Communication and Community Engagement Strategy guidance [13]. Respondents were asked how much confidence they had in elected entities, government, local government (municipality), doctors, journalists, and business leaders to act in the public interest, with Likert-type response options: “no confidence”, “little confidence”, “some confidence”, and “a lot of confidence”, coded from 1 to 4. The Cronbach alpha of the six items is 0.77, indicating good internal consistency.
2.3. Control variables
We investigated a range of control variables, based on existing literature, that might confound the relationship between vaccine acceptance and institutional trust. Demographic factors included age, gender, and marital status. Age is a continuous variable. Marital status is a dichotomized variable: 0 = single/other (including never married, widowed, separated, or divorced) and 1 = currently married. Socioeconomic factors included education, employment, and the national wealth score (estimated and equivalized using the Equity Tool) [14]. A higher score indicates a higher level of wealth. We used a three-category education variable (primary or below, secondary, tertiary) while employment was dichotomized into 0 = unemployed and 1 = employed. A binary rural–urban residence variable was also analyzed.
2.4. Statistical analysis
We first conducted confirmatory factor analysis (CFA) to construct a latent score of institutional trust. The model specification was guided by model fit. We conducted the χ2 test, calculated the coefficient of determination (R2), and evaluated four fit indices including Root Mean Square Error of Approximation (RMSEA), Bentler Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and Standardized Root Mean Square Residual (SRMR). We calculated the predicted institutional trust score from the model with the best fit and normalized it to a scale ranging from 0 (no trust) to 100 (complete trust). The predicted score was included as an independent variable to predict vaccine acceptance.
The vaccine acceptance questions were asked in the three follow-up waves of the survey (namely waves 1–3). However, institutional trust questions were asked in the baseline, wave one and wave three of the survey. To make full use of the information available, using CFA we calculated the institutional trust score of the baseline, wave one and wave three surveys, and treated the mean score of the other three waves as a proxy for the trust score for wave two.
For the three binary acceptance variables, we built multilevel logistic regression models with random intercept (i.e., panel data random effects models) which account for individual-level heterogeneity. The overall acceptance variable is a count variable, so we built multilevel Poisson regression models with random intercept. We conducted likelihood ratio tests and calculated the intra-class correlation to evaluate the usefulness of a multilevel model.
To take full advantage of the longitudinal nature of the dataset, we included time dummy variables in the regression models and mapped out the trajectories of vaccine acceptance over time. We further investigated whether the slopes of trajectories vary according to institutional trust. This involves including an interaction term between the time dummies and institutional trust in the analyses. Taking a life course perspective, previous studies suggest that the determinants of health behaviour vary markedly across different life stages [15]. Profound changes in attitude and values towards health behaviour and social institutions may take place with the accumulation of life experiences [16]. Therefore, we also included an interaction term between age and institutional trust in the regression models to understand the heterogeneity in the relationships between institutional trust and vaccine acceptance across different age groups in the population.
Ethical approval
Our study was based on secondary analyses of data collected in the COVID-19 KAP survey. This survey was determined to be human subjects research and received IRB approval from the Mozambique Comité Nacional de Bioética para Saúde (CNBS) (reference: 439/CNBS/20). All participants gave their informed consent to participate in the study.
3. Results
The sample size in wave 1 was 1,327, falling to 1185 by wave 3. The average age of the sample was 32 years old. Men accounted for 61% of the sample, and over half (54%) of the sample were married. The mean value of the equivalized wealth score was 1.3. The minimum and maximum values were −0.4 and 1.6, respectively. A majority of the participants of the survey received secondary (66%) or tertiary education (29%). Around 30% were unemployed, and 81% were living in urban areas (Table 1 ).
Table 1.
Sample characteristics (N = 3809).
| Wave 1 |
Wave 2 |
Wave 3 |
Waves 1–3 |
|
|---|---|---|---|---|
| Proportions or means | ||||
| Definitely Take vaccine | ||||
| No | 63% | 56% | 71% | 63% |
| Yes | 37% | 44% | 29% | 37% |
| Vaccine efficacy | ||||
| Worried | 67% | 67% | 72% | 69% |
| Not worried | 33% | 33% | 28% | 31% |
| Vaccine safety | ||||
| Worried | 73% | 70% | 77% | 73% |
| Not worried | 27% | 30% | 23% | 27% |
| Vaccine acceptance (Range: 0–3) | 0.96 | 1.07 | 0.79 | 0.95 |
| Institutional trust score | 72.5 | 73.5 | 75.4 | 73.7 |
| Age | 32.3 | 32.3 | 32.5 | 32.3 |
| Gender | ||||
| Female | 41% | 39% | 38% | 39% |
| Male | 59% | 61% | 62% | 61% |
| Marital status | ||||
| Single | 47% | 48% | 43% | 46% |
| Married | 53% | 52% | 57% | 54% |
| Wealth score (Range: −0.42–1.64) | 1.32 | 1.32 | 1.32 | 1.32 |
| Education | ||||
| Primary education | 6% | 6% | 6% | 6% |
| Secondary education | 66% | 66% | 65% | 66% |
| Tertiary education | 28% | 28% | 29% | 29% |
| Employment | ||||
| Unemployed | 31% | 25% | 30% | 29% |
| Employed | 69% | 75% | 70% | 71% |
| Rural/urban residence | ||||
| Rural areas | 19% | 19% | 20% | 19% |
| Urban areas | 81% | 81% | 80% | 81% |
| N | 1327 | 1253 | 1185 | 3809 |
The results of the confirmatory factor analysis show that all six items in the institutional trust battery loaded significantly (p < 0.001) and positively on a single-dimensional construct (Fig. 1 ). Factor loadings for confidence in the government, local governments, and elected entities were higher than those for doctors, journalists, and business leaders. An increase of one standard deviation in institutional trust was associated with an increase of 0.88 standard deviations in confidence in the government, 0.72 standard deviations in confidence in local governments, and 0.69 standard deviations in confidence in elected entities. There were strong correlations between the residuals in relation to trust in governments, doctors, journalists, and business leaders. The post-estimation diagnostic tests show that the model has an excellent fit to the data. The χ2 test is not statistically significant, indicating little difference between the model-implied and sample covariance matrices. Both the RMSEA and SRMR are below the threshold of 0.05, and both the CFI and TLI are above the threshold of 0.95. The R2 statistic suggests that the six items explain 87% of the total variance of the latent construct.
Fig. 1.
Factor analysis of institutional trust.
There was a small increase in the mean institutional trust score between waves 1 and 3 (from 72.5 to 75.4, respectively) (Table 1). The individual variables of institutional trust demonstrated a similar trend (Table A2, supplementary materials). The percentage of respondents reporting they would definitely take the vaccine showed considerable variability over time, from 37% to 44% to 29% between waves 1, 2 and 3. There was an increase in concern about vaccine efficacy between waves 2 and 3: 33% reported that they were not worried about the efficacy of the vaccine in waves 1 and 2, decreasing to 28% in wave 3. Over-time variability was also seen in the percentage reporting they were not worried about the vaccine’s safety between waves 1, 2 and 3 (27%, 30%, and 23%, respectively). Similarly, the mean vaccine acceptance score increased from 1.0 in wave 1 to 1.1 in wave 2 before decreasing to 0.8 in wave 3.
The three dichotomized measures of vaccine acceptance were included as dependent variables in three separate regression models (Table 2 ). The institutional trust score was a statistically significant variable in all three models. A one-unit increase in the trust score was associated with an increase in the odds of: willingness to take the vaccine (1.7%; p < 0.001); perceived vaccine efficacy (0.7%; p < 0.01); and perceived vaccine safety (1.0%; p < 0.001), controlling for other variables. Respondents reported a significantly higher level of willingness to take the vaccine in wave 2 than in wave 1, and a significantly lower level of willingness to take the vaccine, perceived vaccine efficacy, and perceived vaccine safety in wave 3. Older age or being male was significantly associated with increased willingness to take the vaccine, and perceived vaccine safety. Perceived vaccine efficacy did not differ significantly by gender, age or marital status. People in urban areas had a lower level of willingness to take the vaccine. Both the likelihood ratio test and the intra-class correlation coefficients suggest that vaccine acceptance was correlated within participants over time, indicating that a multilevel modelling approach was appropriate.
Table 2.
Multilevel binary logistic regression analysis of vaccine acceptance (N = 3809).
| Taking vaccine (1 = Yes) |
Efficacy of vaccine (1 = Not worried) |
Safety of vaccine (1 = Not worried) |
|
|---|---|---|---|
| Trust score | 1.017*** (1.012–1.022) |
1.007** (1.002–1.011) |
1.010*** (1.005–1.015) |
| Wave 2 | 1.594*** (1.308–1.943) |
1.034 (0.857–1.247) |
1.226* (1.000–1.505) |
| Wave 3 | 0.545*** (0.443–0.670) |
0.736** (0.607–0.892) |
0.715** (0.578–0.886) |
| Age | 1.033*** (1.018–1.048) |
0.999 (0.987–1.011) |
1.023*** (1.009–1.037) |
| Male | 1.348* (1.053–1.727) |
0.928 (0.752–1.144) |
1.329* (1.038–1.703) |
| Married | 1.381** (1.094–1.744) |
0.842 (0.686–1.034) |
1.130 (0.893–1.43) |
| Wealth score | 0.920 (0.620–1.366) |
1.221 (0.866–1.721) |
0.754 (0.511–1.113) |
| Secondary education | 1.239 (0.718–2.139) |
1.045 (0.646–1.689) |
1.12 (0.653–1.923) |
| Tertiary education | 1.342 (0.763–2.359) |
1.102 (0.671–1.808) |
0.873 (0.498–1.53) |
| Employed | 0.884 (0.702–1.114) |
1.022 (0.832–1.256) |
0.949 (0.751–1.199) |
| Urban areas | 0.728* (0.547–0.968) |
1.009 (0.784–1.298) |
1.017 (0.763–1.356) |
| χ2 = 237*** | χ2 = 119*** | χ2 = 182*** | |
| 0.42 | 0.29 | 0.39 |
Notes: Figures outside and inside parenthesis are odds ratio and 95% confidence intervals, respectively; *p < 0.05, **p < 0.01, ***p < 0.001.
Table 3 shows the results of the multilevel Poisson regression models where the overall vaccine acceptance score (range: 0–3) was the dependent variable. The model without interaction terms (Column 2) shows that the results were largely consistent with the findings in Table 2. People with a higher institutional trust score, older people, and men had significantly greater vaccine acceptance. Acceptance increased significantly in wave 2 and then decreased significantly in wave 3.
Table 3.
Multilevel Poisson regression analysis of vaccine acceptance (N = 3809).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Trust score | 1.006*** (1.004–1.008) |
1.016*** (1.009–1.023) |
1.013*** (1.007–1.02) |
| Wave 2 | 1.115** (1.032–1.205) |
1.115** (1.032–1.205) |
0.955 (0.707–1.29) |
| Wave 3 | 0.804*** (0.739–0.874) |
0.805*** (0.74–0.876) |
0.491*** (0.356–0.677) |
| Age | 1.008*** (1.004–1.013) |
1.033*** (1.016–1.05) |
1.033*** (1.016–1.05) |
| Trust × Age | 0.9997** (0.9995–0.9999) |
0.9997** (0.9995–0.9999) |
|
| Trust × Wave 2 | 1.002 (0.998–1.006) |
||
| Trust × Wave 3 | 1.006** (1.002–1.01) |
||
| Male | 1.088* (1.001–1.184) |
1.084 (0.997–1.179) |
1.084 (0.997–1.178) |
| Married | 1.045 (0.962–1.135) |
1.033 (0.951–1.123) |
1.037 (0.954–1.127) |
| Wealth score | 0.979 (0.857–1.118) |
0.977 (0.856–1.115) |
0.976 (0.855–1.114) |
| Secondary education | 1.066 (0.887–1.28) |
1.036 (0.863–1.245) |
1.035 (0.861–1.243) |
| Tertiary education | 1.052 (0.87–1.272) |
1.021 (0.844–1.234) |
1.019 (0.843–1.232) |
| Employed | 0.971 (0.892–1.057) |
0.973 (0.894–1.06) |
0.973 (0.894–1.059) |
| Urban areas | 0.943 (0.855–1.04) |
0.944 (0.856–1.041) |
0.943 (0.855–1.04) |
Notes: Figures outside and inside parenthesis are incidence rate ratio and 95% confidence intervals, respectively; *p < 0.05, **p < 0.01, ***p < 0.001.
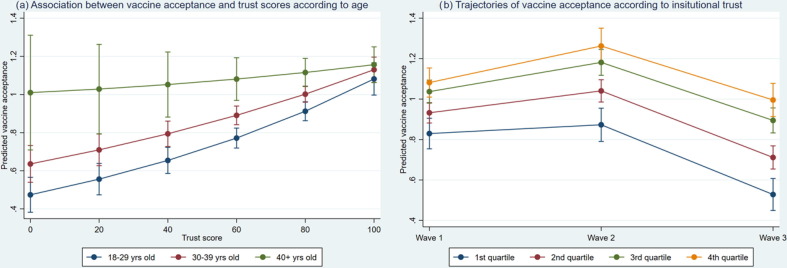
Regression results of model 2 show that age had a significant moderation effect (column 3 in Table 3). The incidence rate ratio (IRR) of the interaction term indicates that the positive correlation between vaccine acceptance and institutional trust was weakened among people in older age groups. Based on the marginal effects derived from the regression analyses, we estimated the predicted scores of vaccine acceptance. For people aged between 18 and 29 years, the predicted score of vaccine acceptance increased by 130%, from 0.47 to 1.08, as the institutional trust score rose from 0 to 100 (Fig. 2 a). This stands in contrast to the predicted acceptance score of people aged 40 and over which increased by 15%, from 1.01 to 1.16.
Fig. 2.
Association between vaccine acceptance and institutional trust.
Model 3 reports the results where an interaction term between institutional trust and time was included in the model (Column 4 in Table 3). Like in models 1 and 2, the IRR for wave 3 was significantly below 1, indicating a marked decrease in vaccine acceptance at that time point. The IRR for the interaction between trust and wave 3 was significant and above 1, which means that the decrease in vaccine acceptance from wave 1 to 3 was attenuated among people with high institutional trust. For people in the first quartile of trust scores (i.e., the lowest quartile), the predicted acceptance score reduced significantly from 0.83 (95% CI: 0.75–0.91) in wave 1 to 0.53 (95% CI: 0.45–0.61) in wave 3 (Fig. 2b). For people in the fourth quartile of trust scores (i.e., the highest quartile), the predicted acceptance score increased significantly from 1.08 (95% CI: 1.01–1.15) in wave 1 to 1.26 (95% CI: 1.17–1.35) in wave 2 before reducing to 1.00 (95% CI: 0.91–1.08) in wave 3. The difference in vaccine acceptance between waves 1 and 3 was not statistically significant in this group of people. People with varied levels of institutional trust followed different trajectories of vaccine acceptance over time. The large decrease in vaccine acceptance between waves 1 and 3 was mainly driven by people with low institutional trust.
4. Discussion
This study examined the relationship between institutional trust and COVID-19 vaccination acceptance in Mozambique. We have several new and compelling findings. First, we found that vaccination acceptance was volatile over the study period of six months. Acceptance increased from September to November 2020, but decreased by the final wave in January-February 2021. One possible explanation is that negative news regarding vaccination safety and efficacy was released by major local and international media around the time of the final data collection period. In addition, both the positivity rate and the fatality rate were on the rise during that period. Evidence from Japan, Portugal and the UK showed that perceived safety and efficacy were important considerations when people made a decision on vaccination [17], [18], [19]. The main reasons for receiving vaccinations are for people to protect themselves and others from COVID-19. However, negative media coverage may lead to uncertainties around vaccination safety and efficacy in the population, which makes people hesitant about taking the vaccination. In this case, it is important for the government and health authorities to engage the public with transparency and accountability, to prevent uncertainties from transforming into negative perceptions.
Based on an institutional trust score we constructed in the survey, we found that higher institutional trust was significantly associated with higher vaccine acceptance. People with a lower level of institutional trust were more likely to refuse vaccination or harbored a higher level of hesitancy in taking it. This finding is consistent with the broader literature on social and political determinants of vaccine acceptance. So far, most of the studies focusing on the association between institutional trust and vaccine acceptance were conducted in high-income countries. It is shown, for example, that trust in federal institutions [20], and trust in the government’s technical and organizational skill to handle a contagious outbreak along with confidence in medical institutions play a salient role in predicting willingness to be vaccinated against influenza in the United States [21]. Similar results have been seen in the UK [22] and Portugal [18], linking positive attitudes towards vaccination with a high level of trust in the National Health Service and the government. Our study is among the first to show that such a strong association can also be observed in African countries. In addition to contributing to this literature for the Global South, our study uses longitudinal data, which shows that people with a high level of trust are less susceptible to a decline in vaccine acceptance over time.
Mozambique has invested considerable efforts toward reliable sources of information, aiming to overcome misinformation and bias against vaccination programs. This approach has involved key figures in the ministry of health, public health and research institutions addressing the public on a daily basis. Scientific virtual conferences on the COVID-19 pandemic have included vaccines and were implemented with renowned and trusted persons taking a prominent role. Scientific conferences and media appearances were broadcast both on radio and television. These informational and communication efforts to build trust in the general population seem well-placed in light of our findings linking greater institutional trust with increased vaccine acceptance. During an active pandemic, these examples in Mozambique represent strong cross-institutional collaboration across government, media, academics, and public health practitioners. We recommend that the Ministry of Health and their partners continue to cultivate such collaboration before, during, and after emerging pandemic threats to ensure robust health system responses that routinely nurture or instill trust, which we found to be highly variable.
On the basis of our findings, it seems reasonable to argue that the public’s trust in institutions can contribute to more resilience in the public health system in terms of vaccine uptake and health service utilization in the context of a global pandemic. In the long run, the government may also want to devote more attention to institution-level reforms. This requires the government to go beyond promoting dialogues within the health system and rethink the governance models of the country.
We found that some demographic factors predicted vaccine acceptance. This is consistent with another study based on an online health worker survey on vaccination acceptance in Mozambique which found that vaccination acceptance was positively and significantly associated with age [10], although existing studies examining gender differences in vaccine acceptance have reported mixed results [10], [18]. Inequities in vaccination acceptance (and thus likely uptake) reflect the need for a greater exploration of its drivers and for interventions to address potential inequalities to allow for more equitable uptake of vaccinations in future. Targeted campaigns to promote vaccination acceptance among those groups with low levels of trust are needed.
Our results have to be interpreted in light of the study limitations. First, vaccine acceptance or hesitancy is a multi-dimensional construct. In this study, we have focused on three important dimensions of this concept according to the existing literature: general acceptance of vaccination, perceived efficacy, and perceived safety [4]. However, due to the unavailability of data in the COVID-19 KAP survey, we have not been able to capture two other dimensions of the concept including complacency and convenience [4]. Future research concerning the acceptance of the COVID-19 vaccine could benefit from expanding investigations into those domains. Second, the data were collected remotely through telephone interviews. This means that our sample consisted solely of people with access to a cell phone, who are also likely to have greater access to health care. These people represent a subset of the target population, and the sample is likely to be biased towards urban, wealthier respondents. Our recruitment strategy achieved a high response rate, but our sample was not representative of the general population so any generalization should be made with caution. Finally, the English version of the question relating to perceived efficacy used ‘infection’. However, the word ‘disease’ was used when that question was translated into Portuguese and asked of respondents in Mozambique. This translation issue may have caused confusion for some respondents.
5. Conclusion
Our study underscores the central role of health communication and trust-building in promoting vaccine acceptance to protect public health. Although personal characteristics such as gender, age, and marital status have an influence on vaccine uptake, the effects of broader structural factors, including trust in institutions, should not be ignored. Simply making vaccines available is not sufficient to ensure access and uptake. Building a resilient health system requires proactive engagement with the public, building and maintaining a trusting relationship between healthcare users and institutions. There is considerable variability in societal attitudes towards vaccine programs, even over short periods of time. Finding ways to build and capitalize on trust in institutions, particularly among those less likely to vaccinate, could prove successful in increasing vaccine acceptance in many contexts, and help underpin the resilience of the health system.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to acknowledge the generosity of the study participants in sharing their time and information with us, often repeatedly over many months. We would also like to thank the field staff working tirelessly during a pandemic to call participants and gather these data.
Patient and public involvement
This study did not collect data from patients specifically. Patients and the public were not involved in the study. However, de-identified data is available to the public on request.
Funding
We are grateful for the support of the Embassy of the Kingdom of the Netherlands, Mozambique to PSI/Mozambique that made this project possible.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2023.03.053.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Data availability
The data consist of deidentified participant data, and are available upon reasonable request from the corresponding author, subject to PSI’s data use policy.
References
- 1.Bok K., Sitar S., Graham B.S., Mascola J.R. Accelerated COVID-19 vaccine development: milestones, lessons, and prospects. Immunity. 2021;54(8):1636–1651. doi: 10.1016/j.immuni.2021.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mellet J., Pepper M.S. A COVID-19 vaccine: big strides come with big challenges. Vaccines (Basel) 2021;9(1):39. doi: 10.3390/vaccines9010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Machingaidze S., Wiysonge C.S. Understanding COVID-19 vaccine hesitancy. Nat Med. 2021;27(8):1338–1339. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- 4.Quinn S.C., Jamison A.M., An J., Hancock G.R., Freimuth V.S. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine. 2019 Feb 21;37(9):1168–1173. doi: 10.1016/j.vaccine.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. 10 global health issues to track in 2021 [Internet]. [cited 2022 Jan 27]. <https://www.who.int/news-room/spotlight/10-global-health-issues-to-track-in-2021>.
- 6.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raude J., Fressard L., Gautier A., Pulcini C., Peretti-Watel P., Verger P. Opening the ‘Vaccine Hesitancy’ black box: how trust in institutions affects French GPs’ vaccination practices. Expert Rev Vaccines. 2016;15(7):937–948. doi: 10.1080/14760584.2016.1184092. [DOI] [PubMed] [Google Scholar]
- 8.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study – ScienceDirect. Brain, Behavior, and Immunity. 94(1):41–50. [DOI] [PMC free article] [PubMed]
- 10.Dula J., Mulhanga A., Nhanombe A., Cumbi L., Júnior A., Gwatsvaira J., et al. COVID-19 vaccine acceptability and its determinants in mozambique: an online survey. Vaccines. 2021;9(8):828. doi: 10.3390/vaccines9080828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Østergaard L.R. Trust matters: a narrative literature review of the role of trust in health care systems in sub-Saharan Africa. Glob Public Health. 2015 Oct;10(9):1046–1059. doi: 10.1080/17441692.2015.1019538. [DOI] [PubMed] [Google Scholar]
- 12.Kittelsen S.K., Keating V.C. Rational trust in resilient health systems. Health Policy Plan. 2019 Sep 1;34(7):553–557. doi: 10.1093/heapol/czz066. [DOI] [PubMed] [Google Scholar]
- 13.COVID-19 Global Risk Communication and Community Engagement Strategy – interim guidance [Internet]. [cited 2021 Dec 3]. <https://www.who.int/publications-detail-redirect/covid-19-global-risk-communication-and-community-engagement-strategy>.
- 14.Equity Tool Metrics. Equity Tool for Mozambique [Internet]. Equity Tool. [cited 2021 Dec 3]. <https://www.equitytool.org/mozambique/>.
- 15.Umberson D., Liu H., Reczek C. Stress and health behaviour over the life course. Adv Life Course Res. 2008;1(13):19–44. [Google Scholar]
- 16.Konty M.A., Dunham C.C. Differences in value and attitude change over the life course. Soc Spectr. 1997;17(2):177–197. [Google Scholar]
- 17.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020 Nov 17;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R., et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021 Mar;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Machida M., Nakamura I., Kojima T., Saito R., Nakaya T., Hanibuchi T., et al. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines. 2021;9(3):210. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jamison A.M., Quinn S.C., Freimuth V.S. “You don’t trust a government vaccine”: narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med. 2019;1(221):87–94. doi: 10.1016/j.socscimed.2018.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mesch G.S., Schwirian K.P. Social and political determinants of vaccine hesitancy: lessons learned from the H1N1 pandemic of 2009–2010. Am J Infect Control. 2015;43(11):1161–1165. doi: 10.1016/j.ajic.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sethi S., Kumar A., Mandal A., Shaikh M., Hall C.A., Kirk J.M.W., et al. The UPTAKE study: a cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. BMJ Open. 2021;11(6):e048856. doi: 10.1136/bmjopen-2021-048856. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data consist of deidentified participant data, and are available upon reasonable request from the corresponding author, subject to PSI’s data use policy.