Abstract
Osteoarticular tuberculosis (OAT) is defined by the set of pathological manifestations secondary to the attacks of osteoarticular structures of the locomotor system by the Bacillus of Koch (BK). We report a case of tuberculosis of the navicular bone, which is a rare location of OAT, on a female patient who consulted for chronic pain (mixed appearance) evolving for more than 7 years and for whom we realized a radiological assessment based on standard radiography and magnetic resonance imaging and a biological assessment. The foot is rarely involved, accounting for about 10% of cases of osteoarticular tuberculosis. The diagnosis is often made at a late stage because osteoarticular tuberculosis is paucibacillary, and it is difficult to isolate or culture Koch's bacillus. Clinical manifestations are aspecific; pain and joint swelling are the 2 usual signs. Pain may be mechanical, inflammatory, or mixed. The standard radiography allows first to orient the diagnosis by the demonstration of a lytic process; a biological inflammatory syndrome and the magnetic resonance imaging allow to give more arguments in favor, then the biopsy comes to confirm the diagnosis. Tuberculosis of the navicular bone is a rare localization of OAT; its diagnosis is the same as well as the treatment.
Keywords: Osteoarticular tuberculosis; Mid-foot; Antibacterial treatment, MRI bone
Introduction
Tuberculosis is a contagious infectious disease due to the pathogenic effects of a mycobacterium of the tuberculosis complex (mainly Mycobacterium tuberculosis hominis, also called Koch's bacillus).
Osteoarticular tuberculosis is defined by the set of pathologic manifestations secondary to the attacks of osteoarticular structures of the locomotor system by the bacillus of Koch. It is classically divided into 4 main types: spinal involvement, tuberculous arthritis or osteoarthritis, osteitis or osteomyelitis, and tenosynovitis and bursitis [1].
It represents 3%-5% of all tuberculosis; about 15% of extra-pulmonary tuberculosis can affect all bone segments of the body. It predominates in the spine and weight-bearing joints [2].
This condition is considered serious because of the functional prognosis which is often threatened by bone destruction and deformity. It has a favorable evolution if diagnosed early. Its diagnosis is sometimes difficult, based on a number of arguments. However, surgical biopsy remains the examination of choice in case of diagnostic difficulty.
The treatment consists of an antibacillary treatment associated with an orthopedic and/or surgical treatment.
Observation
Our patient aged 50 years old, operated 1 year before her admission for uterine fibroma by laparoscopy. The patient not known to be diabetic or being followed for an autoimmune disease without any notion of taking corticoids or immunosuppressants.
The history of her disease goes back 7 years with the installation of chronic pain of the ankle, mechanical aspect, calmed by analgesics, with notion of recurrent sprains treated medically. The evolution was marked by the aggravation of the pain becoming mixed and resistant to analgesic treatment with limping when walking.
On clinical examination, the patient was limping and we do not find a deformity of the foot or forefoot. Palpation was painful over the navicular bone and the entire midfoot joint. The patient does not present clinical signs suggestive of a secondary localization, notably pulmonary, urogenital-genital, or intestinal.
The foot X-ray showed a lytic process at the level of the navicular bone with rupture of the cortical, and the biological assessment revealed an inflammatory syndrome (Fig. 1); a hyperleukocytosis with neutrophils at 15,080 elements/mm3, high sedimentation rate at 24 mm while the CRP was normal at 5 mg/L. In view of these clinical, biological, and radiological arguments, we completed magnetic resonance imaging (MRI) in order to have a more precise assessment and to look for the extension toward the soft parts. It shows several trabecular lytic images eroding the bone cortical surfaces of the joints communicating with the talo-navicular and ulnar-navicular joints and the upper bone cortical. These lytic images are T1 isosignal, T2 hypersignal, enhancing peripherally after contrast. We noticed a synovial thickening of the transverse tarsal joint (Chopart's joint) and of the cuneo navicular joint, in DP fat-sat hypersignal, intensely enhancing after gadolinium injection, measuring approximately 7 mm, associated with an infiltrated aspect of the dorsal talonavicular and cuneonavicular ligament with erosion of the calcaneal entheses and of the intermediate and medial cuneiform, this infiltration also involves the interosseous taloculcaneal ligaments with an infiltrated aspect of the tarsal sinus. In addition, there was joint involvement of the medial part of the subtalar joint and the tarsometatarsal joint of the second ray, with condensation of the subchondral bone (on the calcaneal, cuneiform, and metatarsal sides) in T1 hyposignal, T2 hypersignal, also containing lytic and erosive images (Fig. 2).
Fig. 1.
Standard radiograph of the foot. (A) Lateral, (B) AP showing a lytic process of the navicular bone with rupture of the cortical bone clearly visible on the lateral view (arrow).
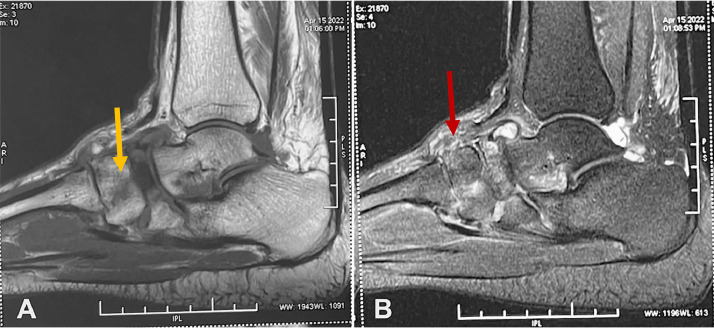
Fig. 2.
MRI of the foot, sagittal section performed for our patient. (A) T1 sagittal showing the collapse of the navicular bone with bone signal aberration in T1 hyposignal “yellow arrow.” (B) Sagittal DPFs (pronton density fat saturation) showing the synovial thickening of the tarsal joint in DPFs hypersignal “red arrow.”.
A surgical biopsy was performed, and the anatomo-pathological study of the bone tissue showed a polymorphic inflammatory granuloma, rich in neutrophils, with epithelioid and gigantocellular nodules with caseous necrosis. The diagnosis of tuberculous osteoarthritis was retained, and an antibacillary treatment was started with isoniazid, rifampicin, ethambutol, and pyrazinamide for 2 months, followed by a dual therapy (isoniazid and rifampicin) for 10 months.
Discussion
Osteoarticular tuberculosis accounts for 2%-5% of all tuberculosis and 11%-15% of extrapulmonary tuberculosis, second only to urogenital, lymph node, and pleural localizations [[3], [4]].
The spine and hip are the most frequently affected sites. The foot is rarely involved, accounting for about 10% of cases of osteoarticular tuberculosis [[5], [6]].
The diagnosis is often made at a late stage because osteoarticular tuberculosis is paucibacillary, and it is difficult to isolate or culture Koch's bacillus. Usually, clinical data, radiological images, elevated sedimentation rate are sufficient to make the diagnosis of tuberculosis and initiate treatment [7].
All foot joints can be affected and all associations are possible. Medioped and Lisfranc joints are predominantly affected, and are often very destructive, as the medioped joints communicate with each other, with the Lisfranc joint, and also with the subtalar joint. The osteoarthritis is therefore often extensive and results in significant osteolysis or radiological demineralization [8].
Clinical manifestations are aspecific; pain and joint gonflement are the 2 usual signs. Pain may be mechanical, inflammatory, or mixed. Gonflement may be due to joint effusion. Functional impotence is common [9]. Systemic manifestations such as fever, nocturnal sweating, and weight loss are rare [10].
Blood tests have little diagnostic value. An increased sedimentation rate (ESR) between 25 and 100 mm 1 h-1 is present in the vast majority of cases; nevertheless, the ESR may be normal [[3], [4], [5], [6], [7], [8], [9]]. An inflammatory anemia is possible. Relative lymphocytosis actually appears to be uncommon [3].
Standard radiography remains the first-line imaging. The radiographic stage varies according to the stage at which the diagnosis is made. Indeed, the signs appear progressively [11]. In the early stage, the radiograph is normal or shows only a bony hypertransparency of the epiphyses and an increase in volume of the soft tissues. Then osteolytic damage appears with geodes or erosions, poorly limited, perichondral, or subchondral in nature. The appearance of pinching of the joint space, a sign of cartilage destruction, is late. Destructive damage progresses with the appearance of joint deformity. The presence of “drop” calcifications within the abscess is suggestive of the tubercular nature [12].
Martini [6] proposed a radiological classification into 4 progressive stages, a classification inspired by that of David Chausse.
MRI is the best imaging test for the diagnosis and follow-up of tuberculous osteoarthritis [13]. It can show synovial pannus, joint effusion, cartilage destruction, bone erosions, bone fragments, periarticular abscesses, periarticular inflammation, and bone edema. MRI, which is more sensitive than radiography, demonstrates bone erosions in 70% of cases. These erosions, which may be central or peripheral, are hyposignal in T1 and T2, but their signal is enhanced after injection of gadolinium. Cartilage destruction is seen in 40% of cases and appears as localized or global thinning on MRI. The cartilage has an intermediate signal in T1 and T2, but is hypersignal on gradient echo sequences. The association of abscess and bone fragments is highly suggestive of the diagnosis of tuberculosis [14].
Histological evidence is essential in osteoarticular tuberculosis, and is considered a fundamental step in the diagnosis. The demonstration of an epithelioid and gigantocellular granuloma with caseous necrosis makes it possible, in the face of a suggestive clinical and radiological picture, to affirm the diagnosis of osteoarticular tuberculosis [[9], [10], [11], [12], [13], [14], [15]].
The treatment is essentially medical with antibacillary drugs, which allow to improve the clinical condition and to limit the evolution toward deformities [16]. The lesions heal in 6-12 weeks with medical treatment. Surgical treatment is indicated in case of failure of medical treatment, or in case of synovitis, fistula, or abscess. Arthrodesis surgery is used to correct sequelae and painful deformities [17,18].
Conclusion
Tuberculosis of the navicular bone is a rare localization of osteoarticular tuberculosis; its diagnosis is the same as well as the treatment.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Rafiki K, Yousri B, Arihi M, Bjitro C, Aboumaarouf M, El Andaloussi M. Unusual locations of osteoarticular tuberculosis in children: a report of 12 cases. Rev Chir Orthop Traumatol. 2013;99:297–303. doi: 10.1016/j.otsr.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Teklali Y, El Alami ZF, El Madhi T, Gourinda H, Miri A. La tuberculose ostéoarticulaire chez l'enfant (mal de Pott exclu): à propos de 106 cas. Rev Rhum. 2003;70:595–599. [Google Scholar]
- 3.Evanchick CC, Davis DE, Harrington TM. Tuberculosis of peripheral joints: an often missed diagnosis. J Rheumatol. 1986;13:187–189. [PubMed] [Google Scholar]
- 4.Monach PA, Daily JP, Rodriguez-Herrera G, Solomon DH. Tuberculous osteomyelitis presenting as shoulder pain. J Rheumatol. 2003;30:851–856. [PubMed] [Google Scholar]
- 5.Tuli SM. 2nd ed. Jaypee Brothers Medical Publishers (P) Ltd; New Delhi: 1991. Tuberculosis of the skeletal system; pp. 3–122. [Google Scholar]
- 6.Martini M, Adjrard A. In: Tuberculosis of the bones and joints. Martini M, editor. Springer Verlag; Berlin: 1988. Tuberculosis of the ankle and foot joint. etc. [Google Scholar]
- 7.Hg Watts, Lifeso RM. Current concepts review: tuberculosis of bones and joints (78-A:288-298, Feb. 1996) by Watts and Lifeso. J Bone Joint Surg (Am) 1998;80(4):604. [PubMed] [Google Scholar]
- 8.Tuberculose osseuse et articulaire des membres - 09/06/15 : [14-185-A-10] E. Pertuiset (Service de rhumatologie, Centre hospitalier René-Dubos, 6, avenue de l'Île-de-France, BP 90079, 95303 Cergy-Pontoise cedex, France) doi: 10.1016/S0246-0521(15)63675-0. [DOI]
- 9.Vaughan K.D. Extraspinal osteoarticular tuberculosis: a forgotten entity. West Indian Med J. 2005;54(3):202–206. doi: 10.1590/s0043-31442005000300009. [DOI] [PubMed] [Google Scholar]
- 10.Pertuiset E, Beaudreuil J, Horusitzky A, Lioté F, Kemiche F, Richette P, et al. Aspects épidémiologiques de la tuberculose ostéo-articulaire de l'adulte. Étude rétrospective de 206 cas diagnostiqués en région parisienne durant la période 1980-1994. Presse Méd. 1997;26:311–315. [PubMed] [Google Scholar]
- 11.Garrido G, Gomez-Reino JJ, Fernandez-Dapica P, Palenque E, Prieto S. A review of peripheral tuberculous arthritis. Semin Arthritis Rheum. 1988;18:142–149. doi: 10.1016/0049-0172(88)90007-8. [DOI] [PubMed] [Google Scholar]
- 12.Ladeb MF, Chehata S, Kouhen J, Radhouane F, Wybier M. In: Imagerie ostéo-articulaire. Laredo JD, Morvan G, Wybier M, editors. Flammarion Médecine-Sciences; Paris: 1998. Tuberculose articulaire des membres; pp. 383–387. [Google Scholar]
- 13.Ridley N, Shaikh MI, Remedios D, Mitchell R. Radiology of skeletal tuberculosis. Orthopedics. 1998;21:1213–1220. doi: 10.3928/0147-7447-19981101-12. [DOI] [PubMed] [Google Scholar]
- 14.Vuyst de D, Vanhoenacker F, Gielen J, Bernaerts A, De Schepper AM. Imaging features of musculoskeletal tuberculosis. Eur Radiol. 2003;13:1809–1819. doi: 10.1007/s00330-002-1609-6. [DOI] [PubMed] [Google Scholar]
- 15.Sawlani V, Chandra T, Mishra RN, Aggarwal A, Jain UK, Gujral RB. MRI features of tuberculosis of peripheral joints. Clin Radiol. 2003;58:755–762. doi: 10.1016/s0009-9260(03)00271-x. [DOI] [PubMed] [Google Scholar]
- 16.Masood S. Diagnosis of tuberculosis of bone and soft tissue by fine-needle aspiration biopsy. Diagn Cytopathol. 1992;8(5):451–455. doi: 10.1002/dc.2840080505. [DOI] [PubMed] [Google Scholar]
- 17.Tuli SM. General principles of osteoarthicular tuberculosis. Clin Orthop Relat Res. 2002;(398):11–19. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Inoue S, Matsumoto S, Iwamatsu Y, Satomura M. Ankle tuberculosis: a report of four cases in a Japanese hospital. J Orthop Sci. 2004;9(4):392–398. doi: 10.1007/s00776-004-0792-5. [DOI] [PubMed] [Google Scholar]