Abstract
Background/Objective
Although levetiracetam has been increasingly utilized as an alternative to phenytoin for early post-traumatic seizure prophylaxis following traumatic brain injury (TBI), an optimal dosing strategy has not been elucidated. The objective of this study is to determine whether different dosing strategies of levetiracetam are associated with the incidence of early post-traumatic seizures when utilized as prophylaxis following TBI.
Methods
This retrospective single-center cohort study included admitted patients ≥18 years of age with a diagnosis of TBI and receiving levetiracetam for early post-traumatic seizure prophylaxis between July 1, 2013 and September 1, 2019. The primary outcome of this study was to evaluate three different dosing strategies of levetiracetam (≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day) and associated rates of early post-traumatic seizures. Secondary outcomes were to summarize absolute total daily maintenance doses of levetiracetam among patients who experienced early post-traumatic seizures compared to those who did not, determine the impact of three different dosing strategies on hospital length of stay and in-hospital mortality, and to assess patient-specific variables on the occurrence of post-traumatic seizures. Overlap propensity score weighting was utilized to address the potential for confounding.
Results
Of the 1,287 patients who received levetiracetam for early post-traumatic seizure prophylaxis during the study time frame, 866 patients met eligibility criteria and were included in the study cohort (289 patients in the ≤1000 mg/day group, 137 patients in the 1500 mg/day group, and 440 patients in the ≥2000 mg/day group). After weighting, the cumulative incidence of early post-traumatic seizure was 2.9% in the ≤1000 mg/day group, 8.8% in the 1500 mg/day group, and 9% in the ≥2000 mg/day group. The 1500 mg/day and ≥2000 mg/day levetiracetam groups had a 209% and 216% increase in the subdistribution hazard of early post-traumatic seizures compared to the ≤1000 mg/day levetiracetam group respectively, but these differences were not statistically significant.
Conclusions
In conclusion, the results of this study demonstrate no statistically significant difference in the cumulative incidence of early post-traumatic seizures within seven days of TBI between three different levetiracetam dosing strategies. After weighting, the levetiracetam ≤1000 mg/day group had the lowest rates of early post-traumatic seizures, death without seizure, and in-hospital mortality.
Keywords: Traumatic Brain Injury, Early Post Traumatic Seizures, Antiepileptic Drugs
Introduction
Post-traumatic seizures are a potential sequela of traumatic brain injury (TBI) which contribute to significant morbidity for affected patients.1,2 The landmark randomized, controlled trial by Temkin and colleagues demonstrated a significant decrease in early post-traumatic seizures following severe TBI in patients who were given phenytoin prophylaxis compared to those who were not (3.6% vs. 14.2%, p <0.01).3 Based on the results of this trial and subsequent studies, the Brain Trauma Foundation Guidelines recommend phenytoin to decrease the incidence of early post-traumatic seizures within seven days of severe TBI.1
In recent years, levetiracetam has been increasingly utilized as an alternative agent to phenytoin due to fewer adverse effects, fewer drug interactions, ease of administration, and absence of pharmacokinetic variability requiring therapeutic drug monitoring.4–10 In 2013, Inaba and colleagues conducted a prospective, observational, multicenter study (n=813) comparing levetiracetam to phenytoin for the prevention of early post-traumatic seizures.9 No significant differences were identified in the incidence of early post-traumatic seizures, adverse drug reactions, or mortality. While the results of this study suggest levetiracetam is as efficacious as phenytoin, it was limited by selection bias, lack of routine electroencephalogram (EEG) monitoring, and inclusion of only patients with blunt trauma. Aside from this study, the majority of available literature comparing phenytoin to levetiracetam for prevention of post-traumatic seizures consists of single-center data with small sample sizes.4–12 Due to this limited evidence, the Brain Trauma Foundation Guidelines do not currently recommend levetiracetam over phenytoin for the prevention of early post-traumatic seizures.1
In addition to limited comparative data, levetiracetam dosing strategies for post-traumatic seizure prophylaxis are highly variable, ranging from 500 mg to 1500 mg twice daily, and may be dependent on institution-specific practices.4–11 Presently, there is a paucity of available literature regarding the effectiveness of various levetiracetam dosing strategies when utilized for this indication. Additionally, the effect of patient-specific factors, including age, weight, renal function, and severity of illness, have not yet been evaluated.13 The aim of this study is to determine whether different dosing strategies of levetiracetam are associated with the incidence of early post-traumatic seizures when utilized as prophylaxis following TBI.
Methods
Design and Setting
This retrospective single-center cohort study conducted at a Level I trauma center included admitted patients ≥18 years of age with a diagnosis of TBI and receiving levetiracetam for early post-traumatic seizure prophylaxis between July 1, 2013, and September 1, 2019. Patients were excluded if they had a past medical history of seizure disorder prior to TBI and were receiving an anti-seizure drug (ASD) at the time of TBI, documented seizure prior to levetiracetam administration during index hospital admission for TBI, death within 24 hours of hospital admission, >24 hours between hospital admission and initiation of levetiracetam, <2 consecutive doses of levetiracetam, or a past medical history of end-stage renal disease or no serum creatinine available to calculate Creatinine Clearance (CrCl). CrCl was calculated using the Cockcroft-Gault Formula.14 Patients with end-stage renal disease were excluded as levetiracetam is cleared with hemodialysis (HD) requiring supplemental dosing after dialysis sessions. Poor medication adherence after HD could result in fluctuating plasma drug levels.15 If a patient was admitted with TBI more than once during the study period, only the first admission was included. At the study institution, indication for seizure prophylaxis was based on a protocolized approach. Based on institutional protocol, seizure prophylaxis was indicated for patients who experienced head trauma and had a Glasgow Coma Scale (GCS) ≤10 with or without computed tomography (CT) head findings or any CT head findings in the setting of head trauma (regardless of GCS). CT head findings included but were not limited to, subdural or epidural hematoma; subarachnoid, intraparenchymal, or intraventricular hemorrhage; linear or depressed skull fracture; penetrating head injury; or cortical contusion. Levetiracetam dosing for early post-traumatic seizure prophylaxis and EEG monitoring were guided by the treating clinician. During the study time frame, an institutional guideline recommended levetiracetam 1000 mg every 12 hours for patients with a CrCl ≥ 30 mL/min or levetiracetam 250–500 mg every 12 hours for patients with CrCl < 30 mL/min. There were additional dosing recommendations for patients who received intermittent hemodialysis or continuous renal replacement therapy, however, these patients were not included in the study. This study was approved by the Institutional Review Board with a waiver of informed consent.
Measures
The primary objective of this study was to evaluate three different dosing strategies of levetiracetam (≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day) and associated rates of early post-traumatic seizures. The secondary objective was to summarize absolute total daily maintenance doses of levetiracetam among patients who experienced early post-traumatic seizures compared to those who did not. Additional objectives included assessment of EEG confirmed seizure, hospital length of stay (LOS), and in-hospital mortality among three different dosing strategies of levetiracetam. The final objective of the study was to assess the association of patient-specific variables on the occurrence of post-traumatic seizures. The specific stratification of levetiracetam dosing strategies (≤1000 mg/day, 1500 mg/day, ≥2000 mg/day) were selected based on the range of observed dosing strategies in the current literature and at our institution, as well as for the treatment of adult and pediatric epilepsy.4–11,15
Patients were categorized into three levetiracetam dosing strategies, ≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day. The primary outcome was a time-to-event outcome, consisting of a binary event indicator of whether the patient experienced early post-traumatic seizure and a continuous variable of the number of days from TBI to the occurrence of early post-traumatic seizure. Post-traumatic seizures were diagnosed by a confirmatory EEG or clinical diagnosis per the treating clinician. Patients who survived or died after the occurrence of post-traumatic seizure within seven days of TBI were included in the seizure group. Death was considered a competing risk to TBI. Patients who survived or were discharged within seven days of TBI without seizures while receiving levetiracetam were included in the no seizure group. Patients were reviewed for readmission with early post-traumatic seizure if discharged within seven days. Since only early post-traumatic seizures were being evaluated, patients were administratively censored on day seven after TBI. Late post-traumatic seizures (>7 days after index TBI) were not evaluated.
Data Source and Data Collection
Individual patient data was collected through retrospective review of the institutional Trauma Registry and electronic health record including demographics and clinical details [e.g., mechanism of injury, Injury Severity Score (ISS), Trauma and Injury Severity Score (TRISS), Abbreviated Injury Scale (AIS), GCS, CT findings, and operative interventions]. Operative interventions included Burr hole procedure, decompressive craniectomy/hemicraniectomy, or other hematoma evacuation. Additionally, ICU and hospital LOS, in-hospital mortality, levetiracetam dosing and frequency, and documentation of seizure occurrence were collected. EEG data were collected when available. If confirmatory EEG data was not available, clinical characteristics of early post-traumatic seizures were collected as documented by the diagnosing clinician. Levetiracetam maintenance dose and frequency were collected for all included patients. Levetiracetam maintenance dose was collected as the first maintenance dose ordered for seizure prophylaxis following admission for TBI. Dose adjustments, including those following early post-traumatic seizure occurrence, were not collected.
Statistical Analysis
Descriptive statistics were utilized to summarize variables. Overlap propensity score weighting was utilized to address the potential confounding when examining the association between the dosing strategy and post-traumatic seizures. Propensity score weighting is a common approach to balancing the distribution of these prognostic factors between treatment groups so that one can directly estimate the association between the treatment and the outcome after weighting. In this study, since the selection of levetiracetam dosing strategy could have depended on various patient characteristics, injury severity, and interventions that may have influenced outcomes, we first built a propensity score model to obtain the probability of being assigned to each treatment group for each patient based on the prognostic factors. Since there were three different common dosing strategies, a generalized propensity score model was adopted for multiple treatments.16 The generalized propensity score model was a multivariable multinomial logistic regression with the dosing group as the outcome variable, adjusting for the following variables: age, AIS head score (≤3 or >3), pre-hospital GCS (≤10 or >10), operative intervention, cortical contusion, depressed skull fracture, intracranial hemorrhage, penetrating head injury, and CrCl. Intracranial hemorrhage included subdural hematoma, epidural hematoma, subarachnoid hemorrhage, intraparenchymal hemorrhage, and/or intraventricular hemorrhage. To improve balance in covariates, age and creatinine clearance were represented as categorical variables in the propensity score model (Age group: 18–30, 31–50, 51–70, >70; CrCl group: ≥ 80 mL/min, 50–80 mL/min, 30–49 mL/min, < 30 mL/min). The study cohort was then weighted to estimate the average treatment effect for the population using the generalized overlap weights (OW) derived from the propensity scores so that patients who were likely to receive all three treatments were up-weighted, whereas patients who were unlikely to receive one of the treatments were down-weighted. In other words, the OW-weighted cohort emphasizes the portion of the study cohort with the most overlap in prognostic factors among treatment groups. To assess balance in covariates, standardized differences of covariates between pairs of dosing strategies were used after overlap propensity score weighting.17 An absolute standardized mean difference of less than 0.1 was considered a negligible imbalance.18 We selected OW instead of inverse probability of treatment weighting to avoid removing patients with extreme propensity scores and because OW achieved better covariate balance than inverse probability of treatment weighting in our study. Effective sample sizes for the weighted cohort were calculated for each dose group.19 Time to post-traumatic seizure and death were modeled using the OW-weighted Fine-Gray model for competing risk analysis. Subdistribution hazard ratios of early post-traumatic seizures comparing different dosing groups were reported with 95% confidence intervals. Subdistribution hazard ratios of post-traumatic seizures can be interpreted as the relative change in the instantaneous rate of the occurrence of early post-traumatic seizures in those patients who were event-free or who had experienced a competing event, death. The estimated cumulative incidences of early post-traumatic seizures and death were estimated and plotted for each dosing group. Generalized propensity scores and balance diagnostics after overlap weighting are further described in the Supplementary Appendix.
Secondary outcomes were summarized for each dosing group using both the original cohort and the OW-weighted cohort. To assess the association of patient-specific variables on the occurrence of post-traumatic seizures, an unweighted Fine-Gray model was utilized using the original cohort to model time to post-traumatic seizures as a function of the dosing group and the same set of variables included in the generalized propensity score model with age and CrCl modeled as continuous variables. A sensitivity analysis was conducted by additionally adjusting for dosing weight, and the results were similar (data not shown). The significance of tests was assessed at alpha=0.05 without accounting for multiplicity due to the exploratory nature of this study. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and R Statistical Software (version 4.1.1; R Foundation for Statistical Computing, Vienna, Austria). Cumulative incidence plots were created using the ggplot2 package.20 Maximum pairwise standardized differences were plotted using functions modified based on the PSweight package.21
Results
Patient Demographics
Of the 1,287 patients who received levetiracetam for early post-traumatic seizure prophylaxis during the study time frame, 866 patients met eligibility criteria and were included in the study cohort (Figure 1). Patient characteristics are reported in Table 1. In the original cohort, there were 289 patients in the ≤1000 mg/day group, 137 patients in the 1500 mg/day group, and 440 patients in the ≥2000 mg/day group. Prior to weighting, patients in the ≥2000 mg/day group were younger and had higher injury severity compared to the other levetiracetam dosing groups. The majority of patients were male, with a primary mechanism of injury of fall or motor vehicle collision. Penetrating head injury was uncommon, representing 4.4% of the total cohort. Pre-hospital GCS was ≤10 in 251 patients (29%) and AIS head score was >3 in 475 patients (54.8%). The most common CT head finding was intracranial hemorrhage and operative intervention was needed in 188 patients (21.7%). The majority of patients required ICU admission (68.8%). After weighting, patient demographics and injury severity were similar amongst all three dosing groups.
Figure 1. Patient Selection.
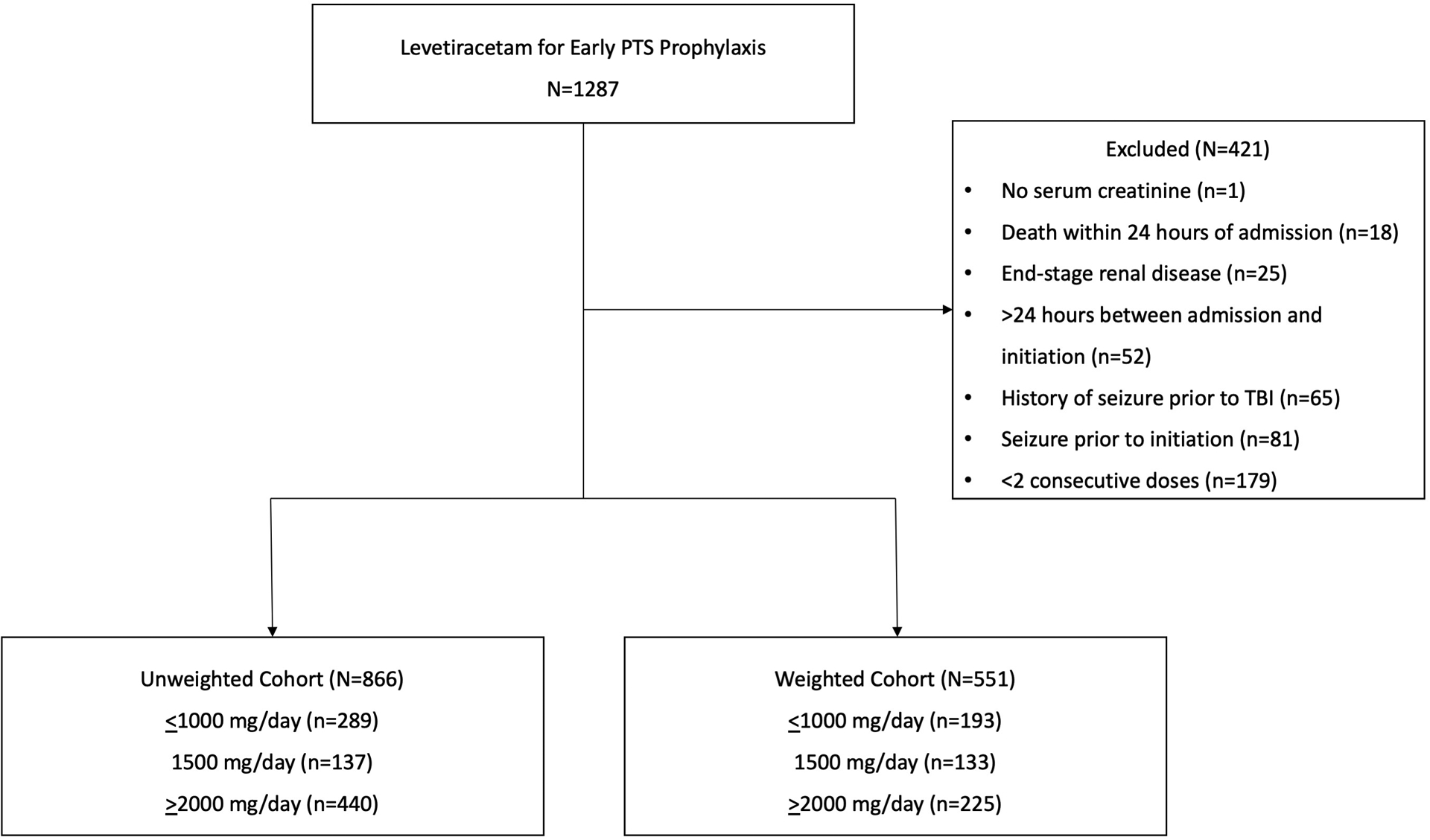
Patient selection, excluded patients, and included patients stratified into unweighted cohorts and weighted cohorts based on levetiracetam dosing group (≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day).
Table 1.
Patient Characteristics
| Original Cohort | Weighted Cohort1 | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (N=866) | Total (N=551) | |||||||
| Age, years (SD) | 72 (17.6) | 63.7 (20.4) | 48.4 (19.2) | 58.7 (21.8) | 62.3 (1.5) | 62.9 (1.8) | 60.5 (1.2) | 61.7 (0.8) |
| Male | 127 (43.9%) | 86 (62.8%) | 335 (76.1%) | 548 (63.3%) | 102 (52.9%) | 84 (63.3%) | 160 (71.3%) | 347 (63.0%) |
| Weight, kg (IQR) | 72.6 (62.1, 85) | 75 (66.4, 87.1) | 79.9 (68.4, 92) | 76.5 (65.3, 89) | 73.9 (63.1, 87.9) | 74.9 (66.3, 86.9) | 79.8 (67.5, 94.9) | 76.5 (64.9, 90.7) |
| CrCl, mL/min (SD) | 73.0 (34.5) | 82.1 (33.3) | 97.3 (36.5) | 86.8 (37) | 84.5 (2.7) | 83.7 (2.9) | 85.7 (2.3) | 84.8 (1.5) |
| Race/ethnicity | ||||||||
| Asian | 5 (1.7%) | 4 (2.9%) | 8 (1.8%) | 17 (2%) | 4 (2.2%) | 3 (2.6%) | 6 (2.5%) | 13 (2.4%) |
| Black | 65 (22.5%) | 31 (22.6%) | 140 (31.8%) | 236 (27.3%) | 59 (30.9%) | 30 (22.4%) | 57 (25.3%) | 146 (26.5%) |
| Hispanic or Latino | 8 (2.8%) | 6 (4.4%) | 33 (7.5%) | 47 (5.4%) | 8 (4%) | 7 (5%) | 10 (4.4%) | 24 (4.4%) |
| White | 201 (69.6%) | 92 (67.2%) | 227 (51.6%) | 520 (60%) | 112 (58.3%) | 89 (67%) | 139 (61.7%) | 340 (61.8%) |
| Other | 10 (3.5%) | 4 (2.9%) | 32 (7.3%) | 46 (5.3%) | 9 (4.6%) | 4 (3.1%) | 14 (6.2%) | 27 (4.9%) |
| Mechanism of injury | ||||||||
| Assault | 15 (5.2%) | 8 (5.8%) | 47 (10.7%) | 70 (8.1%) | 15 (7.9%) | 7 (5.3%) | 20 (8.7%) | 42 (7.6%) |
| Fall | 221 (76.5%) | 86 (62.8%) | 148 (33.6%) | 455 (52.5%) | 125 (65.1%) | 83 (62%) | 122 (54.5%) | 331 (60.0%) |
| GSW | 0 (0%) | 3 (2.2%) | 36 (8.2%) | 39 (4.5%) | 0 (0%) | 3 (2.1%) | 5 (2.2%) | 8 (1.4%) |
| MVC | 37 (12.8%) | 23 (16.8%) | 115 (26.1%) | 175 (20.2%) | 35 (18%) | 23 (17.5%) | 41 (18.3%) | 99 (18.0%) |
| Pedestrian | 10 (3.5%) | 8 (5.8%) | 32 (7.3%) | 50 (5.8%) | 11 (5.9%) | 8 (6.3%) | 13 (5.7%) | 33 (5.9%) |
| Other vehicle | 5 (1.7%) | 8 (5.8%) | 59 (13.4%) | 72 (8.3%) | 5 (2.8%) | 8 (5.9%) | 22 (9.7%) | 35 (6.4%) |
| Other | 1 (0.3%) | 1 (0.7%) | 3 (0.7%) | 5 (0.6%) | 0 (0.2%) | 1 (0.9%) | 2 (0.9%) | 4 (0.7%) |
| CT findings2 | ||||||||
| Cortical contusion | 40 (13.8%) | 25 (18.2%) | 101 (23.0%) | 166 (19.2%) | 40 (20.7%) | 24 (17.7%) | 46 (20.3%) | 109 (19.8%) |
| Intracranial hemorrhage | 281 (97.2%) | 132 (96.4%) | 410 (93.2%) | 823 (95.0%) | 185 (95.8%) | 128 (95.9%) | 214 (95.2%) | 526 (95.6%) |
| Depressed skull fracture | 5 (1.7%) | 6 (4.4%) | 41 (9.3%) | 52 (6%) | 8 (4%) | 4 (3.2%) | 10 (4.3%) | 21 (3.9%) |
| Penetrating head injury | 2 (0.7%) | 2 (1.5%) | 34 (7.7%) | 38 (4.4%) | 3 (1.4%) | 2 (1.2%) | 4 (1.6%) | 8 (1.4%) |
| Pre-hospital GCS | ||||||||
| ≤10 | 33 (11.4%) | 24 (17.5%) | 194 (44.1%) | 251 (29%) | 40 (21%) | 25 (18.6%) | 44 (19.7%) | 110 (19.9%) |
| >10 | 237 (82%) | 105 (76.6%) | 237 (53.9%) | 579 (66.9%) | 142 (73.6%) | 103 (77.2%) | 169 (75%) | 413 (75.1%) |
| AIS Head | ||||||||
| ≤3 | 148 (51.2%) | 65 (47.4%) | 169 (38.4%) | 382 (44.1%) | 93 (48.4%) | 64 (48%) | 109 (48.7%) | 267 (48.4%) |
| >3 | 140 (48.4%) | 71 (51.8%) | 264 (60%) | 475 (54.8%) | 98 (50.7%) | 68 (51.2%) | 113 (50.4%) | 279 (50.7%) |
| Operative intervention3 | 33 (11.4%) | 24 (17.5%) | 131 (29.8%) | 188 (21.7%) | 34 (17.7%) | 23 (17.2%) | 40 (17.8%) | 97 (17.6%) |
| ISS (IQR) | 16 (10, 21) | 17 (10, 25) | 21 (14, 29) | 17 (12, 26) | 16.2 (10, 22.8) | 16.7 (9.6, 24.9) | 16.6 (10, 25.1) | 16.4 (9.9, 24.6) |
| TRISS (IQR) | 0.9 (0.9, 1) | 1.0 (0.9, 1) | 0.9 (0.7, 1) | 0.9 (0.9, 1) | 0.9 (0.9, 1) | 0.9 (0.9, 1) | 0.9 (0.9, 1) | 0.9 (0.9, 1) |
| Treatment for AWS | 25 (8.7%) | 24 (17.5%) | 61 (13.9%) | 110 (12.7%) | 29 (14.9%) | 24 (18.2%) | 29 (13.1%) | 82 (14.9%) |
| ICU admission | 142 (49.1%) | 90 (65.7%) | 364 (82.7%) | 596 (68.8%) | 102 (53.2%) | 87 (65.5%) | 174 (77.3%) | 363 (66.0%) |
| Intubation in the ED | 7 (2.4%) | 12 (8.8%) | 79 (18%) | 98 (11.3%) | 8 (4.4%) | 13 (9.7%) | 20 (9.1%) | 42 (7.6%) |
Data are presented as mean (SD), median (IQR), or n (%)
N’s in the weighted cohort for each dose group are the effective sample sizes.
CT findings are not mutually exclusive. Intracranial hemorrhage included subdural hematoma, subarachnoid hemorrhage, intraparenchymal hemorrhage, intraventricular hemorrhage, or epidural hematoma.
Operative interventions included Burr hole procedure, decompressive craniectomy/hemicraniectomy, or other hematoma evacuation
SD: Standard deviation. IQR: Interquartile range. CrCl: Creatinine clearance. GSW: Gunshot wound. MVC: Motor vehicle collision. GCS: Glasgow Coma Scale. AIS: Abbreviated Injury Scale. ISS: Injury Severity Score. TRISS: Trauma and Injury Severity Score. AWS: Alcohol Withdrawal Syndrome. ICU: Intensive Care Unit. ED: Emergency Department.
Primary Outcome
In the original cohort, 51 (5.9%) patients experienced an early post-traumatic seizure, 54 (6.2%) patients died without seizures, and 761 (87.9%) did not encounter these events in 7 days. Of the patients who experienced early post-traumatic seizures, 27 (51.9%) experienced convulsive seizures, and 25 (48.1%) experienced nonconvulsive seizures. The cumulative incidence of early post-traumatic seizure was 3.9% in the ≤1000 mg/day group, 7.8% in the 1500 mg/day group, and 8.4% in the ≥2000 mg/day group. After weighting, the cumulative incidence of early post-traumatic seizure was 2.9% in the ≤1000 mg/day group, 8.8% in the 1500 mg/day group, and 9% in the ≥2000 mg/day group (Table 2, Figure 2). After weighting, the 1500 mg/day and ≥2000 mg/day levetiracetam groups had a 209% and 216% increase in the subdistribution hazard of early post-traumatic seizures compared to the ≤1000 mg/day levetiracetam group respectively, but these differences were not statistically significant.
Table 2.
Primary Outcome
| Total Daily Maintenance Dose |
Early PTS Cumulative Incidence (95% CI) |
Early PTS OW-weighted Cumulative Incidence (95% CI) |
Death Cumulative Incidence (95% CI) |
Death OW-weighted Cumulative Incidence (95% CI) |
|---|---|---|---|---|
| ≤1000 mg/day | 0.039 (0.02, 0.075) | 0.029 (0.014, 0.062) | 0.058 (0.036, 0.093) | 0.04 (0.022, 0.075) |
| 1500 mg/day | 0.078 (0.044, 0.139) | 0.088 (0.049, 0.158) | 0.067 (0.035, 0.13) | 0.067 (0.031, 0.144) |
| ≥2000 mg/day | 0.084 (0.061, 0.118) | 0.09 (0.059, 0.137) | 0.096 (0.069, 0.133) | 0.094 (0.058, 0.153) |
| Total Daily Maintenance Dose |
Early PTS OW-weighted Estimated sHRs (95% CI) |
P-value | Death OW-weighted Estimated sHRs (95% CI) |
P-value |
| 1500 mg/day vs. ≤1000 mg/day |
3.09 (0.44, 21.85) | 0.26 | 1.67 (0.26, 10.96) | 0.59 |
| ≥2000 mg/day vs. ≤1000 mg/day |
3.16 (0.45, 22.25) | 0.25 | 2.39 (0.4, 14.16) | 0.34 |
| ≥2000 mg/day vs. 1500 mg/day |
1.02 (0.27, 3.91) | 0.98 | 1.43 (0.32, 6.33) | 0.64 |
Cumulative incidences were estimated using the Fine-Gray subdistribution hazard models. Subdistribution hazard ratios (sHR) were obtained from the OW-weighted Fine-Gray model.
PTS: Post-traumatic seizures. OW: Overlap weights. sHRs: Subdistribution hazard ratios.
Figure 2. Overlap weights (OW)-Weighted Cumulative Incidences for Post-Traumatic Seizure and Death by Daily Levetiracetam Maintenance Dose.
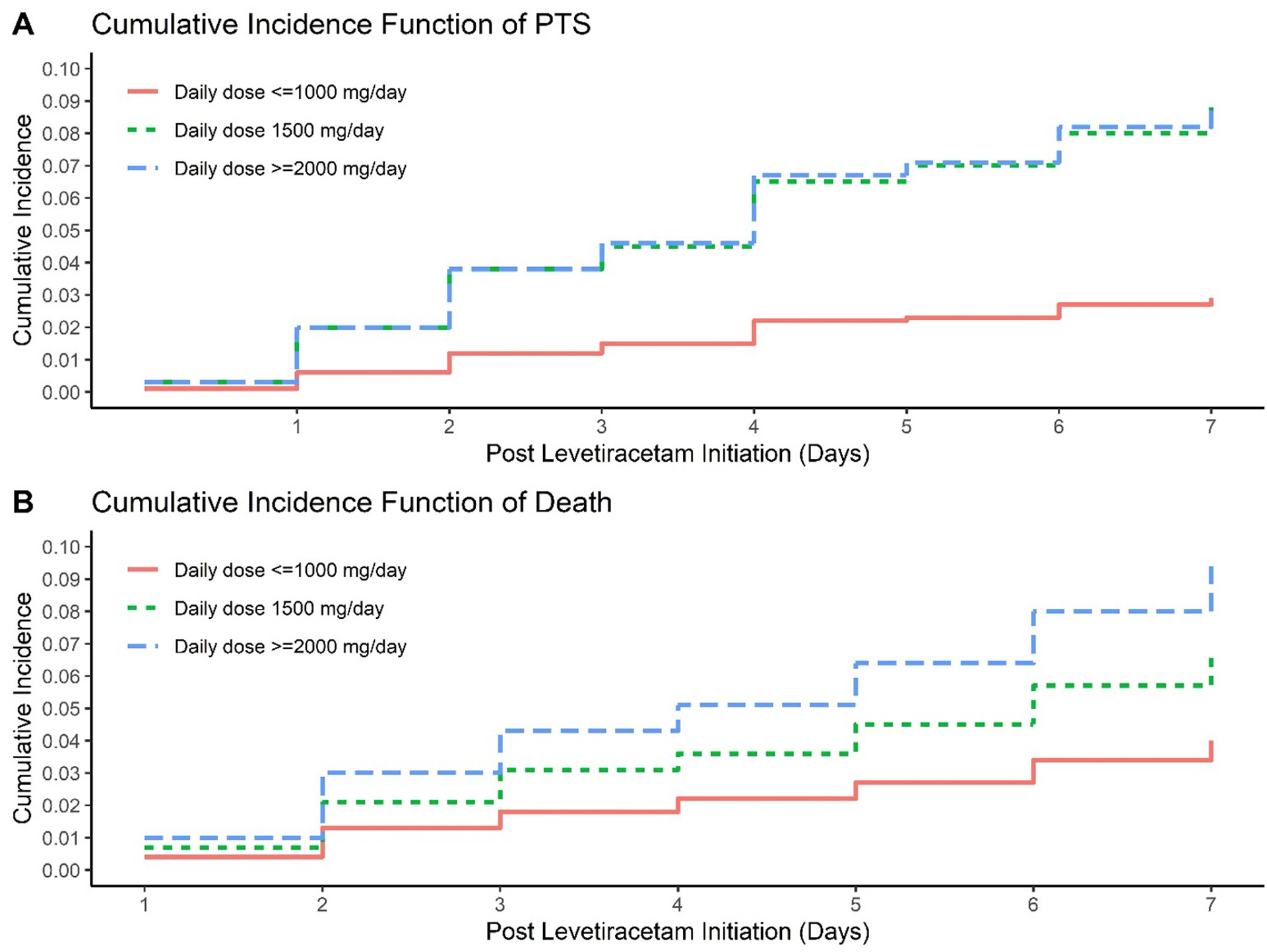
Figure 2A, OW-weighted cumulative incidence of early post-traumatic seizure based on total daily maintenance levetiracetam dose (≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day). Figure 2B, OW-weighted cumulative incidence of death based on total daily maintenance levetiracetam dose (≤1000 mg/day, 1500 mg/day, and ≥2000 mg/day).
Secondary Outcomes
Secondary outcomes are reported in Table 3. In the original cohort, seizures were validated with EEG in 33 of the 51 patients who experienced early post-traumatic seizures (64.7%). The majority of EEG-validated seizures were prolonged/continuous EEG (97.1%), only one seizure was validated with routine EEG (2.94%). The remaining seizures were validated with a clinical diagnosis (35.3%). The mean time to early post-traumatic seizure was 45.9 hours (±29.4 hours) in the ≤1000 mg/day group, 72.6 hours (±44.8 hours) in the 1500 mg/day group, and 57.3 hours (±44.9 hours) in the ≥2000 mg/day group. Death without seizure occurred in 12 patients (4.2%) in the ≤1000 mg/day group, 7 patients (5.1%) in the 1500 mg/day group, and 35 patients (8%) in the ≥2000 mg/day group. In-hospital mortality occurred in 19 patients (6.6%) in the ≤1000 mg/day group, 13 patients (9.5%) in the 1500 mg/day group, and 74 patients (16.8%) in the ≥2000 mg/day group. Hospital LOS was similar amongst the groups, but longest in the ≥2000 mg/day group [9.5 days (IQR 4 days, 23 days)]. Of the patients who experienced early post-traumatic seizures, 31 of 52 needed operative intervention (59.6%). However, the majority of post-traumatic seizures occurred prior to operative intervention (77.4%). Seven early post-traumatic seizures occurred after operative intervention (22.6%). Overall, after weighting, the ≤1000 mg/day group had the lowest rates of early post-traumatic seizures, death without seizure, and in-hospital mortality.
Table 3.
Secondary Outcomes
| Total (N=866) | Total (N=551) | |||||||
|---|---|---|---|---|---|---|---|---|
| Early PTS | 9 (3.1%) | 9 (6.6%) | 33 (7.5%) | 51 (5.9%) | 4 (2.3%) | 9 (7%) | 16 (7.3%) | 30 (5.5%) |
| Time to seizure, hours (SD) | 45.9 (29.4) | 72.6 (44.8) | 57.3 (44.9) | 58 (42.6) | 42.6 (6.7) | 76.6 (16.7) | 66.9 (12.7) | 66.4 (8.8) |
| Clinical diagnosis | 6 (66.7%) | 2 (22.2%) | 10 (30.3%) | 18 (35.3%) | 3 (75.2%) | 2 (19.7%) | 3 (20.7%) | 8 (28.3%) |
| Death without seizure | 12 (4.2%) | 7 (5.1%) | 35 (8%) | 54 (6.2%) | 6 (2.9%) | 7 (5%) | 16 (7.2%) | 28 (5.1%) |
| In-hospital mortality | 19 (6.6%) | 13 (9.5%) | 74 (16.8%) | 106 (12.2%) | 10 (5.2%) | 12 (9.2%) | 37 (16.4%) | 59 (10.7%) |
| Hospital LOS, days (IQR) | 5 (3, 10) | 6 (3, 11) | 9.5 (4, 23) | 7 (3, 17) | 5.5 (2.2, 13.7) | 5.8 (2.4, 11.1) | 6.1 (2.5, 16.4) | 5.8 (2.4, 14.1) |
Data are presented as mean (SD), median (IQR), or n (%)
PTS: Post-traumatic seizures. SD: Standard deviation. EEG: Electroencephalogram. LOS: Length of stay. IQR: Interquartile range.
In the unweighted Fine-Gray multivariable regression model, there were no statistically significant differences in the cumulative incidences of early post-traumatic seizures between the three levetiracetam dosing groups (Table 4). Older age, higher AIS head score, pre-hospital GCS ≤10, and need for operative intervention were associated with a significant increase in the subdistribution hazard rate of early post-traumatic seizures. Additional factors, such as CT head findings and admission CrCl were not associated with the incidence of early post-traumatic seizures. Higher AIS head score, pre-hospital GCS ≤10, and CT finding of penetrating head injury were associated with a significant increase in the subdistribution hazard rate of death.
Table 4.
Unweighted Fine-Gray Subdistribution Hazard Model for Cumulative Incidence of Early PTS
| Early PTS | Death | |||
|---|---|---|---|---|
| sHR (95% CI) | P-value | sHR (95% CI) | P-value | |
| Age (1-year increase) | 1.04 (1.02, 1.07) | <0.01 | 1.02 (1, 1.05) | 0.09 |
| AIS head > 31 | 3.65 (1.47, 9.07) | <0.01 | 2.01 (1.02, 3.97) | 0.04 |
| Pre-hospital GCS >102 | 0.42 (0.22, 0.81) | <0.01 | 0.2 (0.1, 0.37) | <0.01 |
| Operative intervention | 3.89 (2.15, 7.03) | <0.01 | 0.64 (0.33, 1.23) | 0.18 |
| Daily dose <=1000 mg/day3 | 0.53 (0.22, 1.28) | 0.16 | 0.89 (0.36, 2.23) | 0.8 |
| Daily dose >=2000 mg/day3 | 1.22 (0.57, 2.58) | 0.61 | 1.22 (0.57, 2.58) | 0.48 |
| Cortical contusion | 1.31 (0.64, 2.68) | 0.46 | 0.85 (0.42, 1.72) | 0.66 |
| Intracranial hemorrhage | 0.61 (0.07, 5.42) | 0.66 | 0.39 (0.15, 0.99) | 0.05 |
| Penetrating head wound | Not included4 | 2.89 (1.17, 7.16) | 0.02 | |
| Depressed skull fracture | 0.46 (0.05, 4.14) | 0.49 | Not included4 | |
| CrCl (1-unit increase) | 1 (0.99, 1.01) | 0.64 | 0.99 (0.98, 1) | 0.16 |
AIS head ≤3 used as reference value
Pre-hospital GCS ≤10 used as reference value
Daily levetiracetam dose of 1500 mg/day used as reference value
Variable was not included in the model because of the complete separation of patients.
sHR: Subdistribution hazard ratio. AIS: Abbreviated Injury Scale. GCS: Glasgow Coma Scale. CrCl: Creatinine clearance.
Discussion
In this retrospective single-center cohort study, there were no significant differences in the cumulative incidences of early post-traumatic seizures or death within seven days of TBI between three different levetiracetam dosing strategies. These results remained consistent in both the original and weighted cohorts. Additionally, rates of early post-traumatic seizures, death without seizure, in-hospital mortality, and hospital LOS remained lowest in the ≤1000 mg/day levetiracetam group. While the implications of patient-specific factors on levetiracetam dosing strategy are still exploratory, the results of this study demonstrate that higher total daily maintenance doses of levetiracetam were not associated with a reduced incidence of early post-traumatic seizures as was hypothesized. Although causality cannot be established, the results of this study are hypothesis-generating in that lower total daily maintenance doses of levetiracetam (≤1000 mg/day) could be effective in preventing early post-traumatic seizures following TBI.
Post-traumatic seizures are estimated to occur in approximately 1.5% to 3.6% of patients who receive ASDs for prophylaxis following severe TBI.3,5,9,10 The prospective, observational, multicenter study conducted by Inaba and colleagues (n=813) compared levetiracetam to phenytoin for the prevention of early post-traumatic seizures.9 This cohort of patients experienced similar TBI severity as our study cohort, in which patients in the levetiracetam group received levetiracetam 1000 mg every 12 hours intravenously or enterally for 7 days. There were no significant differences in seizure rates (1.5% vs. 1.5%, p=0.997), adverse drug reactions, or mortality. Similarly, the prospective, randomized, single-blinded comparative trial conducted by Szaflarski and colleagues (n=52) demonstrated no difference in early post-traumatic seizures occurrence in patients receiving phenytoin compared to levetiracetam for prophylaxis following TBI with a starting dose of 1000 mg every 12 hours intravenously (16.7% vs. 14.7%, p>0.99).10 In the prospective observational cohort study conducted by Jones and colleagues (n=27), EEG findings were compared in patients receiving phenytoin to those receiving levetiracetam for seizure prophylaxis following severe TBI.5 Patients in the levetiracetam group received levetiracetam 500 mg every 12 hours intravenously for 7 days. Overall, patients had equivalent incidence of seizure activity (p=0.556), but patients receiving levetiracetam had a higher incidence of abnormal EEG findings (p=0.003).5 Although this study is limited by the small sample size, it highlights the need for further investigation into the implications of increased seizure tendency and epileptiform activity observed with levetiracetam when utilized as prophylaxis following TBI.
The cumulative incidence of early post-traumatic seizures was similar in the present study compared to currently published literature.3,5,9,10 Patients who experienced early post-traumatic seizures in our cohort had similar baseline injury severity and operative intervention to those included in previously published studies.3,5,9,10 Although there may have been patient-specific unanticipated confounders that could not be controlled for prospectively in our cohort, the unweighted multivariable regression model utilized in our study demonstrated that older age, AIS head score >3, pre-hospital GCS ≤10, and operative interventions were associated with increased risk of early post-traumatic seizures. These findings are consistent with the currently published literature.3,5,6,9,10 Additionally, prolonged EEG monitoring was obtained for the majority of patients who experienced early post-traumatic seizures in our study, which may have contributed to the increased incidence reported, particularly for nonconvulsive seizures.
Limitations of this study include those inherent to retrospective evaluations, including reliance on accurate documentation in the electronic medical record. Levetiracetam dosing was not standardized during the study period and causality cannot be determined. Administration of levetiracetam loading dose was not standardized practice at the study institution. Additionally, levetiracetam dose adjustments, including adjustments after the occurrence of early post-traumatic seizures, were not collected retrospectively. Aside from new seizure occurrence, adjustments to levetiracetam for the indication of early post-traumatic seizure prophylaxis were anticipated to be minimal at the study institution. However, levetiracetam dose adjustments that were not accounted for may have impacted study findings. Similarly, concomitant medications that may have provided additional anti-seizure benefit, including benzodiazepines, propofol, and gabapentin, were not accounted for retrospectively. Although these medications certainly could have impacted early post-traumatic seizure occurrence, the anticipated impact is expected to be minimal given the small percentage of patients undergoing treatment for alcohol withdrawal as well as mechanical ventilation during the study time frame. Barbiturates were not routinely used at the study institution during the study time frame. Due to the low incidence of observed early post-traumatic seizures in this study cohort, differences have marginal significance due to the small sample size. An a priori sample size calculation was not performed, as all patients who met inclusion criteria were included in the study cohort. Given the retrospective nature of this study, it remains unclear whether clinician selection bias may have influenced the observed higher total daily maintenance doses of levetiracetam in patients who experienced early post-traumatic seizures compared to those who did not. Similarly, without prospective randomization, there may have been unanticipated confounders that were not accounted for. Moreover, patients perceived to be more severely ill and thus more prone to post-traumatic seizures by the clinical team, may have received higher doses of levetiracetam, but experienced similar rates of post-traumatic seizures due to the severity of their underlying disease. Lastly, due to retrospective study design, adverse drug events associated with levetiracetam were not able to be reliably captured. Pertaining to EEG monitoring, if there was a concern for early post-traumatic seizure, routine or prolonged EEG monitoring was obtained per the treating clinician. The majority of early post-traumatic seizures were confirmed by prolonged EEG. However, there was no empiric EEG monitoring conducted at the study institution, so there is a possibility of uncaptured subclinical nonconvulsive seizures.
Strengths of this study include the novel association of various levetiracetam dosing strategies with cumulative incidence of early post-traumatic seizures. Additionally, the use of OW-weighting and completion of a subdistributional hazard regression analysis improve the validity of this study’s findings. Based on the results of this study, higher total daily maintenance doses of levetiracetam (≥1500 mg/day) commonly utilized in clinical practice may not be more effective in preventing early post-traumatic seizures compared to lower doses (≤1000 mg/day). Additional prospective data are needed to further explore these findings and validate these results.
Conclusion
Overall, the results of this study demonstrate no statistically significant difference in the cumulative incidence of early post-traumatic seizures within seven days of TBI between three different levetiracetam dosing strategies. Older age, AIS head score >3, pre-hospital GCS ≤10, and need for operative intervention were associated with an increased risk of early post-traumatic seizures in this cohort. Prospective studies are needed to further validate these findings by including a control group, standardizing levetiracetam dosing, and assessing adverse drug events.
Supplementary Material
Funding and Conflicts of Interest
Research reported in this publication was supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002553. Additionally, research reported in this publication was supported in part by a Pfizer Foundation grant and the Duke Clinical and Translational Science Institute (CTSI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Pfizer Foundation, or the Duke CTSI.
Footnotes
The Institutional Review Board approved the study prior to data collection and waived the need for informed consent.
Contributor Information
Kelsey Ohman, Department of Pharmacy, Duke University Hospital.
Bridgette Kram, Department of Pharmacy, Duke University Hospital.
Jennifer Schultheis, Department of Pharmacy, Duke University Hospital.
Jana Sigmon, Department of Pharmacy, Harris Health System.
Safa Kaleem, Department of Neurology, NewYork-Presbyterian Weill Cornell Medical Center.
Zidanyue Yang, Department of Biostatistics and Bioinformatics, Duke University Hospital.
Hui-Jie Lee, Department of Biostatistics and Bioinformatics, Duke University Hospital.
Cory Vatsaas, Department of Trauma and Critical Care Surgery, Duke University Hospital.
Jordan Komisarow, Department of Neurosurgery, Duke University Hospital.
References
- 1.Carney N, Totten AM, O’Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. Jan 2017;80(1):6–15. doi: 10.1227/NEU.0000000000001432 [DOI] [PubMed] [Google Scholar]
- 2.Ferguson PL, Smith GM, Wannamaker BB, Thurman DJ, Pickelsimer EE, Selassie AW. A population-based study of risk of epilepsy after hospitalization for traumatic brain injury. Epilepsia. May 2010;51(5):891–8. doi: 10.1111/j.1528-1167.2009.02384.x [DOI] [PubMed] [Google Scholar]
- 3.Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. Aug 1990;323(8):497–502. doi: 10.1056/NEJM199008233230801 [DOI] [PubMed] [Google Scholar]
- 4.Gabriel WM, Rowe AS. Long-term comparison of GOS-E scores in patients treated with phenytoin or levetiracetam for posttraumatic seizure prophylaxis after traumatic brain injury. Ann Pharmacother. Nov 2014;48(11):1440–4. doi: 10.1177/1060028014549013 [DOI] [PubMed] [Google Scholar]
- 5.Jones KE, Puccio AM, Harshman KJ, et al. Levetiracetam versus phenytoin for seizure prophylaxis in severe traumatic brain injury. Neurosurg Focus. Oct 2008;25(4):E3. doi: 10.3171/FOC.2008.25.10.E3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan NR, VanLandingham MA, Fierst TM, et al. Should Levetiracetam or Phenytoin Be Used for Posttraumatic Seizure Prophylaxis? A Systematic Review of the Literature and Meta-analysis. Neurosurgery. Dec 2016;79(6):775–782. doi: 10.1227/NEU.0000000000001445 [DOI] [PubMed] [Google Scholar]
- 7.Kruer RM, Harris LH, Goodwin H, et al. Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care. Oct 2013;28(5):883.e9–13. doi: 10.1016/j.jcrc.2012.11.020 [DOI] [PubMed] [Google Scholar]
- 8.Wilson CD, Burks JD, Rodgers RB, Evans RM, Bakare AA, Safavi-Abbasi S. Early and Late Posttraumatic Epilepsy in the Setting of Traumatic Brain Injury: A Meta-analysis and Review of Antiepileptic Management. World Neurosurg. Feb 2018;110:e901–e906. doi: 10.1016/j.wneu.2017.11.116 [DOI] [PubMed] [Google Scholar]
- 9.Inaba K, Menaker J, Branco BC, et al. A prospective multicenter comparison of levetiracetam versus phenytoin for early posttraumatic seizure prophylaxis. J Trauma Acute Care Surg. Mar 2013;74(3):766–71; discussion 771–3. doi: 10.1097/TA.0b013e3182826e84 [DOI] [PubMed] [Google Scholar]
- 10.Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. Apr 2010;12(2):165–72. doi: 10.1007/s12028-009-9304-y [DOI] [PubMed] [Google Scholar]
- 11.Wat R, Mammi M, Paredes J, et al. The Effectiveness of Antiepileptic Medications as Prophylaxis of Early Seizure in Patients with Traumatic Brain Injury Compared with Placebo or No Treatment: A Systematic Review and Meta-Analysis. World Neurosurg. Feb 2019;122:433–440. doi: 10.1016/j.wneu.2018.11.076 [DOI] [PubMed] [Google Scholar]
- 12.Owen E, Creel-Bulos C, Willman M, Keeperman J. High-Versus Low-Dose Levetiracetam Seizure Prophylaxis for Mild to Moderate Traumatic Brain Injury. Crit Care Med. Jan 2018;46(1):455. doi: 10.1097/01.ccm.0000528950.75491.1b [DOI] [Google Scholar]
- 13.Udy AA, Jarrett P, Lassig-Smith M, et al. Augmented Renal Clearance in Traumatic Brain Injury: A Single-Center Observational Study of Atrial Natriuretic Peptide, Cardiac Output, and Creatinine Clearance. J Neurotrauma. January 01 2017;34(1):137–144. doi: 10.1089/neu.2015.4328 [DOI] [PubMed] [Google Scholar]
- 14.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi: 10.1159/000180580 [DOI] [PubMed] [Google Scholar]
- 15.Shiue HJ, Taylor M, Sands KA. Comparison of Levetiracetam Dosing Regimens in End-Stage Renal Disease Patients Undergoing Intermittent Hemodialysis. Ann Pharmacother. Oct 2017;51(10):862–865. doi: 10.1177/1060028017713294 [DOI] [PubMed] [Google Scholar]
- 16.Li F, Li F. Propensity score weighting for causal inference with multiple treatments. The Annals of Applied Statistics 2019. p. 2389–2415. [Google Scholar]
- 17.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. Dec 10 2015;34(28):3661–79. doi: 10.1002/sim.6607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Granger E, Watkins T, Sergeant JC, Lunt M. A review of the use of propensity score diagnostics in papers published in high-ranking medical journals. BMC Med Res Methodol. May 27 2020;20(1):132. doi: 10.1186/s12874-020-00994-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chattopadhyay A, Hase CH, Zubizarreta JR. Balancing vs modeling approaches to weighting in practice. Stat Med. October 30 2020;39(24):3227–3254. doi: 10.1002/sim.8659 [DOI] [PubMed] [Google Scholar]
- 20.H W. Data from: ggplot2: Elegant Graphics for Data Analysis. 2016;ISBN 978–3-319–24277-4. Springer-Verlag; New York. [Google Scholar]
- 21.Zhou T, Tong G, Li F, Thomas L, Li F. PSweight: Propensity Score Weighting for Causal Inference with Observational Studies and Randomized Trials. R package version 1.1.5. 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


