Abstract
Objectives
High sedentary behaviour is associated with adverse effects on central vascular function and cognitive function. Although interventions to mitigate the adverse effects of workplace sitting are intriguing, evidence of the efficacy of such interventions remains lacking. This randomised cross-over trial was aimed at exploring the effectiveness of prolonged sitting, with or without physical activity breaks, on central, peripheral vascular and cognitive function in adults.
Methods
Twenty one healthy adults completed 4 h of simulated work conditions in three experimental visits: (1) uninterrupted sitting (SIT); (2) sitting interrupted by 3 min of walking every hour (LIT); and (3) sitting interrupted by 3 min of stair climbing every hour (MIT). Carotid (CA) and superficial femoral artery (SFA) diameter, velocity, shear rate and blood flow were measured with Duplex ultrasound at 50 MHz at three time points (hours 0, 2 and 4), and executive function was assessed with the computer based Eriksen Flanker task every hour.
Results
The decreases in reaction time (−30.59%) and accuracy (−10.56%) during SIT conditions were statistically significant, and less of a decrease was observed under LIT and MIT conditions. No significant differences in CA and SFA function were observed with LIT and MIT interventions.
Conclusion
Physical activity breaks of varying intensity during prolonged sitting improve reaction time. However, the vascular benefits of physical activity breaks should be confirmed in the future through long term studies in natural environment.
Keywords: Endothelial function, Executive function, Movement breaks, Physical activity, Sedentary behaviour, Sitting posture
المخلص
أهداف البحث
يرتبط السلوك الخامل المرتفع بوظائف الأوعية الدموية المركزية المعاكسة والخلل الإدراكي. التدخلات لتخفيف الآثار السلبية للجلوس في مكان العمل مثيرة للاهتمام، ومع ذلك، فإن الأدلة التي تدعي فعالية مثل هذه التدخلات لا تزال تظهر. تهدف تجربة التقاطع العشوائية الحالية إلى استكشاف فعالية الجلوس لفترات طويلة مع أو بدون فواصل النشاط البدني على وظائف الأوعية الدموية المركزية والطرفية والمعرفية لدى البالغين.
طرق البحث
أكمل واحد وعشرين من البالغين الأصحاء أربع ساعات من محاكاة ظروف العمل في ثلاث زيارات تجريبية: (1) الجلوس دون انقطاع؛ (2) يقطع الجلوس ثلاث دقائق سيرا على الأقدام كل ساعة؛ (3) يقطع الجلوس ثلاث دقائق من صعود السلم كل ساعة. تم قياس قطر الشريان السباتي والسطحي والسرعة ومعدل القص وتدفق الدم باستخدام الموجات فوق الصوتية المزدوجة عند 50 ميجاهرتز في ثلاث نقاط زمنية (الساعة صفر والثانية والرابعة) بينما تم تقييم الوظائف التنفيذية باستخدام إريكسن فلانكر المعتمدة على الحاسوب كل ساعة.
النتائج
كان الانخفاض في أوقات رد الفعل (-30.59٪) والدقة (-10.56٪) أثناء ظروف الجلوس غير المنقطعة ذات دلالة إحصائية، بينما كان الانخفاض أقل أثناء الجلوس المتقطع بثلاث دقائق من المشي كل ساعة والجلوس بثلاث دقائق من صعود السلم كل ساعة. لم يلاحظ وجود فروق ذات دلالة إحصائية في وظائف الشريان السباتي والشريان الفخذي السطحي مع توقف الجلوس لمدة ثلاث دقائق من المشي كل ساعة والجلوس بثلاث دقائق من صعود السلم كل ساعة تدخل.
الاستنتاجات
تم العثور على فواصل النشاط البدني متفاوتة الشدة أثناء الجلوس لفترات طويلة لتحسين أوقات رد الفعل. ومع ذلك، يجب تأكيد الفوائد الوعائية لفواصل النشاط البدني من خلال الدراسات المستقبلية في الوقت الفعلي.
الكلمات المفتاحية: الوظائف البطانية, الوظائف التنفيذية, فواصل الحركة, النشاط البدني, السلوك المستقر, وضعية الجلوس
Introduction
In the modernised world, manual labour has substantially decreased because of computerisation, and high levels of sedentary behaviours are evident in modern workplaces.1,2 Sedentary behaviour, defined as any waking behaviour, e.g., reclined posture or sitting characterised by low energy expenditure, is likely to be associated with chronic disease risk.3 Hyperglycaemia, hyperlipidaemia-induced inflammation and resulting altered vascular stress associated with sedentary behaviour are proposed mechanisms of chronic disease risk.4, 5, 6, 7
Emerging evidence indicates that uninterrupted prolonged sitting decreases carotid and superficial femoral artery blood flow, thereby decreasing blood supply to the temporal and frontal areas of the brain, which are involved in memory and executive function.8, 9, 10, 11 Although periodic movement breaks have been hypothesised to improve central and peripheral vascular function through altered shear stress, vasodilating mediators such as nitric oxide, prostaglandins and vascular compliance, evidence regarding the intensity of these breaks remains under debate.8,12 Moderate to vigorous physical activity is well established to improve adult endothelial function.13,14 Early laboratory studies have suggested a similar favourable vascular benefit with light-intensity activities; however, recent meta-analytic studies have revealed limited evidence regarding the favourable vascular effects of movement breaks or ‘snackivity’.15,16
Substantial evidence now suggests that physical activity breaks can favourably influence executive function in children.17,18 Executive function refers to an array of higher-order mental processes that enable individuals to exert self-control and self-regulate their behaviour.17 Executive function is assessed according to three core processes: (1) inhibition: inhibiting predominant responses and controlling attention; (2) switching between mental tasks or mental rotation; and (3) memory: retaining information and processing at need.18 Executive function is an inherent predictor of problem-solving ability and work productivity.19,20 Low central vascular dysfunction is associated with cognitive decline, poor problem-solving ability and low work productivity.21 Although prolonged sitting is associated with vascular dysfunction, evidence of the efficacy of active physical activity breaks in achieving regional vascular outcomes is mixed.16 The effectiveness of physical activity breaks remain uncertain, because most studies have manipulated the frequency and duration of physical activity breaks but not the intensity—a factor potentially linking physical activity breaks to favourable vascular function in adults.12
Empirical evidence suggests that high-intensity exercise enhances shear stress-induced nitric oxide bioavailability, vascular diameter and blood flow, and restores vascular homeostasis to a greater extent than moderate- and low-intensity exercise.22 Furthermore, high-intensity exercise is a time-efficient and accessible modality for decreasing cardiovascular risk. Evidence regarding active breaks has varied only in duration and frequency, and mixed evidence regarding the vascular benefits of physical activity breaks has been observed.16 However, the favourable vascular effects associated with moderate-to-high-intensity physical activity breaks, such as stair climbing, remain unclear. To our knowledge, only one experimental study by Cho (2020) has found that 5 min stair climbing bouts during prolonged sitting attenuate the decrease in endothelial function after a high-fat meal.23 However, the comparison of vascular effects between active physical activity breaks of varied intensity (light = walking, moderate-high = stair climbing) remains to be investigated.
Here, we aimed to explore the influence of movement breaks of varying intensity during prolonged sitting on vascular and cognitive function during simulated work conditions in young adults. Furthermore, we explored whether the change in vascular function might correspond to a change in executive function with active physical activity breaks during a simulated workday. Our results may encourage occupational and public health experts to design appropriate (time-efficient, accessible and cost-effective) movement break strategies with sufficient intensity to mitigate the adverse vascular and cognitive function associated with prolonged sitting and improve work productivity.
Materials and Methods
Our randomised cross-over trial is presented according to the “Consolidated Standards of Reporting Trials (CONSORT) 2010 statement: extension to randomised cross-over trials”24 (checklist provided in Supplementary file S1).
Trial design and setting
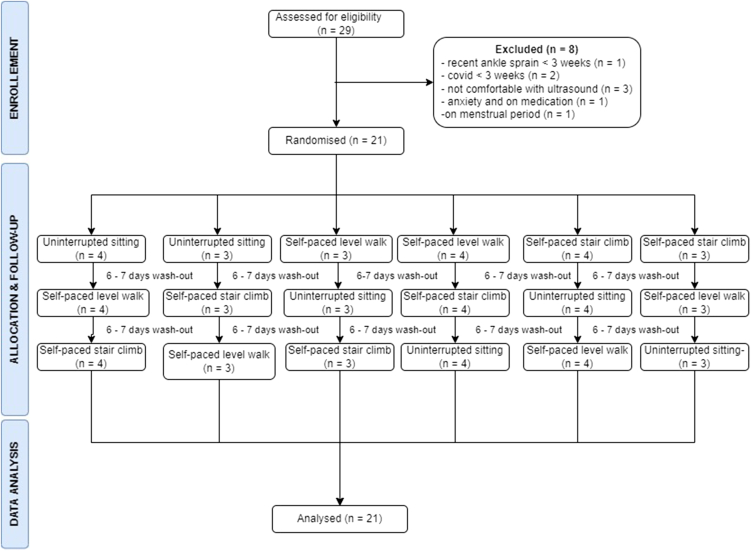
The details of the method have been published previously.25 This counterbalanced randomised crossover trial was conducted between November 2021 and February 2022, with the aim of exploring the effectiveness of physical activity breaks of differing intensity on central and peripheral vascular function, and their association with executive function in young adults. The Kasturba Hospital Institutional Ethics Committee approved the study. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki. The design of the trial is illustrated in Figure 1.
Figure 1.
The study design used for the present randomised cross-over trial. The participants were randomised to three interventions: (1) SIT: uninterrupted sitting for 4 h; (2) LIT: sitting interrupted by light intensity moderate physical activity breaks for 3 min every hour for the next 5 h; and (3) MIT: sitting disrupted by moderate-intensity physical activity breaks for 3 min every hour for the next 5 h. Carotid and superficial femoral artery function were measured every 2 h in the intervention visit. In contrast, executive function was measured every hour for the next 4 h in the intervention visit.
Participants
After the necessary permissions had been granted by the ethical committee and higher authorities, young adults (25–35-year-old men and women), were invited to participate through official emails and advertisements on social media. The participants were deemed eligible if they were physically inactive (self-reported physical activity levels less than 600 METS minutes per week, assessed with the International Physical Activity Questionnaire), had good visual acuity (>5/6) and were able to climb at least two flights of stairs. Volunteers with established cardiovascular, metabolic or mental health disorders affecting central and peripheral vascular and executive function were excluded. Furthermore, participants who were taking drugs that might affect their participation in physical activity (e.g., beta-blockers or anxiolytic drugs) or who had experienced musculoskeletal trauma within 3 weeks that might limit stair climbing were excluded from the study. All participants provided written informed consent.
Physical activity break interventions
In the present study, prolonged sitting was interrupted by physical activity breaks of two intensities: (1) In light intensity breaks (LIT), participants were instructed to break their prolonged sitting time with light intensity walk breaks for 3 min every hour for the next 4 h. The participants walked at a self-selected ‘light’ velocity perception (Borg rate of perceived exertion score (RPE) of 11/20). (2) In moderate intensity breaks (MIT), the participants climbed two flights of stairs for 3 min every hour for the next 4 h of the prolonged sitting period. The participants self-selected their climbing speed to achieve a ‘somewhat difficult’ perception, according to the Borg RPE scores (RPE = 13/20). Walk-and-sir interventions were administered in the 30-m hallway and the stairway close to the ultrasound room where the study was conducted.
Outcomes
Carotid and superficial femoral artery function
On the basis of existing evidence, duplex ultrasound (GE Voluson Swift, Germany) at a pulsed frequency of 50 MHz was used to measure central (right carotid artery) and peripheral vascular (right superficial femoral artery) function (diameter and velocity), with the probe insonated at an angle of 60°.9,16,26, 27, 28 Edge detection software automatically measured the central and peripheral artery diameters and velocities with B Mode automated computer analysis. The shear stress and blood flow were estimated with the formulas 4 × [mean blood velocity/arterial diameter] and 3.14 × (diameter/2)2 × mean blood velocity × 60, respectively.29
Executive function
The Erikson Flanker paradigm was used to assess the response inhibition and executive function with computer-based software (Inquist 6.0, Millisecond Software, Seattle, WA, USA).30
In this computer-based Eriksen Flanker test, the participants were presented with five alphabets, H, K, S and C, on a laptop with Inquist 6.0 software.31 With the central alphabet as the target and the other alphabets on the sides as flankers, the participants were instructed to press either the Q or P buttons according to the H or K, and S or C alphabets displayed on the computer screen. The participants were presented with 120 trials (60 congruent and 60 incongruent). Each stimulus lasted 1500 ms, and was followed by an interval of 3000 ms before the next stimulus. After every 40 trials, the participants were given a 1-min break to recover from the stress of the continuous visual stimuli. The raw and summary files were exported from the software in CSV format. The reaction time (ms) and accuracy (%) were determined from the extracted CSV files.
Sample size
To establish a 43 ml/min difference in superficial femoral velocity with a moderate effect (Cohen's d = 0.52) between the SIT and LIT interventions, we determined that 18 participants would be required to achieve a 95% level of significance and 80% power. Because four experimental visits were conducted, and we anticipated a 20% dropout rate, we calculated that 21 participants would be necessary (G∗Power version 3.1.9.6, Universität Kiel, Germany).32
Randomisation and blinding
Computer-generated randomisation (www.randomiser.org) was used to determine the order of intervention visits (SIT, LIT and MIT). Volunteers were instructed to select one of the concealed envelopes which had randomly generated treatment orders, and this order was followed for subsequent visits. An experienced sonologist unaware of the study or randomisation assessed all vascular outcomes and provided the results in coded envelopes. The primary investigator opened the envelopes and decoded them at the time of analysis. However, the investigators assessing cognitive function and the final data compilation were not blinded to the order of the intervention visits.
Procedure
The interventions were performed in a temperature- and humidity-controlled ultrasound laboratory in a multifaceted teaching hospital. Participants who volunteered to participate in the study visited the laboratory four times on different days for familiarisation, then underwent three interventions: SIT, LIT and MIT. During the familiarisation visits, basic demographic and anthropometric data were collected, and participants were familiarised with vascular ultrasound, and walking or stair climbing for 3 min in the laboratory. Prospective sleep, physical activity and diet were measured for the next 7 days with a diary log. The participants were instructed to avoid smoking, alcohol and vigorous-intensity activities for at least 48 h before the intervention visits. The participants were assured of 8 h of adequate sleep, and the previous dinner was consumed between 8:00 PM and 9:00 PM, according to the sleep and diary log before each intervention visit. The order of the visits was determined according to computer-generated randomisation. A 6–7 day wash-out period was used to avoid the influence of one intervention over the other on the following days.
During the intervention period, participants were instructed to visit the laboratory between 8:00 AM and 9:00 AM, to avoid the influence of diurnal variation on vascular and cognitive function. To avoid vigorous activity during the commute, the participants were passively transported to the laboratory with a motor vehicle. After baseline measurements, the participants had a breakfast providing 33% of their daily requirements.33 During the SIT intervention visit, the participants were instructed to sit throughout the day for the next 4 h and were allowed to read or watch non-stimulating documentary films on the computer. The participants were not allowed to write or type, and avoided vigorous lower limb movements, as monitored by the observer throughout the sitting period. If washroom visits were necessary, the participants were passively transported to the washroom with a wheelchair led by the primary investigator. Ultrasound-based vascular assessments were administered every 2 h, and cognitive measurements were administered hourly. On the LIT intervention day, the participants interrupted their sitting time with light-intensity walking breaks for 3 min every hour for 4 h. During the MIT intervention visits, the participants were instructed to break their sitting time with 3 min of stair climbing at a self-selected velocity every hour for the next 4 h. The intervention visits were interspersed for 6–7 days to provide a wash-out.
Statistical analysis
Baseline demographics, regional vascular outcomes (diameter, velocity, shear and blood flow) and executive function (reaction time and accuracy) are expressed as mean ± standard error in normalised data or median ± interquartile range in skewed data. Skewed data were log-transformed as necessary.
The time course of the regional vascular outcomes (CA and SFA diameter, velocity, blood flow and shear rate) and comparisons among conditions (SIT, LIT and MIT) were analysed with linear mixed models. Each dependent variable (CA and SFA diameter, velocity, blood flow and shear rate) was analysed with linear mixed models, with time and condition as fixed effects and participants as random effects. Simple and interaction effects were analysed within and between experimental visits. Marginal means were estimated, and a post-hoc Holm test was used to correct the differences at each time point within the different conditions. Descriptive plots were drawn with time as the horizontal axis and groups as separate lines. The level of significance was set at p < 0.05. Multiple linear regression models were used to determine the association between carotid arterial and cognitive function. Statistical analysis was performed with the statistical software JASP (version 0.14.0; University of Amsterdam, Netherlands).
Results
Twenty-one participants completed all four experimental visits. Figure 2 shows the inclusion and the counterbalancing of the interventional visits.
Figure 2.
Flowchart demonstrating the screening, inclusion, randomisation, follow-up and analysis of the participants in the study.
Baseline characteristics
The mean BMI was 24.88 ± 3.50 (n = 19; 91%). The baseline characteristics are depicted in Table 1.
Table 1.
Baseline characteristics of the participants.
| Variables | Mean ± SD | n (%) | ||||
|---|---|---|---|---|---|---|
| Males | 17 (81%) | |||||
| Education | Undergraduate | 5 (29.41) | ||||
| Postgraduate | 16 (70.58) | |||||
| Overall |
Male |
Female |
p |
|||
| Age (years) | 26.65 ± 2.64 | 24.41 ± 3.84 | 27.82 ± 2.88 | 0.182 | ||
| Body mass index (kg/m2) | 22.32 ± 2.46 | 24.88 ± 3.50 | 21.83 ± 1.26 | 0.041∗ | ||
| Waist circumference (cm) | 97.32 ± 6.31 | 98.46 ± 8.31 | 96.54 ± 1.34 | 0.824 | ||
∗Significance shown by independent t test, p < 0.05.
Changes in regional vascular function with movement breaks
Central vascular function
The carotid artery diameter decreased by −5.45%, and the blood flow decreased by −7.84%, whereas carotid artery velocity and shear stress increased by 2.59% and 8.02%, respectively at the 2nd hour of SIT; however statistical significance was not reached. The LIT and MIT interventions had less pronounced effects on carotid vascular function (Table 2, Table 3). Supplementary file Figure S3 (a–d) illustrates the mean change in carotid artery function from baseline to the 2nd and 4th hour among three conditions: SIT, LIT and MIT.
Table 2.
Changes in central vascular endothelial function and executive function within conditions.
| Variable | Intervention [expressed as mean difference (standard error)] Δ |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| SIT |
LIT |
MIT |
|||||||
| T0 − T2 | T2 − T4 | T0 − T4 | T0 − T2 | T2 − T4 | T0 − T4 | T0 − T2 | T2 − T4 | T0 − T4 | |
| Central vascular function | |||||||||
| Carotid artery diameter (cm) | 0.03 (0.03) | −0.00 (0.03) | 0.03 (0.03) | 0.02 (0.03) | 0.00 (0.03) | 0.02 (0.03) | −0.02 (0.03) | 0.00 (0.03) | −0.01 (0.03) |
| Carotid artery velocity (cm/s) | −3.22 (5.64) | −1.63 (5.73) | −4.85 (5.73) | −2.84 (5.64) | −7.32 (5.73) | −5.54 (5.56) | 8.71 (5.64) | 1.65 (5.64) | 10.35 (5.64) |
| Carotid artery shear rate (/s) | −134.50 (112.90) | −1.32 (114.65) | −135.82 (114.65) | −66.73 (112.90) | −41.20 (111.32) | −107.93 (111.32) | 159.48 (112.90) | 14.91 (112.90) | 174.39 (112.90) |
| Carotid artery blood flow (ml/min) | 169.24 (204.86) | −48.45 (208.04) | 120.79 (208.04) | 43.25 (204.86) | −21.38 (202.00) | 21.88 (202.00) | 25.55 (204.86) | 36.76 (204.86) | 62.31 (204.86) |
| SFA diameter (cm) | 0.00 (0.04) | 0.01 (0.04) | 0.01 (0.04) | 0.02 (0.04) | 0.01 (0.04) | 0.03 (0.04) | −0.06 (0.04) | 0.05 (0.04) | −0.09 (0.04) |
| SFA velocity (cm/s) | 33.29 (17.85) | −1.86 (18.12) | 31.44 (18.12) | −2.02 (17.85) | −0.14 (17.60) | −2.16 (17.85) | 2.95 (17.85) | −0.86 (17.85) | 2.09 (17.85) |
| SFA shear rate (/s) | 382.66 (209.78) | −36.34 (213.04) | 397.01 (206.85) | −52.94 (209.74) | −10.75 (206.85) | −63.68 (206.85) | 112.84 (209.78) | 10.57 (209.78) | 123.41 (209.78) |
| SFA blood flow (ml/min) | 725.12 (442.90) | 5.84 (449.77) | 730.95 (449.77) | 66.38 (442.90) | 32.53 (436.71) | 98.91 (436.71) | −223.09 (442.90) | −142.22 (442.90) | −365.32 (442.90) |
| Executive function | |||||||||
| Reaction time (ms) | 111.14 (45.66)∗∗ | −30.70 (46.37) | 80.44 (46.37)∗ | 28.11 (45.66) | 22.89 (45.02) | 50.99 (45.02)∗ | 29.83 (45.66) | 24.31 (45.66) | 54.14 (45.66)∗ |
| Accuracy (%) | 7.37 (4.97)∗ | 4.39 (5.05) | 11.77 (5.05)∗ | 5.42 (4.97) | 3.14 (4.90) | 8.57 (4.90)∗ | 0.25 (4.97) | −2.93 (4.97)∗ | −2.67 (4.97) |
Abbreviations: LIT = sitting interrupted by light intensity activity, MIT = sitting interrupted by moderate intensity activity, SIT = uninterrupted sitting, T0 − T2 = difference in variables between baseline and the 2nd hour, T2 − T4 = difference in variables between the 2nd hour and 4th hour, T0 − T4 = difference in variables between baseline and the 4th hour, ‘−’ indicates the decrease with respect to earlier measurements, ‘+’ indicates the increase with respect to earlier measurements, Δ = mean change in the values calculated from analysis of variance, ∗p < 0.05, ∗∗p < 0.01.
Table 3.
Post hoc analysis comparing light intensity and moderate intensity microbreaks with sitting. All values are relative to prolonged sitting as the baseline.
| Variable | Group comparison |
Time comparison |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SIT vs LIT |
SIT vs MIT |
LIT vs MIT |
Baseline vs 2nd hour |
2nd hour vs 4th hour |
Baseline vs 4th hour |
|||||||||||||||||||
| Δ | 95% CI | d | p | Δ | 95% CI | d | p | Δ | 95% CI | d | p | Δ | 95% CI | d | p | Δ | 95% CI | d | p | Δ | 95% CI | d | p | |
| Vascular function | ||||||||||||||||||||||||
| Carotid artery diameter (cm) | −0.02 | −0.06, 0.012 | −0.304 | 0.380 | 0.00 | −0.03, 0.04 | 0.022 | 1.000 | 0.02 | −0.01, 0.06 | 0.327 | 0.304 | 0.01 | −0.03, 0.05 | 0.133 | 1.000 | 0.01 | −0.02, 0.05 | 0.159 | 1.000 | 0.00 | −0.03, 0.04 | 0.026 | 1.000 |
| Carotid artery velocity (cm/s) | 2.58 | −5.13, 10.30 | 0.157 | 0.858 | 4.80 | −2.95, 12.55 | 0.292 | 0.434 | 2.22 | −5.46, 9.89 | 0.135 | 0.858 | 0.88 | −6.83, 8.59 | 0.054 | 1.000 | −0.01 | −7.73, 7.70 | −0.007 | 1.000 | −0.89 | −8.61, 6.82 | −0.054 | 1.000 |
| Carotid artery shear rate (/s) | 94.08 | −60.38, 248.54 | 0.286 | 0.454 | 60.88 | −94.30, 216.05 | 0.185 | 0.709 | −33.20 | −186.85, 120.45 | −0.101 | 0.709 | −13.92 | −168.29, 140.45 | −0.042 | 1.000 | −23.12 | −177.58, 131.34 | −0.070 | 1.000 | −9.21 | −163.67, 145.25 | −0.028 | 1.000 |
| Carotid artery blood flow (ml/min) | −119.25 | −399.52, 161.02 | −0.200 | 0.631 | 111.58 | −169.98, 393.14 | 0.187 | 0.631 | 230.83 | −47.98, 509.64 | 0.386 | 0.156 | 79.35 | −200.76, 359.45 | 0.133 | 1.000 | 68.33 | −211.94, 348.59 | 0.114 | 1.000 | −11.02 | −291.29 | −0.018 | 1.000 |
| SFA diameter (cm) | −0.01 | −0.06, 0.04 | −0.056 | 0.777 | −0.04 | −0.09, 0.02 | −0.323 | 0.32 | −0.03 | −0.08, 0.02 | −0.267 | 0.356 | −0.014 | −0.064, 0.036 | −0.132 | 1.000 | −0.02 | −0.067, 0.033 | −0.160 | 1.000 | −0.003 | −0.05, 0.05 | −0.028 | 1.000 |
| SFA velocity (cm/s) | 14.21 | −10.20, 38.63 | 0.273 | 0.42 | 15.33 | −9.20, 39.86 | 0.295 | 0.42 | 1.12 | −23.17, 25.41 | 0.021 | 0.912 | 11.41 | −12.99, 35.81 | 0.219 | 0.810 | 10.46 | −13.96, 34.87 | 0.201 | 0.810 | −0.95 | −25.37, 23.46 | −0.018 | 0.927 |
| SFA shear rate (/s) | 178.83 | −108.17, 465.83 | 0.292 | 0.284 | 224.84 | −63.49, 513.16 | 0.368 | 0.201 | 46.01 | −239.49, 331.51 | 0.075 | 0.703 | 147.52 | −139.31, 434.35 | 0.241 | 0.676 | 135.35 | −151.65, 422.35 | 0.221 | 0.676 | −12.17 | −299.17, 274.83 | −0.020 | 0.920 |
| SFA blood flow (ml/min) | 255.99 | −349.93, 861.91 | 0.198 | 0.956 | 153.14 | −455.58, 761.85 | 0.119 | 1.000 | −102.85 | −705.61, 499.91 | −0.080 | 1.000 | 189.47 | −416.10, 795.04 | 0.147 | 1.000 | 154.85 | −451.07, 760.77 | 0.120 | 1.000 | −34.62 | −640.54, 571.30 | −0.027 | 1.000 |
| Executive function | ||||||||||||||||||||||||
| Reaction time (ms) | −110.6 | −173.06, −48.13 | −0.831 | <0.001∗∗∗ | −163.03 | −225.78, −100.27 | −1.225 | <0.001∗∗∗ | −52.43 | −114.57, 9.71 | −0.394 | 0.048∗ | 56.36 | −6.07, 118.79 | 0.423 | 0.068 | 61.86 | 0.61, 124.32 | 0.465 | 0.061 | 5.50 | −56.96, 67.96 | 0.041 | 0.835 |
| Accuracy (%) | −10.04 | −16.84, −3.24 | −0.693 | 0.002∗∗ | −8.87 | −15.70, −2.04 | −0.612 | 0.005∗∗ | 1.17 | −5.60, 7.94 | 0.081 | 0.682 | 4.35 | −2.45, 11.15 | 0.300 | 0.264 | 5.89 | −0.92, 12.69 | 0.406 | 0.127 | 1.54 | −5.26, 8.34 | 0.106 | 0.593 |
Abbreviations: LIT = sitting interrupted by light intensity activity, MIT = sitting interrupted by moderate intensity activity, SIT = uninterrupted sitting, T0 − T2 = difference in variables between baseline and the 2nd hour, T2 − T4 = difference in variables between the 2nd hour and 4th hour, T0 − T4 = difference in variables between baseline and the 4th hour, ‘−’ indicates the decrease with respect to earlier measurements, ‘+’ indicates the increase with respect to earlier measurements, Δ = mean change in the values calculated from analysis of variance, ∗p < 0.05, ∗∗p < 0.01.
Peripheral vascular function
We found no significant changes in SFA diameter, blood flow, velocity and shear stress from baseline to the 2nd hour of SIT. However, movement breaks during the LIT and MIT interventions mitigated arterial dysfunction during prolonged sitting. The LIT intervention resulted in non-significant changes in SFA function during the 2nd hour of sitting: SFA diameter −3.31%; SFA velocity, 2.86%; SFA shear stress, 6.15%; and SFA blood flow, −4.32% (Table 2, Table 3). Supplementary file Figure S3 (e–h) illustrates the mean change in SFA function from baseline to the 2nd and 4th hour among three conditions: SIT, LIT and MIT.
Cognitive function
Our study indicated significant interaction effects in executive function between groups and over time (Table 3). Reaction time decreased significantly during the first 2 h of prolonged sitting (−30.59%) but increased marginally during the second 2 h (7.79%). This decrease in reaction time was not observed with the LIT and MIT interventions. However, accuracy decreased significantly in the first 2 h of prolonged sitting (−10.56%) and continued to decrease in the next 2 h (−6.72%). This decrease in accuracy was only marginal on LIT and MIT intervention visit days (Table 2, Table 3 and Supplementary file S2). Supplementary file Figure S4 illustrates the changes in executive function between groups and times.
Association between carotid arterial function and executive function
No significant association was found in the changes observed in carotid artery function and executive function (reaction time and accuracy) during the three intervention visits: SIT, LIT, and MIT (Table 4).
Table 4.
Association between changes in carotid vascular function and executive function.
| Central vascular function | Intervention | Executive function (Eriksen Flanker paradigm) β (p) |
|||||
|---|---|---|---|---|---|---|---|
| Reaction time (ms) |
Accuracy (%) |
||||||
| SIT | LIT | MIT | SIT | LIT | MIT | ||
| Carotid artery diameter (cm) | SIT | 3.398 (0.194) | 2.200 (0.412) | ||||
| LIT | 1.895 (0.299) | 2.400 (0.186) | |||||
| MIT | −0.585 (0.737) | −0.173 (0.914) | |||||
| Carotid artery velocity (cm/s) | SIT | 8.535 (0.102) | 2.471 (0.547) | ||||
| LIT | 0.848 (0.735) | 2.216 (0.373) | |||||
| MIT | −1.889 (0.409) | 2.916 (0.177) | |||||
| Carotid artery shear rate (/s) | SIT | −3.391 (0.182) | −0.718 (0.706) | ||||
| LIT | 0.426 (0.830) | −0.533 (0.784) | |||||
| MIT | −0.860 (0.604) | −1.598 (0.304) | |||||
| Carotid artery blood flow (ml/min) | SIT | −7.283 (0.115) | −3.844 (0.371) | ||||
| LIT | −1.028 (0.500) | −1.650 (0.277) | |||||
| MIT | 1.952 (0.398) | −1.864 (0.382) | |||||
Note: Values are expressed as standardised association (β) and significance values (p) in parentheses. ‘p’ is set at a significance level of less than 0.5. Abbreviations: LIT = sitting interrupted by light intensity activity walk breaks, MIT = sitting interrupted by moderate intensity stair climbing breaks, SIT = uninterrupted sitting.
Discussion
Our randomised cross-over trial was aimed at exploring the vascular effects of varied intensity movement breaks during prolonged sitting in simulated work conditions. Although we observed central and peripheral vascular compromise with prolonged sitting, which was mitigated by movement breaks of light and moderate intensity, the observations did not reach statistical significance. Our study did not demonstrate significant positive vascular effects of interrupting sedentary behaviour in simulated work conditions. However, executive function was improved with interruption of prolonged sitting.
We found no significant differences in carotid vascular function during prolonged sitting or interruption with movement breaks of any intensity. Our findings concur with recent laboratory studies indicating no significant differences in carotid vascular function during prolonged sitting or interruption with physical activity breaks of varying intensity.34, 35, 36 Evans (2019) has concluded that intermittent calf raises do not alter aortic pulse wave velocity, whereas Wanders (2021) did not find any significant difference in carotid artery reactivity with moderate intensity cycling breaks for 5 min every 30 min with varied meal composition.35,36 Although empirical evidence has demonstrated an approximately 10% improvement in carotid artery diameter, approximately 50% carotid artery blood flow and decreased arterial stiffness after 12 weeks of aerobic or resistance training, our acute cross-over study did not indicate a significant difference in carotid artery diameter, blood flow, velocity and shear rate with acute movement breaks, even with moderate intensity, during prolonged sitting.37,38 However, the discordance in carotid vascular effects due to physical activity might also be due to inherent differences in carotid artery function observed in healthy adults.39
Because the lower limb arteries are prone to arterial stiffness and atherosclerosis pathology, experimental studies have administered behavioural interventions to mitigate lower limb vascular pathology in simulated work conditions.10,28,40 However, the findings from laboratory studies remain mixed.16,41 We did not observe significant adverse SFA arterial function during prolonged sitting visits or favourable SFA arterial outcomes with movement breaks of varied intensity during prolonged sitting. Although our findings were not statistically significant, prolonged sitting decreased the SFA diameter and flow. In contrast, moderate-intensity stair climbing breaks increased the SFA diameter and the blood flow in the lower limb arteries, in agreement with previous laboratory findings.10
Similarly, we did not find any significant differences in SFA velocity or shear stress during prolonged sitting or interruption with movement breaks of varied intensity, in agreement with several studies.10,42 We measured carotid and SFA arterial function before every movement break in the seated position to avoid transient vascular effects of physical activity, although heterogeneity in measurement has been observed across experimental studies, thus potentially explaining the non-significant findings in our study, as compared with other studies.26,43 Future studies should explore the long-term effects of these interruptions of varied intensity during prolonged sedentary periods in natural work conditions.
We found a statistically significant improvement in reaction time during the first 2 h of SIT compared with LIT and MIT interventions. The above finding contrasts with existing evidence indicating adverse effects on reaction time with prolonged sitting.8,44,45 Nonetheless, confounding factors such as race, heterogeneity in cognitive tests, social interaction and standardisation of diet and sleep should be considered.46, 47, 48 We observed a significant decrease in accuracy, particularly during the second 2 h of SIT, compared with LIT and MIT interventions. This finding has clinical relevance and public health importance, because existing evidence associates executive function with improved work productivity.
We did not find a significant relationship between the carotid artery and cognitive function. Although epidemiological studies have revealed a significant association between carotid artery function and cognitive function, our randomised cross-over study did not indicate any significant association.49,50
Limitations
(1) Our study explored only the acute effects of breaking periods of sitting with physical activity of varying intensity on vascular and cognitive function. The vascular and cognitive effects may vary according to real-world workplace conditions. Future studies should explore central and peripheral haemodynamics in real work-life scenarios in the long term. (2) The ultrasound laboratory where the study occurred could host three participants at a time. Although every attempt was made to minimise social interaction, the presence of peers or social support might have influenced the study results.51 (3) We used diary logs to assess baseline sleep, which may not be valid and might have influenced the results.47 Future trials should consider objective sleep measurement and the influence of physical activity on cognition.
Implications for practice
On the basis of the present study findings, periodic physical activity breaks might potentially improve executive function without compromising central or vascular function in workplaces. Because the modern workforce is at risk of high sedentary time and chronic disease risk, including cognitive dysfunction, the results of this study may be of value in formulating strong organisational policies advocating for movement breaks to support workers' health and promoting workforce sustainability.
Recommendations
Future studies should be undertaken by considering the following.
-
•
Long term effects of sedentary time interruptions on cognitive and vascular function in real life situations should be determined.
-
•
Diet, sleep and psychological wellbeing were not quantified but might have influenced the findings.
Conclusion
Physical activity breaks during prolonged sitting improved executive function but did not show any favourable effects on vascular function. Furthermore, our study did not demonstrate adverse vascular effects associated with prolonged sitting. During prolonged sitting, physical activity breaks may improve cognitive function without altering central or peripheral regional vascular dynamics.
Data availability
The dataset will be made available upon reasonable request to the corresponding author.
Disclosure statement
The authors declare that the secondary objective of the study (association between vascular and cognitive function) has been submitted to F1000 research and is under consideration (https://f1000research.com/articles/11-397). However, the primary objective regarding the difference in vascular and cognitive function with different movement breaks during prolonged sitting has not been submitted to any journal. Furthermore, all authors approved the final version of the manuscript. The authors also declare that if the article is accepted, it will not be published elsewhere by the authors, including electronically in the same form, in English or in any other language, without the written consent of the copyright-holder.
Source of funding
BC received a faculty seed grant supported by the Manipal Academy of Higher Education Faculty Seed grant (COAMA 369).
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This study was approved by the Institutional Ethics Committee (IEC 383/2021) on 20th August 2021 and was prospectively registered in the Clinical Registry of India (CTRI/2021/09/036496).
Authors contributions
BC and SS conceived and designed the study. BC received funding for this study. OC, SS and BC conducted the research, and collected and organised the data. OC, PS and BC analysed and interpreted the data. OC and RK wrote the initial and final drafts of the manuscript. CRR and KC provided critical input in the manuscript's current form. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The authors wish to thank the Manipal Academy of Higher Education for the support and necessary resources needed for the conduct of research. The authors also extend their thanks to the participants who spent their weekends supporting the data collection.
Footnotes
Study type: Randomised controlled trial.
Peer review under responsibility of Taibah University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtumed.2023.03.004.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Owen N., Sparling P.B., Healy G.N., Dunstan D.W., Matthews C.E. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010;85:1138–1141. doi: 10.4065/mcp.2010.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenkranz S.K., Mailey E.L., Umansky E., Rosenkranz R.R., Ablah E. Workplace sedentary behavior and productivity: a cross-sectional study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17186535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasheminasabgorji E., Jha J.C. Dyslipidemia, diabetes and atherosclerosis: role of inflammation and ros-redox-sensitive factors. Biomedicines. 2021;9 doi: 10.3390/biomedicines9111602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duvivier B., Bolijn J.E., Koster A., Schalkwijk C.G., Savelberg H., Schaper N.C. Reducing sitting time versus adding exercise: differential effects on biomarkers of endothelial dysfunction and metabolic risk. Sci Rep. 2018;8:8657. doi: 10.1038/s41598-018-26616-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grace M.S., Formosa M.F., Bozaoglu K., Bergouignan A., Brozynska M, Carey A.L., et al. Acute effects of active breaks during prolonged sitting on subcutaneous adipose tissue gene expression: an ancillary analysis of a randomised controlled trial. Sci Rep. 2019;9 doi: 10.1038/s41598-019-40490-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunstan D.W., Dogra S., Carter S.E., Owen N. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol. 2021;(18):637–648. doi: 10.1038/s41569-021-00547-y. [DOI] [PubMed] [Google Scholar]
- 8.Chandrasekaran B., Pesola A.J., Rao C.R., Arumugam A. Does breaking up prolonged sitting improve cognitive functions in sedentary adults? A mapping review and hypothesis formulation on the potential physiological mechanisms. BMC Muscoskel Disord. 2021;22 doi: 10.1186/s12891-021-04136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carter S.E., Draijer R., Holder S.M., Brown L., Thijssen D.H.J., Hopkins N.D. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J Appl Physiol. 2018;125:790–798. doi: 10.1152/japplphysiol.00310.2018. [DOI] [PubMed] [Google Scholar]
- 10.Carter S.E., Draijer R., Holder S.M., Brown L., Thijssen D.H.J., Hopkins N.D. Effect of different walking break strategies on superficial femoral artery endothelial function. Physiol Rep. 2019;7 doi: 10.14814/phy2.14190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wennberg P., Boraxbekk C.J., Wheeler M., Howard B., Dempsey P.C., Lambert G., et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-009630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tuckwell G.A., Vincent G.E., Gupta C.C., Ferguson S.A. Does breaking up sitting in office-based settings result in cognitive performance improvements which last throughout the day? A review of the evidence. Ind Health. 2022;60:501–513. doi: 10.2486/indhealth.2021-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell A., Grace F., Ritchie L., Beaumont A., Sculthorpe N. Long-term aerobic exercise improves vascular function into old age: a systematic review, meta-analysis and meta regression of observational and interventional studies. Front Physiol. 2019;10:31. doi: 10.3389/fphys.2019.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva J.K.T.N., Menêses A.L., Parmenter B.J., Ritti-Dias R.M., Farah B.Q. Effects of resistance training on endothelial function: a systematic review and meta-analysis. Atherosclerosis. 2021;333:91–99. doi: 10.1016/j.atherosclerosis.2021.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Whipple M.O., Masters K.S., Huebschmann A.G., Scalzo R.L., Reusch J.E., Bergouignan A., et al. Acute effects of sedentary breaks on vascular health in adults at risk for type 2 diabetes: a systematic review. Vasc Med. 2021;26:448–458. doi: 10.1177/1358863X211009307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paterson C., Fryer S., Zieff G., Stone K., Credeur D.P., Barone Gibbst B., et al. The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: a meta-analysis. Sports Med. 2020;50:1929–1942. doi: 10.1007/s40279-020-01325-5. [DOI] [PubMed] [Google Scholar]
- 17.Graham J.D., Bremer E., Fenesi B., Cairney J. Examining the acute effects of classroom-based physical activity breaks on executive functioning in 11- to 14-year-old children: single and additive moderation effects of physical fitness. Front Pediatr. 2021;9 doi: 10.3389/fped.2021.688251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benzing V., Chang Y.K., Schmidt M. Acute physical activity enhances executive functions in children with ADHD. Sci Rep. 2018;8 doi: 10.1038/s41598-018-30067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abubakar A.M., Elrehail H., Alatailat M.A., Elçi A. Knowledge management, decision-making style and organizational performance. J Innov Knowl. 2019;4:104–114. [Google Scholar]
- 20.Balconi M., Angioletti L., Crivelli D. Neuro-empowerment of executive functions in the workplace: the reason why. Front Psychol. 2020;11:1519. doi: 10.3389/fpsyg.2020.01519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alvarez-Bueno C., Cunha P.G., Martinez-Vizcaino V., Pozuelo-Carrascosa D.P., Visier-Alfonso M.E., Jimenez-Lopez E. Arterial stiffness and cognition among adults: a systematic review and meta-analysis of observational and longitudinal studies. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.014621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramírez-Vélez R., Hernández-Quiñones P.A., Tordecilla-Sanders A., Álvarez C., Ramírez-Campillo R., Izquierdot M., et al. Effectiveness of HIIT compared to moderate continuous training in improving vascular parameters in inactive adults. Lipids Health Dis. 2019;18:42. doi: 10.1186/s12944-019-0981-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho M.J., Bunsawat K., Kim H.J., Yoon E.S., Jae S.Y. The acute effects of interrupting prolonged sitting with stair climbing on vascular and metabolic function after a high-fat meal. Eur J Appl Physiol. 2020;120:829–839. doi: 10.1007/s00421-020-04321-9. [DOI] [PubMed] [Google Scholar]
- 24.Dwan K., Li T., Altman D.G., Elbourne D. Consort 2010 statement: extension to randomised crossover trials. BMJ. 2019;366:l4378. doi: 10.1136/bmj.l4378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shruthi P.P., Chandran M.O., Chandrasekaran B., Vaishali K., Sukumar S., Kadavigere R. Alteration in central vascular and cognitive functions during simulated work conditions in males – a secondary analysis from a randomised controlled trial [awaiting peer review] F1000Res. 2022;11:397. [Google Scholar]
- 26.Peddie M.C., Kessell C., Bergen T, Gibbons T.D., Campbell H.A., Cotter J.D., et al. The effects of prolonged sitting, prolonged standing, and activity breaks on vascular function, and postprandial glucose and insulin responses: a randomised crossover trial. PLoS One. 2021:16. doi: 10.1371/journal.pone.0244841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stoner L., Barone Gibbs B., Meyer M.L., Fryer S., Credeur D., Paterson C., Stone K., et al. A primer on repeated sitting exposure and the cardiovascular system: considerations for study design, analysis, interpretation, and translation. Front Cardiovasc Med. 2021;8:716938. doi: 10.3389/fcvm.2021.716938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thosar S.S., Bielko S.L., Mather K.J., Johnston J.D., Wallace J.P. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc. 2015;47:843–849. doi: 10.1249/MSS.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 29.Morishima T., Restaino R.M., Walsh L.K., Kanaley J.A., Padilla J. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci (Lond) 2017;131:1045–1053. doi: 10.1042/CS20170031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Juvonen K., Lapveteläinen A., Närväinen J., Absetz P., Kantanen T., Kolehmainen M., et al. Effect of metabolic state on implicit and explicit responses to food in young healthy females. Appetite. 2020;148:104593. doi: 10.1016/j.appet.2020.104593. [DOI] [PubMed] [Google Scholar]
- 31.Konijnenberg C., Fredriksen P.M. The effects of a school-based physical activity intervention programme on children's executive control: the health oriented pedagogical project (HOPP) Scand J Public Health. 2018;46:82–91. doi: 10.1177/1403494818767823. [DOI] [PubMed] [Google Scholar]
- 32.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using g∗power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 33.Howden J.A., Chong Y.H., Leung S.F., Rabuco L.B., Sakamoto M., Tchai B.S., et al. Breakfast practices in the Asian region. Asia Pac J Clin Nutr. 1993;2:77–84. [PubMed] [Google Scholar]
- 34.Kelsch E., Diana J.C., Burnet K., Hanson E.D., Fryer S.F., Credeur D.P., et al. Arterial stiffness responses to prolonged sitting combined with a high-glycemic-index meal: a double-blind, randomized crossover trial. J Appl Physiol (1985) 2021;131:229–237. doi: 10.1152/japplphysiol.00030.2021. [DOI] [PubMed] [Google Scholar]
- 35.Wanders L., Cuijpers I., Kessels R., van de Rest O., Hopman M., Thijssen D. Impact of prolonged sitting and physical activity breaks on cognitive performance, perceivable benefits, and cardiometabolic health in overweight/obese adults: the role of meal composition. Clin Nutr. 2021;40:2259–2269. doi: 10.1016/j.clnu.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Evans W.S., Stoner L., Willey Q., Kelsch E., Credeur D.P., Hanson E.D. Local exercise does not prevent the aortic stiffening response to acute prolonged sitting: a randomized crossover trial. J Appl Physiol (1985) 2019;127:781–787. doi: 10.1152/japplphysiol.00318.2019. [DOI] [PubMed] [Google Scholar]
- 37.Dinenno F.A., Tanaka H., Monahan K.D., Clevenger C.M., Eskurza I., DeSouza C.A., et al. Regular endurance exercise induces expansive arterial remodelling in the trained limbs of healthy men. J Physiol. 2001;534:287–295. doi: 10.1111/j.1469-7793.2001.00287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stebbings G.K., Morse C.I., McMahon G.E., Onambele G.L. Resting arterial diameter and blood flow changes with resistance training and detraining in healthy young individuals. J Athl Train. 2013;48:209–219. doi: 10.4085/1062-6050-48.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kadoglou N.P., Iliadis F., Liapis C.D. Exercise and carotid atherosclerosis. Eur J Vasc Endovasc Surg. 2008;35:264–272. doi: 10.1016/j.ejvs.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 40.Restaino R.M., Walsh L.K., Morishima T., Vranish J.R., Martinez-Lemus L.A., Fadel P.J., et al. Endothelial dysfunction following prolonged sitting is mediated by a reduction in shear stress. Am J Physiol Heart Circ Physiol. 2016;310:H648–H653. doi: 10.1152/ajpheart.00943.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taylor F.C., Pinto A.J., Maniar N., Dunstan D.W., Green D.J. The acute effects of prolonged uninterrupted sitting on vascular function: a systematic review and meta-analysis. Med Sci Sports Exerc. 2022;54:67–76. doi: 10.1249/MSS.0000000000002763. [DOI] [PubMed] [Google Scholar]
- 42.Taylor F.C., Dunstan D.W., Homer A.R., Dempsey P.C., Kingwell B.A., Climie R.E., et al. Acute effects of interrupting prolonged sitting on vascular function in type 2 diabetes. Am J Physiol Heart Circ Physiol. 2021;320:H393–H403. doi: 10.1152/ajpheart.00422.2020. [DOI] [PubMed] [Google Scholar]
- 43.McManus A.M., Ainslie P.N., Green D.J., Simair R.G., Smith K., Lewis N. Impact of prolonged sitting on vascular function in young girls. Exp Physiol. 2015;100:1379–1387. doi: 10.1113/EP085355. [DOI] [PubMed] [Google Scholar]
- 44.Chrismas B.C.R., Taylor L., Cherif A., Sayegh S., Bailey D.P. Breaking up prolonged sitting with moderate-intensity walking improves attention and executive function in Qatari females. PLoS One. 2019;14 doi: 10.1371/journal.pone.0219565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhat M., Dehury K., Chandrasekaran B., Palanisamy H.P., Arumugam A. Does standing alter reaction times and event related potentials compared to sitting in young adults? A counterbalanced, crossover trial. Theor Issues Ergon Sci. 2022:1–24. [Google Scholar]
- 46.Waongenngarm P., Rajaratnam B.S., Janwantanakul P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. J Phys Ther Sci. 2015;27:2183–2187. doi: 10.1589/jpts.27.2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vincent G.E., Jay S.M., Sargent C., Kovac K., Vandelanotte C., Ridgers N.D., et al. The impact of breaking up prolonged sitting on glucose metabolism and cognitive function when sleep is restricted. Neurobiol Sleep Circadian Rhythms. 2018;4:17–23. doi: 10.1016/j.nbscr.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dewitt S, Hall J, Smith L, Buckley JP, Biddle SJH, Mansfield L, et al. Office workers’ experiences of attempts to reduce sitting-time: an exploratory, mixed-methods uncontrolled intervention pilot study. BMC Public Health. 2019;19:819. doi: 10.1186/s12889-019-7196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pucite E., Krievina I., Miglane E., Erts R., Krievins D. Influence of severe carotid stenosis on cognition, depressive symptoms and quality of life. Clin Pract Epidemiol Ment Health. 2017;13:168–180. doi: 10.2174/1745017901713010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yue W., Wang A., Zhu R., Yan Z., Zheng S., Wang J., et al. Association between carotid artery stenosis and cognitive impairment in stroke patients: a cross-sectional study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0146890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gallagher S., Creaven A.M., Howard S., Ginty A.T., Whittaker A.C. Gratitude, social support and cardiovascular reactivity to acute psychological stress. Biol Psychol. 2021;162 doi: 10.1016/j.biopsycho.2021.108090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset will be made available upon reasonable request to the corresponding author.