ABSTRACT
Objectives:
To uncover numerous post-COVID symptoms in individuals after SARS-CoV-2 infection and to raise concerns about the consequences for health care planning.
Methodology:
Patients declared negative with RTPCR and discharged from the hospital were followed up for three months.
Results:
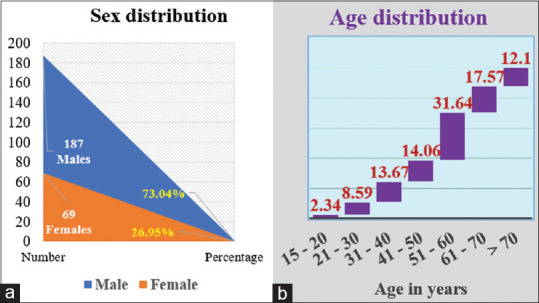
The majority of patients who suffered from weakness since discharge are 63 (25.40%), body aches 40 (16.12%), loss of taste 26 (10.48%), and loss of smell 18 (7.25%). The total of reinfected patients in the 4th week was 9 (3.62%), in the 6th week 10 (4.03%), in the 8th week 7 (2.82%), and in the 12th week 11 (4.43%). A total of 54.7% of individuals still have the persistence of symptoms at the end of the 12th week.
Conclusions:
A significant number of participants developed long-term health issues as a result of post-COVID-19 syndrome. Our findings highlight the importance of initial preventive measures and patient-centered benefit programs in reducing post-COVID-19 complications.
Keywords: Long-haul COVID, post-COVID symptoms, post-COVID syndrome, SARS-CoV-2 infection
Introduction
The coronavirus disease 2019 (COVID-19) initially appeared in December 2019 in China and turned into a global emergency in a short time of its outbreak due to a beta coronavirus called severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2).[1] WHO declared COVID-19 as a pandemic because of its aggressive spreading nature.[2] Multiple system involvement is the primary reason for most of the complications of COVID-19.[3] To minimize the adverse consequences of COVID-19, the uninterrupted scrutiny of SARS-CoV-2 symptomatology is needed as it has an unsteady character of RNA viruses.[4,5] After recovering from the initial infection from COVID-19, throughout the world, many people have been presenting with symptoms like chronic fever, myalgia, fatigue, confused brain, tachycardia, breathlessness, loss of appetite-smell-taste, pain in the chest, has led to several panic attacks, diarrhea, insomnia, headaches, and sore throat.[2] Some experienced ringing in the ears and dramatic mood swings. All these post-COVID-19 symptoms are otherwise called long-haul COVID, long COVID, or post-COVID syndrome. Perego coined the term “long COVID” to describe symptoms that lasted weeks or months after early SARS-CoV-2 infection, while Watson and Yong coined the term “long haulers.”[5-7] Regardless of viral status, the existence of various symptoms spanning weeks or months, relapsing and remitting, as well as the onset of new symptoms, characterizes the post-COVID syndrome.[8,9] Approximately 80% of people affected had mild to moderate disease, while 5% of those with severe disease developed critical illness.[1] Most patients with post-COVID syndrome test negative for RT-PCR, implying that they have recovered microbiologically. Most individuals with long haulers recover microbiologically, biochemically, and radiologically indicating that there is a time lag between diagnostic and symptomatic recovery.[10] Post-COVID or long COVID can be split up into two stages based on the duration of symptoms: (1) post-acute COVID (symptoms lasting more than 3 weeks and far less than 12 weeks) and (2) chronic COVID (symptoms lasting more than 12 weeks).[11] There are no FDA-approved treatments for post-COVID syndrome, but experts opine those patients with post-viral syndrome can get better with time. Close monitoring of the post-COVID-19 persistent symptoms can help in establishing the possible relationship between chronic inflammatory symptoms and COVID-19. Long-term implications of COVID-19 and the drugs used in its treatment may constrain the natural immune system and its responses. This may lead to reinfection with COVID-19, reactivation of other latent diseases, and worsening of pre-existing diseases. Hence there is a need for documentation of the spectrum of persistent post-COVID symptoms.
The main aim of our study is to identify and enumerate the symptoms that linger even after recovery from corona infection. There is a lack of consolidated study data on post-COVID-19 symptoms from central India, and to the best of our knowledge, no scientific study was undertaken in the state of Chhattisgarh. We will be assessing persistent symptoms in patients who recovered and were discharged from the hospital.
Methodology
Study design
A prospective observational questionnaire-based pilot study was conducted on the discharged COVID-19 patients by the Department of Pharmacology, All India Institute of Medical Sciences (AIIMS), at Raipur during the stipulated time. The COVID-19 recovered patients who were confirmed microbiologically negative with RTPCR, from AIIMS Raipur, were included in the study. The written informed consent was obtained from the patients while getting discharged from the hospital.
Questionnaire survey and validation
Based on COVID-symptoms-related research publications that sought information during and after COVID-19 acute infection,[12-16] a semi-structured survey was made to prepare a questionnaire. Based on the survey results, a questionnaire has been developed for use in pilot research to identify post-COVID symptoms during a three-month follow-up period. The questionnaire was validated by 30 participants who had COVID-19 and were in the recovery phase. The pilot study enabled the identification of new questions to assess systemic compromise, as well as the structuring and modification of queries to ensure their interpretability by the respondent. After validation was completed and IEC approval was acquired (AIIMSRPR/IEC/2020/698), a prospective cohort questionnaire-based study was conducted.
Questionnaire distribution and data collection
A total of 28 questions were included in the structured survey and system-wise distributed in the following areas: cardiovascular; pulmonary; musculoskeletal; gastrointestinal; neuropsychological; ear, nose, throat, and sensual organs. A telephonic interview was conducted every week in the first month and thereafter every 15 days for up to three months.
Study objectives
The primary objective was to identify the post-COVID-19 symptoms and their duration in discharged patients in AIIMS Raipur.
The secondary objectives were to collect the demographic profile of post-COVID-19 patients; to verify if any recurrence of symptoms similar to COVID-19 occurs within three months of follow-up, and to find out any further health problems experienced in post-COVID-19 patients that are not mentioned in the questionnaire.
Eligibility criteria
The following criteria were included: (a) Patients in the age group of more than 15 years who recovered and were discharged as per existing guidelines during the study period; b) those who were willing, and co-operative was enrolled, after obtaining duly signed informed consent forms; c) RTPCR COVID-19 (positive) patients discharged with negative PCR report was included in the study as RTPCR is considered a gold standard and specific for COVID-19 confirmation.
Exclusion criteria
Patients with any of the following criteria were excluded from the study: (a) Those who were tested COVID positive based on antigen and NAAT tests were not included in the study as there is a higher chance of false-positive reporting; (b) those who are less than 15 years of age; (c) patients on anti-psychotic medication; d) patients with organ failure – (i) congestive heart failure, New York Heart Association types 3 & 4, (ii) end-stage liver disease, (iii) chronic obstructive pulmonary disease, (iv) chronic kidney disease stage 4 and 5, (v) sickle cell disease.
Data analysis
All the information was exported to an excel spreadsheet. We considered a P value of 0.05 as statistically significant. As a result, the data gathered has been evaluated for definitive remarks. We employed the Chi-squared method for categorical data.
Results
In our study, 300 people were enrolled, and they were discharged from the AIIMS, Raipur, with RTPCR COVID negative results between February 16 and May 15, 2021. Contact information was available for 300 people, 44 of whom were eliminated according to the criteria.
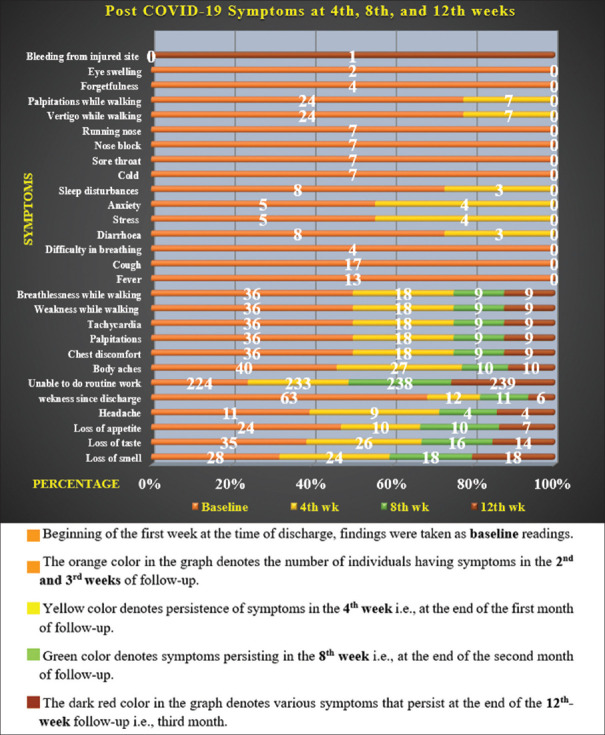
The ages ranged from 15 to 86 years old, as per the results. The males outnumbered the females by a margin of 74% (187) to 27% (69) [Figure 1]. Eight people died during the post-COVID follow-up period. As a consequence, the data of 248 individuals were analyzed [Figure 2]. 9 patients, 7 patients, and 11 patients were reinfected at the fourth, eighth, and twelfth weeks of the 12-week follow-up, respectively. The COVID-19 patients admitted to AIIMS, Raipur, their post-COVID status and follow-up, as well as their age, gender, and highest age group involved, are all listed in Figure 1a and 1b.
Figure 1.
Figures depicting the gender distribution and the highest age group involved. (a) A graph illustrating the distribution of sex. (b) A graph representing the distribution of age
Figure 2.
A graph demonstrating the presence of various post-COVID symptoms over time
The symptoms that were observed as chronic COVID symptoms lasting more than 12 weeks for the whole three-month follow-up period are listed in Table 1.
Table 1.
Persistence of chronic Post-COVID symptoms (present more than 12 weeks)
| Symptoms | Yes/no | Baselinevreadings | 4th WK. | 8th WK. | 12th WK. | P |
|---|---|---|---|---|---|---|
| Loss of smell (LOS) | Y | 28 | 24 | 18 | 18 | 0.309111 |
| N | 220 | 224 | 230 | 230 | ||
| Loss of taste (LOT) | Y | 35 | 26 | 16 | 14 | 0.003369# |
| N | 213 | 222 | 232 | 234 | ||
| Loss of appetite (LOA) | Y | 24 | 10 | 10 | 7 | 0.002354# |
| N | 224 | 238 | 238 | 241 | ||
| Headache (HE) | Y | 11 | 9 | 4 | 4 | 0.13357 |
| N | 237 | 239 | 244 | 244 | ||
| Weakness since discharge (WN) | Y | 63 | 12 | 11 | 6 | <0.00001# |
| N | 185 | 236 | 237 | 242 | ||
| Able to do routine work as before admission (RW) | Y | 24 | 15 | 10 | 9 | 0.015974# |
| N | 224 | 233 | 238 | 239 | ||
| Body aches (BACH) | Y | 40 | 27 | 10 | 10 | <0.00001# |
| N | 208 | 221 | 238 | 238 | ||
| Chest discomfort (CD) | Y | 36 | 18 | 9 | 9 | <0.00001# |
| N | 212 | 230 | 239 | 239 | ||
| Palpitations (PAL) | Y | 36 | 18 | 9 | 9 | <0.00001# |
| N | 212 | 230 | 239 | 239 | ||
| Tachycardia (TAC) | Y | 36 | 18 | 9 | 9 | <0.00001# |
| N | 212 | 230 | 239 | 239 | ||
| While walking weakness (W-W) | Y | 36 | 18 | 9 | 9 | <0.00001# |
| N | 212 | 230 | 239 | 239 | ||
| While walking breathlessness (W-B) | Y | 36 | 18 | 9 | 9 | <0.00001# |
| N | 212 | 230 | 239 | 239 |
#P value showing significant
In the current study, it was observed that by the end of the third week, symptoms such as fever, cough, difficulty breathing, cold, sore throat, nasal block, and running nose had gradually subsided in most participants. Few symptoms in our study were categorized under post-acute COVID symptoms depending on the duration of persistence of symptoms in individuals [Figure 3]. During the three-month follow-up period, no one in our study sample complained of constipation or mood swings. Two people reported new symptoms such as left eye puffiness, and four people reported forgetfulness, while one person complained of non-stop bleeding at the site of injury.
Figure 3.
Depicts a case of post-acute COVID (symptoms lasting in between 3 weeks and 12 weeks)
Discussion
Main sequels of the current survey
Our findings revealed that a significant proportion of patients infected with SARS-CoV-2 have a “post-COVID syndrome.” As per our findings, patients have not fully recovered even after 12 weeks and individuals have continued to suffer from loss of smell, loss of taste, loss of appetite, headache, weakness since hospital discharge, inability to perform routine tasks, body aches, chest discomfort, palpitations, tachycardia, weakness while walking, and breathlessness. However, the majority of patients who had not recovered from their infirmity and wanted to know their current state need additional follow-up. Some people have multiple symptoms. This study found that a significant number of patients had a clinical spectrum after recovering from SARS-CoV-2 infection, impairing their quality of life and necessitating an interdisciplinary treatment.
Evidence in context
Post-COVID-19 syndrome is described by the National Institute for Health and Care Excellence (NICE) guidelines as signs and symptoms that appear during or after COVID-19 infection and that last for more than 12 weeks.[4] Prior research has found that individuals with COVID-19 had broad symptoms that lasted up to six months following SARS-CoV-2 infection.[17,18,19,20,21,22,23,24,25,26,27,28,29,30,31] Furthermore, case reports of three women after three months of COVID infection noted temporary hair loss and telogen effluvium.[32] Numerous case studies even more than eight months have revealed chronic fatigue, dyspnoea, shortness of breath, chest pains, headache, loss of smell or taste, myalgia, psychological disorders, dermatitis, palpitations, tachycardia, anorexia, tingling palms, and foggy brain in COVID-affected individuals.[33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] Considering the overall picture of extensive long-term symptoms reported in this survey, persistent fatigue or weakness is the most common complaint. This is consistent with a previous study that found high levels of post-infectious fatigue among victims of outbreaks like severe acute respiratory distress syndrome (SARS) and Ebolavirus.[49,50] According to the findings of this study, a large percentage of patients present with a clinical spectrum after recovering from COVID-19 infection, impairing their quality of life and necessitating a multidisciplinary treatment. The etiology of long COVID is unknown, although the most common hypotheses are a chronic inflammatory process, an autoimmune condition, or a hormonal imbalance caused by a change in the hypothalamic-pituitary-adrenal axis.[51] A survey on COVID-19 patients after three to six months of recuperation revealed that patients with post-COVID syndrome have high levels of CD8+ T cells, CD27IgDB cells (which is associated with autoimmune disorders such as multiple sclerosis),[52] and higher production of Th1 and Th17 cytokines, promoting a hyperinflammatory environment. Tumor necrosis factor (TNF), interleukin (IL-1ß) levels, increased endothelial activation, and pro-inflammatory mediators were found to be high in convalescent patient’s incomparable research.[53,54] Although the persisting viral gene fragments are not infectious, they may nevertheless cause a strong immunological overreaction, which could explain the persistence of symptoms in COVID-19-free patients.[55] A better understanding of elements such as the complete spectrum of SARS CoV-2-related diseases and their extending effects; underlying correlations between viral spreading; variations of viral load during SARS CoV-2 infection and long COVID phase, fluctuating pro-inflammatory mediators, pathogenesis, and the impact of antiviral drugs could help researchers to gain knowledge about the reasons of long-term illnesses, as well as the immune system’s role and the potential of transmission.
Home message for primary health care professionals
This dataset could help clinicians remember what to expect during the post-COVID period and be better prepared to manage post-COVID symptoms in recovered patients. Close monitoring in the post-COVID period may also aid in assessing immune health, pathophysiology, vulnerable groups, COVID recurrence patterns, and providing advice on cures and strategies to deal with mild post-COVID symptoms at the household level. To better understand the incidence, clinical spectrum, pathophysiology, and prognosis of this unique clinical entity, more research is needed. To summarize, the full range of the duration and severity of post-acute COVID-19 is yet unknown. These data suggest the importance of a proactive approach to the management of this high-risk population in order to fully understand the new “post-COVID syndrome” and create the conceptual model for conducting therapeutic intervention trials and establishing prospective follow-up programs. Our population-based cohort analysis found that a significant proportion of COVID-19-affected people had long-term repercussions.
Conclusion
Since SARS-CoV-2 infection is still in its early stages, it is impossible to predict its long-term prognosis. However, to overlook the hidden “iceberg” of long COVID, further timely planning of resources, multidisciplinary approaches such as patient-centered and health care services are essential. Our population-based cohort analysis found that a significant proportion of COVID-affected people had long-term repercussions. And it emphasizes the need for the high demand for additional follow-ups and medical services at primary care centers for those individuals suffering from post- COVID-19 syndrome. As a result, conducting similar surveys or therapeutic intervention studies, as well as developing future follow-up plans, is crucial in addressing all global health concerns and illuminating the way for the betterment of public health.
Limitations
It was a one-center study. A telephonic interview was used to follow up with patients. As a result, an accurate evaluation of the patient’s quality of life was impossible. In addition, patients’ follow-up time was restricted to three months. To establish a strong relationship, a larger sample size is required. Another drawback is the lack of published evidence from long-term follow-up COVID-19 registries across the country. Furthermore, the material in this page about the clinical spectrum of post-COVID syndrome is based on current findings but may be expanded if more data becomes available in the future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Consent for publication
This manuscript is original and has not been published before and is not currently being considered for publication elsewhere.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to acknowledge Dr. Suryaprakash Dhaneria Sir for his constant support and valuable guidance.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–42. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: Prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudre C, Lee K, Lochlainn M, Varsavsky T, Murray B, Graham MS, et al. Symptom clusters in covid 19: A potential clinical prediction tool from the COVID Symptom study app. Sci Adv. 2021;7:eabd4177. doi: 10.1126/sciadv.abd4177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Who-China Joint Mission Members. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). World Health Organization. 2020 [Google Scholar]
- 5.Perego E. Twitter 20 May. 2020. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7539940/
- 6.Edwards E. COVID-19 “long-haulers” report nearly 100 symptoms for more than 100 days NBC News 2020. Available from: https://www.nbcnews.com/health/health-news/covid-19-long-haulers-report-nearly-100-symptoms-more-100-n1235217 .
- 7.Yong E. COVID-19 can last for several months. The Atlantic. 2020. Available from: https://www.newscientist.com/article/mg24632881-400-why-strange-and-debilitating-coronavirus-symptoms-can-last-for-months/
- 8.Geddes L. Why strange and debilitating coronavirus symptoms can last for months. New Sci. 2020. Available from: https://www.newscientist.com/article/mg24632881-400-why-strange-and-debilitatingcoronavirus-symptoms-can-last-formonths/
- 9.Nikki N. Long covid: How to define it and how to manage it. BMJ. 2020;370 doi: 10.1136/bmj.m3489. doi: 10.1136/bmj.m3489.m3489. [DOI] [PubMed] [Google Scholar]
- 10.Garg P, Arora U, Kumar A, Wig N. The “post-COVID” syndrome: How deep is the damage? J Med Virol. 2021;93:673–4. doi: 10.1002/jmv.26465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 12.Vicente Herrero MT, Delgado Bueno S, Bandrés Moyá F, Ramírez Iñiguez de la Torre MV, Capdevila García L. Valoración del dolor. Revisión Comparativa de Escalas y Cuestionarios. Rev Soc Esp Dolor. 2018 doi: 10.20986/resed.2018.3632/2017. [Google Scholar]
- 13.GeCo Group. Italy: Politec Di Milan; 2020. Towards a Cooperative Construction of Questionnaires for Covid-19 Host Genetics Initiative. [Google Scholar]
- 14.Guler SA, Ebner L, Aubry-Beigelman C, Bridevaux P-O, Brutsche M, Clarenbach C, et al. Pulmonary function and radiological features 4 months after COVID-19: First results from the national perspective observational Swiss COVID-19 lung study. Eur Respir J. 2021;57 doi: 10.1183/13993003.03690-2020. doi: 10.1183/13993003.03690-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zung WWK. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 16.Cirulli ET, Schiabor Barrett KM, Riffle S, Bolze A, Neveux I, Dabe S, et al. Longterm COVID-19 symptoms in a large unselected population. MedRxiv. 2020 doi: 10.1101/2020.10.07.20208702. [Google Scholar]
- 17.Arnold DT, Hamilton FW, Milne A. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: Results from a prospective UK cohort. Thorax. 2021;76:399–401. doi: 10.1136/thoraxjnl-2020-216086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen KY, Li T, Gong FH, Zhang JS, Li XK. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a followup at one month. Front Psychiatry. 2020;11:668. doi: 10.3389/fpsyt.2020.00668. doi: 10.3389/fpsyt 2020.00668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post-COVID-19 manifestations. Int J Clin Pract. 2021;75:e13746. doi: 10.1111/ijcp.13746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Del Rio C, Collins LF, Malani P. Long-term health consequences of COVID- 19. JAMA. 2020;324:1723–24. doi: 10.1001/jama.2020.19719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayes JP. Considering the long-term respiratory effects of Covid-19. Occup Med. 2021;671:325–7. doi: 10.1093/occmed/kqaa224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iacobucci G. Long covid: Damage to multiple organs presents in young, low risk patients. BMJ. 2020;371:m4470. [Google Scholar]
- 23.Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Developing services for long COVID: Lessons from a study of wounded healers. Clin Med. 2021;21:59–65. doi: 10.7861/clinmed.2020-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manolis AS, Manolis TA. Long COVID: An emerging puzzle. Rhythmos. 2021;16:89–94. [Google Scholar]
- 25.Mendelson M, Nel J, Blumberg L, Madhi SA, Dryden M, Stevens W, et al. Long-COVID: An evolving problem with an extensive impact. S Afr Med J. 2020;111:10–2. doi: 10.7196/SAMJ.2020.v111i11.15433. [DOI] [PubMed] [Google Scholar]
- 26.Nikhra V. Living with ‘Long COVID-19’ : The long-term complications and sequelae. Int J Clin Virol. 2021;5:011–7. [Google Scholar]
- 27.Outhoff K. Sick and tired of COVID-19: Long haulers and post viral (fatigue) syndromes. S Afr Gen Pract. 20201:132–4. [Google Scholar]
- 28.Saigal A, Naidu SB, Shah AJ, Brill SE, Jarvis H, Goldring JG, et al. S54 ‘long- COVID’ : The need for multi-disciplinary working. Thorax. 2021;76:A33–4. [Google Scholar]
- 29.Simani L, Ramezani M, Darazam IA, Sagharichi M, Aalipour MA, Ghorbani F, et al. Prevalence and correlates of chronic fatigue syndrome and posttraumatic stress disorder after the outbreak of the COVID-19. J Neurovirol. 2021;27:154–9. doi: 10.1007/s13365-021-00949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yong SJ. Long-haul COVID-19: Putative pathophysiology, risk factors, and treatments. Preprints. 2020 doi: 10.1080/23744235.2021.1924397. 2020120242. doi: 10.1080/23744235.2021.1924397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zapatero DC, Hanquet G, Van Den Heede K. Epidemiology of Long Covid: A Pragmatic Review of the Literature. Available from: https://kce.fgov.be/sites/default/files/2021-11/2020-04HSR_LongCOVID_COVID%20Contributions_01022021.pdf .
- 32.Saeed W, Hussain I, Altaf F. Telogen effluvium: Long term Covid-19 symptom. J Pakistan Assoc Dermatol. 2020;30:700–3. [Google Scholar]
- 33.Abdallah H, Porterfield F, Fajgenbaum D. Symptomatic relapse and longterm sequelae of COVID-19 in a previously healthy 30-year-old man. BMJ Case Rep. 2020;13:e239825. doi: 10.1136/bcr-2020-239825. doi: 10.1136/bcr-2020-239825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buselli R, Corsi M, Necciari G, Pistolesi P, Baldanzi S, Chiumiento M, et al. Sudden and persistent dysphonia within the framework of COVID-19: The case report of a nurse. Brain Behav Immun Health. 2020;9:100160. doi: 10.1016/j.bbih.2020.100160. doi: 10.1016/j.bbih.2020.100160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D'Cruz RF, Waller MD, Perrin F, Periselneris J, Norton S, Smith LJ, et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID- 19 pneumonia. ERJ Open Res. 2021;7 doi: 10.1183/23120541.00655-2020. doi: 10.1183/23120541.00655-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15:e0243882. doi: 10.1371/journal.pone.0243882. doi: 10.1371/journal.pone. 0243882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al. ‘Long-COVID’ : A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76:396–8. doi: 10.1136/thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sofian M, Velayati AA, Banifazl M, Fotouhi F, Sadat Larijani M, Afzali N, et al. SARS-CoV2, a virus with many faces: A series of cases with prolonged persistence of COVID-19 symptoms. Wien Med Wochenschr. 2021;171:3–6. doi: 10.1007/s10354-020-00793-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stavem K, Ghanima W, Olsen MK, Gilboe HM, Einvik G. Persistent symptoms 1.5-6 months after COVID-19 in nonhospitalised subjects: A population-based cohort study. Thorax. 2021;76:405–7. doi: 10.1136/thoraxjnl-2020-216377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, Gaffney F, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020;15:e0240784. doi: 10.1371/journal.pone.0240784. doi: 10.1371/journal.pone. 0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Varghese J, Sandmann S, Vollenberg R, Ochs K, Schrempf I, Froemmel C, et al. Follow up of COVID-19 features in recovered adults without comorbidities-persistent symptoms and lab-abnormalities. Res Square. doi: 10.21203/rs. 3.rs-116030/v1. [Google Scholar]
- 42.Davido B, Seang S, Tubiana R, de Truchis P. Post-COVID-19 chronic symptoms: A postinfectious entity? Clin Microbiol Infect. 2020;26:1448–9. doi: 10.1016/j.cmi.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miglis MG, Goodman BP, Chémali KR, Stiles L. Re: ‘Post-COVID-19 chronic symptoms’ by Davido et al. Clin Microbiol Infect. 2020;27:494. doi: 10.1016/j.cmi.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yelin D, Wirtheim E, Vetter P, Kalil AC, Bruchfeld J, Runold M, et al. Longterm consequences of COVID-19: Research needs. Lancet Infect Dis. 2020;20:1115–7. doi: 10.1016/S1473-3099(20)30701-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams FMK, Muirhead N, Pariante C. Covid-19 and chronic fatigue. BMJ. 2020;370:m2922. doi: 10.1136/bmj.m2922. [DOI] [PubMed] [Google Scholar]
- 46.Nehme M, Braillard O, Alcoba G, Aebischer Perone S, Courvoisier D, Chappuis F, et al. COVID-19 symptoms: Longitudinal evolution and persistence in outpatient settings. Ann Intern Med. 2020;8:723–5. doi: 10.7326/M20-5926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zuin M, Rigatelli G, Zuliani G, Roncon L. Fatigue as long-term consequence of ARDS in COVID-19 patients. Anaesth Crit Care Pain Med. doi: 10.1016/j.accpm.2020.10.016. 202026: 100787. doi: 10.1016/j.accpm.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bliddal S, Banasik K, Pedersen OB, Nissen I, Cantwell L, Schwinn M, et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. medRxiv [Preprint. 2021 doi: 10.1038/s41598-021-92045-x. doi: 10.1101/2021.01.22.21249945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome;a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilson HW, Amo-Addae M, Kenu E, Ilesanmi OS, Ameme DK, Sackey SO. Post-ebola syndrome among Ebola virus disease survivors in Montserrado County, Liberia (2016) Biomed Res Int 2018. 2018 doi: 10.1155/2018/1909410. 1909410. doi: 10.1155/2018/1909410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fraussen J, Marquez S, Takata K, Beckers L, Montes Diaz G, Zografou C, et al. Phenotypic and Ig repertoire analyses indicate a common origin of IgD, CD27, double negative B cells in healthy individuals and multiple sclerosis patients. J Immunol. 2019;203:1650–64. doi: 10.4049/jimmunol.1801236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Talla A, Vasaikar SV, Lemos MP, Moodie Z, Pebworth M-PL, Henderson KE, et al. Longitudinal immune dynamics of mild COVID-19 define signatures of recovery and persistence. BioRxiv. 2021 doi: 10.1101/2021.05.26.442666. [Google Scholar]
- 54.Ong SWX, Fong S-W, Young BE, Chan Y-H, Lee B, Amrun SN, et al. Persistent symptoms and association with inflammatory cytokine signatures in recovered coronavirus disease 2019 patients. Open Forum Infect Dis. 2021;8 doi: 10.1093/ofid/ofab156. doi: 10.1093/ofid/ofab156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.British Society for Immunology. Long-Term Immunological Health Consequences of COVID-19. Available from: https://www.immunology. org/sites/default/files/BSI_Briefing_Note_August_2020_FINAL.pdf .