ABSTRACT
Bee sting can lead to allergic reactions which can present as life-threatening emergencies. Kounis syndrome is an acute coronary syndrome caused by mast cell activation after exposure to an allergen. Atrial fibrillation (AF) along with Kounis syndrome after allergen exposure is a rare presentation. A 40-year-old male patient presented to the emergency department (ED) with multiple bee stings to the face and neck. He complained of retrosternal chest pain along with facial pain and swelling. An electrocardiogram (ECG) showed AF with ST elevation in aVR and generalized ST segment depression. Troponin levels were elevated. He was diagnosed with Kounis syndrome along with AF secondary to a bee sting. The patient improved symptomatically with removal of stings and conservative management (steroids, antihistamines, antiplatelet drugs). ECG reverted to sinus rhythm and resolution of ST-T changes. He was discharged from the ED in stable condition. The bee sting may lead to significant cardiovascular events such as AF and Kounis syndrome, which require a high index of suspicion and prompt treatment. Kounis syndrome should be suspected in the ED in young patients with no cardiovascular risk factors after exposure to an allergen.
Keywords: Atrial fibrillation, bee sting, Kounis syndrome
Introduction
Allergic reactions from bee stings have various manifestations from itching to life-threatening anaphylaxis. Rarely, organ systems can be involved. Acute coronary syndrome secondary to allergen exposure, known as Kounis syndrome, needs timely diagnosis and emergent treatment. Primary health care professionals have an important role in early identification, initial treatment and timely referral of this condition. Kounis syndrome is an uncommon entity with less than 100 cases reported but is suspected to be more common and frequently overlooked.[1] We present a rare case of Kounis syndrome and atrial fibrillation (AF) following a bee sting.
Case Report
A 40-year-old male patient with nil comorbidities presented to the emergency department (ED) with complaints of multiple bee stings to the face and neck 1 h ago. The patient was working on his farm when 30–40 bees attacked him. He had an episode of syncope lasting for 2 min after the sting. He complained of retrosternal chest pain along with facial pain and swelling [Figure 1].
Figure 1.

Facial swelling after a bee sting
On examination, his heart rate was 120/min, blood pressure 92/40 mmHg, respiratory rate 24/min and room air saturation 98%. The patient had 15–20 bee stings on his face and neck which were removed. An electrocardiogram (ECG) showed AF with ST elevation in aVR and generalized ST segment depression [Figure 2a]. Troponin level was 0.07 ng/mL which rose to 0.42 ng/mL after 3 h. Since the patient had no previous comorbidities, he was diagnosed with Kounis syndrome along with AF secondary to a bee sting. The patient was administered intravenous fluids, hydrocortisone and histamine blockers along with aspirin, clopidogrel and enoxaparin. Epinephrine was deferred as it would cause further cardiac ischaemia. He did not consent to coronary angiography.
Figure 2.
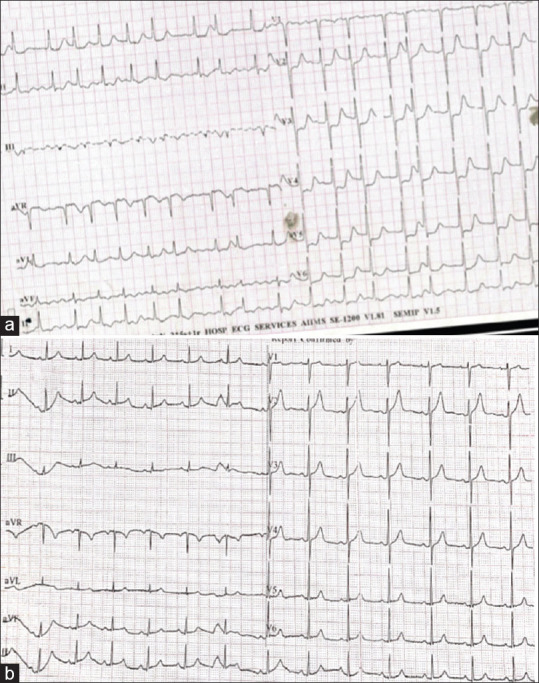
Images (a): Initial ECG showing atrial fibrillation with ST elevation in aVR and generalized ST segment depression. (b) Normalization of ECG changes after treatment
The patient improved symptomatically, and ECG showed sinus rhythm and resolution of ST-T changes [Figure 2b]. He was discharged home with antihistamine and steroids and advised follow-up for allergy work-up. The patient is asymptomatic at a one-month follow-up.
Discussion
Bee stings are known to cause allergic reactions and anaphylaxis and may affect organ systems. The various clinical manifestations are due to the content of bee venom – histamine, melittin, dopamine, norepinephrine, phospholipase A2, leukotrienes and thromboxanes.[2] Cardiovascular system involvement in the form of angina, acute coronary syndrome, bradycardia, trifascicular block, atrial flutter has been reported.[2] AF with an acute coronary syndrome, present in our patient, is a rare complication of a bee sting and only a few cases have been reported in the literature.[3]
Kounis syndrome, defined as an acute coronary syndrome caused by mast cell activation, was seen in our patient secondary to a bee sting.[4] Other commonly implicated agents are drugs, chemicals and environmental exposures like fire ant stings, wasp stings, scorpion stings, snake bites, poison ivy and latex contact.[5] Three variants of this syndrome have been described. Type I is ‘allergic angina’ in patients with no predisposing cardiac risk factors as in this patient. They have normal coronary arteries on angiography. The allergen results in coronary artery spasms with or without elevation of cardiac biomarkers. Type II is ‘allergic myocardial infarction’ in patients with pre-existing atheromatous coronary arteries. The allergen results in plaque erosion or rupture, which leads to myocardial infarction. Type III is ‘stent thrombosis’ caused by an allergic reaction.[6] Our patient most probably had type I Kounis syndrome as he did not have any cardiac risk factors.
Patients with a bee sting and clinical symptoms usually present to the nearest primary care physician. Our patient directly presented to a tertiary care centre as it was close by, but this may not always be the case. Hence, it is important for all primary physicians to identify the condition early, provide primary care promptly and refer to a higher centre in a timely fashion. Kounis syndrome is diagnosed based on history, physical examination, laboratory and electrocardiographic findings. Serum tryptase, histamine and cardiac enzymes like troponins are elevated. It has been suggested to measure troponin in all patients with allergic reactions to timely diagnose cardiac events manifesting as Kounis syndrome.[7] Echocardiography and angiography help in diagnosing wall abnormalities and coronary vessel anatomy.[8] Prompt ECG and troponin helped us diagnose and manage this condition timely.
Treatment of Kounis syndrome comprises of removal of the offending agent, aborting the allergic reaction and coronary perfusion restoration. Prompt removal of the offending agent decreases further exposure to the allergen. Allergic treatment consists of corticosteroids, antihistamines and epinephrine. Epinephrine must be used with caution as it can cause coronary vasospasm and worsen coronary ischaemia.[4] Coronary reperfusion includes vasodilators like nitrates and calcium channel blockers in the type I variant as vasospasm is the pathogenesis.[9] Type II and III variants require coronary interventions for plaque rupture and thrombosis formation.[10] Morphine can cause histamine release and should be avoided. Beta-blockers cause unopposed coronary vasospasm and make epinephrine ineffective, requiring glucagon for beta-blockade reversal. Suspicion of Kounis syndrome should be considered in all young, healthy patients with no cardiac risk factors developing acute coronary events.[9] Primary care providers being adept with the early recognition, initial management and appropriate referral can play a pivotal role in the outcome of patients with Kounis syndrome. Our patient improved with antiallergic medications and did not require vasodilators or coronary interventions. Detailed allergy work-up should be done on these patients. Our patient was advised to follow up in the allergy clinic.
Conclusion
The bee sting may lead to significant cardiovascular events such as AF and Kounis syndrome, which require a high index of suspicion and prompt treatment. Kounis syndrome should be suspected in young patients with no cardiovascular risk factors developing acute coronary events after exposure to an allergen.
Key points
Bee sting allergy may manifest in a wide spectrum, ranging from itching to life-threatening anaphylaxis. Acute coronary syndrome caused by mast cell activation is known as Kounis syndrome.
Treatment of Kounis syndrome involves removal of the offending agent, aborting the allergic reaction and coronary perfusion restoration.
Epinephrine should be used with caution; morphine and beta-blockers should be avoided.
Kounis syndrome requires early identification, prompt initial care and timely referral.
Author’s contribution list
Authors BG and RN managed the case on the floor under the supervision of ME. GK followed up the case and helped in obtaining the images of the case. All authors have contributed to the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kadeli D, Mangesh D, Keshava R, Gopi A. Kounis syndrome:Allergic myocardial infarction!! J Indian Coll Cardiol. 2019;9:108. [Google Scholar]
- 2.Gupta PN, Kumar BK, Velappan P, Sudheer MD. Possible complication of bee stings and a review of the cardiac effects of bee stings. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2015-213974. doi:10.1136/bcr-2015-213974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sahinkus S, Demirel S. 74.eestings and a review of. Atrial fibrillation due to bee sting. J Clin Toxicol. 2017;7:361. [Google Scholar]
- 4.Kounis NG. Coronary hypersensitivity disorder:The Kounis syndrome. Clin Ther. 2013;35:563–71. doi: 10.1016/j.clinthera.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction):A natural paradigm? Int J Cardiol. 2006;110:7–14. doi: 10.1016/j.ijcard.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Memon S, Chhabra L, Masrur S, Parker MW. Allergic acute coronary syndrome (Kounis syndrome) Proc Bayl Univ Med Cent. 2015;28:358–62. doi: 10.1080/08998280.2015.11929274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lippi G, Buonocore R, Schirosa F, Cervellin G. Cardiac troponin I is increased in patients admitted to the emergency department with severe allergic reactions. A case-control study. Int J Cardiol. 2015;194:68–9. doi: 10.1016/j.ijcard.2015.05.093. [DOI] [PubMed] [Google Scholar]
- 8.Kounis NG. Natural Paradigm:Kounis is llin G. Cardiac troponin IaKounis NG. Natural Par. Ach Iatrike. 2016;35:16–21. [Google Scholar]
- 9.Cevik C, Nugent K, Shome GP, Kounis NG. Treatment of Kounis syndrome. Int J Cardiol. 2010;143:223–6. doi: 10.1016/j.ijcard.2010.02.040. [DOI] [PubMed] [Google Scholar]
- 10.Sebaldt RJ, Sheller JR, Oates JA, Roberts LJ, FitzGerald GA. Inhibition of eicosanoid biosynthesis by glucocorticoids in humans. Proc Natl Acad Sci U S A. 1990;87:6974–8. doi: 10.1073/pnas.87.18.6974. [DOI] [PMC free article] [PubMed] [Google Scholar]


