ABSTRACT
Background:
Cancer is often detected much later to its onset, resulting in poor prognosis. This makes cancer the second most common cause of death globally. Looking for cancers much before any symptoms occur is termed “cancer screening” and is a powerful strategy for prevention, early diagnosis, and better management of several cancers. This paper examines the status of cancer screening in India from the National Family Health Survey (NFHS)-5 report for the period of 2019–2021.
Methods:
Secondary data on participation in screening for cervical, breast, and oral cancer were extracted from the NFHS-5 report. Participation status for all the above cancer types is represented as percentages and compared across 28 states and eight union territories in India.
Results:
The percentages of women who have ever undergone cervical, breast, and oral cavity screening were 1.9%, 0.9%, and 0.9%, respectively. About 1.2% of men participated in oral cavity screening. The highest percentage of cervical and breast cancer screening participation was reported in Tamil Nadu (9.8% and 5.6%, respectively), followed by Puducherry (7.4% and 4.2%) and Mizoram (6.9% and 2.7%). Andaman and Nicobar Islands reported the highest oral cancer screening among women (10.1%) while Andhra Pradesh (6.3%) reported the highest participation among men.
Conclusion:
Cancer screening participation in India is extremely inadequate and calls for the immediate attention of national and state governments. Additional efforts are warranted to improve public awareness of cancer screening, and appropriate measures should be implemented to conduct well-organized screening programs across the country to ensure maximum participation.
Keywords: Cancer screening, India, National Family Health Survey, prevention and control
Introduction
The worldwide cancer burden will likely approach 27 million new cancer cases by 2040, up from 18.1 million cancer cases estimated in 2018, with a significant contribution from countries with low and medium Human Development Index (HDI).[1] Population growth, aging, and changes in the prevalence of risk factors contribute to this increasing burden of cancer.[1,2,3] Under the framework of a collective and integrated motion of prevention strategies, the World Health Assembly (WHA) prompts the governments and the World Health Organization (WHO) to hasten efforts to ensure healthy lives and promote well-being for all. It is hoped that, by the year 2030, these efforts and initiatives will reduce the number of premature deaths due to any noncommunicable diseases, which includes cancer, by one-third.[4]
India accounts for 1,324,413 new cases and 8,51,678 deaths attributed to cancer in 2020. Breast, oral cavity, and cervix-uteri are the first, second, and third most common sites of cancers among both sexes and all ages, contributing to about 4,38,197 cases in India.[5] As per the report of the National Cancer Registry Programme (2012–2016) in India, Hyderabad district ranked top in breast cancer incidence (age-adjusted rate [ASR]: 48.0/100,000) and Papumpare district in West Arunachal Pradesh rated first in cervical cancer incidence (ASR: 27.7/100,000). Breast cancer incidence was lowest in Meghalaya (ASR: 7/100,000) and cervical cancer incidence was lowest in the Dibrugarh district in Assam (ASR: 4.8/100,000). Papumpare district in Arunachal Pradesh had the highest incidence rate of head and neck cancers (21.7/100,000) in females. Among males, the East Khasi Hills district in Meghalaya had the highest head and neck cancer incidence (ASR: 78.5/100,000) and the lowest in Barshi rural registry in Maharashtra (ASR: 10.6/100,000).[6]
Cost-effective screening approaches to reduce breast, cervical, and oral cancer mortality and morbidity are well established globally.[7,8,9] The precancerous lesions can be detected early by visual examination of the oral cavity during general health check-ups or screening by doctors/dentists/health professionals or through self-examination.[8,9] For the prevention and early detection of cervical cancer, interventions range from prophylactic human papilloma virus (HPV) vaccines to various screening approaches such as visual inspection with acetic acid or Lugol’s iodine (VIA/VILI), Papanicolaou test (Pap test or Pap smear), and HPV DNA testing (deoxyribose nucleic acid).[7,9] Clinical Breast Examination (CBE) by trained health workers is a low-cost breast cancer screening method for low- and middle-income countries. Given the late stage of diagnosis, average tumor size upon detection, and socioeconomic realities of a developing nation like India, CBE may be a pragmatic method for baseline breast cancer screening.[7,9]
As part of the Ayushman Bharat Comprehensive Primary Health Care Programme and the National Programme for Prevention and Control of Cardiovascular Disease, Diabetes, Cancer and Stroke (NPCDCS), India proposed a plan for launching a national cancer screening program in 2016.[9,10] Population-based screening for cervical, breast, and oral cancers is being implemented under the National Health Mission (NHM) as part of comprehensive care, complementing the NPCDCS.[9] The National Family Health Surveys (NFHS-5), for the first time, provide information on oral, breast, and cervical cancer screening in all states and union territories (UT) in India. Presently, this is the only source to evaluate the utilization of population-based cancer screening implemented under the NPCDCS, thus helping to understand the gap between implementation and utilization of cancer screening in India. This paper looks into the current status of cancer screening attendance in all states and UTs in India, which may help to improvise strategies for the early detection and prevention efforts in a country that contributes largely to the global burden of cancer.
Material and Methods
Study setting
The NFHS in India are coordinated by the International Institute for Population Sciences (IIPS) in Mumbai and supervised by the Ministry of Health and Family Welfare of the Government of India.
Study duration
The fifth round of National Family Health Survey (NFHS-5) was conducted from June 17, 2019 to January 30, 2021.[11] For the present paper, we extracted the data from the NFHS fact sheets and analyzed during February–March, 2022.
Study design
The NFHS survey used a two-stage sampling design for both rural and urban areas. The survey covered women and men aged 15–49 and 15–54 years, respectively, and gathered information on fertility, infant and child mortality, reproductive health, etc. We did secondary data analysis for the present paper.
Sample size and sampling
NFHS-5 report provided information on screening participation for the first time, to our knowledge, in India among adults aged 30–49 years. The information on the proportion of women who have ever undergone screening for cervical, breast, and oral cancer and men who have ever experienced screening for oral cancer in 28 states and eight UTs were gathered from the NFHS factsheets.[11] Hence, for the present study, we used the aggregated data on the proportions of screening participation in 28 states and eight UTs for rural, urban, and total, respectively.
Data collection
The first author extracted the data from the NFHS fact sheets and the extracted information was stored as Microsoft Excel sheets, and a descriptive analysis was done using STATA SE 17.0. (Texas, USA).
Data analysis
The median and range of the proportions for rural, urban, and the combined population were described. The states with the highest percentage of cervical and breast cancer screening participation in the first five positions were listed and compared between rural and urban areas. We also assessed a male-female variation in oral cancer screening participation between the states and UTs.
Ethical issues
Since the present paper is based on extracted information from a public domain report, no ethical concerns are raised.
Results
Cancer screening participation in India
The women who have ever undergone cervical cancer screening in India were 1.9%, ranging from 0.2% in Gujarat, Assam, and West Bengal to 9.8% in Tamil Nadu. Half of the states or UTs had screening participation of less than 1%. Women who have ever undergone a breast examination for breast cancer detection in India were only 0.9%. The highest percentage of women screened for breast cancer was in Tamil Nadu (5.6%), and none were screened in Chandigarh.
The ever participation in oral cancer screening among women was 0.9%, and it ranged from 0.2% in Gujarat, Jharkhand, Assam, Chhattisgarh, Rajasthan, West Bengal, and Ladakh to 10.1% in Andaman and Nicobar Islands. The ever participation in oral cancer screening was 1.2% among men, and the highest was recorded in Andhra Pradesh (6.3%) while the lowest was in Lakshadweep and Ladakh (0%) [Table 1].
Table 1.
Cancer screening participation in India
| Urban (%) | Rural (%) | Total (%) | |
|---|---|---|---|
| Ever undergone a screening test for cervical cancer. | |||
| India | 2.2 | 1.7 | 1.9 |
| Among states or UTs | |||
| Median | 1.1 | 0.6 | 0.8 |
| Min-Max | 0.1-10 | 0-12.6 | 0.2-9.8 |
| Ever undergone a breast examination for breast cancer | |||
| India | 1.2 | 0.7 | 0.9 |
| Among states or UTs | |||
| Median | 0.4 | 0.3 | 0.3 |
| Min-Max | 0.0-5.9 | 0.0-5.3 | 0.0-5.6 |
| Ever undergone an oral cavity examination for oral cancer (women) | |||
| India | 1.2 | 0.8 | 0.9 |
| Among states or UTs | |||
| Median | 0.6 | 0.2 | 0.5 |
| Min-Max | 0.0-10 | 0.1-0.6 | 0.2-10.1 |
| Ever undergone an oral cavity examination for oral cancer (men) | |||
| India | 1 | 1.3 | 1.2 |
| Among states or UTs | |||
| Median | 0.6 | 0.8 | 0.9 |
| Min-Max | 0.0-7.3 | 0.0-5.9 | 0.0-6.3 |
Screening participation: States or UTs in the first five positions
Figures 1 and 2 represent the states or UTs in top five positions with the highest percentage of women who participated in cervical and breast cancer screening. Tamil Nadu recorded the highest participation compared with the rest of the states and UTs in India, followed by Puducherry. The cervical screening was higher in rural areas of Puducherry than in urban areas, whereas in Mizoram, cervical screening participation in urban areas was higher compared with rural areas. The variation between rural-urban regions in other states or UTs, including Tamil Nadu, was minimal [Figure 1]. Tamil Nadu, Puducherry, Mizoram, and Kerala were among the first five states with the highest percentage of screening for breast and cervical cancer. However, in Andhra Pradesh, though cervical screening participation was 4.7%, breast cancer screening was only among 0.8% of women. The rural-urban difference in breast cancer screening was minimal in all states [Figure 2].
Figure 1.
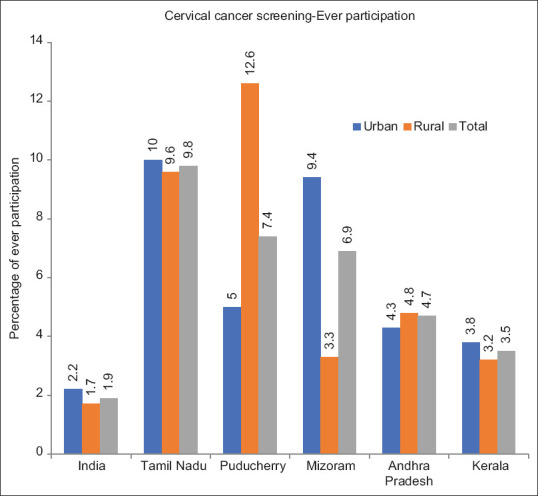
Percentage of women ever participated in cervical cancer screening: States or UTs in the first five positions
Figure 2.
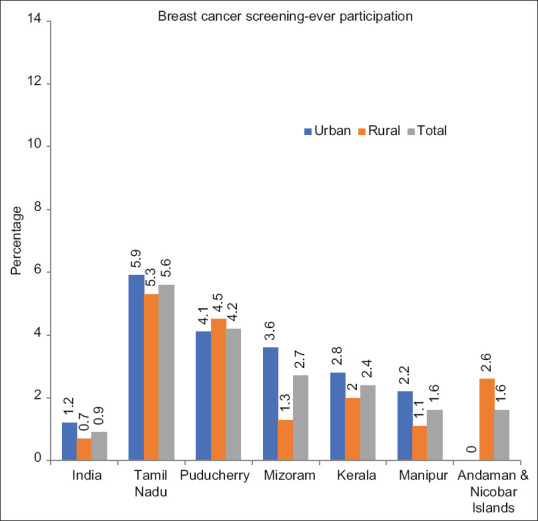
Percentage of women ever participated in breast cancer screening: States or UTs in the first five positions
There was no considerable rural-urban variation among males and females for oral cancer. The five states with the highest percentage of oral cancer screening among males were Andhra Pradesh, Sikkim, Andaman and Nicobar Islands, Telangana, and Chandigarh, and among females, Andaman and Nicobar Islands, Andhra Pradesh, Telangana, Puducherry, and Maharashtra. The notable contribution of Tamil Nadu in cervical and breast cancer screening was not there for oral cancer screening. There was a considerable male-female variation in the participation of oral cancer screening in Andaman and Nicobar Island [Figure 3].
Figure 3.
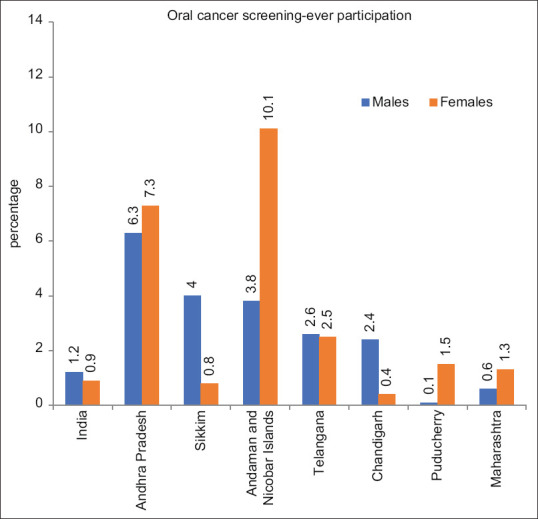
Comparison among women and men who have ever participated in oral cancer screening: five states or UTs in the first five positions in percentage
Discussion
Screening participation in India
Major observation from this study is that the proportion of women and men who have ever undergone screening for cervical, breast, and oral cancer was only nearly 1% in India, which shows the inadequacy of cancer screening status in India. Additional efforts are necessary to appropriately implement NPCDCS guidelines for screening eligible men and women for different cancers in all states and UTs in India.
Tamil Nadu makes a slightly more significant contribution to cervical and breast cancer screening than other parts of India. In 2005, the Tamil Nadu Health Systems Project (TNHSP) under the Government of Tamil Nadu initiated World Bank-funded noncommunicable disease (NCD) intervention program in all districts. Opportunistic screening for cancer of the cervix and breast among women aged 30 and above was one of the program’s mandates.[12] This could account for a slightly higher percentage of women screened for cervical and breast cancer in Tamil Nadu. Puducherry is a Union Territory with four small geographically unconnected districts within Tamil Nadu, Andhra Pradesh, and Kerala. The highest proportion of women ever screened for cervical cancer was observed in rural Puducherry, and a substantial difference was observed between rural and urban areas of Puducherry.
The highest percentage of oral cancer screening was recorded among women in Andaman and Nicobar Islands (10.1%). The opportunistic population-based screening was implemented in Andaman and Nicobar Islands under the NPCDCS program with Accredited Social Health Activist (ASHA) and Auxiliary Nurse Midwife (ANM) and subsequently managed by medical officers.[13] However, the male-female difference in oral cancer screening participation is a question that needs to be addressed appropriately for a better implementation of the screening program. The small sample size for males in the Andaman and Nicobar Islands also can be a reason for showing such a difference between males and females.
There are many states and UTs with no women or men who have ever participated in screening. For example, in Chandigarh, no women were screened for breast cancer while in Ladakh and Lakshadweep, no men were screened for oral cancer. Also, we found that screening participation was scarce in places where cancer burden is very high. For instance, cervical screening participation (0.8%) was meager in Arunachal Pradesh, where an increased incidence of cervical cancer (ASR of 27.7/100,000) was observed in the Papumpare Registry in the state. Breast cancer screening was minimal in Andhra Pradesh, where the incidence of breast cancer reported was 48 per 100,000 in the Hyderabad Registry. Similarly, the East Khasi Hills district in Meghalaya had the highest incidence rate of head and neck cancers (78.5/100,000) in men. In contrast, oral cancer screening coverage was only 1.2% in the state.[9,11]
NFHS-5 report reveals that screening guidelines of NPCDCS have not been appropriately utilized and effectively implemented anywhere in India.[14] It is crucial to identify if there is a lack of integration of program activities at the health system level, and necessary steps to overcome the situation are urgently warranted. In addition, lack of knowledge about cancer screening, socioeconomic disparities, and social stigma associated with acceptance of screening are to be addressed appropriately. Educational interventions and awareness programs for the public, and adequate training for healthcare professionals regarding cancer screening and prevention at the primary and community health centers, along with infrastructure and human resource development, are essential for effective implementation of population-wide screening in India.[7,15,16] Social media platforms can be a powerful means to spread awareness about cancer screening, early detection, and prevention on a large scale. They can also help to motivate people from general negligence of health issues.[17]
Strength and limitations
The accessibility of cancer screening data in NFHS-5 allows us to evaluate the levels and patterns of screening for breast, oral, and cervical cancer across India. Some states/UTs had small sample sizes, which may affect the estimation of proportions (Chandigarh, Lakshadweep, Goa, Ladakh, and Andaman and Nicobar Islands, etc). However, this is the first time we have national data available to assess screening participation in India. NFHS-4 collected information from 15- to 49-year-old women who have ever undergone examinations of the cervix, breast, and oral cavity and reported proportions were 22.3%, 9.8%, and 12.4%, respectively. However, these examinations were never mentioned to be intended for cancer screening and could be for other general examinations such as dental caries (oral cavity), menstrual abnormalities (cervix), etc., In NFHS-5, data on 30–49 years old adults who specifically attended a screening for the three cancers were presented. Also, screening status in the previous round was provided as “nil” in NFHS-5.[11,18] So, a comparison of the proportions cannot be made. Moreover, limiting the data on the proportion of people who have ever participated in screening would not reflect the comprehensive status of cancer screening. It is ideal to have more detailed sections on the number of times each person has been screened, the time gap between each screening, and the outcome of screening, such as screen positivity, diagnostic confirmation, follow-up details, etc., in the upcoming NFHS surveys.
Conclusion
In conclusion, NFHS-5 data demonstrate that the screening coverage is next to nothing in India, regardless of several schemes, programs, and facilities. This has severe implications, as India contributes majorly to cancer worldwide, and if implemented effectively, population-wide screening can substantially bring down the burden of cancer incidence. Screening is only effective when available and being utilized by the public, and hence NPCDCS must be strengthened nationwide.
Key message
NFHS-5 data demonstrate that the screening coverage is next to nothing in India, regardless of several schemes, programs, and facilities. Screening is only effective when available and being utilized by the public, and hence NPCDCS must be strengthened nationwide to reduce the cancer burden in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wild C, Weiderpass E, Stewart BW, editors. World Cancer Report:Cancer Research for Cancer Prevention. IARC Press; 2020. [Last accessed on 2022 Apr 30]. Available from:https://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report -Cancer-Research-For-Cancer- Prevention-2020 . [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer:Priorities for prevention. J Carcinog. 2010;31:100–10. doi: 10.1093/carcin/bgp263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Cancer prevention and control in the context of an integrated approach. [Last accessed on 2022 Apr 25];World Health Assembly Resolution WHA70. 2017 12 Available from:https://apps.who.int/iris/handle/10665/275676 . [Google Scholar]
- 5.International Agency for Research on Cancer. [Last accessed on 2022 Apr 18];Globocan. 2020 Available from:https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf . [Google Scholar]
- 6. [Last accessed on 2022 Apr 18];Report of National Cancer Registry Programme (ICMR-NCDIR). Bengaluru, India. 2020 Available from:https://www.ncdirindia.org/All_Reports/Report_2020/default.aspx . [Google Scholar]
- 7.Mishra R. An epidemiological study of cervical and breast screening in India:District-level analysis. BMC Women's Health. 2020;20:1–5. doi: 10.1186/s12905-020-01083-6. doi:10.1186/s12905-020-01083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irani S. New insights into oral cancer-Risk factors and prevention:A review of literature. Int J Prev Med. 2020;11:202. doi: 10.4103/ijpvm.IJPVM_403_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bharat A. New Delhi: MoHFW, Government of India; 2018. [Last accessed on 2022 Apr 24]. Comprehensive Primary Health Care through Health and Wellness Centers:Operational Guidelines. Available from:https://www.nhm.gov.in/New_Updates_2018/NHM_Components/Health_System_Stregthening/Comprehensive_primary_health_care/letter/Operational_Guidelines_For_CPHC.pdf . [Google Scholar]
- 10.Bagcchi S. India launches plan for national cancer screening programme. BMJ. 2016;355:i5574. doi: 10.1136/bmj.i5574. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health and Family Welfare. [Last accessed on 2022 Feb 22];Key indicators National Family Health Survey (NHFS-5) 2019-20. 2021 Available from:http://rchiips.org/nfhs/factsheet_NFHS-5.shtml . [Google Scholar]
- 12. [Last accessed on 2022 Apr 19];Cervical cancer prevention screening and treatment A pilot initiative of Tamil Nadu health system project. Available from:https://darpg.gov.in/sites/default/files/57-Cervical-Cancer-Screening-Programme.pdf . [Google Scholar]
- 13. [Last accessed on 2022 Apr 19];Directorate of health services-Andaman and Nicobar Islands, NPCDS. Available from:https://dhs.andaman.gov.in/NPCDCS.aspx . [Google Scholar]
- 14.Subba SH. Too little too late?Or a small step in the right direction?-Cancer screening in India. Indian J Community Fam Med. 2021;7:71–3. [Google Scholar]
- 15.Sahu DP, Subba SH, Giri PP. Cancer awareness and attitude towards cancer screening in India:A narrative review. J Family Med Prim Care. 2020;9:2214–18. doi: 10.4103/jfmpc.jfmpc_145_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shanker N, Mathur P, Das P, Sathishkumar K, Shalini AM, Chaturvedi M. Cancer scenario in North-East India &need for an appropriate research agenda. Indian J Med Res. 2021;154:27. doi: 10.4103/ijmr.IJMR_347_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Negi J, Nambiar D. Intersectional social-economic inequalities in breast cancer screening in India:Analysis of the National Family Health Survey. BMC Women's Health. 2021;21:1–9. doi: 10.1186/s12905-021-01464-5. doi:10.1186/s12905-021-01464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. [Last accessed on 2022 Apr 19];Ministry of Health and Family Welfare. Key indicators National Family Health Survey (NHFS-4) 2015-16. Available from:http://rchiips.org/nfhs/factsheet_NFHS-4.shtml . [Google Scholar]


