ABSTRACT
Introduction:
Leukemia is a neoplastic disorder originating in a hematopoietic cell that has undergone an intrinsic change, causing it to escape from the normal restraints imposed on proliferative activity. Immunophenotyping is now the preferred method for diagnosing, classifying, staging and monitoring the disease progression as well as response to therapy.
Material and Method:
The material of the present study consisted of 51 patients suffering from hematological malignancies who attended and /or were admitted in Rajendra Institute of Medical Sciences, Ranchi during the period from March 2018 to August 2019.
Results:
A total of 51 cases were diagnosed as acute leukemia on microscopic examination. On immunophenotyping, 36 cases (70.6%) were diagnosed as Acute Myeloid Leukemia (AML), 15 cases (29.4%) were diagnosed as Acute Lymphoblastic Leukemia (ALL). ALL cases were further divided into B-Cell ALL and T-Cell ALL with 8 cases (15.7%) and 7 cases (13.7%) respectively. Cytogenetics could not be done for these cases due to non-availability of the set-up for the same at the institute.
Conclusion:
Flowcytometry can be a great tool in diagnosis and categorisation of leukemia especially at centres where cytogenetics is not available.
Keywords: Flow cytometry, immunophenotyping, leukemia
Introduction
Leukemia is a neoplastic disorder originating in a hematopoietic cell that has undergone an intrinsic change, causing it to escape from the normal restraints imposed on proliferative activity.[1] The diagnosis and classification of leukemia rely on the simultaneous application of multiple techniques. Cytomorphology and histomorphology are combined with cytochemistry and multi-parameter flow cytometry to assign the diagnostic sample to the correct entity. Furthermore, chromosomal analysis, often supplemented by Fluorescence in situ hybridization (FISH), and molecular techniques, such as Polymerase chain reaction (PCR), are needed to definitely confirm the diagnosis. Immunophenotyping is now the preferred method for diagnosing, classifying, and staging and monitoring the disease progression as well as response to therapy. It is particularly helpful in cases when a specific subtype cannot be diagnosed by morphological features. It is a technique in which cells labeled with a fluorescent dye which is coupled to a monoclonal antibody bind to those cells coated with the antigen for which the antibody is specific. The stream of cells is passed through a laser beam and light scattering by the cells is analyzed by flow cytometer software. It is helpful in differentiating ALL from AML, diagnosing mixed phenotypic acute leukemia, differentiating B-cell ALL from T-cell ALL, and differentiating ALL from Malignant Lymphoma. This distinguishing ability of flow cytometry is important as the treatment modality and prognosis of each subtype are different. Flow cytometry can be used by the family physicians for categorizing the cases and thus further referral. Emergency cases such as acute promyelocytic leukemia (APML) can be given primary management.
Material and Methods
The present study consisted of 51 patients suffering from hematological malignancies who attended and/or were admitted in the Rajendra Institute of Medical Sciences, Ranchi, during the period from March 2018 to August 2019. The study was conducted in the department of Pathology of Rajendra Institute of Medical Sciences, Ranchi (Institutional Ethics Committee Letter no. 34 RIMS, Ranchi, Dated 20/02/2018). Proper clinical history was taken followed by Peripheral Blood Smear (PBS) and Bone Marrow examination. Those cases having at least 20% blasts in the PBS and/or Bone marrow aspirate were considered for immunophenotyping. Immunohenotyping was done using BD biosciences 6 color Flow-cytometer. Table 1 shows Tube1 has CD45 only, tube 2 has B-cell markers, tube 3 has T-cell markers, tube 4 has myeloid markers and tube 5 has cytoplastic markers.
Table 1.
Table showing the CD markers used in different tubes for the purpose of immunophenotyping (original table)
| Fluorochromes | Tube1/Blank | Tube2/B-Tube | Tube3/T-Tube | Tube4/Myeloid | Tube5/Cytoplasmic |
|---|---|---|---|---|---|
| FITC | - | CD20 | CD8 | CD64 | cMPO |
| PE | - | CD10 | CD5 | CD33 | cCD79a |
| PCP-C5.5 | - | CD38 | CD3 | HLA-DR | cCD3 |
| PC-7 | - | CD19 | CD4 | CD13 | - |
| APC | - | CD34 | CD7 | CD117 | CD34 |
| APC H7 | CD45 | CD45 | CD45 | CD45 | CD45 |
Results
A total of 51 cases were diagnosed as acute leukemia on microscopic examination. On immunophenotyping, 36 cases (70.6%) were diagnosed as Acute Myeloid Leukemia (AML) and 15 cases (29.4%) were diagnosed as Acute Lymphoblastic Leukemia (ALL). ALL cases were further divided into B-Cell ALL and T-Cell ALL with eight cases (15.7%) and seven cases (13.7%), respectively.
Table 2 shows Incidence of AML is higher than ALL.
Table 2.
Table showing the incidence of various leukemias (original table)
| Type of acute leukemia | Total no. of cases | |
|---|---|---|
| AML (Acute myeloid leukemia) | 36 (70.6%) | |
| ALL (Acute lymphoid leukemia) | 15 (29.4%) | B-ALL- 8 (15.7%) T-ALL- 7 (13.7%) |
| Total | 51 (100%) | |
Table 3 shows CD13, CD33, CD117, CD64, HLA-DR, CD34, cMPO and CD68 are showing myeloid lineage (AML).
Table 3.
Table showing immunophenotyping of AML group (original table)
| CD13 | CD33 | CD117 | CD64 | HLA-DR | CD34 | cMPO | CD38 | |
|---|---|---|---|---|---|---|---|---|
| AML | 30/36 | 30/36 | 28/36 | 6/36 | 36/36 | 33/36 | 34/36 | 27/36 |
Table 4 shows T and B cell ALL are showing positivity for their respective lineage markers.
Table 4.
Table showing immunophenotyping of ALL group (original table)
| Type of ALL | CD20 | CD10 | CD38 | CD19 | cCD79a | CD8 | CD5 | CD3 | CD4 | CD7 | cCD3 | CD34 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T-ALL | 0/7 | 0/7 | 0/7 | 1/7 | 0/7 | 1/7 | 5/7 | 5/7 | 3/7 | 6/7 | 7/7 | 5/7 |
| B-ALL | 6/8 | 5/8 | 5/8 | 8/8 | 8/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 10/8 |
Table 5 shows indicates that the immunophenotypic diagnosis is more accurate than morphological diagnosis. Table 6 shows In majority of the studies AML is more common than ALL.
Table 5.
Morphological diagnosis vs. Immunophenotypic diagnosis (original table)
| Morphological diagnosis | Immunophenotypic diagnosis | ||
|---|---|---|---|
| AML | 34 | AML | 34 |
| ALL | 17 | ALL | 15 |
| AML | 2 | ||
Table 6.
Incidence of different types of leukemias in various parts of the country and world (reference of data cited)
| Authors | Total no. Of cases | Acute Leukemias | AML | ALL | CML | CLL | Others |
|---|---|---|---|---|---|---|---|
| Parekh et al.[2] | 544 | 58.6% | 25.6% | 20.2% | 35.9% | 5.5% | 12.8% |
| Menezes and Mallick[3] | 278 | 65.8% | 16.5% | 35.3% | 31.9% | 3.2% | 14% |
| Kushwaha et al.[4] | 456 | 56.2% | 34.9% | 14.9% | 28.5% | 15.3% | 6.4% |
| Salem DA et al.[5] | 164 | 100% | 68.9% | 31.1% | 0% | 0% | 0% |
| Gupta N, et al.[6] | 375 | 96.3% | 59.7% | 36.6% | 0.8% | - | 2.9% |
Figure 1 shows incidence of AML is higher than that of ALL.
Figure 1.
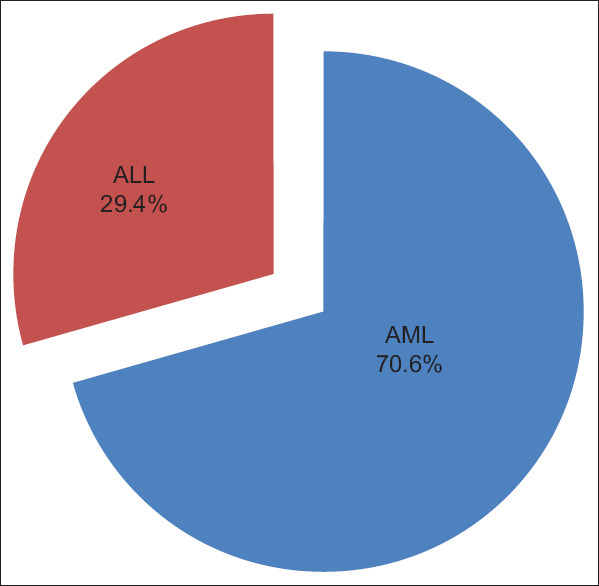
Pie chart showing patients with AML and ALL (original image)
Figure 2 shows cMPO, CD13, CD33 and CD117 positivity indicating myeloid lineage while CD10 positivity indicating B-cell lymphoid lineage.
Figure 2.
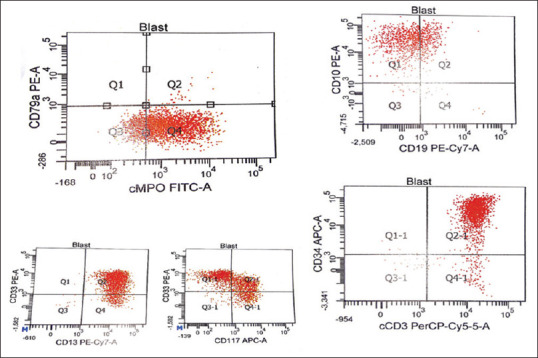
Graphs showing positivity for cMPO, CD10, CD13, CD33, and CD117 cCD3 (original image)
Figure 3 shows Myeloid blasts seen in a case of AML.
Figure 3.
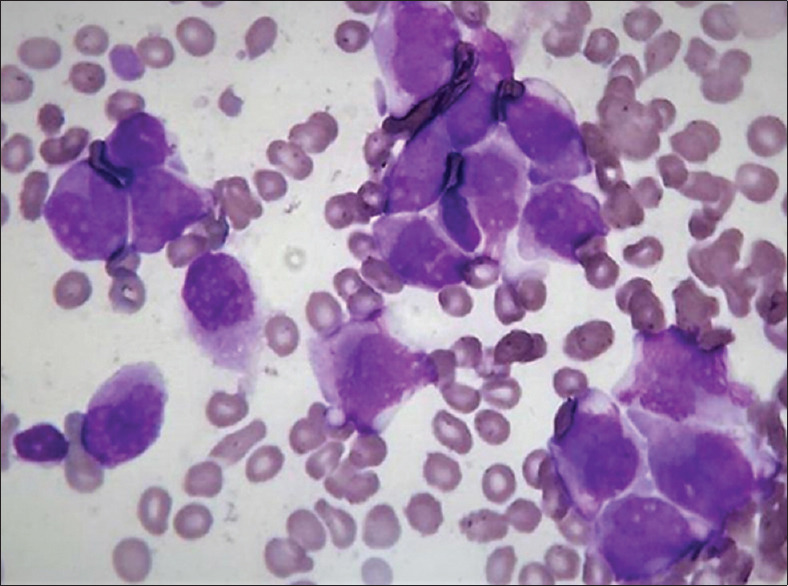
Micrograph showing bone marrow picture of Acute Myeloid Leukaemia (100× magnification) (original image)
Figure 4 shows Auer rods seen in myeloid blasts.
Figure 4.
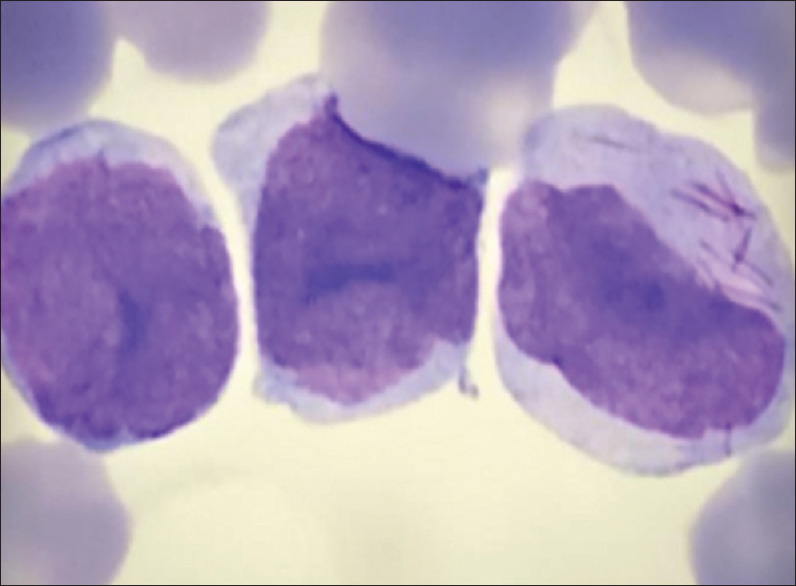
Micrograph showing Myeloblast with Auer rods (100× magnification) (original image)
Figure 5- Lymphoid blasts seen in a case of ALL. ALL.blasts.
Figure 5.

Micrograph showing bone marrow picture of Acute lymphoblastic leukemia (100× magnification) (original image)
Figure 5- Lymphoid blasts seen in a case of ALL.
Discussion
The incidence of AML (70.6%) was found to be more than that of ALL (29.4%). In this study, out of the total ALL cases, B-ALL was 53.3% and T-ALL was 46.7%. Flow cytometry was particularly found useful in cases where morphology failed to give any diagnosis.
There are certain limitations of this study too. Cytogenetics is now an integral part of classifying acute leukemias as per W.H.O. classification. However, due to the non-availability of cytogenetic study at our center, we could not proceed to further investigations.
Conclusion and Take Home Message
Incidence of AML is higher than in ALL and B-ALL is more common than T-ALL. Flow cytometry can be a great tool in the diagnosis and categorization of leukemia, especially at centers where cytogenetics is not available.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. Revised 4th ed. Lyon: IACR; 2017. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues; p. 25. 30, 200, 216. [Google Scholar]
- 2.Parekh BJ. Incidence of different types of leukaemias in various parts of India. 1962 [Google Scholar]
- 3.Menezes and Mallick. Incidence of different types of leukaemias in various parts of the world. 1976 [Google Scholar]
- 4.Shah PM, Patel TB, Patel KM, Parikh BJ. Leukaemia analysis of 1259 cases. In tropics in haematology. Ahmedabad Ed, 1978:35–46. [Google Scholar]
- 5.Salem DA, Abd El-Aziz SM. Flowcytometric immunophenotypic profile of acute leukemia:Mansoura experience. Indian J Hematol Blood Transfus. 2012;28:89–96. doi: 10.1007/s12288-011-0110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta N, Pawar R, Banerjee S, Brahma S, Rath A, Shewale S, et al. Spectrum and immunophenotypic profile of acute leukemia:A tertiary center flow cytometry experience. Mediterr J Hematol Infect Dis. 2019;11:e2019017. doi: 10.4084/MJHID.2019.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


