Abstract
Exertional heat illness (EHI) risk is a serious concern among athletes, laborers, and warfighters. US Governing organizations have established various activity modification guidelines (AMGs) and other risk mitigation plans to help ensure the health and safety of their workers. The extent of metabolic heat production and heat gain that ensue from their work are the core reasons for EHI in the aforementioned population. Therefore, the major focus of AMGs in all settings is to modulate the work intensity and duration with additional modification in adjustable extrinsic risk factors (e.g., clothing, equipment) and intrinsic risk factors (e.g., heat acclimatization, fitness, hydration status). Future studies should continue to integrate more physiological (e.g., valid body fluid balance, internal body temperature) and biometeorological factors (e.g., cumulative heat stress) to the existing heat risk assessment models to reduce the assumptions and limitations in them. Future interagency collaboration to advance heat mitigation plans among physically active population is desired to maximize the existing resources and data to facilitate advancement in AMGs for environmental heat.
Keywords: Exertional heat illness, Heat hazard, Safety, Policy and procedure, Health
Introduction
Diverse occupational settings put athletes, service members, and employees at risk of exertional heat illnesses (EHIs) or death due to excessive heat exposure. Increasingly warm conditions observed in recent years further necessitate risk reduction strategies, such as activity modification. Activity modification guidelines (AMGs) for heat stress aim to optimize performance, maintain work efficiency, and protect individuals from EHIs and their associated morbidity and mortality. Currently, athletic, occupational, and military settings have separate AMGs, and utilize a variety of heat indices (e.g., wet bulb globe temperature [WBGT], heat index [HI]) to quantify potential for environmental heat stress under varying thermal loads. At first glance, AMGs from different settings share common features; however, no previous attempt has been made to identify opportunities to harmonize guidelines where possible. In addition, such an opportunity allows for insights into policy development and implementation, and recognition of important research gaps and applications for use beyond their current settings.
In pursuit of AMG comparison and harmonization, the Korey Stringer Institute convened an interagency, interdisciplinary team of US-based heat health experts. The Korey Stringer Institute, housed at the University of Connecticut, is a nonprofit organization focused on providing research, education, advocacy, and consultation to maximize performance, optimize safety, and prevent sudden death for the athlete, warfighter, and laborer. The team of experts compared current approaches to activity modification and identified opportunities to expand and improve upon these approaches. Particular consideration was given to the guidelines within the context of projected increase in frequency and intensity of heat waves, as well as associated increased heat-related human health consequences (Crimmins et al. 2016) and economic losses (Wenz and Levermann 2016). This meeting of experts was convened under the auspices of the National Integrated Heat Health Information System (NIHHIS), an interagency, multidisciplinary, and nationwide system intended to inform decision-making for heat health risk reduction from long-term planning to short-term responses. Here, we document the outcomes of the discussion and provide opportunities for future research and application of AMGs.
AMGs outline how to identify and assess potentially unhealthy levels of physical exertion given the current or predicted environmental conditions and give guidelines for modifying activity level or behavior to remain healthy. AMGs are established by various methods (e.g., governing bodies, working groups, and consensus panels), often for a specific demographic of worker, athlete, or warfighter. In all AMGs, environmental conditions (e.g., heat) are primary variables. Most AMGs utilize the WBGT to assess risk of exposure to the heat hazard. Compared to simpler, traditional metrics (e.g., air temperature, or temperature-humidity only metrics like HI), WBGT better accounts for heat exchange between the individual and the environment, by integrating the influence of temperature, humidity, radiant heat (e.g., solar radiation), and air movement. Other indices can be used as well, with varying degrees of complexity, predictability, and interoperability (e.g., air temperature, HI, Humidex, Universal Thermal Climate Index [UTCI]).
In addition to an environmental variable, most AMGs account for the individual’s level of physical activity or work load, which when combined with environmental heat stress, allows total heat stress to be determined. Guidelines can also address personal vulnerability factors such as personal protective equipment (PPE) and heat acclimatization status (e.g., (Casa et al. 2012a, b, 2013; Navy and Marine Corps Public Health Center 2014; NIOSH 2016; Secretary of the Air Force 2016; Department of the Army Headquarters 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a)).
After identifying hazard, exposure, and vulnerability components, various interventions are recommended by AMGs to modify these elements of risk—from adequate hydration to reduced work intensity and increased rest cycles. For example, the heat AMG by the Georgia High School Association specifies that athletes must be given unlimited access to hydration and that the rest breaks should be taken in areas where exposure to direct sunlight is avoided (Georgia High School Association 2016). Advanced weather forecasts and in situ observations can also inform measures to heat risk. Although current predictability of complex indicators such as WBGT is limited to less than 1 week lead time (Ministry of the Environment Government of Japan), simpler indicators (e.g., HI) may be predicted with more lead time, and may allow for longer-range planning. For example, temperature and dew point (or relative humidity) can be predicted up to ≈12 days in advance. In contrast, parameters such cloud cover (i.e., the inverse of solar exposure) and wind speed can only be predicted 2–3 days in advance (Haiden et al. 2015). For such predictions to have practical significance, the forecasted values should at least predict WBGT within the same AMG risk category (Cheuvront et al. 2015).
Understanding the methodology behind various guidelines is an essential first step toward comparing the indices and extending them for improved use. This paper will critically examine heat AMGs currently used in athletic, occupational, and military settings in the USA to: (1) identify strengths and weaknesses of commonly used heat stress indices, (2) compare current AMGs and different assumptions of each, and (3) establish an expert consensus on directions for future research on heat safety standards for activity modification and their implementation.
Activity modification guideline enforcement in the USA
Recommendations for occupational heat activity modification standards have been issued since 1972 by the National Institute for Occupational Safety and Health (NIOSH), which is part of the US Centers for Disease Control and Prevention (CDC), in response to an act of Congress (Occupational Safety and Health Act of 1970). These guidelines were reiterated by NIOSH in 2016 (NIOSH 2016) and are consistent with workplace heat AMGs published by the American Conference of Governmental Industrial Hygienists® (ACGIH), a US-based organization of occupational and environmental hygienists (ACGIH 2017). Heat guidelines are communicated to the Occupational Safety and Health Administration (OSHA) for regulatory consideration, while the NIOSH and ACGIH are not regulatory bodies. OSHA enforces workplace safety and health regulations at most private sector employers across the USA and its territories. In most US states, OSHA regulates heat stress under the General Duty Clause (section 5[a][1] of the Occupational Safety and Health Act of 1970; https://www.osha.gov/laws-regs/oshact/toc), which stipulates that employers must furnish workplaces that are free of recognized hazards causing or likely to cause serious harm or death. OSHA also tracks workplace injuries and deaths resulting from heat and other occupational exposures and provides publicly available data on these outcomes (Occupational Safety and Health Administration 2017b; Tustin et al. 2018). However, some situations have been identified that limit the implementation of these guidelines. A recent report by Tustin et al. (2018) found that all cases of EHS fatalities among outdoor workers (n = 14) were exposed to environments where WBGT-based occupational exposure limits were exceeded. For example, heat strain in migrant workers is often undocumented, and the resulting negative consequences of occupational heat exposure are underreported (Jackson and Rosenberg 2010).
Standards in athletic settings are established by various governing bodies for sports (e.g., the National Collegiate Athletic Association, state high school activities associations, youth sport leagues), most of which are not subject to federal or state agency regulations. One of the few administrative controls being implemented at this date is the consideration for hydration breaks by the Fédération Internationale de Football Association (FIFA) (The Associated Press 2014). FIFA recommends that an extra hydration break should be considered at the 30th minute of each half when the environmental condition exceeds 32 °C in WBGT, which was mandated during the FIFA Brazil World Cup in 2014 (The Associated Press 2014). In tennis, the International Tennis Federation and the World Tennis Association employ the WBGT-based AMG by the American College of Sports Medicine (Armstrong et al. 2007) for junior tennis players and female tennis players (Racinais et al. 2015). In US high school athletics, many state high school athletics associations have also adopted environmental monitoring and subsequent activity modification to prevent EHI (Kerr et al. 2014). Some mass participation athletic events, such as distance races, have also adopted environmental monitoring to activate activity modification plans. These plans inform participants about the conditions and potential for heat stress and guide race aid stations to prepare sufficient resources so as to not overwhelm local medical services (Mears and Watson 2015).
In the US Department of Defense (DoD), the Technical Bulletin, Medical 507 (Headquarters, Department of the Army and Air Force 2013) is prepared by the Department of Army and Air Force to provide guidance for heat stress control and casualty management. The first TB MED 507 was published in July in 1980 as a joint publication with the Navy and Air Force (Headquarters, Departments of the Army and Air Force 1980). The next TB MED 507 was not published until March 2003 and again was a joint publication with the Air Force (Headquarters, Departments of the Army and Air Force 2003); it replaced the 1980 version. However, in 1991, the US Army Research Institute of Environmental Medicine in Natick, Massachusetts, published a document entitled “Heat Illness: A Handbook for Medical Officers” because the first TB MED 507 was not up-to-date. The TB MED has again been revised, but each version was developed to provide guidance on heat stress control. The newest bulletin is for military and civilian health care providers and allied medical personnel so they are able to develop preventive programs for protecting military personnel from the potential adverse health effects of working in the heat. Some of the key preventive measures include understanding risk factors, the importance of fluid replacement, how to use WBGT appropriately, the body’s responses and adaptations to heat, and the different types of heat casualties. The TB MED 507 also delineates the roles of unit commanders, medical officers, medics, and combat lifesavers in their coordination of education, planning, and managing to achieve the stated goal. The bulletin is directive in nature and specifically states that unit commanders will perform a series of actions to maintain their troops. Three of such actions are to ensure acclimatization of warfighters; provide adequate clothing, shade, and sunscreens to prevent sunburn; and implementation of appropriate fluid replacement guidance and work-rest cycles, when possible. Likewise, the medical officer is provided directives in the form of “unit medical officers will.” Again, the directives relate to work load and work/rest cycles, education with regard to risk mitigation, recognizing keys signs of impending heat illness, and many other topics. Thus, over the past 38 years, at least four formal documents for heat stress mitigation have been put forward within the DoD.
Heat stress indices
As previously described, environmental variables to estimate external heat exposure include air temperature, humidity, wind speed, and radiant heat. Behavioral factors such as metabolic activity and clothing/equipment are also considered by some heat indices (Epstein and Moran 2006). Multiple heat exposure metrics are available that account for these factors with varying degrees of sophistication. The simplest measures are direct observations of meteorological variables that do not include information on behavioral factors. Empirical heat indices are based on empirical studies of human comfort, and rationale indices use a human heat budget approach (i.e., balance between environmental and metabolic heat loads) to account for both environmental and behavioral factors.
Here, we present a sample of heat measures commonly used by various governmental agencies and governing bodies worldwide, including their main benefits and limitations, with examples of direct and rationale approaches (Table 1). Air temperature is a simple direct measure that uses a thermometer sheltered from the sun and expresses the extent of hot and cold. (American Meteorological Society 2018) It is widely measured at weather stations and thus has wide applicability and is easy to interpret; however, it does not account for other meteorological factors such as humidity, wind speed, or radiant energy that influence the human heat balance. The appropriateness of air temperature to infer heat stress may vary by climate zone. For example, the use of temperature to estimate heat stress in humid climates such as the Southeastern USA may grossly underestimate thermal discomfort, but it may be more suitable in dry climate such as the desert Southwest (US Department of Commerce 2018).
Table 1.
Examples of common direct and rationale indices of heat stress
| Air temperature | Heat index | Humidex | Wet Bulb Globe Temperature (WBGT) |
Universal Thermal Climate Index (UTCI) |
||
|---|---|---|---|---|---|---|
| Typea | Direct | Simplified rationale | Direct | Direct | Rationale | |
| Measured or derived | Measured | Derived | Derived | Derived | Derived | |
| Equation | NA | See footnoteb | See footnoteb | WBGT = 0.7Tnwb + 0.2Tg + 0.1Ta | Mathematical model | |
| Heat stress quantification | Environmental inputsc | T a | Ta, RH, or Td | Ta, vapor pressure or Td | Ta, Tnwb, Tg, Vw | Ta, Vw, RH, MRT |
| Model assumptions/-range of validity | NA | Shaded | Shaded | Sun exposure | Sun exposure | |
| Ta: 26.67–43.33 °C (80–110 °F) | Ta: 21–43 °C (70–109 °F) | Ta: wami weatherd | Ta: all ranges | |||
| Humidity: RH ≥ 40% | Humidity: vapor pressure > 10 mb | Humidity: Tnwb range 5–40 °C | Humidity: RH or vapor pressure, all ranges | |||
| MET = 180 W·m−2 | MET: non-active | MET: Nonspecific; the WBGT limit values set by ACGIH and ISO 7243 (2017) are used for resting (115 W), low (180 W), moderate (300 W), high (415 W), and very high (520 W) work rates. Differing work rates may be used in athletic or military situations based on easy, moderate, or hard work | MET = 135 W m−2 | |||
| Vw: wind speed and person movement = 2.57 m s−1 (5 kts) | Vw: “ventilated” from wind speed | Vw: natural ventilation, all ranges | Vw: wind speed of 0.5–30.3 m s−1 and person movement of 1.1 m s−1 | |||
| Clothing: trousers, T-shirt | Clothing: unknown | Clothing: “light” (0.60 clo)e | Clothing: varies with Ta | |||
| Public data availability | Common from weather station data | Common; derived from weather standard station data | Common; derived from weather standard station data | Uncommon; in situ collection | Less common, derived from standard weather station data plus solar radiation data | |
| Ease of interpretation | Simple | Moderate | Moderate | Moderate | Complex | |
| Sample applications | Some National Weather Service (NWS) forecast offices in arid climates use Ta to inform issuance of heat alerts, such as the HeatRisk tool in Phoenix | Inform issuance of heat alerts via NWS | Environment Canada issuance of heat alerts; CCOHS for outdoor work | Used for activity modification in athletics, the military, and occupational safety | General thermal comfort of population; occupational heat exposure | |
| Reference(s) | Hawkins et al. (2017) | Rothfusz (1990) | Masterton and Richardson (1979) | Yaglou and Minard (1957) | Bröde et al. (2012) | |
| NOAA (2017) | Hawkins et al. (2017) | ISO 7243 (2017) | ||||
| Armstrong et al. (2007) | ||||||
| NIOSH (2016) | ||||||
| Government of Canada (2017) | Departments of Army and Air Force (2003) | |||||
| ACGIH (2017) | ||||||
| CCOHS (2017) | ||||||
Full equations can be found in Gosling et al. (2014)
Air temperature (Ta), relative humidity (RH), dew point temperature (Td), natural wet bulb temperature (Tnwb), globe temperature (Tg), mean radiant temperature (MRT), wind speed (Vw), and metabolic activity (MET)
ISO 7243 states that for accurate WBGT, the Tnwb should measure a range of 5–40 °C and the Tg should measure a range of 20–120 °C
WBGT can be adjusted for changes to clothing/equipment (see ISO 7243 (2017) and Havenith and Fiala (2015))
ACGIH the American Conference of Governmental Industrial Hygienists, CCOHS Canadian Centre for Occupational Health and Safety
In North America, the HI (USA) and the Humidex (Canada) are more complex measures that incorporate both air temperature and humidity with the resulting value provided on an adapted “feels like” temperature scale. The HI is the primary heat measure used by the National Oceanic and Atmospheric Administration’s National Weather Service in issuing public messages on heat safety (Hawkins et al. 2016) while the Humidex is used in a similar way by Environment and Climate Change Canada (Government of Canada 2017). The HI is a simplified version of the complex human energy budget model of the Apparent Temperature (AT) by Steadman (Steadman 1979a, b). The AT is simplified into the HI by holding clothing (long trousers and short-sleeved shirt) and metabolic factors (person is walking at 5 km/h) constant, assuming an individual is in the shade, and controlling other environmental factors (e.g., wind) (Rothfusz 1990) (Table 1). The simplified version of the HI is thus limited with respect to changes in activity, clothing, sun intensity, and wind speed. The Humidex is a discomfort index derived by Anderson (Anderson 1965). It was definitively introduced by Masterton and Richardson and is related to a degree of discomfort with no empirical basis. In its original creation, the Humidex formulation was based on two assumptions of thermoregulation: (1) the “neutral point” of the human body (where the body is neither losing or gaining heat) occurs at an air temperature range of 27 to 30 °C for standard conditions (i.e., nude male, still air, resting), and (2) if the air temperature and RH exceeds 32 and 75%, respectively (or a psychrometric wet bulb of 28 °C), the body cannot continue to maintain equilibrium (Bair and Ruffner 1977). The final categorical ranges for the Humidex are simply based on “… a public relations value in a weather service and conveys, in a simple way to the layman a general idea of atmospheric discomfort” (Landsberg and World Meteorological Organization 1972). Based on such simplicity, the Humidex also suffers from limitations due to human behavior, sun and wind exposure. Alfano et al. (d’Ambrosio Alfano et al. 2011) provide detailed comparisons, limitations, and calculations of the Humidex. Today, it is used in most Canadian provinces and by the Canadian Center for Occupational Health and Safety for monitoring outdoor work in the heat. Both the HI and Humidex are widely available as they can be derived from weather station data. The assumptions, however, may lead to inaccuracies of the actual heat strain in particular cases such as athletes or laborers who may be in the sun and/or highly active.
The WBGT is a direct measure that is designed to account for the influences of air temperature, radiant heating, wind speed, and humidity on heat stress (Yaglou and Minard 1957; International Organization for Standardization 2017). It is widely employed by military agencies, occupational safety agencies, and governing bodies in athletics (Armstrong et al. 2007; Headquarters, Department of the Army and Air Force 2013; NIOSH 2016). Often, these organizations also consider activity and/or clothing to set guidelines and recommendations for behavior modification during excessive heat (Table 2). The WBGT is not commonly measured at weather stations but rather should be collected onsite with a measuring device. However, models are available and can be used to estimate the WBGT by using meteorological data routinely measured at high-end weather stations (Lemke and Kjellstrom 2012). The severity of heat stress based on WBGT is sometimes misunderstood because the calculated values may be lower than air temperatures depending on the amount of solar radiation and water vapor present in air (d’Ambrosio Alfano et al. 2014). For example, a combination of an air temperature of 35 °C and a relative humidity of 50% under full sun will result in approximately 35 °C in WBGT, whereas the resulting HI in the same condition is 41 °C. Based on its initial creation (see [Budd 2008] for a detailed review), caveats to its use exist. Analyses from the 1950s show that exertional heat stroke deaths were not solely attributed to the high WBGT as they occurred across a range of temperatures, with increased mortality among those who were unfit, obese, and unacclimatized recruits during basic training (Budd 2008). Therefore, authors of the original WBGT studies (Schickele 1947; Cook 1955) concluded that “no single heat limit can be set to apply to all situations” (Yaglou and Minard 1957).
Table 2.
Comparison of activity modification guidelines
| Occupational |
Athletic |
|||||
|---|---|---|---|---|---|---|
| Occupational Safety and Health Administrationa |
National Institute for Occupational Safety and Health (NIOSH)b |
American Conference of Governmental Industrial Hygienists (ACGIH)c |
American College of Sports Medicined | |||
| Assumptions | Workers across all industries | Unacclimatized worker | Acclimatized worker | Unacclimatized worker | Acclimatized worker | Training and noncontinuous activity in non-acclimatized, unfit, high-risk individuals |
| Allowable work duration |
|
WBGT-based recommended alert limit (RAL) | WBGT-based recommended exposure limit (REL) | WBGT-based action limit (AL) | WBGT-based threshold limit value (TLV) |
|
| Allowable work intensity | NS |
|
|
|
|
|
| Work-to-rest ratio | NS |
|
|
|||
| Equipment considerations | NS |
|
|
NS | ||
| Hydration plan |
|
|
|
NS | ||
| Athletic |
Military |
|||||
| American College of Sports Medicined |
National Athletic Trainers’ Associatione | U.S. Army and Air Force Soldiers/Airmenf | ||||
| Assumptions | Training and noncontinuous activity in acclimatized, fit, low-risk individuals | Pre-fall season American Football athletes and other sports | Average size and heat-acclimatized soldier wearing battle dress uniform doing easy work (250 W) | Average size and heat-acclimatized soldier wearing battle dress uniform doing moderate work (425 W) | Average size and heat-acclimatized soldier wearing battle dress uniform doing hard work (600 W) | |
| Allowable work duration |
|
|
|
|
|
|
| Allowable work intensity |
|
NS |
|
|
|
|
| Work-to-rest ratio | NS |
|
|
|
|
|
| Equipment considerations | NS |
|
|
|||
| Hydration plan |
|
|
|
|
|
|
NS not specified, WBGT wet bulb globe temperature, WRR work-to-rest ratio, Light 180 W, Moderate 300 W, Heavy 415 W, Very Heavy 520 W
Occupational Safety and Health Administration (2017)
Finally, the UTCI is a fully rationale index, where activity and clothing levels can be adjusted within the model to optimize the index for particular needs (Bröde et al. 2012). The UTCI can also be presented as a temperature scale with 10 categorical designations ranging from “extreme cold stress” to “extreme heat stress”. Recent research by Bröde et al. (Bröde et al. 2017) introduced a procedure for adjusting the UTCI to those extended conditions of high metabolic activity and clothing insulation over longer durations. However, UTCI is new for most people, and thus the interpretation of the categories is not widely known, which can result in confusion and misuse of a new, more complicated index.
Heat risk considerations
Overview of the heat balance equation
Normal physiological function requires deep body temperature regulation. The rate and amount of the heat exchange is governed by the fundamental laws of thermodynamics. The rate of heat exchange with the environment is a function of air temperature and humidity, skin temperature, air velocity, evaporation of sweat, radiant temperature, and type, amount, and characteristics of the clothing worn (Parsons 2014). The following is a simple version of the heat balance equation:
| (1) |
where: (M – W) = total metabolism minus external work performed, C = convective heat exchange, R = radiative heat exchange, K = conductive heat exchange, E = evaporative heat loss, and S = change in body heat content.
The heat balance equation contains both physiological and environmental factors that affect heat exchange. These factors may determine individual vulnerability to environmental heat stress. For example, evaporative heat loss is a primary means for heat loss in hot environments and/or when generating a high level of metabolic heat. However, a low skin-to-air vapor pressure gradient and/or clothing permeability may prevent evaporative sweat from the skin and thus limit evaporative cooling (Vanos et al. 2010). This ability to evaporate sweat is described by the ratio of required evaporation needed to maintain thermoregulation (Ereq) to the maximum evaporation allowed by the external environment (Emax) (i.e., Ereq/Emax). Ereq is calculated based on convection, radiation, and metabolic heat loads. It is used for heat stress assessment by a method entitled the “Required Sweat Rate” (ISO7933 2004), later revised to the “Predicted Heat Strain” (Malchaire et al. 2001; ISO7933 2004). Emax is determined based on the vapor pressure gradient, clothing resistance, and wind speed, to a maximum of 390 W m−2 (Parsons 2014). As suggested by Belding and Hatch, when Emax > Ereq, body temperature can be controlled; however, if Emax < Ereq, sweat evaporation and cooling are limited (Brotherhood 2008).
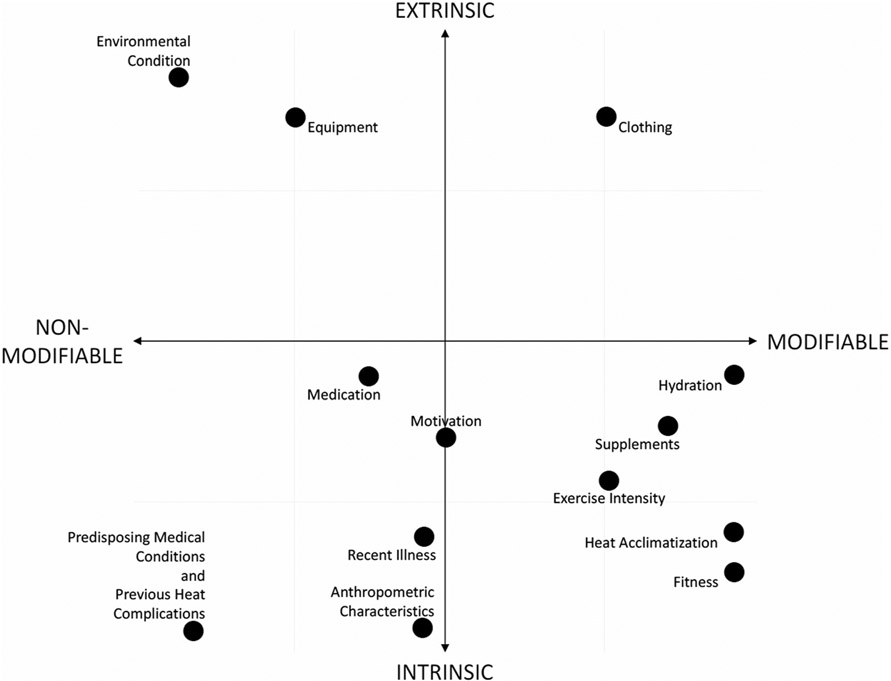
Factors that increase the rate of heat gain to the body or diminish the rate of heat dissipation away from the body may predispose athletes, workers, and warfighters to EHIs. Factors affecting heat exchange can be classified as either intrinsic (inherent to the individual) or extrinsic (a feature of their environment). Figure 1 plots common intrinsic and extrinsic risk factors associated with EHIs. Most of the risk factors associated with exertion in the heat are somewhat modifiable (quadrant IV in Fig. 1). However, both intrinsic and extrinsic factors must be addressed to minimize the risk of EHIs. Catastrophic and fatal outcomes from heat stress typically occur when there is a perfect storm of intrinsic and extrinsic risks (Rav-Acha et al. 2004; Tustin et al. 2018).
Fig. 1.
Cartesian coordinate graph displaying factors that influence body heat balance when performing physical activity in the heat. Horizontal axis weighs the degree to which the factor is modifiable (+) or non-modifiable (−). Vertical axis weighs whether the factor is influenced by extrinsic variable (+) or intrinsic variable (−) of the exercising individual
Intrinsic risk factors
The largest contributor to heat gain is the metabolic heat production resulting from muscular work, which is primarily dictated by the intensity and efficiency of movement (Whipp and Wasserman 1969). Therefore, individuals who are more fit perform more efficient work and demonstrate lower body temperatures during exercise by the heat when completing a given absolute workload, compared to individuals who are less fit (Smoljanić et al. 2014). This inefficiency can be further compounded by the extra mass carried in obese individuals (Bedno et al. 2014; Moyen et al. 2016). Diminished thermoregulatory responses that may also result from aging (Kenny et al. 2010; Stapleton et al. 2015), cardiovascular disease (Balmain et al. 2017), and diabetes (Carter et al. 2014; Kenny et al. 2016) are also being explored as vulnerabilities associated with the ability to work in the heat. Thus, certain individuals may need specific AMGs. Due to the recognition that personal risk factors can predispose individuals to EHI, some occupational AMGs recommend that these individuals be exposed to lower levels of environmental heat (Table 2). For example, ACGIH states that its heat Threshold Limit Value (TLV®) only applies to workers without predisposing medical conditions (ACGIH 2017).
As expected, conditions that compromise thermoregulation also elevate risk for EHI and classical heat injury, particularly among workers who are older (i.e., > 65 years of age), obese (BMI > 30), or have certain medical conditions (cardiovascular disease, diabetes, and taking certain medications) (NIOSH 2016). Older individuals sweat less in response to heat and may have chronic hypohydration (Kenny et al. 2010; Stapleton et al. 2015). Obesity is a risk factor for an increased susceptibility to heat injury because high body fat results in a greater physical effort (increased at any given level of activity), which then leads to an increase in metabolically produced body heat. In addition, high body fat results in a decrease in body surface area relative to body volume, which becomes less ideal for loss of body heat. All of these factors reduce heat transfer from the obese individual to the environment (Wells and Buskirk 1971; Vroman et al. 1983).
Finally, workers of any age or body mass who are taking certain medications are at elevated risk for the development of heat stroke. The list of medications is comprehensive and beyond the scope of this paper (see NIOSH 2016 table 4.2 for a list of commonly used medications that affect heat tolerance). Particularly risky medications include those affecting cardiac function (beta blockers), which prevent cutaneous vasodilation, thus limiting the efficacy of this thermoregulatory mechanism. In addition, common diuretics used for treating hypertension have the potential for inducting dehydration in workers.
In workers, most fatal EHIs occur during the first week after a person starts a new job in a warm environment (Arbury et al. 2016). Likewise, most EHIs occur in the first week of American football practice (Cooper et al. 2016), or military recruits originating from northern states (Carter et al. 2005). These findings suggest that lack of heat acclimatization and physical readiness (i.e., fitness) are important intrinsic risk factors. Occupational guidelines suggest that employers create a formal plan to allow newly hired workers, and those who return after an extended absence, time to adapt to environmental stress (NIOSH 2016). Similar policies have been adopted for American football (Casa et al. 2009). Population specific guidelines are discussed in detail in a later section.
Behavioral factors (i.e., motivation to work hard to impress a new boss, coach, or supervisor or to make money) may also put newly hired workers at risk. In cases of exertional heat stroke, it is common for individuals performing exercise not matched to their fitness level, compounded by a hypermotivation to perform well, to create situations wherein their heat gain exceeds their ability to dissipate heat (Rav-Acha et al. 2004).
Febrile illnesses and underlying infections, whether symptomatic or sub-clinical, also limit exercise in the heat due to a diminished range of safe body temperatures and a pro-inflammatory state (Cleary 2007). These can be further complicated by drugs or supplements that increase metabolism, like amphetamine derivatives (Bailes et al. 2002). Globally, whether through sweat-based fluid losses or another mechanism, hypohydration increases the thermoregulatory strain of a given workload and should be minimized to help keep exercising individuals safe (Cheuvront et al. 2005). Therefore, any factor that influences hydration (e.g., alcohol consumption, medications) can be broadly considered a risk.
Genetically, malignant hyperthermia (Hosokawa et al. 2017), along with other polymorphisms that alter skeletal muscle metabolism (Li et al. 2014), may in theory predispose individuals to EHIs. Finally, individuals with a previous medical history of EHIs may be predisposed to future heat injuries, either due to an underlying condition or damage from the initial heat illness (Casa et al. 2015).
Extrinsic risk factors
Key extrinsic factors that dictate the capacity for human activity in the heat incorporate ambient conditions and organizational risk reduction strategies; these are both covered in more detail below. However, it is important to consider that extrinsic risks can be magnified by clothing and equipment. Encapsulating PPEs (e.g., firefighter bunker gear; nuclear, biological, and chemical warfare equipment; or football uniforms) limit heat exchange because the protective layer of clothing blocks heat losses through convection, conduction, and emitted radiation—the other primary means for heat exchange with the environment (as in Eq. 1) (Armstrong et al. 2010; Parsons 2014; Costello et al. 2015). Furthermore, the increased clothing weight and reduced ergonomics from the PPEs will result in increased metabolic rate (Dorman and Havenith 2009).
Another important extrinsic factor to be noted is self-pacing (Miller et al. 2011; Jay and Brotherhood 2016). For example, in occupational settings, the mechanism of pay may alter worker behaviors in that those who are paid piecemeal (i.e., by basket) may decide to avoid breaks because they can negatively impact their earnings (CDC 2008; Mitchell et al. 2018). Workers who are less productive in the heat may often compensate for their lower productivity by working longer hours (Sahu et al. 2013), which may also be the result of self-pacing and the need to meet a quota. This type of financial compensation is an issue in low-income populations (Fleischer et al. 2013). From a sport or athletics perspective, there are many times an athlete may be either highly motivated or does not have control over their work-to-rest ratio, which could push them into the realm of exertional heat stroke (Rav-Acha et al. 2004).
Comparison of activity modification guidelines in the heat
Extreme heat risk reductions start with identification and reduction of heat stress hazards. Some of these hazards may be inherent to the work setting and may be inevitable (e.g., firefighting, outdoor sports, combat training). Therefore, modifications in the total exposure time and work intensity are commonly utilized to set limits on the maximal heat production (i.e., total heat strain as a time weighted factor), thereby reducing the heat strain (Armstrong et al. 2007; Headquarters, Department of the Army and Air Force 2013; ACGIH 2017). Additionally, various engineering, administrative, and personal controls have been proposed to serve as preventative measures in optimizing the work environment (Armstrong et al. 2007; Headquarters, Department of the Army and Air Force 2013; Casa et al. 2015; NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a).
Table 2 summarizes key characteristics of AMGs used in the occupational, athletic, and military settings (Armstrong et al. 2007; Headquarters, Department of the Army and Air Force 2013; Casa et al. 2015; NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a). Each setting has unique assumptions that represent traditional contexts in which one may be exposed to extreme heat (Table 2). All examples included in the table utilize WBGT as the standard measurement to quantify the environmental heat. As the WBGT value increases, allowable work duration, allowable work intensity, and the work-to-rest ratio are reduced (i.e., less work hour with longer breaks).
In occupational settings, engineering controls are implemented to modify metabolic heat production, or to increase heat loss through convection, radiation, or evaporation. (NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a). Engineering controls might include those that increase air velocity (e.g., cooling fans in rest stations, ventilated clothing), reflective or heat absorbing shielding or barriers, and reduction of steam leaks, wet floors, or humidity. Other engineering controls may be more straightforward, such as using powered assistance for heavy tasks, providing air conditioning or shaded areas at worksites for breaks. It should be noted that fans may have limited effectiveness in extreme wet-heat environments (e.g., air temperature at 42 °C with relative humidity greater than 60%) (Gagnon et al. 2017). Administrative controls in occupational settings may include: limiting time in the heat and/or increasing recovery time in a cool area (e.g., work/rest schedules); reducing the metabolic demands of the job (e.g., mechanization, use of special tools, increasing the number of workers per task, limiting strenuous tasks); instituting a heat acclimatization plan and increasing physical fitness; implementing a buddy system to watch for early signs and symptoms of heat intolerance; providing adequate amounts of cool, potable water near the work area and encouraging all workers to drink (i.e., 1 cup [0.24 L] of water or other fluids every 15–20 min); and requiring workers to conduct self-monitoring (e.g., monitoring work and recovery heart rate) and creating a work group (e.g., workers, a qualified health care provider, and a safety manager) to make decisions on self-monitoring options and standard operating procedures (NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a).
In addition, a heat alert program (HAP) should be implemented if a heat wave is forecasted. The HAP provides procedures to follow in the event a Heat Alert is declared, emphasizing prevention and early recognition of heat-related illnesses. Workplace training programs should also be implemented for all workers and their supervisors who work in areas where there is reasonable likelihood of EHI (NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a). Training should include information on heat stress hazards, risk factors, proper hydration, heat protective clothing and equipment, acclimatization, signs and symptoms, first aid, and specific criteria to call emergency medical services. Additionally, supervisors should also receive training on how to monitor weather reports and advisories, as well as how to use adjusted temperature scales (e.g., WBGT and HI) for decision-making concerning protective measures (Table 1). Recommended alert limit (RAL) and recommended exposure limit (REL) serve as the action limit (AL) and threshold limit value (TLV) for unacclimatized and non-acclimatized workers, respectively (NIOSH 2016; ACGIH 2017). These limits are calculated using the metabolic rate (M) in watts, and the unit of derived TLV and AL is in WBGT (°C) (ACGIH 2017):
| (2) |
| (3) |
When engineering and administrative controls are not enough, PPE and clothing provide supplemental protection (NIOSH 2016; ACGIH 2017; Occupational Safety and Health Administration 2017a). PPE that may reduce heat stress include fire proximity suits, water-cooled garments, air-cooled garments, cooling vests, wetted over-garments, ventilated clothing, sun hats, and light-colored clothing.
In athletics, heat-specific activity modification within competition rules and protective equipment guidelines are limited. Most risk reduction interventions are focused on activity modification during training through the adjustment of exercise duration, intensity, work-to-rest ratio, and amount of equipment worn (Armstrong et al. 2007; Casa et al. 2015). In the USA, American football has received special attention because of their vulnerability to EHI due to the multiple factors unique to the sport: preseason training starting in the midst of the summer, requirement to wear protective equipment, high-intensity intermittent exercise, and large body mass (Grundstein et al. 2012). Collegiate and some secondary school state high school organizations have implemented American football-specific heat acclimatization programs to mandate gradual introduction to workouts during the first 10–12 days of the preseason in summer months (Casa et al. 2009; National Collegiate Athletic Association 2013). This strategy is now widely implemented in varied sport settings, both in individual and team sports (Sunderland et al. 2008; James et al. 2017; Casadio et al. 2017). Importantly, key factors such as hydration and fitness status can greatly impact the influence of heat acclimatization. If an individual is hypohydrated, the benefits can be negated (Sawka et al. 1983); in contrast, a highly fit individual will already have an increase in their individual sweat rate, one of the benefits that accompanies heat acclimatization. Heat acclimatization through exercise can increase sweat rate by as much as 20 ± 10%, thereby reducing body temperature for a given workload (Daanen et al. 2018). Changes in factors that influence heat acclimation (e.g., changes in fitness, hydration, or overall acclimatization status) may therefore impact risk for heat illness. The National Athletic Trainers’ Association also recommends to provide opportunities to cool the body when the environmental condition exceeds 30 °C in WBGT (Casa et al. 2015). In fact pre and per-cooling are common methods used in the athletic settings, which aim to lower the internal body temperature to maximize the capacity of temperature gain or to moderate the rapid rise in internal body temperature, respectively (Adams et al. 2016). The type, timing, and duration of cooling modalities should be dictated by the nature of sport for practical application, such as the difference in game intermissions, substitution limits, and amount of equipment worn, and there is currently no restriction in the usage of such interventions as long as they are not invasive nor harmful to the athletes (Adams et al. 2016). Although there are varying results to support and refute the benefits of body cooling, most literature supports its effectiveness in reducing physiological strain associated under appropriate cooling modalities (McDermott et al. 2009). Generally speaking, as it pertains to cooling modalities, the larger the surface area that is cooled, the longer the duration, and the colder the modality, the greater the benefit (McDermott et al. 2009). Because performance optimization in the heat and EHI prevention are inextricably associated in an athletic context, teams with well-trained coaches and sports medicine teams often implement the aforementioned strategies without being prompted by the governing organizations (Casadio et al. 2017). However, this is frequently not the case in youth and recreational levels where financial resources and heat illness prevention knowledge may be limited. In recent years, several state high school athletics associations and youth sport governing bodies have been encouraged to promote emergency health and safety best practices related to heat illness (Casa et al. 2013; Huggins et al. 2017). In response to these task force documents, many have incorporated educational contents to equip coaches with proper knowledge regarding EHI prevention (Kerr et al. 2014; Adams et al. 2017). However, there is minimal research regarding the effectiveness of this education or adoption of these best-practice policy recommendations. Reports of fatal exertional heat stroke cases strongly suggest a lack of awareness among the coaches in recognizing the EHI risks and supports continued effort to correct the misconceptions regarding EHI risk (Adams et al. 2014; Valdes et al. 2014).
Within the US Army, a five-step risk management process is used by the unit command teams to mitigate EHI risk (Army 2014). Risk management is a continuous, dynamic process that occurs throughout both planning and execution of training and operational activities. The steps include: (1) identify the hazards, (2) assess the hazards, (3) develop controls and make risk decisions, (4) implement controls, and (5) supervise and evaluate.
Identification of heat hazards includes gathering information on current and future weather conditions, uniform requirements, and physical fitness of warfighters. Assessment of training areas for terrain, available shade, and proximity of medical support provide additional key information. By assessing the hazards for impact on operations, command teams determine the level of associated risk. High ambient temperatures and humidity for several days will increase the risk of EHI (Wallace et al. 2005). Warfighters who are not acclimatized will also be at increased risk (Rav-Acha et al. 2004). Commanders then estimate the probability of EHI and the expected severity (from negligible to catastrophic), and predict the level of risk with a risk assessment matrix (Army 2014). Specific controls, such as fluid replacement and work-to-rest ratio guidelines for warfighters performing training or operations in the heat are summarized in the Technical Bulletin Heat Stress Control and Heat Casualty Management (TB MED 507) (Headquarters, Department of the Army and Air Force 2013). These guidelines as listed will sustain performance and hydration for at least 4 h in the specified heat category and have recently been revalidated for an update of TB MED 507. Medical support planning is an additional control, also directed by TB MED 507 treatment guidelines. A comprehensive treatment plan, from point of injury through definitive hospital care, is created, resourced, and evaluated. Unit level medical providers deliver essential input to commanders for this risk management step. Once a training event or operational mission commences, command teams provide supervision and ongoing risk management. Training may be discontinued, or a mission aborted, if unexpected conditions arise, or if increasing numbers of EHI compromise the training or mission intent. Surveillance of EHI further contributes to the planning process. Heat exhaustion and exertional heat stroke are currently reportable medical events under the 2017 Armed Forces Reportable Medical Events Guidelines (Armed Forces Health Surveillance Branch 2017). This system provides EHI information to commanders and medical providers to incorporate into their future risk management process.
Comparison of heat acclimation and acclimatization guidelines
Between 1980 and 2015, 44 EHS fatalities occurred during preseason high school football (Attanasio et al. 2016); however, only one death was documented from the states that has implemented the heat acclimatization guidelines, which lends some support AMG’s efficacy. Heat acclimation can be defined as a complex series of adaptations that occur in a controlled environment over the course of 7 to 14 days (Armstrong and Maresh 1991). Heat acclimatization is the same process but occurs in a natural environment, which is the most common for military personnel, athletes, and outdoor laborers to experience. Heat acclimation/acclimatization adaptions lead to reductions in heart rate, decreased body and skin temperature responses, decreased perceived exertion, increased sweat rate, hastened sweat onset, decreased sodium losses in sweat and urine, increased stroke volume, increased plasma volume, and an overall enhanced ability to physically exert oneself in the heat (Armstrong and Maresh 1991; Pawelczyk 2001).
Acclimation is known to depend on volume, intensity, and maintenance of an elevated body temperature during physical activity (Pandolf 1979; Armstrong and Maresh 1991). Additionally, it is reported that acclimation in hot and dry environments elicits a lower increase in sweat rate compared to heat acclimatization occurring in hot and humid environments (Armstrong and Maresh 1991). Below, we outline population-specific (athlete, laborer, or warfighter) guidelines that have been published for the implementation of heat acclimatization within each of the listed cohorts. A comparison of heat acclimatization recommendations and guidelines is also summarized in Table 3.
Table 3.
Population specific heat acclimatization induction guidelines
| Population | Area of Modification | Days 1–2 | Days 3–5 | Days 6–14 | |
|---|---|---|---|---|---|
| Occupational | OSHA (OSHA 2017) | Increase heat exposure time each day over 7–14 days | |||
| NIOSH (NIOSH New workers 2016) | New workers | Day 1, < 20% of usual exposure | Subsequent days, < 20% increase from previous day | ||
| Workers with job specific experience | Day 1, < 50% of usual exposure | Day 3, < 80% of usual exposure | |||
| Day 2, < 60% of usual exposure | Day 4 and beyond, 100% exposure | ||||
| ACGIH (ACGIH 2017) | 3 weeks of physical activity under heat stress | ||||
| Athletic (Casa 2012a, b, 2013) | Number of practices permitted per day | 1 | 2, only every other day | ||
| Equipment | Helmets only | Helmets and shoulder pads | Full equipment | ||
| Maximum duration of single practice session* | 3 h | 3 h (a total maximum of 5 h on double session days) | |||
| Walk through time (not included as practice time) | 1 h (but must be separated from practice for 3 continuous hours) | ||||
| Contact | No contact | Contact only with blocking sleds/dummies | Full, 100% live contact drills | ||
| Military | Air Force (Secretary of the Air Force 2016) | > 2 continuous hours of work/exercise in 5 of the last 7 or 10 of the last 14 days define those who are acclimatized | |||
| Army (Department of the Army Headquarters 2016) | Regular strenuous exercise in the heat for 10-14 days defines heat acclimatized | ||||
| Navy (Navy and Marine Corps Public Health Center 2014) | Gradually increase physical training and work in hot, humid environments over days or weeks | ||||
Laborers
The OSHA technical manual (OTM) provides information about workplace hazards and controls to OSHA’s Compliance Safety and Health Officers to ensure safe work conditions (Occupational Safety and Health Administration 2017a). The OTM states that employers should use a structured program to help workers acclimatize to the heat and provides the following guidelines: (1) increase the time each day, over a 7- to 14-day period that an unacclimatized worker is exposed to heat stress while the worker conducts normal work activities and (2) acclimatized workers who are not exposed to high heat loads for a week or more may need some time to re-acclimatize—typically 2 or 3 days. While this second point is accurate, it should be noted that most of the adaptive changes gained from the acclimatization will be lost without heat exposure for more than a week (Daanen et al. 2018). In such a circumstance, one may need to start the acclimatization process from the beginning.
NIOSH states “employers should have an acclimatization plan for new and returning workers, because lack of acclimatization has been shown to be a major factor associated with worker heat-related illness and death” (NIOSH 2016). To ensure that workers are acclimatized, NIOSH recommends employers include heat acclimatization questions within the preplacement medical evaluation. For implementing an acclimatization plan, NIOSH recommends: (1) gradually increase workers’ time in hot conditions over 7 to 14 days; (2) for new workers, the schedule should be no more than 20% of the usual duration of work in the heat on day 1 and no more than 20% increase on each additional day; (3) for workers with previous experience, the schedule should be no more than 50% of the usual duration of work in the heat on day 1, 60% on day 2, 80% on day 3, and 100% on day 4; (4) non-physically fit workers require more time to fully acclimatize; (5) closely supervise new employees for the first 14 days or until they are fully acclimatized; (6) acclimatization can be maintained for a few days of non-heat exposure; (7) taking breaks in air conditioning will not affect acclimatization; and (8) absence from work in the heat for a week or more results in a significant loss in the beneficial adaptations.
The ACGIH also puts forth guidelines for heat acclimatization (ACGIH 2017). While this publication is specifically directed at threshold limit values (TLVs) or biological exposure indices (BEIs), the value of heat acclimatization within both of these is acknowledged. The main recommendations state: (1) full heat acclimatization requires up to 3 weeks of continued physical activity under heat stress conditions similar to those anticipated for the work and (2) a noticeable loss occurs after 4 days of the discontinued activity.
Athletes and the physically active
It has been recommended that heat acclimatization be implemented during the preseason period for both high school (Casa et al. 2009) and college athletes (Casa et al. 2012a). This recommendation has been highlighted in more recent years due to the number of athlete deaths that have occurred during the first few days when athletes return to activity (Bergeron et al. 2005; Grundstein et al. 2012; Kerr et al. 2013; Casa et al. 2013). It is recommended that all athletes follow a heat acclimatization program at the start of all preseason or return to activity periods (Casa et al. 2012a, b, 2013). The main recommendations can be seen in Table 3. Starting with the first day of preseason practice, these guidelines allow the introduction of longer practice sessions and protective equipment. It should be noted that while these recommendations are specific to sports with equipment/helmets, it should not prohibit other sports from following the guidelines.
Warfighters
Each branch of the US Military has its own version of acclimatization schedules and AMGs for the primary purpose of reducing EHI in a training environment. They share several concepts about acclimatization; for example, they occur over days to weeks and require near daily sweat-inducing exertion in target environmental conditions.
Air Force policy states “An individual is considered acclimatized if he or she has undertaken at least two continuous hours of work or exercise in five of the last seven days, or 10 of the last 14 days in the same environmental conditions as the proposed activity” (Secretary of the Air Force 2016). The Air Force and Army use a table of workload versus WBGT to determine modification of the work/rest cycle; however, the Air Force further limits work based on acclimatization status.
From the Army, the heat acclimatization guidelines suggest, “Most Soldiers’ physiological responses to heat stress improve in 10-14 days of exposure to heat and regular strenuous exercise. Factors to consider in acclimatizing Soldiers are the WBGT index; work rates and duration; uniform and equipment; and Soldiers’ physical and mental conditions.” (Department of the Army Headquarters 2016).
The U.S. Navy, in NAVMED P-5010-3, Heat And Cold Stress Injuries (Navy and Marine Corps Public Health Center 2014), states: “Acclimation is important to prevent heat stress injuries. Acclimation can best be accomplished by exposing individuals to a gradual increase in physical training and work in a hot, humid environment over a period of days or weeks. Various body systems adapt at different rates, but two thirds or more of the adaptation may be obtained within 5 days.” Lastly, all branches of the US military acknowledge that combat operations may require activity that does not comply with these guidelines.
Limitations and future research
As is apparent in the preceding sections, numerous efforts are in place across diverse sectors to protect individuals from EHIs and heat mortality. However, preventable EHIs and EHS death still occur in athletics (4.42 EHI per 100,000 athlete exposures in high school American football players (Kerr et al. 2013)), military (1.96 EHIs per 1000 person-years (Armed Forces Health Surveillance Bureau 2017)), and occupational settings (0.22 EHS fatalities per 1000,000 workers (Gubernot et al. 2015)). Therefore, further research is needed concerning heat health impacts and implementation of AMGs. Several lines of research will be required to better understand attributes of human-environment heat exchange during real-world experiences. These should include validation and evaluation of current AMGs; environmental monitoring of personal exposures; real-time monitoring of individuals with new mobile biometrics; data collection on diverse, vulnerable populations; mathematical modeling; and finally, combinations of these approaches.
Systematic validation and evaluation of guidelines
Despite the availability of AMGs, data on how well they actually perform to limit heat casualties are typically lacking. Active surveillance and data on adherence to the particular guidelines are critical for validation and to improve the quality of actions or responses. Currently, the data on EHI and death are limited, likely underreported, and rely heavily on reports from medical professionals and case reports (Rav-Acha et al. 2004; Carter et al. 2005; Grundstein et al. 2012; Gubernot et al. 2015; Tustin et al. 2018). Identifying and reporting a heat-related injury can be confounded by medical coding, inconsistencies with terminology, and/or comorbid medical conditions or symptoms resembling other conditions. Examples of existing database include: National Center for Catastrophic Injury in Sport (http://nccsir.unc.edu), National Collegiate Athletic Association (https://www.sportinjuryreport.org/NCAAReport), the Armed Forces Health Surveillance Center, and OSHA for tracking heat illnesses that occur when employees are at work. Efforts to coordinate and merge medical, environmental, and physiologic data would be important for validation and evaluation of current guidelines (Minard 1961; Attanasio et al. 2016). It is often difficult to study the true efficacy of AMG, due to a lack of similar control groups to quantify the magnitude of changes (i.e., reduction in EHI morbidity) (Toloo et al. 2013). For example, a heat warning system has shown to reduce EHI (Toloo et al. 2013); however, little is known about these system’s optimal timings, as this is difficult to study when accounting for multiple real-world factors (e.g., population awareness, willingness to change, sociodemographic factors).
Environmental monitoring of personal exposures
For AMGs to be applied in an accurate manner, decision makers require data at fine micro-scales that are spatially and temporally congruent with the health impact (Solís et al. 2017). This is particularly important when weather information underestimates the actual environment experienced at the field or work sites (Cheuvront et al. 2005), which may demand people to stay active in potentially harmful environment. Although the use of portable devices to monitor environments in specific known locations is becoming more common, new mobile technologies are required to understand and respond when exposed to extreme heat in remote environments (e.g., farmworkers in fields, workers in mines, firefighters, deployed Service members). Monitoring individually experienced temperatures (IET) (Kuras et al. 2017) with miniaturized sensors (e.g., iButtons®, Kestrel Drops®) can assess exposure-response relationships in non-laboratory settings. This may facilitate individualistic AMGs in groups who are working outdoors and exposed to lengthy heat exposure under shifting microenvironments throughout the day (Sugg et al. 2018). Heat exposure (and thus potential physiological strain) is based on temperature, radiation, wind, and vapor pressure, plus metabolic activity and clothing (Kuras et al. 2017; Hosokawa et al. 2018). Identifying variables related to personal environmental monitoring that result in clinically important difference (i.e., decreased EHI incidents, increased performance) coupled with wearable devices that measure physiological loads will maximize the use of limited resources and help direct future guidelines. When wearable devices are not practical, parameterizations based on studies from wearables are needed so that individual impacts can be modeled without direct observations. Predictive models should include individual factors that modulate human thermal comfort and response, such as gender, fitness, and body mass (Zhang et al. 2001).
At the same time, in order for AMGs to be relevant to early warning systems and long-term planning to reduce heat risk, they must be scalable to meet spatial and temporal resolutions available in weather and climate models. Studies to connect micro-scale environmental exposure monitoring with macroscale remotely sensed information available from satellites and in situ observations from ground-based stations can identify accurate ways to “downscale” coarser predictions from traditional environmental observing systems to make them applicable to activity modification decision-making needs.
Physiological monitoring of heat stain through wearable technologies
AMGs targeting individuals within a group are needed but will only be possible when physiological monitoring is continuously updated, and integrated into group physical activities. For example, real-time feedback of hydration status and internal body temperature during heat exposures may allow for prescribed, individualized activity modification, yet there remains a need for further development and testing of sensor accuracy and real-world applicability. Many techniques used to assess core temperature or hydration (e.g., blood draws, urine samples, and nude body weights) are not realistic in many field settings and definitely not in remote locations, especially when monitoring large number of people. Skin temperature, heart rate, and possibly sweat responses can be captured using new technologies with Bluetooth-enabled epidermal electrodes (Bandodkar et al. 2014; Choi et al. 2018) or commercially wearable activity sensors (Düking et al. 2016; Guo et al. 2017). For example, flexible microfluid devices adhered to human skin can collect and analyze sweat during exercise through colorimetric assays to detect lactate, glucose, and chloride ion concentrations and can be further integrated with smartphones (Koh et al. 2016). With real-time knowledge of heat-health biomarkers, individual-level information can be used to dictate work-to-rest ratios, inform optimal training regimes and fluid or electrolyte replacement, inform individualized heat acclimatization schedules, limit individuals from reaching critical heat-health thresholds, provide guidance for implementing heat acclimatization guidelines during initial heat exposures, and in the worst-case scenarios provide an initial assessment of exertional heat stroke. Monitoring of continuous, real-time core body temperature during activity remains challenging. Other research using direct temperature measurement via ingestible thermometer pills (e.g., e-Celsisus®, HQInc, VitalSense®) as well as indirect temperature measurement via the zero-heat flux thermometry, regression and multi-parameter estimation approaches, or sequential heart rate estimated internal temperature (ECTemp™) have also created opportunities for monitoring and applying individualized AMGs in these same populations (Huggins et al. 2018). However, the feasibility of these measurements, locale, and cost associated with larger numbers remains challenging. Currently, no noninvasive device can accurately assess core body temperature within mean bias of less than 0.27 °C from rectal temperature during exercise, which is the level of accuracy required to minimize the possibility of failing to identify dangerous hyperthermia (Casa et al. 2007; Ganio et al. 2009). The most accurate methods (e.g., pulmonary artery, esophageal, rectal, and ingestible thermistor) are not feasible for constant, real-time assessment, and at this time we do not believe a suitable solution that meets the rigor of acceptable standards can be recommended at this time (Casa et al. 2007; Ganio et al. 2009).
As technological development in this area emerge, emphasis should be given to long-term observations in acute heat-health outcomes (e.g., dehydration, elevated core temperature) associated with prolonged exposure to extreme heat, which are crucial for improving the current AMGs through evidence-based statistical analyses. Such long-term monitoring of health impacts would improve understanding the acute, chronic, or delayed impacts of extreme heat exposure. For example, victims of previous EHI may also be more vulnerable to future heat-related incidents: long-term monitoring could help explain this connection (Stacey et al. 2015; Nelson et al. 2018). Furthermore, chronic kidney disease (CKD) is found to be associated with prolonged exposure to high heat and dehydration, and is one of the first documented health epidemics associated with climate change (Glaser et al. 2016). Research into the cause and origin of CKD is ongoing; a recent comprehensive review indicates that occupational heat exposure may (Wesseling et al. 2013) or may not be (Herath et al. 2018) a causal factor. Further long-term studies are needed.
Considerations for individual circumstances and special populations
A paucity of research is available surrounding special considerations for individuals with potential heat vulnerabilities. Individual vulnerabilities include: those with chronic diseases (Nerbass et al. 2017) or taking medications that decrease the ability to thermoregulate (Leon and Bouchama 2015), amputees (Klenck and Gebke 2007; Ghoseiri and Safari 2014), persons with spinal cord injuries (Bhambhani 2002; Griggs et al. 2015), persons with mental disabilities (Patel and Greydanus 2010), children and elderly (Leon and Bouchama 2015), those with diabetes (Kenny et al. 2016), and individuals with previous EHI (including exertional heat stroke) (Stacey et al. 2015). Collecting real-time physiological data on such populations would be important in assessing approaches for mitigating the modifiable risks. In a health care setting, ensuring such information is collected via clinical reporting, is linked to outcome information such as ICD (International Classification of Diseases) codes, and is accessible to researchers regardless of the health system of origin, would support much larger studies. Furthermore, at a policy level, robust representation of vulnerability characteristics in censuses and the American Community Survey would enable longer-term planning and preparedness when matched with environmental exposure predictions.
Mathematical modeling of real-time data
Sensor technologies measuring internal temperature, sweat and heart rate, and other biometrics, coupled with mathematical predictive models, could potentially minimize the incidence of heat injuries. Although AMGs are critical for limiting the numbers of heat injuries during various types of physical training, early recognition of an individual’s heat load will be key in the future. Indirect methods of predicting internal body temperature by using noninvasive methods have been investigated; however, validity of these models requires further research (Buller et al. 2015). Furthermore, current models lack the outcomes-based research necessary to function as standalone tools in the environment laborers, warfighters, and athletes require. The relationship between modeled or measured physiological strain and necessary interventions to modify that strain is poorly understood. For example, ACGH TLWs are modeled on the basis of keeping body temperature less than 38.5 °C, but little evidence is available to support this threshold temperature.
Researchers (Gribok et al. 2007, 2008, 2010; Laxminarayan et al. 2015) have developed data-driven models (artificial neural networks and autoregression), which use time series of recent-past measurements of internal temperature (via ingestible pills) to predict when activity modifications and cooling strategies should be applied. Their latest model suggested a 20-min auto-regressive model prediction window and a temperature alert threshold of 39 °C could be useful (Laxminarayan et al. 2015). They concluded these parameters should be sufficient to ensure legitimate alerts and allow for proactive interventions. Future research should focus on investigating the potential role of other physiological measures coupled with perceptions of heat load in the mathematical models. Importantly, individual monitoring under various environmental and exercise conditions could be used to develop algorithms for tracking risk of heat stress and predicting the need for activity modifications. Such approaches have already been tested for learning how to distinguish a wounded and bleeding Service member from one who is engaged in exercise or differentiating central hypovolemia from physical activity (Rickards et al. 2014). The same concepts could be pursued for predicting who will be at risk for EHI. Ultimately, a system capable of reliably predicting individual physiologic and perceived strain and generating alerts to modify activity and institute cooling strategies real-time will be essential for reducing the morbidity and mortality associated with EHIs. Importantly, qualitative data for perceived discomfort and effort should also be collected in future research as they are key features of heat exposure and EHI risk. Furthermore, once an accurate methodology is established, additional considerations should be made to address items such as information overload, usability in varying environmental conditions, how the tool will be used to make decisions and take actions, battery power, durability, and data security.
Environmental predictions
Provided ample lead time and planning, extreme heat exposure can often be prevented in athletic, occupational, and military settings (e.g., by rescheduling practices and games, installing shade at a worksite, shortening total exposure time). Predictions of weather and climate variables such as temperature, humidity, wind speed, and cloud cover (the inverse of solar exposure) can be employed to make determinations about these protective actions at many timescales. However, these predictions vary in skill not only across parameters (Haiden et al. 2015), but also in time and space (Becker et al. 2014). The use of recurring climate patterns, such as the El Nino Southern Oscillation (ENSO), as data source improve predictions in some regions of the world (Arribas et al. 2010), but are also known to succumb to “predictability barriers” at certain times of year (Duan and Wei 2013).
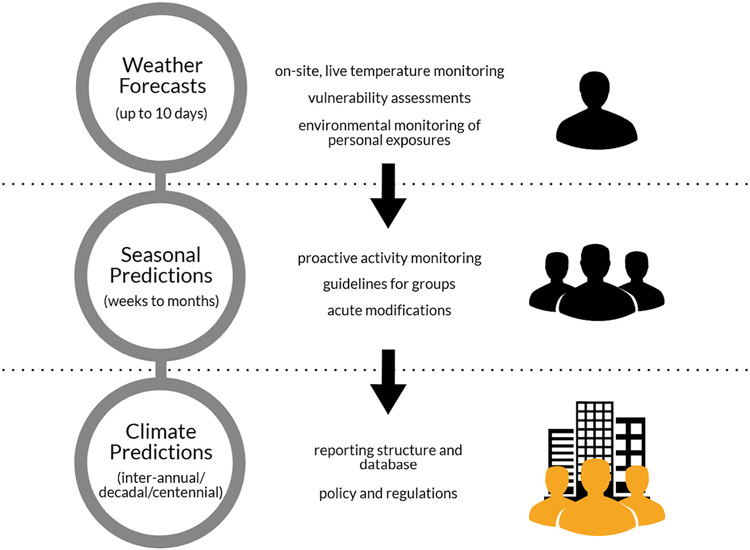
Research is needed to improve predictions of these complementary environmental variables to facilitate the forecasts of several heat indices which could supplement direct measurements in real-time as well as improve early warning, planning, and preparedness (Fig. 2). Additionally, as these variables are often combined to derive more complex indices such as WBGT or UTCI, more research into the predictability of complex indices using the forecasted complementary environmental variables is needed. Social science research on improving forecast communications to the public, including the provision of accompanying uncertainty information, would improve the utility of existing and novel prediction products at this scale.
Fig. 2.
A model illustrating different time scales of environmental observations and their relations to extreme heat management strategies
Of particular note are forecasts at the seasonal to sub-seasonal scale (S2S). S2S predictions fill a gap between short-term deterministic weather forecasts and longer-term, probabilistic seasonal to inter-annual predictions. These predictions have improved dramatically over the past several decades as a result of strong investment in understanding climate modes which operate at this time scale (Vitart and Robertson 2018), community modeling exercises (Mariotti et al. 2018), and sustained observations (McPhaden et al. 2009), and this presents new opportunities to use information that had not yet been previously available (White et al. 2017). Predictions 3–4 weeks in advance, and monthly to seasonal predictions, could be used to make scheduling decisions and to alert managers to evaluate acclimatization and readiness in advance of extreme heat, if the information meets the user needs identified through field exploration and application (Ray and Webb 2016). For that reason, improvements in user perceptions and communication strategies should not be neglected when considering the environmental prediction delivery methods.
Climate predictions, such as those already issued by the US National Climate Assessment and the Intergovernmental Panel on Climate Change, are useful in a general sense (USGCRP 2018), but additional research on the impacts of extreme heat for the vulnerable groups identified here, and adaptive strategies to address them, are needed in order to make interventions less reactive and more proactive—including changing policies and regulations governing how urban areas are developed. Additionally, more usable fine-scale spatial predictions and applications of climate information developed in close consultation with those who make decisions to protect these vulnerable groups.
Economic impacts of extreme heat mediated by activity modification
Beyond the need for adequate health data, limited information is available concerning the economic impact of implementing heat AMGs. The decline in economic productivity due to rising temperature is related to labor supply (Graff Zivin and Neidell 2014) and labor productivity (Hsiang 2010). Although an increasing number of research studies have addressed the economic productivity concerns of working in hot environments (Kjellstrom et al. 2009; Dunne et al. 2013; Stoecklin-Marois et al. 2013; Zander et al. 2015), minimal research has explored either the compliance costs or the intersection of climate extremes, health, and economics, and/or historical/projected trends at these intersections.
Importantly, further research is also needed to express the potential compliance costs and benefits to those using AMGs. Compliance costs in the context of heat activity guidelines refer to the financial cost burden for time lost because of heat injury and lost worker output due to conforming to extreme heat guidelines (Nerbass et al. 2017). Dunne et al. (Dunne et al. 2013) reported that “heat stress impaired global labor capacity by up to 10%”, and the 2012 DARA and Climate Vulnerable Forum report (DARA 2012) estimated net costs of USD $2.4 trillion by 2030 attributed to heat-related reductions in work productivity alone. A comparative review of the costs of AMGs versus heat casualties has not been identified and is needed. In addition to occupational compliance costs, compliance costs in athletics can result in high social and monetary costs of postponing or canceling a sporting event. To balance costs versus health risks, studies to examine the external validity of WBGT or other indicators for inferring the extent of economic impact are warranted.
The future effectiveness of activity modification guidelines
The frequency, intensity, and duration of heat waves are increasing and today’s AMGs may not be enough to keep people safe under future conditions. The need for proactive usage of AMGs based on mathematical models, forecasts, and other data may be further increased in the future to determine event and work cancelations (Hinkson 2017). In some places, there may not be enough “safe” days to conduct physical activity/labor if we follow the current guidelines due to the worsening of extreme heat condition (Grundstein et al. 2013). Additionally, guidelines surrounding cumulative heat stress may be needed as there may be fewer days where individuals are reprieved from high heat in the future (Wallace et al. 2005). Integration of physiological and biometeorological factors will help individuals identify the timing for optimal productivity while still accounting for safety. This is particularly important if the magnitude of heat stress continues to intensify and temperature levels reach those of uncompensable heat stress by human thermoregulatory system. In such a scenario, behavioral modifications to balance the heat stress from physiological and biometeorological influence are key.
Conclusion
Various heat indices and AMGs have been introduced to the athletic, occupational, and military settings to safeguard the health and optimize the work environment for athletes, laborers, and warfighters. Future interagency collaboration to advance heat mitigation plans among physically active population is desired to maximize the existing resources and data to facilitate advancement in AMGs for environmental heat. Specifically, the following key points should be considered. Agencies should: (1) learn from each other’s AMGs and related experiences, (2) leverage data collection and research capabilities to engage in more formal collaboration, and (3) continue dialoguing and utilize the Delphi technique to ultimately come to a consensus regarding AMGs for heat. Whereas AMGs have allowed governing organizations to systematically address the heat stress, further improvements are warranted to quantify the effectiveness of such AMGs, integrate physiological and biometeorological components, and reduce the assumptions and limitations in current models.
Acknowledgements
We would like to thank the National Integrated Heat Health Information System for their support in hosting the expert meeting that preceded to the writing of this paper. We would also like to acknowledge Dr. Richard J. Thomas and Dr. Aaron W. Tustin for their contributions in writing the paper.
Footnotes
Disclaimer The scientific results, views, and conclusions expressed in this publication are those of the author(s) and do not reflect the official policy or position of the Department of the Army, Department of Defense, National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC), National Weather Service (NWS), National Oceanic and Atmospheric Administration (NOAA), Department of Commerce, or the US Government.
References
- ACGIH (2017) TLVs and BEIs: threshold limit values for chemical substances and physical agents and biological exposure indices. American Conference of Governmental Industrial Hygienists [Google Scholar]
- Adams WM, Mazerolle SM, Casa DJ, Huggins RA, Burton L (2014) The secondary school football coach’s relationship with the athletic trainer and perspectives on exertional heat stroke. J Athl Train 49:469–477. 10.4085/1062-6050-49.3.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams WM, Hosokawa Y, Casa DJ (2016) Body-cooling paradigm in sport: maximizing safety and performance during competition. J Sport Rehabil 25:382–394. 10.1123/jsr.2015-0008 [DOI] [PubMed] [Google Scholar]
- Adams WM, Scarneo SE, Casa DJ (2017) State-level implementation of health and safety policies to prevent sudden death and catastrophic injuries within secondary school athletics. Orthop J Sports Med 5: 2325967117727262. 10.1177/2325967117727262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Meteorological Society (2018) “Air temperature” Glossary of Meteorology. http://glossary.ametsoc.org/wiki/Air_temperature. Accessed 14 Oct 2018 [Google Scholar]
- Anderson SR (1965) Humidex calculation. Atmospheric Environment Service of Canada, C.D.S., Toronto, pp 24–65 [Google Scholar]
- Arbury S, Lindsley M, Hodgson M (2016) A critical review of OSHA heat enforcement cases: lessons learned. J Occup Environ Med 58: 359–363. 10.1097/JOM.0000000000000640 [DOI] [PubMed] [Google Scholar]
- Armed Forces Health Surveillance Branch (2017) Armed Forces reportable medical events guidlines and case definitions [Google Scholar]
- Armed Forces Health Surveillance Bureau (2017) Update: heat illness, active component, U.S. armed forces, 2016. MSMR 24:9–13 [Google Scholar]
- Armstrong LE, Maresh CM (1991) The induction and decay of heat acclimatisation in trained athletes. Sports Med 12:302–312 [DOI] [PubMed] [Google Scholar]
- Armstrong LE, Casa DJ, Millard-Stafford M et al. (2007) American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc 39:556–572. 10.1249/MSS.0b013e31802fa199 [DOI] [PubMed] [Google Scholar]
- Armstrong LE, Johnson EC, Casa DJ, Ganio MS, McDermott BP, Yamamoto LM, Lopez RM, Emmanuel H (2010) The American football uniform: uncompensable heat stress and hyperthermic exhaustion. J Athl Train 45:117–127. 10.4085/1062-6050-45.2.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Army USGU (2014) Army techniques publication ATP 5-19 risk management April 2014. CreateSpace Independent Publishing Platform, Scotts Valley [Google Scholar]
- Arribas A, Glover M, Maidens A, Peterson K, Gordon M, MacLachlan C, Graham R, Fereday D, Camp J, Scaife AA, Xavier P, McLean P, Colman A, Cusack S (2010) The GloSea4 ensemble prediction system for seasonal forecasting. Mon Weather Rev 139:1891–1910. 10.1175/2010MWR3615.1 [DOI] [Google Scholar]
- Attanasio SM, Adams WM, Stearns RL et al. (2016) Occurrence of exertional heat stroke in high school football athletes before and after implementation of evidence based heat acclimatization guidelines. J Athl Train 51:S168 [Google Scholar]
- Bailes JE, Cantu RC, Day AL (2002) The neurosurgeon in sport: awareness of the risks of heatstroke and dietary supplements. Neurosurgery 51:283–286 discussion 286-288 [PubMed] [Google Scholar]
- Bair FE, Ruffner J (1977) The weather almanac. Harpercollins [Google Scholar]
- Balmain BN, Sabapathy S, Jay O, Adsett J, Stewart GM, Jayasinghe R, Morris NR (2017) Heart failure and thermoregulatory control: can patients with heart failure handle the heat? J Card Fail 23:621–627. 10.1016/j.cardfail.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Bandodkar AJ, Molinnus D, Mirza O, Guinovart T, Windmiller JR, Valdés-Ramírez G, Andrade FJ, Schöning MJ, Wang J (2014) Epidermal tattoo potentiometric sodium sensors with wireless signal transduction for continuous non-invasive sweat monitoring. Biosens Bioelectron 54:603–609. 10.1016/j.bios.2013.11.039 [DOI] [PubMed] [Google Scholar]
- Becker E, van den Dool H, Zhang Q (2014) Predictability and forecast skill in NMME. J Clim 27:5891–5906. 10.1175/JCLI-D-13-00597.1 [DOI] [Google Scholar]
- Bedno SA, Urban N, Boivin MR, Cowan DN (2014) Fitness, obesity and risk of heat illness among army trainees. Occup Med Oxf Engl 64:461–467. 10.1093/occmed/kqu062 [DOI] [PubMed] [Google Scholar]
- Bergeron MF, McKeag DB, Casa DJ et al. (2005) Youth football: heat stress and injury risk. Med Sci Sports Exerc 37:1421–1430 [DOI] [PubMed] [Google Scholar]
- Bhambhani Y (2002) Physiology of wheelchair racing in athletes with spinal cord injury. Sports Med Auckl NZ 32:23–51 [DOI] [PubMed] [Google Scholar]
- Bröde P, Fiala D, Błazejczyk K, Holmér I, Jendritzky G, Kampmann B, Tinz B, Havenith G (2012) Deriving the operational procedure for the Universal Thermal Climate Index (UTCI). Int J Biometeorol 56:481–494. 10.1007/s00484-011-0454-1 [DOI] [PubMed] [Google Scholar]
- Bröde P, Fiala D, Kampmann B (2017) Considering varying clothing, activities and exposure times with the Universal Thermal Climate Index UTCI. Durham, UK, p 57, Sept 2017 [Google Scholar]
- Brotherhood JR (2008) Heat stress and strain in exercise and sport. J Sci Med Sport Sports Med Aust 11:6–19. 10.1016/j.jsams.2007.08.017 [DOI] [PubMed] [Google Scholar]
- Budd GM (2008) Wet-bulb globe temperature (WBGT)—its history and its limitations. J Sci Med Sport Sports Med Aust 11:20–32. 10.1016/j.jsams.2007.07.003 [DOI] [PubMed] [Google Scholar]
- Buller MJ, Tharion WJ, Duhamel CM, Yokota M (2015) Real-time core body temperature estimation from heart rate for first responders wearing different levels of personal protective equipment. Ergonomics 58:1830–1841. 10.1080/00140139.2015.1036792 [DOI] [PubMed] [Google Scholar]
- Canadian Centre for Occupational Health and Safety (2016) Humidex Rating and Work. https://www.ccohs.ca/oshanswers/phys_agents/humidex.html. Accessed 12 Dec 2017 [Google Scholar]
- Carter R, Cheuvront SN, Williams JO et al. (2005) Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc 37:1338–1344 [DOI] [PubMed] [Google Scholar]
- Carter MR, McGinn R, Barrera-Ramirez J et al. (2014) Impairments in local heat loss in type 1 diabetes during exercise in the heat. Med Sci Sports Exerc 46:2224–2233. 10.1249/MSS.0000000000000350 [DOI] [PubMed] [Google Scholar]
- Casa DJ, Becker SM, Ganio MS, Brown CM, Yeargin SW, Roti MW, Siegler J, Blowers JA, Glaviano NR, Huggins RA, Armstrong LE, Maresh CM (2007) Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train 42:333–342 [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, Csillan D, Inter-Association Task Force for Preseason Secondary School Athletics Participants et al. (2009) Preseason heat-acclimatization guidelines for secondary school athletics. J Athl Train 44:332–333. 10.4085/1062-6050-44.3.332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, Anderson SA, Baker L, Bennett S, Bergeron MF, Connolly D, Courson R, Drezner JA, Eichner ER, Epley B, Fleck S, Franks R, Guskiewicz KM, Harmon KG, Hoffman J, Holschen JC, Jost J, Kinniburgh A, Klossner D, Lopez RM, Martin G, McDermott BP, Mihalik JP, Myslinski T, Pagnotta K, Poddar S, Rodgers G, Russell A, Sales L, Sandler D, Stearns RL, Stiggins C, Thompson C (2012a) The inter-association task force for preventing sudden death in collegiate conditioning sessions: best practices recommendations. J Athl Train 47:477–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, Guskiewicz KM, Anderson SA, Courson RW, Heck JF, Jimenez CC, McDermott BP, Miller MG, Stearns RL, Swartz EE, Walsh KM (2012b) National athletic trainers’ association position statement: preventing sudden death in sports. J Athl Train 47:96–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, Almquist J, Anderson SA, Baker L, Bergeron MF, Biagioli B, Boden B, Brenner JS, Carroll M, Colgate B, Cooper L, Courson R, Csillan D, DeMartini JK, Drezner JA, Erickson T, Ferrara MS, Fleck SJ, Franks R, Guskiewicz KM, Holcomb WR, Huggins RA, Lopez RM, Mayer T, McHenry P, Mihalik JP, O'Connor FG, Pagnotta KD, Pryor RR, Reynolds J, Stearns RL, Valentine V (2013) The inter-association task force for preventing sudden death in secondary school athletics programs: best-practices recommendations. J Athl Train 48:546–553. 10.4085/1062-6050-48.4.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, DeMartini JK, Bergeron MF et al. (2015) National Athletic Trainers’ Association position statement: exertional heat illnesses. J Athl Train 50:986–1000. 10.4085/1062-6050-50.9.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadio JR, Kilding AE, Cotter JD, Laursen PB (2017) From lab to real world: heat acclimation considerations for elite athletes. Sports Med 47:1467–1476. 10.1007/s40279-016-0668-9 [DOI] [PubMed] [Google Scholar]
- CDC (2008) Heat-related deaths among crop workers– United States, 1992–2006. Morb Mortal Wkly Rep 57:649–653 [PubMed] [Google Scholar]
- Cheuvront SN, Carter R, Castellani JW, Sawka MN (2005) Hypohydration impairs endurance exercise performance in temperate but not cold air. J Appl Physiol Bethesda Md 1985 99:1972–1976. 10.1152/japplphysiol.00329.2005 [DOI] [PubMed] [Google Scholar]
- Cheuvront SN, Caruso EM, Heavens KR et al. (2015) Effect of WBGT index measurement location on heat stress category classification. Med Sci Sports Exerc 47:1958–1964. 10.1249/MSS.0000000000000624 [DOI] [PubMed] [Google Scholar]
- Choi J, Ghaffari R, Baker LB, Rogers JA (2018) Skin-interfaced systems for sweat collection and analytics. Sci Adv 4:eaar3921. 10.1126/sciadv.aar3921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleary M (2007) Predisposing risk factors on susceptibility to exertional heat illness: clinical decision-making considerations. J Sport Rehabil 16:204–214 [DOI] [PubMed] [Google Scholar]
- Cook EL (1955) Epidemiological approach to heat trauma. Mil Med 116:317–322 [PubMed] [Google Scholar]
- Cooper ER, Ferrara MS, Casa DJ, Powell JW, Broglio SP, Resch JE, Courson RW (2016) Exertional heat illness in American football players: when is the risk greatest? J Athl Train 51:593–600. 10.4085/1062-6050-51.8.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello JT, Stewart KL, Stewart IB (2015) Inside the “hurt locker”: the combined effects of explosive ordnance disposal and chemical protective clothing on physiological tolerance time in extreme environments. Ann Occup Hyg 59:922–931. 10.1093/annhyg/mev029 [DOI] [PubMed] [Google Scholar]
- Crimmins A, Balbus J, Gamble J, et al. (2016) Impacts of climate change on human health in the United States: a scientific assessment. https://cfpub.epa.gov/si/si_public_record_report.cfm?dirEntryID=291975. Accessed 19 Dec 2017 [Google Scholar]
- d’Ambrosio Alfano FR, Palella BI, Riccio G (2011) Thermal environment assessment reliability using temperature–humidity indices. Ind Health 49:95–106 [DOI] [PubMed] [Google Scholar]
- d’Ambrosio Alfano FR, Malchaire J, Palella BI, Riccio G (2014) WBGT index revisited after 60 years of use. Ann Occup Hyg 58:955–970. 10.1093/annhyg/meu050 [DOI] [PubMed] [Google Scholar]
- Daanen HAM, Racinais S, Périard JD (2018) Heat acclimation decay and re-induction: a systematic review and meta-analysis. Sports Med Auckl NZ 48:409–430. 10.1007/s40279-017-0808-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- DARA (2012) Climate vulnerability monitor 2nd Edition. A guide to the cold calculus of a hot planet [Google Scholar]
- Department of the Army Headquarters (2016) Prevention of heat and cold casualties [Google Scholar]
- Dorman LE, Havenith G (2009) The effects of protective clothing on energy consumption during different activities. Eur J Appl Physiol 105:463–470. 10.1007/s00421-008-0924-2 [DOI] [PubMed] [Google Scholar]
- Duan W, Wei C (2013) The ‘spring predictability barrier’ for ENSO predictions and its possible mechanism: results from a fully coupled model. Int J Climatol 33:1280–1292. 10.1002/joc.3513 [DOI] [Google Scholar]
- Düking P, Hotho A, Holmberg H-C, Fuss FK, Sperlich B (2016) Comparison of non-invasive individual monitoring of the training and health of athletes with commercially available wearable technologies. Front Physiol 7:71. 10.3389/fphys.2016.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunne JP, Stouffer RJ, John JG (2013) Reductions in labour capacity from heat stress under climate warming. Nat Clim Chang 3:563–566 [Google Scholar]
- Epstein Y, Moran DS (2006) Thermal comfort and the heat stress indices. Ind Health 44:388–398 [DOI] [PubMed] [Google Scholar]
- Fleischer NL, Tiesman HM, Sumitani J, Mize T, Amarnath KK, Bayakly AR, Murphy MW (2013) Public health impact of heat-related illness among migrant farmworkers. Am J Prev Med 44:199–206. 10.1016/j.amepre.2012.10.020 [DOI] [PubMed] [Google Scholar]
- Gagnon D, Romero SA, Cramer MN et al. (2017) Age modulates physiological responses during fan use under extreme heat and humidity. Med Sci Sports Exerc 49:2333–2342. 10.1249/MSS.0000000000001348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganio MS, Brown CM, Casa DJ, Becker SM, Yeargin SW, McDermott BP, Boots LM, Boyd PW, Armstrong LE, Maresh CM (2009) Validity and reliability of devices that assess body temperature during indoor exercise in the heat. J Athl Train 44:124–135. 10.4085/1062-6050-44.2.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgia High School Association (2016) Practice policy for heat and humidity. https://www.ghsa.net/practice-policy-heat-and-humidity. Accessed 8 Sep 2016 [Google Scholar]
- Ghoseiri K, Safari MR (2014) Prevalence of heat and perspiration discomfort inside prostheses: literature review. J Rehabil Res Dev 51:855–868. 10.1682/JRRD.2013.06.0133 [DOI] [PubMed] [Google Scholar]
- Glaser J, Lemery J, Rajagopalan B, Diaz HF, García-Trabanino R, Taduri G, Madero M, Amarasinghe M, Abraham G, Anutrakulchai S, Jha V, Stenvinkel P, Roncal-Jimenez C, Lanaspa MA, Correa-Rotter R, Sheikh-Hamad D, Burdmann EA, Andres-Hernando A, Milagres T, Weiss I, Kanbay M, Wesseling C, Sánchez-Lozada LG, Johnson RJ (2016) Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol CJASN 11:1472–1483. 10.2215/CJN.13841215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling SN, Bryce EK, Dixon PG et al. (2014) A glossary for biometeorology. Int J Biometeorol 58:277–308. 10.1007/s00484-013-0729-9 https://www.ncbi.nlm.nih.gov/pubmed/24550042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada (2017) Criteria for public weather alerts. https://www.canada.ca/en/environment-climate-change/services/types-weather-forecasts-use/public/criteria-alerts.html#heat. Accessed 14 Dec 2017 [Google Scholar]
- Graff Zivin J, Neidell M (2014) Temperature and the allocation of time: implications for climate change. J Labor Econ 32:1–26 [Google Scholar]
- Gribok AV, Buller MJ, Hoyt RW, Reifman J (2007) Providing statistical measures of reliability for body core temperature predictions. Conf Proc Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf 2007:545–548. 10.1109/IEMBS.2007.4352348 [DOI] [PubMed] [Google Scholar]
- Gribok AV, Buller MJ, Reifman J (2008) Individualized short-term core temperature prediction in humans using biomathematical models. IEEE Trans Biomed Eng 55:1477–1487. 10.1109/TBME.2007.913990 [DOI] [PubMed] [Google Scholar]
- Gribok AV, Buller MJ, Hoyt RW, Reifman J (2010) A real-time algorithm for predicting core temperature in humans. IEEE Trans Inf Technol Biomed Publ IEEE Eng Med Biol Soc 14:1039–1045. 10.1109/TITB.2010.2043956 [DOI] [PubMed] [Google Scholar]
- Griggs KE, Leicht CA, Price MJ, Goosey-Tolfrey VL (2015) Thermoregulation during intermittent exercise in athletes with a spinal-cord injury. Int J Sports Physiol Perform 10:469–475. 10.1123/ijspp.2014-0361 [DOI] [PubMed] [Google Scholar]
- Grundstein AJ, Ramseyer C, Zhao F, Pesses JL, Akers P, Qureshi A, Becker L, Knox JA, Petro M (2012) A retrospective analysis of American football hyperthermia deaths in the United States. Int J Biometeorol 56:11–20. 10.1007/s00484-010-0391-4 [DOI] [PubMed] [Google Scholar]
- Grundstein A, Elguindi N, Cooper E, Ferrara MS (2013) Exceedance of wet bulb globe temperature safety thresholds in sports under a warming climate. Clim Res 58:183–191. 10.3354/cr01199 [DOI] [Google Scholar]
- Gubernot DM, Anderson GB, Hunting KL (2015) Characterizing occupational heat-related mortality in the United States, 2000–2010: an analysis using the census of fatal occupational injuries database. Am J Ind Med 58:203–211. 10.1002/ajim.22381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Yu Y, Xiang T, Li H, Zhang D (2017) The availability of wearable-device-based physical data for the measurement of construction workers’ psychological status on site: from the perspective of safety management. Autom Constr 82:207–217. 10.1016/j.autcon.2017.06.001 [DOI] [Google Scholar]
- Havenith G, Fiala D (2015) Thermal Indices and Thermophysiological Modeling for Heat Stress. Compr Physiol 6:255–302 [DOI] [PubMed] [Google Scholar]
- Haiden T, Forbes R, Ahlgrimm M, Bozzo A (2015) The skill of ECMWF cloudiness forecasts [Google Scholar]
- Hawkins MD, Brown V, Ferrell J (2016) Assessment of NOAA national weather service methods to warn for extreme heat events. Weather Clim Soc 9:5–13. 10.1175/WCAS-D-15-0037.1 [DOI] [Google Scholar]
- Hawkins MD, Brown V, Ferrell J (2017) Assessment of NOAA National Weather Service methods to warn for extreme heat events. Weather Clim Soc 9:5–13 [Google Scholar]
- Headquarters, Department of the Army and Air Force (2013) TB MED 507: heat stress control and heat casualty management [Google Scholar]
- Headquarters, Departments of the Army And Air Force (1980) TB MED 507 NAVMED P-5052-5 AFP 160–1 [Google Scholar]
- Headquarters, Departments of the Army And Air Force (2003) Heat Stress control and heat casualty management [Google Scholar]
- Herath C, Jayasumana C, De Silva PMCS et al. (2018) Kidney diseases in agricultural communities: a case against heat-stress nephropathy. Kidney Int Rep 3:271–280. 10.1016/j.ekir.2017.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinkson K (2017) Runners’ health behind decision to cancel Montreal marathon, organizers say. In: CBC News. http://www.cbc.ca/news/canada/montreal/montreal-marathon-cancelled-1.4300019. Accessed 2 Jan 2018 [Google Scholar]
- Hosokawa Y, Casa DJ, Rosenberg H, Capacchione JF, Sagui E, Riazi S, Belval LN, Deuster PA, Jardine JF, Kavouras SA, Lee EC, Miller KC, Muldoon SM, O'Connor FG, Sailor SR, Sambuughin N, Stearns RL, Adams WM, Huggins RA, Vandermark LW (2017) Round table on malignant hyperthermia in physically active populations: meeting proceedings. J Athl Train 52:377–383. 10.4085/1062-6050-52.2.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosokawa Y, Grundstein AJ, Vanos JK, Cooper E (2018) Environmental condition and monitoring. In: Sport and physical activity in the heat - maximizing performance and safety, 1st edn. Springer, Berlin [Google Scholar]
- Hsiang SM (2010) Temperatures and cyclones strongly associated with economic production in the Caribbean and Central America. Proc Natl Acad Sci 107:15367–15372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins RA, Scarneo SE, Casa DJ, Belval LN, Carr KS, Chiampas G, Clayton M, Curtis RM, Duffy AJ III, Flury A, Gammons M, Hosokawa Y, Jardine JF, LaBella CR, Oats R, Ransone JW, Sailor SR, Scott K, Stearns RL, Vandermark LW, Weston T (2017) The inter-association task force document on emergency health and safety: best-practice recommendations for youth sports leagues. J Athl Train 52:384–400. 10.4085/1062-6050-52.2.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins RA, Adams WM, Buller MJ, Looney DP (2018) Chapter 10 technology. In: Sport and physical activity in the heat: maximizing performance and safety. Springer, Berlin, pp 163–190 [Google Scholar]
- International Organization for Standardization (2017) ISO 7243 Ergonomics of the thermal environment– Assessment of heat stress using the WBGT (wet bulb globe temperature) index [Google Scholar]
- ISO7933 (2004) Ergonomics of the thermal environment—analytical determination and interpretation of heat stress using calculation of the predicted heat strain [Google Scholar]
- Jackson LL, Rosenberg HR (2010) Preventing heat-related illness among agricultural workers. J Agromedicine 15:200–215. 10.1080/1059924X.2010.487021 [DOI] [PubMed] [Google Scholar]
- James CA, Richardson AJ, Watt PW, Willmott AGB, Gibson OR, Maxwell NS (2017) Short-term heat acclimation improves the determinants of endurance performance and 5-km running performance in the heat. Appl Physiol Nutr Metab Physiol Appl Nutr Metab 42:285–294. 10.1139/apnm-2016-0349 [DOI] [PubMed] [Google Scholar]
- Jay O, Brotherhood JR (2016) Occupational heat stress in Australian workplaces. Temperature 3:394–411. 10.1080/23328940.2016.1216256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O (2010) Heat stress in older individuals and patients with common chronic diseases. CMAJ Can Med Assoc J J Assoc Medicale Can 182:1053–1060. 10.1503/cmaj.081050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny GP, Sigal RJ, McGinn R (2016) Body temperature regulation in diabetes. Temp Austin Tex 3:119–145. 10.1080/23328940.2015.1131506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr ZY, Casa DJ, Marshall SW, Comstock RD (2013) Epidemiology of exertional heat illness among U.S. high school athletes. Am J Prev Med 44:8–14. 10.1016/j.amepre.2012.09.058 [DOI] [PubMed] [Google Scholar]
- Kerr ZY, Marshall SW, Comstock RD, Casa DJ (2014) Implementing exertional heat illness prevention strategies in US high school football. Med Sci Sports Exerc 46:124–130. 10.1249/MSS.0b013e3182a11f45 [DOI] [PubMed] [Google Scholar]
- Kjellstrom T, Kovats RS, Lloyd SJ, Holt T, Tol RSJ (2009) The direct impact of climate change on regional labor productivity. Arch Environ Occup Health 64:217–227 [DOI] [PubMed] [Google Scholar]
- Klenck C, Gebke K (2007) Practical management: common medical problems in disabled athletes. Clin J Sport Med Off J Can Acad Sport Med 17:55–60. 10.1097/JSM.0b013e3180302587 [DOI] [PubMed] [Google Scholar]
- Koh A, Kang D, Xue Y et al. (2016) A soft, wearable microfluidic device for the capture, storage, and colorimetric sensing of sweat. Sci Transl Med 8:366ra165. 10.1126/scitranslmed.aaf2593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuras ER, Richardson MB, Calkins MM, Ebi KL, Hess JJ, Kintziger KW, Jagger MA, Middel A, Scott AA, Spector JT, Uejio CK, Vanos JK, Zaitchik BF, Gohlke JM, Hondula DM (2017) Opportunities and challenges for personal heat exposure research. Environ Health Perspect 125:085001. 10.1289/EHP556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsberg HE, World Meteorological Organization (1972) The assessment of human bioclimate: a limited review of physical parameters. Secretariat of the World Meteorological Organization, Geneva [Google Scholar]
- Laxminarayan S, Buller MJ, Tharion WJ, Reifman J (2015) Human Core temperature prediction for heat-injury prevention. IEEE J Biomed Health Inform 19:883–891. 10.1109/JBHI.2014.2332294 [DOI] [PubMed] [Google Scholar]
- Lemke B, Kjellstrom T (2012) Calculating workplace WBGT from meteorological data: a tool for climate change assessment. Ind Health 50:267–278 [DOI] [PubMed] [Google Scholar]
- Leon LR, Bouchama A (2015) Heat stroke. Compr Physiol 5:611–647. 10.1002/cphy.c140017 [DOI] [PubMed] [Google Scholar]
- Li Y, Wang Y, Ma L (2014) An association study of CASQ1 gene polymorphisms and heat stroke. Genomics Proteomics Bioinformatics 12:127–132. 10.1016/j.gpb.2014.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malchaire J, Piette A, Kampmann B, Mehnert P, Gebhardt H, Havenith G, den Hartog E, Holmer I, Parsons K, Alfano G, Griefahn B (2001) Development and validation of the predicted heat strain model. Ann Occup Hyg 45:123–135 [PubMed] [Google Scholar]
- Mariotti A, Ruti PM, Rixen M (2018) Progress in subseasonal to seasonal prediction through a joint weather and climate community effort. Npj Clim Atmospheric Sci 1:4. 10.1038/s41612-018-0014-z [DOI] [Google Scholar]
- Masterton JM, Richardson FA (1979) Huidex: A method of quantifying human discomfort due to excessive heat and humidity. CLI 1–7, Environment Canada, Downsview, Ontario. [Google Scholar]
- McDermott BP, Casa DJ, Ganio MS et al. (2009) Acute whole-body cooling for exercise-induced hyperthermia: a systematic review. J Athl Train 44:84–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhaden MJ, Ando K, Bourlès B et al. (2009) The global tropical moored buoy array. Sustained ocean observations and information for society. Proc Ocean 2:459–480, ESA Publication WPP–306, Venice. 10.5270/OceanObs09.cwp.61 [DOI] [Google Scholar]
- Mears S, Watson P (2015) IIRM Medical Care Manual. International Institute for Race Medicine, Norfolk [Google Scholar]
- Miller V, Bates G, Schneider JD, Thomsen J (2011) Self-pacing as a protective mechanism against the effects of heat stress. Ann Occup Hyg 55:548–555. 10.1093/annhyg/mer012 [DOI] [PubMed] [Google Scholar]
- Minard D (1961) Prevention of heat casualties in Marine Corps recruits. Period of 1955-60, with comparative incidence rates and climatic heat stresses in other training categories. Mil Med 126:261–272 [PubMed] [Google Scholar]
- Ministry of the Environment Government of Japan Heat Illness Prevention Information (n.d.) In: Heat Stress Index WBGT. http://www.wbgt.env.go.jp/en/wbgt_data.php. Accessed 31 Aug 2018 [Google Scholar]
- Mitchell DC, Castro J, Armitage TL, Tancredi DJ, Bennett DH, Schenker MB (2018) Physical activity and common tasks of California farm workers: California Heat Illness Prevention Study (CHIPS). J Occup Environ Hyg:1–32. 10.1080/15459624.2018.1519319 [DOI] [PubMed] [Google Scholar]
- Moyen NE, Burchfield JM, Butts CL, Glenn JM, Tucker MA, Treece K, Smith AJ, McDermott BP, Ganio MS (2016) Effects of obesity and mild hypohydration on local sweating and cutaneous vascular responses during passive heat stress in females. Appl Physiol Nutr Metab Physiol Appl Nutr Metab 41:879–887. 10.1139/apnm-2016-0142 [DOI] [PubMed] [Google Scholar]
- Klossner D, National Collegiate Athletic Association (2013) 2013–14 NCAA sports medicine handbook, 24th edn. Indianapolis [Google Scholar]
- Navy and Marine Corps Public Health Center (2014) NAVMED P 5010-3 Prevention and heat and cold stress injuries [Google Scholar]
- Nelson DA, Deuster PA, O’Connor FG, Kurina LM (2018) Timing and predictors of mild and severe heat illness among new military enlistees. Med Sci Sports Exerc 50:1603–1612. 10.1249/MSS.0000000000001623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nerbass FB, Pecoits-Filho R, Clark WF, Sontrop JM, McIntyre CW, Moist L (2017) Occupational heat stress and kidney health: from farms to factories. Kidney Int Rep 2:998–1008. 10.1016/j.ekir.2017.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIOSH (2016) NIOSH criteria for a recommended standard: occupational exposure to heat and hot environments [Google Scholar]
- National Oceanic and Atmospheric Administration (2017) NWS Experimental HeatRisk. https://www.wrh.noaa.gov/wrh/heatrisk. Accessed 20 Dec 2017 [Google Scholar]
- Occupational Safety, Health Administration (2017a) OSHA Technical Manual (OTM) Section III: Chapter 4 - Heat stress. https://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_4.html. Accessed 24 Oct 2017 [Google Scholar]
- Occupational Safety and Health Administration (2017b) Severe injury reports. https://www.osha.gov/severeinjury/index.html. Accessed 19 Dec 2017 [Google Scholar]
- Pandolf KB (1979) Effects of physical training and cardiorespiratory physical fitness on exercise-heat tolerance: recent observations. Med Sci Sports 11:60–65 [PubMed] [Google Scholar]
- Parsons K (2014) Human thermal environments: the effects of hot, moderate, and cold environments on human health, comfort, and performance. CRC Press, Third Edition [Google Scholar]
- Patel DR, Greydanus DE (2010) Sport participation by physically and cognitively challenged young athletes. Pediatr Clin N Am 57:795–817. 10.1016/j.pcl.2010.03.002 [DOI] [PubMed] [Google Scholar]
- Pawelczyk J (2001) Neural control of skin and muscle blood flow during exercise and thermal stress. In: Gisolfi CV, Lamb DR, Nadel ER (eds) Exercise, heat and thermoregulation. Cooper Publishing Group, Traverse City [Google Scholar]
- Racinais S, Alonso J-M, Coutts AJ, Flouris AD, Girard O, González-Alonso J, Hausswirth C, Jay O, Lee JKW, Mitchell N, Nassis GP, Nybo L, Pluim BM, Roelands B, Sawka MN, Wingo J, Périard JD (2015) Consensus recommendations on training and competing in the heat. Sports Med 45:925–938. 10.1007/s40279-015-0343-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rav-Acha M, Hadad E, Epstein Y et al. (2004) Fatal exertional heat stroke: a case series. Am J Med Sci 328:84–87 [DOI] [PubMed] [Google Scholar]
- Ray AJ, Webb RS (2016) Understanding the user context: decision calendars as frameworks for linking climate to policy, planning, and decision-making. Climate in Context. Wiley-Blackwell, In, pp 27–50 [Google Scholar]
- Rickards CA, Vyas N, Ryan KL, Ward KR, Andre D, Hurst GM, Barrera CR, Convertino VA (2014) are you bleeding? Validation of a machine-learning algorithm for determination of blood volume status: application to remote triage. J Appl Physiol Bethesda Md 1985 116:486–494. 10.1152/japplphysiol.00012.2013 [DOI] [PubMed] [Google Scholar]
- Rothfusz LP (1990) The heat index “equation” (or more than you ever wanted to know about the heat index) [Google Scholar]
- Sahu S, Sett M, Kjellstrom T (2013) Heat exposure, cardiovascular stress and work productivity in rice harvesters in India: implications for a climate change future. Ind Health 51:424–431 [DOI] [PubMed] [Google Scholar]
- Sawka MN, Toner MM, Francesconi RP, Pandolf KB (1983) Hypohydration and exercise: effects of heat acclimation, gender, and environment. J Appl Physiol 55:1147–1153. 10.1152/jappl.1983.55.4.1147 [DOI] [PubMed] [Google Scholar]
- Schickele E (1947) Environment and fatal heat stroke; an analysis of 157 cases occurring in the Army in the U.S. during World War II. Mil Surg 100:235–256 [PubMed] [Google Scholar]
- Secretary of the Air Force (2016) Air Force Instruction 48–151 [Google Scholar]
- Smoljanic J, Morris NB, Dervis S, Jay O (2014) Running economy, not aerobic fitness, independently alters thermoregulatory responses during treadmill running. J Appl Physiol 117:1451–1459. 10.1152/japplphysiol.00665.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solis P, Vanos JK, Forbis RE (2017) The decision-making/accountability spatial incongruence problem for research linking environmental science and policy. Geogr Rev 107:680–704. 10.1111/gere.12240 [DOI] [Google Scholar]
- Stacey MJ, Parsons IT, Woods DR, Taylor PN, Ross D, J Brett S (2015) Susceptibility to exertional heat illness and hospitalisation risk in UK military personnel. BMJ Open Sport Exerc Med 1:e000055. 10.1136/bmjsem-2015-000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton JM, Poirier MP, Flouris AD, Boulay P, Sigal RJ, Malcolm J, Kenny GP (2015) Aging impairs heat loss, but when does it matter? J Appl Physiol Bethesda Md 1985 118:299–309. 10.1152/japplphysiol.00722.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadman RG (1979a) The assessment of sultriness. Part I: A temperature-humidity index based on human physiology and clothing science. J Appl Meteorol 18:861–873. [DOI] [Google Scholar]
- Steadman RG (1979b) The assessment of sultriness. Part II: effects of wind, extra radiation and barometric pressure on apparent temperature. J Appl Meteorol 18:874–885. [DOI] [Google Scholar]
- Stoecklin-Marois M, Hennessy-Burt T, Mitchell D, Schenker M (2013) Heat-related illness knowledge and practices among California hired farm workers in the MICASA study. Ind Health 51:47–55 [DOI] [PubMed] [Google Scholar]
- Sugg MM, Fuhrmann CM, Runkle JD (2018) Temporal and spatial variation in personal ambient temperatures for outdoor working populations in the southeastern USA. Int J Biometeorol 62:1521–1534. 10.1007/s00484-018-1553-z [DOI] [PubMed] [Google Scholar]
- Sunderland C, Morris JG, Nevill ME (2008) A heat acclimation protocol for team sports. Br J Sports Med 42:327–333. 10.1136/bjsm.2007.034207 [DOI] [PubMed] [Google Scholar]
- The Associated Press (2014) Court orders FIFA to implement water breaks. In: USA TODAY. https://www.usatoday.com/story/sports/soccer/2014/06/20/court-orders-fifa-to-implement-water-breaks/11106571/. Accessed 18 Dec 2017 [Google Scholar]
- Toloo G(S), FitzGerald G, Aitken P et al. (2013) Are heat warning systems effective? Environ Health 12:27. 10.1186/1476-069X-12-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tustin AW, Lamson GE, Jacklitsch BL et al. (2018) Evaluation of occupational exposure limits for heat stress in outdoor workers - United States, 2011-2016. MMWR Morb Mortal Wkly Rep 67:733–737. 10.15585/mmwr.mm6726a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Commerce N Heat Index (2018). https://www.weather.gov/safety/heat-index. Accessed 31 Aug 2018 [Google Scholar]
- USGCRP Climate science special report (2018) https://science2017.globalchange.gov/. Accessed 31 Aug 2018 [Google Scholar]
- Valdes AS, Hoffman JR, Clark MH, Stout JR (2014) National collegiate athletic association strength and conditioning coaches’ knowledge and practices regarding prevention and recognition of exertional heat stroke. J Strength Cond Res 28:3013–3023. 10.1519/JSC.0000000000000365 [DOI] [PubMed] [Google Scholar]
- Vanos JK, Warland JS, Gillespie TJ, Kenny NA (2010) Review of the physiology of human thermal comfort while exercising in urban landscapes and implications for bioclimatic design. Int J Biometeorol 54:319–334. 10.1007/s00484-010-0301-9 [DOI] [PubMed] [Google Scholar]
- Vitart F, Robertson AW (2018) The sub-seasonal to seasonal prediction project (S2S) and the prediction of extreme events. Npj Clim Atmospheric Sci 1:3. 10.1038/s41612-018-0013-0 [DOI] [Google Scholar]
- Vroman NB, Buskirk ER, Hodgson JL (1983) Cardiac output and skin blood flow in lean and obese individuals during exercise in the heat. J Appl Physiol 55:69–74. 10.1152/jappl.1983.55.1.69 [DOI] [PubMed] [Google Scholar]
- Wallace RF, Kriebel D, Punnett L et al. (2005) The effects of continuous hot weather training on risk of exertional heat illness. Med Sci Sports Exerc 37:84–90 [DOI] [PubMed] [Google Scholar]
- Wells CL, Buskirk ER (1971) Limb sweating rates overlying active and nonactive muscle tissue. J Appl Physiol 31:858–863. 10.1152/jappl.1971.31.6.858 [DOI] [PubMed] [Google Scholar]
- Wenz L, Levermann A (2016) Enhanced economic connectivity to foster heat stress–related losses. Sci Adv 2:e1501026. 10.1126/sciadv.1501026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH (2013) The epidemic of chronic kidney disease of unknown etiology in Mesoamerica: a call for interdisciplinary research and action. Am J Public Health 103:1927–1930. 10.2105/AJPH.2013.301594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whipp BJ, Wasserman K (1969) Efficiency of muscular work. J Appl Physiol 26:644–648. 10.1152/jappl.1969.26.5.644 [DOI] [PubMed] [Google Scholar]
- White CJ, Carlsen H, Robertson AW, Klein RJT, Lazo JK, Kumar A, Vitart F, Coughlan de Perez E, Ray AJ, Murray V, Bharwani S, MacLeod D, James R, Fleming L, Morse AP, Eggen B, Graham R, Kjellström E, Becker E, Pegion KV, Holbrook NJ, McEvoy D, Depledge M, Perkins-Kirkpatrick S, Brown TJ, Street R, Jones L, Remenyi TA, Hodgson-Johnston I, Buontempo C, Lamb R, Meinke H, Arheimer B, Zebiak SE (2017) Potential applications of subseasonal-to-seasonal (S2S) predictions. Meteorol Appl 24:315–325. 10.1002/met.1654 [DOI] [Google Scholar]
- Yaglou CP, Minard D (1957) Control of heat casualties at military training centers. AMA Arch Ind Health 16:302–316 [PubMed] [Google Scholar]
- Zander KK, Botzen WJW, Oppermann E, Kjellstrom T, Garnett ST (2015) Heat stress causes substantial labour productivity loss in Australia. Nat Clim Chang 5:647–651 [Google Scholar]
- Zhang H, Huizenga C, Arens E, Yu T (2001) Considering individual physiological differences in a human thermal model. J Therm Biol 26:401–408. 10.1016/S0306-4565(01)00051-1 [DOI] [Google Scholar]