Abstract
Objective:
To evaluate whether patients discharged to home after an emergency department (ED) visit for headache face a heightened short-term risk of stroke.
Background:
Stroke hospitalizations that occur soon after ED visits for headache complaints may reflect diagnostic error.
Methods:
We conducted a retrospective cohort study using statewide administrative claims data for all ED visits and admissions at nonfederal hospitals in Florida 2005–2018 and New York 2005–2016. Using standard International Classification of Diseases (ICD) codes, we identified adult patients discharged to home from the ED (treat-and-release visit) with a benign headache diagnosis (cohort of interest) as well as those with a diagnosis of renal colic or back pain (negative controls). The primary study outcome was hospitalization within 30 days for stroke (ischemic or hemorrhagic) defined using validated ICD codes. We assess the relationship between index ED visit discharge diagnosis and stroke hospitalization adjusting for patient demographics and vascular comorbidities.
Results:
We identified 1,502,831 patients with an ED treat-and-release headache visit; mean age was 41 (standard deviation: 17) years and 1,044,520 (70%) were female. A total of 2150 (0.14%) patients with headache were hospitalized for stroke within 30 days. In adjusted analysis, stroke risk was higher after headache compared to renal colic (hazard ratio [HR]: 2.69; 95% confidence interval [CI]: 2.29–3.16) or back pain (HR: 4.0; 95% CI: 3.74–4.3). In the subgroup of 26,714 (1.78%) patients with headache who received brain magnetic resonance imaging at index ED visit, stroke risk was only slightly elevated compared to renal colic (HR: 1.47; 95% CI: 1.22–1.78) or back pain (HR: 1.49; 95% CI: 1.24–1.80).
Conclusion:
Approximately 1 in 700 patients discharged to home from the ED with a headache diagnosis had a stroke in the following month. Stroke risk was three to four times higher after an ED visit for headache compared to renal colic or back pain.
Keywords: diagnostic error, emergency medicine, headache, stroke
INTRODUCTION
Missed emergency department (ED) diagnosis of dangerous cerebrovascular disease, particularly among patients presenting with mild or transient neurological symptoms, is a well-recognized public health issue estimated to occur in approximately 9% of all stroke patients.1,2 Headache complaints account for a substantial proportion of national ED visits.3,4 While the majority of headache complaints evaluated in the emergency setting are benign,4 an estimated 40,000 patients per year in the United States suffer adverse neurological events shortly after an ED headache visit resulting in discharge to home.5 Given that a variety of cerebrovascular conditions can manifest mainly as headache4,6,7 and that differentiating transient cerebral ischemia from migraine aura symptoms can be challenging,8 failure to accurately diagnose high-risk cerebrovascular events manifesting as headache may occur.
In this analysis, we evaluate whether ED headache visits that result in discharge to home are associated with a heightened risk of short-term stroke hospitalization and thus are suggestive of probable diagnostic error at index ED visit.9 We hypothesized that patients with an ED visit for headache would have a higher risk of stroke compared to patients with an ED visit for conditions not typically associated with stroke missed diagnosis: renal colic and back pain.5,10
METHODS
Design
We conducted a retrospective cohort study using publicly available, statewide administrative claims data provided to the Agency for Healthcare Research and Quality for its Healthcare Cost and Utilization Project (HCUP) by the Florida Agency for Health Care Administration and the New York Statewide Planning and Research Cooperative System. We included available data from all ED visits and hospitalizations to nonfederal hospitals in Florida from 2005–2018 and New York from 2006–2016.11 The two selected states in this study are large and demographically diverse; combined they compromise >10% of the US population.12 Each patient included in the HCUP database is assigned a personal linkage number that allows for anonymous tracking through ED and hospital encounters across institutions.13 The Weill Cornell Medicine institutional review board approved this study and granted a waiver of informed consent.
Diagnostic errors have been defined by the National Academies of Sciences, Engineering, and Medicine (NASEM) as a failure to establish an accurate and timely explanation of a patient’s health problem.1 Measuring diagnostic error rates using two points in time by pairing non-specific symptoms initially thought to be benign with an unexpected adverse health event is known as the Symptom-Disease Pair Analysis of Diagnostic Error (SPADE) conceptual approach.9 This approach has been previously employed to measure rates of missed cerebrovascular events using administrative claims data.14–16 In the current study, our direction of analysis is from index ED visit to subsequent stroke hospitalization for all patient groups constituting a look-forward SPADE study design.9 We consider a probable missed ED diagnosis of cerebrovascular disease as one in which a patient has a subsequent stroke hospitalization within 30 days of their index ED visit.14,17 Using ED visits that result in a discharge to home (treat-and-release) in a look-forward SPADE analysis is a popular strategy that relies on the presumption that patients who are sent home from the ED are those who are thought, at the time of their initial ED evaluation, to have low-risk conditions that can be managed in the outpatient setting.
Population
To construct our main study cohort, we identified patients ≥18 years of age with a first ED treat-and-release visit for headache during the study period. We defined an ED headache visit as one that resulted in a primary discharge diagnosis of tension-type headache, migraine with or without aura, cluster headache, cephalgia, or headache not otherwise specified using discharge diagnosis codes. Patients with an index ED visit prior to October 1, 2015 were identified using International Classification of Disease 9 Clinical Medicine (ICD-9-CM) codes; those with a visit on or after that date were identified using International Classification of Disease 10 (ICD-10) codes because this is when US hospitals transitioned from ICD-9-CM to ICD-10 codes. We used the ICD-9-CM codes 339, 346, 784.0, 307.81, 627.2, and the ICD-10 codes G43-G43.5x, G43.7x-G43.9x, G43.A-G43.D, G44, or R51 to identify headache patients.18,19 We defined patients with migraine with aura as those with primary ICD-9-CM discharge diagnosis of 346.0 or ICD-10 codes of G43.1 or G43.5.
To construct our negative control cohorts, we defined visits for renal colic as those that resulted in a primary ICD-9-CM discharge diagnosis code of 788.0 or an ICD-10 code of N2310 and back pain as those that resulted in primary ICD-9-CM discharge diagnosis codes 722.1, 722.2, 724, 847.1, 847.2, 847.9, or ICD-10 codes M54, M51.26 M51.27, M51.9, M48.00, or S39.0.5 Patients with ED treat-and-release visits for both headache and renal colic, both headache and back pain, or both back pain and renal colic were excluded from the analysis entirely to avoid contamination between groups. Patients who left the ED against medical advice, were hospitalized, or were transferred to another institution were also excluded from all study cohorts.
Measurements
We collected demographic data from HCUP. We used ICD-9-CM and ICD-10 codes to measure the following vascular comorbidities documented prior to and at index ED visit: hypertension, diabetes, coronary artery disease, congestive heart failure, hyperlipidemia, atrial fibrillation, peripheral vascular disease, chronic obstructive pulmonary disease, chronic kidney disease, tobacco use, and alcohol abuse.20–22 We captured vascular comorbidities documented prior to the index ED visit for as far back as we had available data, including comorbidities documented at any prior ED visits or inpatient admissions. We used Current Procedural Terminology (CPT) codes to measure the use of magnetic resonance imaging (MRI) of the brain. Patients with CPT codes 70551 or 70553 in any position at index ED visit were classified as having had a brain MRI at that visit.
Outcomes
The primary study outcome was hospitalization within 30 days for all stroke (ischemic or hemorrhagic). Secondary outcomes were ischemic stroke (IS), intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH) within 30 days of index ED visit. Stroke hospitalizations were defined using validated ICD-9-CM and ICD-10 discharge diagnosis codes. The ICD-9-CM diagnosis code algorithm we used was previously found to have a sensitivity of 86%, specificity of 95%, and a positive predictive value of 90% compared to medical record review;23 corresponding ICD-10 diagnostic codes for stroke are also highly reliable compared to medical record review.24
Statistical analysis
Standard descriptive statistics were used to characterize the study population, including means with standard deviations (SD) for normally distributed continuous variables and medians with interquartile ranges (IQR) for non-normally distributed continuous variables. Exact confidence intervals (CIs) were used to report crude stroke hospitalization rates for all cohorts at 30 days. We used Cox proportional hazards modeling to assess the relationship between index ED treat-and-release visit for the main study cohort (headache) compared to the two negative control cohorts (renal colic, back pain) and subsequent stroke hospitalization, while adjusting for all vascular comorbidities and demographics. We constructed cumulative hazard plots using the Nelson–Aalen estimator25,26 to graphically represent the proportion of subjects who experienced the outcome over time and derived smoothed hazard functions to show changes in the estimated incidence rate over time. Data were right censored in all models. To explore the impact of brain MRI testing on 30-day stroke risk, we used Cox proportional hazards modeling to compare the risk of stroke after headache in those with versus without MRI obtained at index ED visit.
We evaluated for effect modification by age (<40 vs. ≥40), sex, and vascular comorbidity burden (zero vs. ≥1 comorbidities) using formal interaction term analysis; we also performed analyses stratified by these factors. We evaluated these patient subgroups because age is used in existing clinical rules to identify secondary headaches acutely,27 disparities in ED stroke diagnosis by sex have been observed,28 and because low vascular comorbidity burden may reduce clinical suspicion for cerebrovascular disease. We performed a sensitivity analysis wherein patients with migraine with aura were excluded from the main study cohort as migraine with aura has been independently associated with increased IS risk.29,30 The threshold for statistical significance was set as <0.05. No statistical power calculation was conducted prior to the study because the sample size was based on the available HCUP data. There were no missing data. All tests of comparison were two-sided. Analyses were performed using Stata/MP, version 15.1 (StataCorp).
RESULTS
We identified 1,502,831 patients with an ED treat-and-release headache visit (Figure S1 in supporting information). The mean age of headache patients was 41 years (SD: 17) and 70% were female. For our negative control comparison cohorts, we identified 183,028 patients with renal colic and 2,729,020 with back pain (Figures S2 and S3 in supporting information). Baseline vascular comorbidities were similar between groups; more patients with headache were female (Table 1).
TABLE 1.
Characteristics of patients with headache, renal colic, and back pain
| Cohortsa | |||
|---|---|---|---|
| Characteristic | Headache (N = 1,502,831) | Renal colic (N = 183,028) | Low back pain (N = 2,729,020) |
| Age, mean (SD), years | 41 (17) | 45 (15) | 46 (18) |
| Female | 1,044,520 (70) | 64,690 (35) | 1,436,938 (53) |
| Race | |||
| White | 688,111 (46) | 120,994 (66) | 1,426,942 (52) |
| Black | 382,327 (25) | 12,333 (7) | 606,515 (22) |
| Hispanic | 295,955 (20) | 33,147 (18) | 478,697 (18) |
| Other | 136,438 (9) | 16,554 (9) | 216,866 (8) |
| Primary payer | |||
| Medicare | 192,869 (13) | 21,820 (12) | 471,629 (17) |
| Medicaid | 284,135 (19) | 18,014 (10) | 409,695 (15) |
| Private insurance | 668,982 (45) | 104,418 (57) | 1,066,069 (39) |
| Self-pay | 284,117 (19) | 31,840 (17) | 530,889 (19) |
| Other | 72,728 (5) | 6936 (4) | 250,738 (9) |
| Vascular comorbidities | |||
| History of stroke or transient ischemic attack | 25,725 (2) | 1070 (1) | 30,197 (1) |
| Coronary heart disease | 81,645 (5) | 9284 (5) | 195,428 (7) |
| Hypertension | 397,227 (26) | 38,808 (21) | 731,869 (27) |
| Diabetes | 152,544 (10) | 17,592 (10) | 326,781 (12) |
| Congestive heart failure | 29,468 (2) | 1830 (1) | 74,146 (3) |
| Peripheral vascular disease | 23,487 (2) | 2183 (1) | 57,901 (2) |
| Chronic kidney disease | 25,821 (2) | 1839 (1) | 56,947 (2) |
| Chronic obstructive pulmonary disease | 90,738 (6) | 5910 (3) | 208,000 (8) |
| Atrial fibrillation | 29,676 (2) | 2839 (2) | 69,928 (3) |
| Tobacco use | 76,219 (5) | 7181 (4) | 161,722 (6) |
| Alcohol abuse | 233,042 (16) | 21,452 (12) | 545,499 (20) |
| Number of vascular comorbidities | |||
| ≥1 | 628,659 (42) | 64,176 (35) | 1,233,783 (45) |
Abbreviation: SD, standard deviation.
Data are presented as number (%) unless otherwise specified.
A total of 2150 (0.14%) patients with headache were hospitalized for stroke within 30 days. Median time to stroke hospitalization from ED visit was 6 (IQR: 2–15) days among patients with headache. Thirty-eight (0.02%) patients were hospitalized for stroke in the cohort of patients with renal colic and 1193 (0.04%) patients were hospitalized for stroke in the cohort of patients with back pain.
After adjusting for demographics and vascular comorbidities, stroke risk was higher among patients with headache compared to patients diagnosed with renal colic (hazard ratio [HR]: 2.69; 95% CI: 2.29–3.16) or back pain (HR: 4.0; 95% CI: 3.74–4.3; Figure 1). After excluding patients with migraine with aura (n = 9416), stroke risk after ED headache visit remained elevated compared to patients with renal colic (HR: 2.29; 95% CI: 1.93–2.72) and back pain (HR: 3.28; 95% CI: 3.02–3.57).
FIGURE 1.
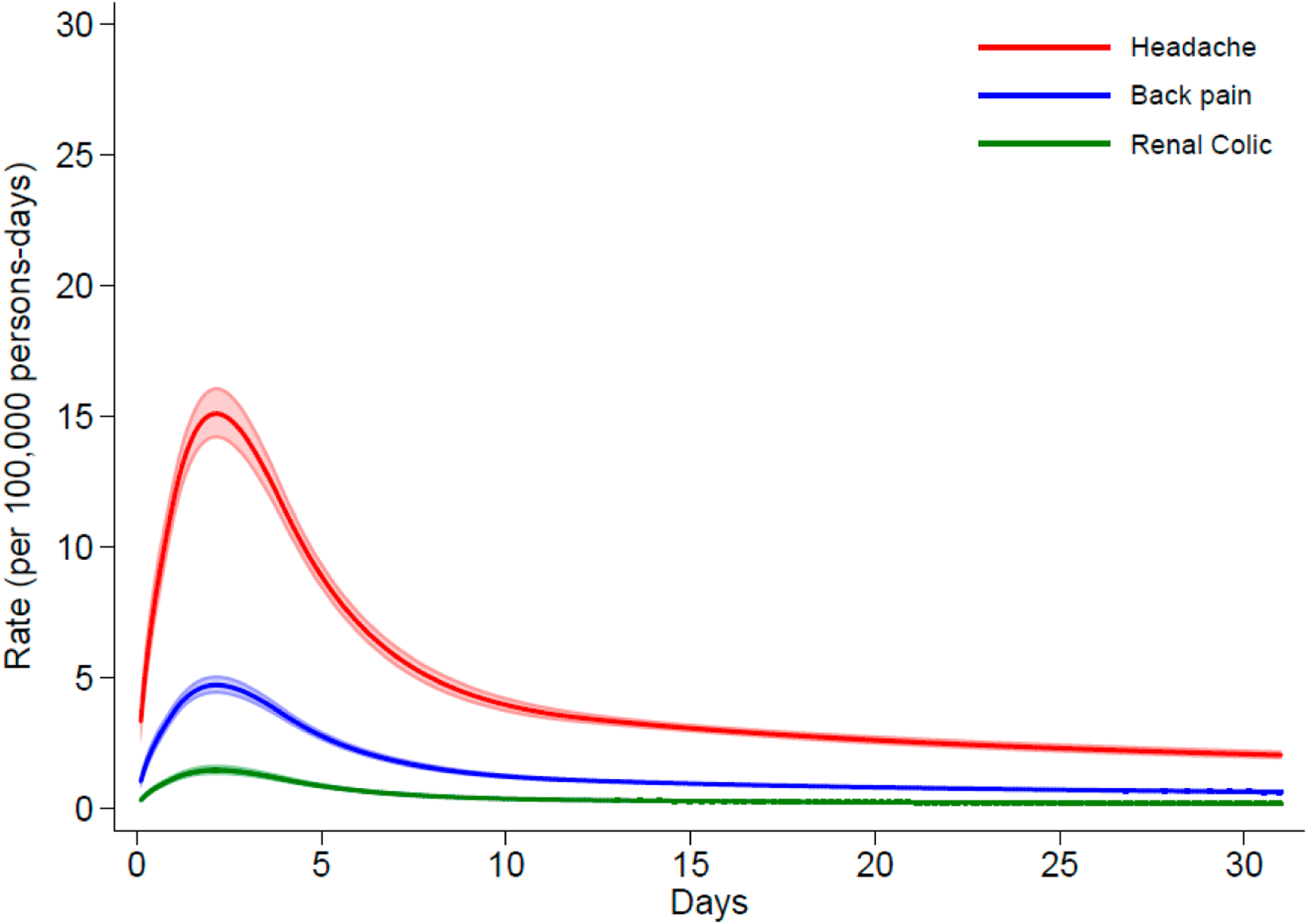
Stroke risk after emergency department (ED) treat-and-release visit. Rate per 100,000 person-days of stroke hospitalizations among patients discharged from EDs with diagnosis of headache or renal colic or low back pain. Shaded areas represent the 95% confidence intervals.
For our secondary outcomes, we identified a total of 1478 (63%) patients with a primary diagnosis of IS, 328 (14%) with ICH, and 527 (23%) with SAH. Risk of IS was higher among patients with headache compared to patients with renal colic (HR: 2.3; 95% CI: 1.93–2.73) or back pain (HR: 3.30; 95% CI: 3.03–3.58), as was the risk of ICH compared to patients with renal colic (HR: 2.88; 95% CI: 1.84–4.5) or back pain (HR: 4.5; 95% CI: 3.72–5.5). Among patients with headache, risk of SAH within 30 days of index ED visit was considerably higher compared to patients with back pain (HR: 14.5; 95% CI: 11.2–18.9); no SAH occurred in renal colic patients (Table 2).
TABLE 2.
Primary and secondary outcomes at 30 days from headache visita
| HR (compared to renal colic) | HR (compared to back pain) | |
|---|---|---|
| Primary outcome | ||
| All stroke | 2.69 (95% CI, 2.29–3.16) | 4.0 (95% CI, 3.74–4.3) |
| Secondary outcomes | ||
| Ischemic stroke | 2.30 (95% CI, 1.93–2.73) | 3.30 (95% CI, 3.03–3.58) |
| Intracerebral hemorrhage | 2.88 (95% CI, 1.84–4.5) | 4.5 (95% CI, 3.72–5.5) |
| Subarachnoid hemorrhage | -b | 14.5 (95% CI, 11.2–18.9) |
Abbreviations: CI, confidence interval; HR, hazard ratio.
Model adjusted for age, race/ethnicity, and all vascular comorbidities.
No one had a subarachnoid hemorrhage in the renal colic group.
A total of 26,714 patients with headache (1.78%) had a brain MRI at index ED visit. Of those with a brain MRI, 28 (0.10%) had a stroke hospitalization within 30 days. Stroke risk remained slightly elevated among headache patient with an MRI obtained compared to patients with renal colic (HR: 1.47; 95% CI: 1.22–1.78) or back pain (HR: 1.45; 95% CI: 1.24–1.80); among patients with headache who did not have an MRI, stroke risk was higher compared to patients with renal colic (HR: 2.70; 95% CI: 2.30–3.18) or back pain (HR: 4.0; 95% CI: 3.77–4.3; Table 3). Comparing patients with headache who did versus did not have an MRI at index ED visit, short-term stroke risk was lower for those who had an MRI (HR: 0.686; 95% CI: 0.598–0.786) after adjustment for demographics and vascular comorbidities.
TABLE 3.
Stroke admissions within 30 days from headache visit by brain MRIa
| HR (compared to renal colic) | HR (compared to back pain) | |
|---|---|---|
| All stroke | ||
| Headache without MRI | 2.70 (95% CI,2.30–3.18) | 4.0 (95% CI, 3.77–4.3) |
| Headache with MRI | 1.47 (95% CI, 1.22–1.78) | 1.49 (95% CI, 1.24–1.80) |
Abbreviations: CI, confidence interval; HR, hazard ratio; MRI, magnetic resonance imaging.
Model adjusted for age, race/ethnicity, and all vascular comorbidities.
Among patients <40 years of age, stroke risk was higher among patients with headache compared to those with back pain (HR: 10.7; 95% CI: 7.9–14.7); no strokes occurred in patients with renal colic less than 40 years of age (Figure 2). There was an interaction between age (p < .001) and headache in relation to stroke, with a significantly higher risk of stroke associated with headache in younger patients than that seen in older patients. No interactions between sex and headache in relation to stroke were seen. Compared to both renal colic and back pain, there was an interaction between vascular comorbidity burden and headache (p = .013 and p < .001, respectively) in relation to stroke, with significantly higher risk of stroke associated with having no vascular comorbidities (Table 4).
FIGURE 2.
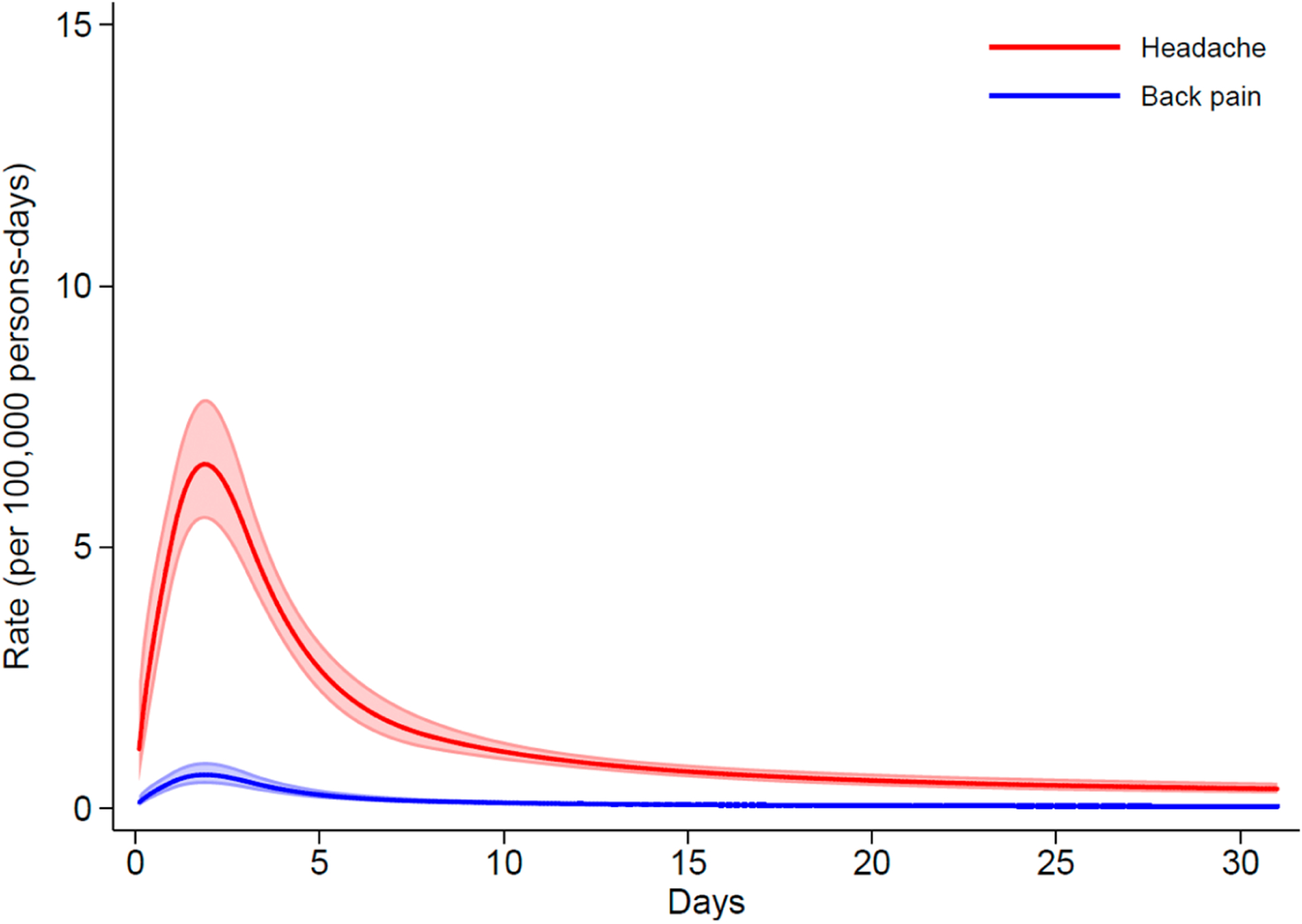
Stroke risk after emergency department (ED) treat-and-release visit in patients <40 years of age. Rate per 100,000 person-days of stroke hospitalizations among patients <40 years of age discharged from EDs with diagnosis of headache or low back pain. Shaded areas represent the 95% confidence intervals.
TABLE 4.
Risk of all stroke at 30 days from headache visit: subgroup analysisa
| HR (compared to renal colic) | HR (compared to back pain) | |
|---|---|---|
| Age (years) | ||
| Age < 40 | -b | 10.7 (95% CI, 7.9–14.7) |
| Age ≥ 40 | 2.65 (95% CI, 2.26–3.12) | 3.74 (95% CI, 3.47–4.0) |
| P for interaction | -b | p < .001 |
| Sex | ||
| Female | 2.64 (95% CI, 1.98–3.50) | 3.92 (95% CI, 3.57–4.31) |
| Male | 2.76 (95% CI, 2.27–3.36) | 4.1 (95% CI, 3.70–4.6) |
| P for interaction | p = .891 | p = .490 |
| Number of vascular comorbidities | ||
| 0 | 3.92 (95% CI, 2.82–5.5) | 7.5 (95% CI, 6.4–8.7) |
| ≥1 | 2.26 (95% CI, 1.88–2.73) | 3.30 (95% CI, 3.04–3.58) |
| P for interaction | p = .013 | p < .001 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
Model adjusted for age, race/ethnicity, and all vascular comorbidities.
No one had a stroke in the renal colic group.
DISCUSSION
We found that approximately 1 out of every 700 patients with an ED treat-and-release headache visit had a stroke within 30 days. Stroke risk after a headache visit was higher than stroke risk after ED visits for renal colic and back pain after accounting for vascular comorbidities and demographics.
The rate of stroke hospitalization within 30 days of ED headache treat-and-release visit that we found is similar to that of previously published studies (0.14%–0.5%).5,31 These associations between headache visits and subsequent stroke hospitalizations suggest that, for a small proportion of patients, ED headache visits may represent an opportunity to reduce short-term stroke risk. Though the absolute percentages are small, because the annual volume of headache complaints seen in US EDs is approximately 3 million patients per year, they correspond to 4200–15,000 potentially missed opportunities to prevent cerebrovascular disease annually.3 Improving diagnostic accuracy for cerebrovascular conditions in the ED may play an important role in decreasing subsequent stroke hospitalizations, particularly in younger patients. Indeed, prior research has demonstrated non-trivial rates of probable missed ED diagnoses of transient ischemic attack (TIA), minor stroke, cervicocephalic dissection, cerebral venous thrombosis, and SAH, which can all present acutely with headache.6,14–16 The proportion of ED treat-and-release headache visits before stroke hospitalization that were clear instances of diagnostic error (as opposed to just being temporally associated with stroke hospitalizations for other reasons) should be studied further.
Our finding that patients with headache who received a brain MRI at index ED visit were at decreased risk of subsequent stroke compared to headache patients who did not have an MRI and that stroke risk among headache patients with brain MRI is only slightly higher than that of renal colic or back pain patients is novel. Prior research has shown that among patients with non-specific neurological complaints (dizziness, headache, non-motor symptoms) obtaining a head computed tomography (CT) in the ED prior to discharge to home is associated with increased subsequent stroke risk compared to patients who do not have a head CT.19,32,33 Some investigators have postulated that this increased risk is explained by ED providers being falsely reassured by a negative head CT in the setting of a true cerebrovascular event (e.g., sentinel bleed or high-risk TIA/minor stroke).33 In contrast, we found that ED patients with headache upon whom a brain MRI was obtained had low rates of short-term stroke. Given the superior accuracy of MRI for ischemic stroke detection compared to head CT,34 our findings suggest that patients with headache upon whom brain MRI is obtained at index ED treat-and-release visit truly lack acute cerebrovascular pathology. Determining which ED patients with headache complaints warrant advanced neuroimaging or other diagnostic testing to expedite a safe discharge to home and avoid short-term cerebrovascular events as well as the cost effectiveness of various ED-based evaluative approaches is an important topic for future health services research.35–37
In our subgroup and sensitivity analyses, stroke risk remained consistently higher after ED headache treat-and-release visits than renal colic and back pain visits. Headache patients <40 years of age were at substantially increased risk of stroke compared to renal colic and back pain patients of the same age; this subgroup of young headache patients may be a particularly important one to focus on when designing interventions to improve ED diagnostic accuracy.14,38 Additionally, headache patients without vascular comorbidities were at increased risk of subsequent stroke compared to renal colic and back pain patients. This suggests that physicians should remain vigilant when evaluating ED patients without typical stroke risk factors who have neurological complaints.
Our current study has several limitations. Classifying primary headache subtypes in the ED is a known challenge that is difficult to address even when structured interviews are used for classification.39 Furthermore, reliance on administrative claims data to identify headache subtypes, including migraine with aura, is imperfect and can lead to headache misclassification.40 We do not know patients’ exact presenting symptoms, imaging results, nor medications administered or stopped in the ED. We are thus unable to assess whether guideline recommendations regarding diagnostic evaluation of headache complaints, which may include lumbar puncture in some cases, were followed. Additionally, though we used validated ICD-9-CM and ICD-10 codes to identify all study outcomes, our outcome ascertainment relies on a subsequent hospitalization occurring and, therefore, we could not identify stroke patients who were never hospitalized (those who did not seek care, those who were cared for exclusively in the outpatient setting, and those who died before hospitalization). Therefore, our measurement of stroke hospitalization likely underestimates the true rate of subsequent cerebrovascular events in all cohorts. Finally, we did not evaluate the influence of facility-level and/or provider-level factors on subsequent stroke risk though some of these factors have been previously associated with diagnostic error.6,14
Strengths of our study include using a multicenter, large database that can account for hospital crossover (being seen at one health-care organization and then hospitalized at a separate organization), which frequently occurs in patients with delayed or missed diagnosis.31 We also carefully accounted for known vascular comorbidities when comparing stroke risk between our cohort of interest and the negative comparator groups in contrast to prior large studies measuring missed stroke diagnosis among ED patients with neurological symptoms, including headache.5,18,19
CONCLUSION
In a SPADE style look-forward analysis, we found that short-term stroke risk is higher after an ED treat-and-release visit for headache compared to visits for renal colic or back pain. In the subgroup of patients with headache who received brain MRI prior to ED discharge, stroke risk was reduced. Patients younger than 40 years of age as well as those lacking vascular comorbidities who come to the ED with headache complaints are at substantially higher risk of subsequent stroke hospitalization and may represent an important target for future interventions to improve ED diagnostic accuracy.
Supplementary Material
Funding information
NINDS research grant K23NS10764
CONFLICTS OF INTEREST
Dr. Liberman is supported by NINDS research grant K23NS10764. Dr. Lipton reports receiving research support from the NIH, FDA as well as the National Headache Foundation and the Marx Foundation. Dr. Parikh is supported by NIA research grant K23AG073524 and the Florence Gould Foundation, has received support from the NY State Empire Clinical Research Investigator Program and Leon Levy Foundation, and has received personal fees for medicolegal consulting. Dr. Lipton also receives research support from Allergan/Abbvie, Amgen, Eli Lilly and Electrocore. He receives personal fees as a consultant or advisor from Allergan/Abbvie, Amgen, Biohaven Holdings, Dr. Reddy’s, GlaxoSmithKline, Grifols, Lundbeck, Merck, Novartis and Teva Pharmaceuticals. He holds stock or options in Biohaven Holdings, CtrlM Health and Manistee. In addition, he receives royalties for Wolff’s Headache 7th and 8th Edition. Dr. Kamel serves as a PI for the NIH-funded ARCADIA trial (NINDS U01NS095869), which receives inkind study drug from the BMS-Pfizer Alliance for Eliquis® and ancillary study support from Roche Diagnostics; as Deputy Editor for JAMA Neurology; on clinical trial steering/executive for Peer Review committees for Medtronic, Janssen, and Javelin Medical; and on endpoint adjudication committees for NovoNordisk and Boehringer-Ingelheim, not directly related to this work. Dr. Merkler has received personal fees for serving as a neurology expert witness.
Abbreviations:
- CT
computed tomography
- ED
emergency department
- HCUP
Healthcare Cost and Utilization Project
- ICH
intracerebral hemorrhage
- IS
ischemic stroke
- MRI
magnetic resonance imaging
- NASEM
National Academies of Sciences, Engineering, and Medicine
- SAH
subarachnoid hemorrhage
- SPADE
Symptom-Disease Pair Analysis of Diagnostic Error
Footnotes
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study can be obtained through application directly from HCUP. The analytical code used will be made available upon reasonable request from the corresponding author.
REFERENCES
- 1.Balogh E, Miller BT, Ball J, et al. Improving Diagnosis in Health Care. The National Academies Press; 2015. [PubMed] [Google Scholar]
- 2.Tarnutzer AA, Lee SH, Robinson KA, Wang Z, Edlow JA, Newman-Toker DE. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: a meta-analysis. Neurology. 2017;88(15):1468–1477. doi: 10.1212/WNL.0000000000003814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lucado J, Paez K, Elixhauser A. Headaches in U.S. Hospitals and Emergency Departments, 2008. HCUP statistical brief #111. Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 4.Goldstein JN, Camargo CA Jr, Pelletier AJ, Edlow JA. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 2006;26(6):684–690. doi: 10.1111/j.1468-2982.2006.01093.x [DOI] [PubMed] [Google Scholar]
- 5.Dubosh NM, Edlow JA, Goto T, Camargo CA Jr, Hasegawa K. Missed serious neurologic conditions in emergency department patients discharged with nonspecific diagnoses of headache or Back pain. Ann Emerg Med. 2019;74(4):549–561. doi: 10.1016/j.annemergmed.2019.01.020 [DOI] [PubMed] [Google Scholar]
- 6.Vermeulen MJ, Schull MJ. Missed diagnosis of subarachnoid hemorrhage in the emergency department. Stroke. 2007;38(4): 1216–1221. doi: 10.1161/01.STR.0000259661.05525.9a [DOI] [PubMed] [Google Scholar]
- 7.Koudstaal PJ, van Gijn J, Kappelle LJ. Headache in transient or permanent cerebral ischemia. Dutch TIA Study Group. Stroke. 1991;22(6):754–759. doi: 10.1161/01.str.22.6.754 [DOI] [PubMed] [Google Scholar]
- 8.Otlivanchik O, Liberman AL. Migraine as a stroke mimic and as a stroke chameleon. Curr Pain Headache Rep. 2019;23(9):63. doi: 10.1007/s11916-019-0801-1 [DOI] [PubMed] [Google Scholar]
- 9.Liberman AL, Newman-Toker DE. Symptom-disease pair analysis of diagnostic error (SPADE): a conceptual framework and methodological approach for unearthing misdiagnosis-related harms using big data. BMJ Qual Saf. 2018;27(7):557–566. doi: 10.1136/bmjqs-2017-007032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atzema CL, Grewal K, Lu H, Kapral MK, Kulkarni G, Austin PC. Outcomes among patients discharged from the emergency department with a diagnosis of peripheral vertigo. Ann Neurol. 2016;79(1):32–41. doi: 10.1002/ana.24521 [DOI] [PubMed] [Google Scholar]
- 11.Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; 2019. Accessed February 13, 2020. https://www.hcup-us.ahrq.gov. [PubMed]
- 12.United States Census Bureau. Accessed February 20, 2021. 2021. https://data.census.gov/.
- 13.Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues When Studying Readmissions and Revisits Using Hospital Administrative Data. HCUP Methods Series Report 2011–01; online March 9, 2011. Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 14.Newman-Toker DE, Moy E, Valente E, Coffey R, Hines AL. Missed diagnosis of stroke in the emergency department: a cross-sectional analysis of a large population-based sample. Diagnosis. 2014;1(2):155–166. doi: 10.1515/dx-2013-0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberman AL, Gialdini G, Bakradze E, Chatterjee A, Kamel H, Merkler AE. Misdiagnosis of cerebral vein thrombosis in the emergency department. Stroke. 2018;49(6):1504–1506. doi: 10.1161/STROKEAHA.118.021058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liberman AL, Navi BB, Esenwa CC, et al. Misdiagnosis of Cervicocephalic artery dissection in the emergency department. Stroke. 2020;51(6):1876–1878. doi: 10.1161/STROKEAHA.120.029390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang TP, Bery AK, Wang Z, et al. Stroke hospitalization after misdiagnosis of “benign dizziness” is lower in specialty care than general practice: a population-based cohort analysis of missed stroke using SPADE methods. Diagnosis. 2021;9:96–106. doi: 10.1515/dx-2020-0124 [DOI] [PubMed] [Google Scholar]
- 18.Liberman AL, Lu J, Wang C, Cheng NT, Moncrieffe K, Lipton RB. Factors associated with hospitalization for ischemic stroke and TIA following an emergency department headache visit. Am J Emerg Med. 2020;46:503–507. doi: 10.1016/j.ajem.2020.10.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberman AL, Wang C, Friedman BW, et al. Head computed tomography during emergency department treat-and-release visit for headache is associated with increased risk of subsequent cerebrovascular disease hospitalization. Diagnosis. 2020;8:199–208. doi: 10.1515/dx-2020-0082 [DOI] [PubMed] [Google Scholar]
- 20.Boehme AK, Esenwa C, Elkind MS. Stroke risk factors, genetics, and prevention. Circ Res. 2017;120(3):472–495. doi: 10.1161/CIRCRESAHA.116.308398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Portegies ML, Lahousse L, Joos GF, et al. Chronic obstructive pulmonary disease and the risk of stroke. The Rotterdam study. Am J Respir Crit Care Med. 2016;193(3):251–258. doi: 10.1164/rccm.201505-0962OC [DOI] [PubMed] [Google Scholar]
- 22.Masson P, Webster AC, Hong M, Turner R, Lindley RI, Craig JC. Chronic kidney disease and the risk of stroke: a systematic review and meta-analysis. Nephrol Dial Transplant. 2015;30(7):1162–1169. doi: 10.1093/ndt/gfv009 [DOI] [PubMed] [Google Scholar]
- 23.Tirschwell DL, Longstreth WT Jr. Validating administrative data in stroke research. Stroke. 2002;33(10):2465–2470. doi: 10.1161/01.str.0000032240.28636.bd [DOI] [PubMed] [Google Scholar]
- 24.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36(8):1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1 [DOI] [PubMed] [Google Scholar]
- 25.Nelson W. Theory and applications of Hazard plotting for censored failure data. Dent Tech. 1972;14(4):945–966. doi: 10.1080/00401706.1972.10488991 [DOI] [Google Scholar]
- 26.Aalen O Nonparametric inference for a family of counting processes. Ann Stat. 1978;6(4):701–726. doi: 10.1214/aos/1176344247 [DOI] [Google Scholar]
- 27.Do TP, Remmers A, Schytz HW, et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology. 2019;92(3):134–144. doi: 10.1212/WNL.0000000000006697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu AYX, Penn AM, Lesperance ML, et al. Sex differences in presentation and outcome after an acute transient or minor neurologic event. JAMA Neurol. 2019;76(8):962–968. doi: 10.1001/jamaneurol.2019.1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurth T, Kase CS, Schurks M, Tzourio C, Buring JE. Migraine and risk of haemorrhagic stroke in women: prospective cohort study. BMJ. 2010;341:c3659. doi: 10.1136/bmj.c3659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339:b3914. doi: 10.1136/bmj.b3914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liberman AL, Hassoon A, Fanai M, et al. Cerebrovascular disease hospitalizations following emergency department headache visits: a nested case-control study. Acad Emerg Med. 2021;29:41–50. doi: 10.1111/acem.14353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenman MB, Oh E, Richards CT, et al. Risk of stroke after emergency department visits for neurologic complaints. Neurol Clin Pract. 2020;10(2):106–114. doi: 10.1212/CPJ.0000000000000673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grewal K, Austin PC, Kapral MK, Lu H, Atzema CL. Missed strokes using computed tomography imaging in patients with vertigo: population-based cohort study. Stroke. 2015;46(1):108–113. doi: 10.1161/STROKEAHA.114.007087 [DOI] [PubMed] [Google Scholar]
- 34.Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369(9558):293–298. doi: 10.1016/S0140-6736(07)60151-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liberman AL, Zhang H, Rostanski SK, et al. Cost-effectiveness of advanced neuroimaging for transient and minor neurological events in the emergency department. J Am Heart Assoc. 2021;10(12):e019001. doi: 10.1161/JAHA.120.019001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coutts SB, Moreau F, Asdaghi N, et al. Rate and prognosis of brain ischemia in patients with lower-risk transient or persistent minor neurologic events. JAMA Neurol. 2019;76(12):1439–1445. doi: 10.1001/jamaneurol.2019.3063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Newman-Toker DE, McDonald KM, Meltzer DO. How much diagnostic safety can we afford, and how should we decide? A health economics perspective. BMJ Qual Saf. 2013;22:ii11–ii20. doi: 10.1136/bmjqs-2012-001616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuruvilla A, Bhattacharya P, Rajamani K, Chaturvedi S. Factors associated with misdiagnosis of acute stroke in young adults. J Stroke Cerebrovasc Dis. 2011;20(6):523–527. doi: 10.1016/j.jstrokecerebrovasdis.2010.03.005 [DOI] [PubMed] [Google Scholar]
- 39.Friedman BW, Hochberg ML, Esses D, et al. Applying the international classification of headache disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. 2007;49(4):409–419, 19 e1–9. doi: 10.1016/j.annemergmed.2006.11.004 [DOI] [PubMed] [Google Scholar]
- 40.Kolodner K, Lipton RB, Lafata JE, et al. Pharmacy and medical claims data identified migraine sufferers with high specificity but modest sensitivity. J Clin Epidemiol. 2004;57(9):962–972. doi: 10.1016/j.jclinepi.2004.01.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study can be obtained through application directly from HCUP. The analytical code used will be made available upon reasonable request from the corresponding author.


